To the Editor: The symptoms of cerebral fat embolism (CFE) are often a triad of acute respiratory failure, unconsciousness, and petechial rash after a symptom-free interval of 12–24 h following trauma. Although cases of CFE have been reported since the 1960s, to our knowledge, a few reports have discussed the beneficial effects of corticosteroids for CFE treatment though corticosteroids are generally believed to have preventative effects. Here, we report a case of CFE in a 63-year-old woman who had fractures of the right tibia and fibula without cranial trauma. We gave her intravenous injections of dexamethasone for 11 days starting from the 1st day of trauma, and the patient experienced good recovery.
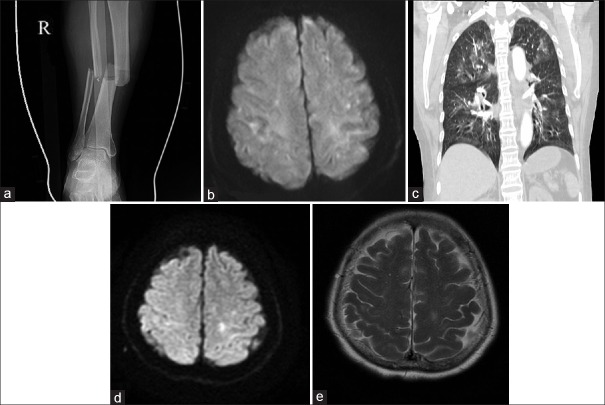
A 63-year-old previously healthy woman was involved in a traffic accident while running. She was diagnosed with the right tibia and fibula fractures without cranial trauma or initial loss of consciousness [Figure 1a]. Emergent debridement was performed, and a calcaneus traction pin was placed in the preparation for surgical reduction. Four hours after the accident, the patient became confused, agitated, and exhibited tachycardia (heart rate 110 beats/min) while showing a normal oxygen saturation of 98%, partial pressure of blood oxygen (PaO2) of 95.8 mmHg (1 mmHg = 0.133 kPa), fraction of inspired oxygen (FiO2) of 30%, and body temperature of 36.8°C. Immediate diffusion-weighted magnetic resonance imaging (DW-MRI) of the brain revealed punctate foci of restricted diffusion in a “starfield” pattern [Figure 1b]. Dexamethasone (10 mg) was administered through intravenous injection. Twenty hours after the accident, the patient developed acute respiratory failure (oxygen saturation 80%, FiO245%) and became progressively unconscious with a Glasgow Coma Scale (GCS) score of 3, requiring intubation and admission to the Intensive Care Unit. Computed tomography angiography of the chest showed bilateral ground-glass opacities without pulmonary embolism [Figure 1c]. After about 30 min, her hypoxemia was corrected with intensive mechanical ventilation (oxygen saturation 100%, PaO2221 mmHg, FiO250%). Nevertheless, she remained in a coma (GCS score of 5). Another 10 mg dexamethasone was administered intravenously, and supportive care including ventilator-assisted breathing and nutritional support was continued. Then, a petechial rash was noted in her axillary and lumbar regions, her body temperature reached 38.0°C, and she became highly irritable. Dexmedetomidine (0.04 µg·kg−1·min−1) was given continuously through an intravenous pump, and a Richmond Agitation and Sedation Scale score of around −2 was maintained. Her blood platelet count was 96 × 109/L at admission but then gradually decreased to 68 × 109/L by the 3rd day and then gradually recovered to within the normal range. Transthoracic echocardiography showed a patent foramen ovale, with no signs of structural anomalies, such as right-to-left shunt or intrapulmonary shunt, which could potentially lead to respiratory failure.
Figure 1.
(a) Radiograph of the right leg showing tibia and fibula fractures. (b) Four hours after the accident, diffusion-weighted magnetic resonance imaging of the brain showed some punctate foci of restricted diffusion in a starfield pattern. (c) Twenty hours after the accident, computed tomography angiography of the chest showed bilateral ground-glass opacities, without pulmonary embolism. Ten days after the accident, diffusion-weighed magnetic resonance imaging (d) and T2-weighted magnetic resonance imaging (e) of the brain showed a high-signal focus in the left semioval center.
Considering the patient had acute respiratory failure, a petechial rash in remote areas far from the trauma, and starfield-patterned restricted diffusion in the brain, the diagnosis of CFE was made. Six days after the accident, dexmedetomidine was stopped temporarily to allow neurological assessment, which showed that the patient was responsive to external stimuli. Nine days after the accident, she was successfully extubated and began to show neurological recovery. Ten days after the accident, DWI and T2-weighted MRI of the brain showed a high-signal focus in the left semioval center [Figure 1d and 1e]. Dexamethasone had been administered intravenously on a daily basis consecutively with a single dose of 10 mg for 7 days from the day of the accident and at a reduced dose of 5 mg for 4 days from the 8th day after the accident until the patient was transferred to the Orthopedics Department on the 11th day. Fourteen days after the accident, the tibial fracture was treated with external fixation. One month later, the patient was discharged from the hospital without any residual neurological deficit. At the 6-month follow-up, no residual neurological deficits were noted, and the patient could live independently and work as before.
CFE is a rare but potentially life-threatening complication of orthopedic trauma and intramedullary manipulation, with a mortality rate of up to 10% currently.[1] The diagnostic criteria for CFE were first proposed by Gurd[2] in 1970. Consistently, our patient presented with acute respiratory failure without signs of pulmonary embolism, a petechial rash far from the trauma, and starfield-patterned restricted diffusion in the brain. Such restricted diffusion formed within 20 h after trauma and developed into confluent cytotoxic cerebral edema in the left semioval center by 10 days after trauma. This was largely consistent with findings reported in the literature.[3]
CFE is mostly seen in cases of closed, long bone fractures of the lower extremities, particularly with multiple (≥3 sites) long bone fractures.[4] The pathogenesis of CFE is still not entirely clear. After long bone fractures, fat may be mobilized from the bone marrow, enter the circulation, and embolize the lung, brain, and skin, causing acute respiratory failure, neurological symptoms, and petechial rash, respectively.[3]
CFE is often self-limiting, and usually, patients eventually recover over weeks or months. Nevertheless, appropriate early management is essential to reduce the risk of mortality. There are currently no disease-specific treatments for CFE, and the management is mainly supportive.[1] Corticosteroids were thought to be beneficial only for preventing but not treating fat embolism.[5] However, our patient showed a sensitive response to intravenous dexamethasone therapy. She was extubated early, and her brain MRI showed recovery of most of the spot lesions. This may be related to the relatively longer period of dexamethasone injection, especially in the early stage. For a comprehensive discussion of the diagnosis, pathology, management, prevention, and prognosis of CFE, one can refer to previous publications.[1,2] This study highlights the potential of CFE after unilateral tibia and fibula fracture. More importantly, this report provides evidence of the usefulness of early-initiated, prolonged intravenous dexamethasone therapy for CFE management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Kosova E, Bergmark B, Piazza G. Fat embolism syndrome. Circulation. 2015;131:317–20. doi: 10.1161/CIRCULATIONAHA.114.010835. doi: 10.1161/CIRCULATIONAHA.114.010835. [DOI] [PubMed] [Google Scholar]
- 2.Gurd AR. Fat embolism: An aid to diagnosis. J Bone Joint Surg Br. 1970;52:732–7. [PubMed] [Google Scholar]
- 3.Aman J, van Koppenhagen L, Snoek AM, van der Hoeven JG, van der Lely AJ. Cerebral fat embolism after bone fractures. Lancet. 2015;386:e16. doi: 10.1016/S0140-6736(15)60064-2. doi: 10.1016/S0140-6736(15)60064-2. [DOI] [PubMed] [Google Scholar]
- 4.Han YT, Tang J, Gao ZQ, Hu HT. Clinical features and neuroimaging findings in patients with cerebral fat embolism. Chin Med J. 2016;129:874–6. doi: 10.4103/0366-6999.178963. doi: 10.4103/0366-6999.178963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bederman SS, Bhandari M, McKee MD, Schemitsch EH. Do corticosteroids reduce the risk of fat embolism syndrome in patients with long-bone fractures?A meta-analysis. Can J Surg. 2009;52:386–93. [PMC free article] [PubMed] [Google Scholar]