Abstract
Background
Cocaine use and its consequences are disproportionately higher and more severe among African Americans compared to other ethnic/racial groups.
Objectives
The aims of this study were to examine a risk model specific for African American users and assess whether risk varies as a function of sex.
Methods
270 African American adults in a residential drug treatment facility completed measurements assessing first and past year crack/cocaine use frequency, childhood trauma, and stress reactivity. Multiple linear regression analysis was used to examine the unique effect of each predictor variable on past year crack/cocaine frequency. Sex was included as a moderator variable in the regression analysis.
Results
All predictor variables were positively correlated with past year crack/cocaine use. However, sex differences were also observed: females reported higher rates of childhood emotional abuse, childhood sexual abuse, and stress reactivity – as well as past year crack use and cocaine use – than males. Regression analyses were performed with sex, first year use, and stress reactivity emerging as the only significant predictors for frequency of crack and cocaine use among all study participants. Moreover, sex differences were observed in the influence of first year crack use frequency on past year crack use frequency, such that the effect was stronger for males than for females.
Conclusion/Importance
This study offers a clearer understanding of the risk factors for crack and cocaine abuse specific to African Americans, as well as sex specific pathways to risk, providing useful implications for future prevention and treatment efforts.
Keywords: African American, race, cocaine use, risk, treatment
INTRODUCTION
Cocaine is a highly addictive drug, with one in every 16 to 20 cocaine users becoming dependent within their first year of use (Wagner & Anthony, 2002). Moreover, the negative health consequences of cocaine use are manifold – some of the most frequent being cardiovascular effects, such as disturbances in heart rhythm and heart attacks (NIDA, 2010; Pozner, Levine, & Zane, 2005); reduction in pulmonary functioning (NIDA, 2010); respiratory failure (Riezzo, Fiore, Ce Carlo, Pasacale, Neri, Turillazzi, & Fineschi, 2012); neurological effects, including strokes, seizures, headaches, and coma (NIDA, 2010; Treadwell & Robinson, 2007); sexual dysfunction (Carey, 2006; Palha & Esteves, 2008); gastrointestinal complications, including abdominal pain and nausea (Muniz & Evans, 2001; NIDA, 2010); kidney and liver damage (Riezzo et al., 2012; Valente, Carvalho, Bastos, de Pinho, & Carvalho, 2012); and death (NIDA, 2010).
Important racial disparities in prevalence and consequences from cocaine use have also been noted, indicating heightened risk of cocaine use frequency (Palamar, Davies, Ompad, Cleland, & Weitzman, 2015), lifetime cocaine use (Ma & Shive, 2000), cocaine dependence (Chen & Kandel, 2002; Compton, Cottler, Ben Abdallah, Phelps, Spitznagel, & Horton, 2000; O’Brien & Anthony, 2005) and adverse health and social consequences due to cocaine use (Bernstein, Bucciarelli, Piper, Gross, Tardiff, & Galea, 2007; Blumstein, 2003; Lejuez, Bornovalova, Reynolds, Daughters, & Curtin, 2007) among African American users compared to users of other ethnic/racial groups. For example, based on national statistics, non-Hispanic African Americans are nine times more likely to become cocaine dependent within 24 months of initiating cocaine use than non-Hispanic White recent-onset users (O’Brien & Anthony, 2005). Moreover, fatalities due to cocaine use also disproportionally affect African Americans compared to other racial/ethnic groups. Coffin and colleagues (2003) conducted a study among New York City hospitals, finding that fatal accidental drug overdoses were significantly higher among African Americans than Caucasians – with cocaine overdose being most common African American decedents, while alcohol and opiate overdose being most common among Latino and Caucasian decedents.
Further race differences have been noted in the literature based on cocaine type (powder cocaine versus crack cocaine). The use of “crack” – the street name given to freebase cocaine that is typically smoked, versus injected or snorted – is prevalent among all ethnic groups (Substance Abuse and Mental Health Services Administration [SAMHSA], 2009; SAMHSA, 2010), but has the highest documented prevalence among African Americans (SAMHSA, 2009), especially among those residing in low-income inner-city neighbourhoods (SAMHSA, 2010; Chen & Kandel, 2002). For example, Falck and colleagues (2007) documented that African Americans were less likely to stop smoking crack compared to Caucasian participants over the course of their 9-year study. Adverse health consequences of crack cocaine use, such as dependence rates, are also more prevalent among African Americans than other racial/ethnic groups (Chen & Kandel, 2002).
Among African American populations, gender differences in the prevalence and consequences of cocaine use have been observed, indicating greater use among males than females (11.1% versus 7.0%, respectively; U.S. Department of Health and Human Services, 2013). However, within inner city African American communities, converse finings have been observed, indicating that females are significantly more likely to use and/or be dependent upon cocaine compared to their male counterparts (Bornovalova, Lejuez, Daughters, Zachary Rosenthal, & Lynch, 2005; Lejuez, Bornovalova, & Daughters, 2005; Sterk, Theall, Elifson, & Kidder, 2003). For example, Lejuez and colleagues (2007) found that among individuals in an inner-city residential substance use treatment program, females reported higher cocaine use (current and lifetime heaviest) and were significantly more likely to report cocaine dependence than male participants.
Given the pronounced negative social and health consequences associated with cocaine use, models have been constructed to better understand underlying risk factors for cocaine dependence (e.g., Wagner & Anthony, 2002) and intensity of cocaine use (e.g., Buckner, Proctor, Reynolds, Kopetz, & Lejuez, 2011; Easton, Swan, & Sinha, 2000; Lejuez et al., 2007) – an important correlate of cocaine dependence (González-Sáiz, Domingo-Salvany, Barrio, Sánchez-Niubó, Brugal,de la Fuente, & Alonso, 2009; Moss, Chiung, & Hsiao-Ye, 2012; NIDA, 2010). However, to date, little is known about the mechanisms of risk for African Americans, which are at high-risk for cocaine use and adverse outcomes from its use. For the current study, we will examine three premorbid factors that have been linked to crack/cocaine use among the general population (i.e., frequency of baseline use, trauma history, and personality), and will consider the extent to which these variables present a unique risk for current use among a sample of African American users.
Risk Factors Related to Increased Crack/Cocaine Use
Frequency of Baseline Use
Duration and frequency of substance use have been consistently shown to increase risk for continued substance use, substance dependence and substance use problems (Arias et al., 2013; Chung, Kim, Hipwell, & Stepp, 2013; DeWit, Adlaf, Offord, & Ogborne, 2000; Dawson, Goldstein, Chou, Ruan, & Grant, 2008; Halley Grigsby, Forster, Soto, Baezconde-Garbanati, & Unger, 2014). This is also true for cocaine use: The more frequently one uses, the higher the risk for continued use at problematic levels (NIDA, 2010). Preclinical research has shown that higher doses of self-administered cocaine in laboratory rats increases their cocaine intake and leads to more regular patterns of use compared to rats with low-cocaine doses (Mantsch, Ho, Schlussman, & Kreek, 2001). Moreover, frequent doses of cocaine have been linked to a range of neuroadaptive responses associated with addiction (Koob et al., 2004; Unterwald, Kreek, & Cuntapay, 2001). In humans, frequency of cocaine use has been associated with risk of adverse psychological or physiological effects (NIDA, 2010), greater drug cravings (Fox, Talih, Malison, Anderson, Kreek, & Sinha, 2005), and greater difficulty maintaining abstinence (Ahmadi, Kampman, Oslin, Pettinati, Dackis, & Sparkman, 2009; Kiluk, Nich, Witkiewitz, Babuscio, & Carroll, 2014).
Childhood Trauma
A second risk factor for frequent cocaine use is childhood trauma. Studies have shown that even when abuse is disaggregated by type (i.e., childhood sexual, emotional, and physical abuse), the experience of abuse is a significant risk factor for subsequent negative outcomes, such as anxiety, depression, aggression, and substance dependence (Brems, Johnson, Neal, & Freemon, 2004; Duncan et al., 2008; Easton, Swan, & Sinha, 2000; Ompad et al., 2005; Roy, 2002). Pertaining to cocaine use, several studies have documented an association between history of abuse and cocaine use (Armour, Shorter, Elhai, Elklit, & Christoffersen, 2014; Banducci, Hoffman, Lejuez, & Koenen, 2014; Freeman, Collier & Parillo, 2002). When disaggregated based on type of childhood trauma, results have been mixed as to which type of trauma predicts cocaine use and/or dependence. For example, Hyman and colleagues (2006) found that only severity of emotional abuse – not sexual or physical abuse – was associated with severity of substance use among their sample of cocaine dependent adults. Few studies have examined the influence of childhood trauma on cocaine use, particularly among African American users. Lejuez and colleagues (2007) found among their sample of predominately African American users that although women reported higher rates of childhood abuse compared to male participants, childhood abuse was not associated with crack/cocaine (not disaggregated based on type of use) dependence or past year use.
Personality: Stress Reactivity
A third risk factor for frequent cocaine use relates to adaptation to stressful events. Numerous studies have documented the association between stress and drug use across development (Cardoso, Goldbach, Cervantes, & Swank, 2015; Cornelius, Kirisci, Reynolds, & Tarter, 2014; Enoch, 2011; Sinha, 2008). Studies specific to cocaine use have also documented this association, such that the experience of stress is positively associated with cocaine cravings (Duncan et al., 2007), cocaine use (Waldrop, Back, Brady, Upadhyaya, McRae, & Saladin, 2007) and duration of cocaine use (Karlsgodt, Lukas, & Elman, 2003). Moreover, individuals who rate high on personality traits associated with difficulty adapting to stress (i.e., stress reactivity) tend to also be at heightened risk for using substances in response to stressors (Elkins, King, McGue, & Iacono, 2006; Jackson & Sher, 2003; Krueger, 1999; Prisciandaro, Korte, McRae-Clark, & Brady, 2012. Stress reactivity has been shown to predict cocaine cravings and cocaine use in laboratory studies with rodents (Back et al. 2010; Sinha, Garcia, Paliwal, Kreek, & Rounsaville, 2006) and field studies with human participants (Fox et al., 2005; Lejuez et al., 2007; Sinha et al., 2003).
Taken together, the current study seeks to further clarify the relationship between three premorbid factors and current crack and cocaine use for African American users. In addition, given sex difference in the prevalence of use, we aim to delineate possible sex differences in the risk process of cocaine use among African Americans. Given that there has been limited work conducted within this specific population, we hypothesize – based on broader research findings – that each premorbid factor (i.e. baseline use, childhood trauma, and stress reactivity) and crack/cocaine use will be more prevalent for females compared to males. We hypothesize that when all premorbid variables are included in the same regression model, each will provide unique variance in the predictability of past year crack and cocaine use frequency; however, we have no ad hoc hypotheses regarding the moderating effect of sex on these relationships.
METHOD
Subjects and Procedures
Participants were recruited from a residential substance abuse treatment facility in Washington D.C. (N = 508, mean age = 43.3, S.D. = 9.8; 70.1% male; 88.4% African American). For the current study, analyses were conducted among the portion of individuals who identified themselves as African American and reported using crack or cocaine in the past year (N = 270, mean age = 44, S.D. = 9.7; 73% male [n = 198]). IRB-approved consent forms were obtained for each participant, after which participants completed the substance dependence module of the Structured Clinical Interview for DSM-IV, Axis I (SCID; First, Spitzer, Gibbon & Williams, 1996). Following the interview, participants completed a self-report questionnaire packet including the measures described below. All assessment procedures were completed within four to seven days of entering the treatment facility (the four-day waiting period was intended to minimize potential interference from withdrawal symptoms in participants) and were completed with doctoral-level graduate students and senior-level research staff. Participants were paid $25 in the form of a grocery store gift card upon discharge from treatment.
Measures
Demographics Questionnaire
A short self-report questionnaire was administered to obtain information on age, sex, race, marital status, education level, and income.
Drug Use Diagnostic Identification Test (DUDIT; Babor & Del Boca, 2003)
The DUDIT was used as a quantity/frequency measure of drug and alcohol use (Babor & Del Boca, 2003). Frequencies of crack and cocaine use during the first year and in the past year were assessed by a one-item measure using the following Likert scale: never (0), one time (1), monthly or less (2), 2–4 times a month (3), 2–3 times per week (4), 4 or more times a week (5).
Multidimensional Personality Questionnaire-Brief Form (MPQ-BF; Patrick, Curtin, & Tellegen, 2002)
The MPQ is a 155-item version of the original 300-item MPQ, developed to assess a variety of personality traits and temperamental dispositions. Like the original MPQ, the brief form of the MPQ includes 11 primary trait scales, which load onto three higher-order factors. The traits of Well-Being, Achievement, Social Closeness, and Social Potency load onto the higher-order factor of Positive Emotionality; the traits of Stress Reactivity, Alienation, and Aggression make up the higher-order factor of Negative Emotionality; the traits of Control, Harm Avoidance, and Traditionalism load on the higher-order factor of Constraint; and the trait of Absorption does not load on any of the higher-order factors. Scores from the traits scales of the MPQ-BF are highly correlated with the equivalent trait scales from the original MPQ (r’s ranged from .92 to .96) and have demonstrated high internal consistency (Cronbach’s alphas range from .74 to .84). In the current study, only the Negative Emotionality traits were used.
The Childhood Trauma Questionnaire-Short Form (CTQ-SF; Bernstein, Stein, Newcomb, Walker, Pogge & Ahluvalia, 2003)
The CTQ-SF is a self-report questionnaire, comprised of three subscales that assess childhood trauma. Each subscale has 5 items utilizing a 5-point scale ranging from 1 (never true) to 5 (very often true). Each subscale has been shown to be internally consistent (α’s: emotional abuse = .89, physical abuse = .86, sexual abuse = .95) (Bernstein et al., 2003).
Statistical Analyses
All analyses were done using SPSS 20.0 as well as SPSS macros for testing moderation. In order to examine the unique predictability of each risk factor on past year frequency of cocaine use among our sample of African American users, we first conducted bivariate correlations between the predictor variables (i.e., frequency of first year use, childhood trauma, personality) and outcome variables (i.e., frequency of crack and cocaine use in the past 12 months). Second, we conducted independent sample t-tests to determine if sex differences were observed among the three risk factors and outcome variables. Third, we used a series of multiple linear regression analyses to test the unique effect of each risk factor on past year crack and cocaine frequencies and observe any sex differences. Analyses were run separately for crack and cocaine due to differences in the prevalence of each by sex and negative outcomes associated with use. Specifically, we conducted a multiple regression in which sex was entered at step one (female = 0, male = 1). The specified risk factors, first year use, childhood trauma subscales and stress reactivity, were entered at step two. An interaction term between any significant risk factor and sex was entered at step three. The MODPROBE macro (Hayes & Matthes, 2009) was used to probe the interaction (as suggested by Aiken & West, 1991). The macro uses the Johnson-Neyman technique (see e.g., Bauer & Curran, 2005; Hayes & Matthes, 2009), which determines at what value(s) of the moderator the effect of the independent variable on the dependent variable becomes non-significant (Hayes, 2012).
RESULTS
First descriptive statistics and associations between study variables were assessed. Among the subsample of African Americans cocaine users, there were no significant sex differences based on age, marital status, or education level. However, females reported lower yearly income than males (t (261) = 2.37, p < .05). Specifically, 53% of males reported earning less than $10,000/year compared to 64% of females. Descriptive statistics of the study variables disaggregated based on sex are presented in Table 1. Partial support for our first hypothesis was found, with female participants reporting higher scores on past year crack/cocaine use, childhood emotional and sexual abuse, and stress reactivity compared to males. Bivariate associations between cocaine use and all predictor variables (i.e., sex, first year use, childhood trauma, and trait stress reactivity) are presented in Table 2.
Table 1.
Means, standard deviations, and p values for predictor variables and cocaine use at baseline and during past year of use for females and males.
| Female (M/SD) | Male (M/SD) | |
|---|---|---|
| Predictor Variables | ||
| Cocaine Use (First Year) | 3.4 (1.8) | 3.0 (1.8) |
| Crack Use (First Year) | 3.4 (1.9) | 3.2 (1.8) |
| Child Emotional Abuse | 10.8 (6.07) | 9.1(5.1)* |
| Child Physical Abuse | 8.7 (5.3) | 8.9 (4.8) |
| Child Sexual Abuse | 9.1 (5.9) | 7.0 (4.9)** |
| Stress Reactivity | 8.0 (4.5) | 6.6 (4.3)* |
| Outcome Variables | ||
| Cocaine Use (Past Year) | 3.9 (1.7) | 3.1 (2.1)** |
| Crack Use (Past Year) | 4.2 (1.7) | 3.3 (2.1)** |
Note: cocaine: N = 270; crack cocaine: N = 85.
p < .05;
p < .01
Table 2.
Bivariate correlations of study variables.
| Sex | CO1 | CO2 | CR1 | CR2 | EA | PA | SA | SR | |
|---|---|---|---|---|---|---|---|---|---|
| Sex | −.11 | −.18** | −.05 | −.20 | −.13* | .02 | −.17** | −.14* | |
| CO1 | .67** | .93** | .67** | .23** | .11 | .09 | .08 | ||
| CO2 | .75** | .98** | .15* | .06 | .14* | .19** | |||
| CR1 | .77** | .22* | .20 | .17 | .23* | ||||
| CR2 | .16 | .08 | .23* | .31* | |||||
| EA | .69** | .52** | .38** | ||||||
| PA | .44** | .25** | |||||||
| SA | .26** | ||||||||
| SR |
Note: N = 270. Sex: female=0, male=1; CO1: frequency of cocaine use during the first year of use; CO2: frequency of cocaine use during the past 12 months; CR1: frequency of crack use during the first year of use; CR2: frequency of crack use during the past 12 months; EA: childhood emotional abuse; PA: childhood physical abuse; SA: childhood sexual abuse; SR: level of trait stress reactivity.
p < .05;
p < .01
Regression Model for Cocaine Use
In the regression analysis for cocaine use, as hypothesized, sex positively predicted past year cocaine use (β = −.19, p < .01). Moreover, consistent with our hypothesis, frequency of cocaine use at year one (β = .66, p < .001), history of sexual abuse (β = .11, p < .05) and high levels of trait stress reactivity (β = .15, p < .01) predicted cocaine use above and beyond the other predictor variables, explaining 45% of the variance for past year use. However, neither history of physical abuse nor emotional abuse was a significant predictor in the risk model. To further examine sex differences in risk, interaction terms were constructed between sex and frequency of baseline cocaine use, sexual abuse history, and stress reactivity, each of which was entered in step three of the regression analysis. However, no significant sex differences were observed (see Table 3).
Table 3.
Multiple linear regression analysis in predicting past year cocaine use frequency from baseline levels of cocaine use, childhood abuse history, and trait stress reactivity by sex.
| Variable | B | SE B | β | R2 |
|---|---|---|---|---|
| Step One | ||||
| Sex | −.90 | .29 | −.19** | |
| .04* | ||||
| Step Two | ||||
| Year 1 Cocaine Use | .76 | .05 | .66*** | |
| Emotional Abuse | −.04 | .03 | −.10 | |
| Physical Abuse | −.03 | .03 | −.07 | |
| Sexual Abuse | .04 | .02 | .11* | |
| Trait Stress Reactivity | .07 | .02 | .15** | |
| .49*** | ||||
| Step Three | ||||
| Stress Reactivity × Sex | .06 | .05 | .10 | |
| .49 |
Note: N = 270.
Abbreviations: B = unstandardized regression coefficient; SE = standard error; β = standardized regression coefficient; R2 = explained variance.
p < .05;
p < .01;
p < .001
Regression Model for Crack Cocaine Use
In the regression analysis for crack cocaine use, as hypothesized, sex positively predicted past year crack cocaine use (β = −.22, p < .05). Also as hypothesized, frequency of crack cocaine use at year one predicted crack cocaine use above and beyond the other predictor variables (β = .76, p < .001), explaining 62% of the variance for past year use. There was also a trend towards significance for history of sexual abuse (β = .15, p = .05) and high levels of trait stress reactivity (β = .14, p = .06) in predicting past year crack cocaine use. Sex differences were investigated for first year use, with findings showing a significant interaction between sex and first year frequency, such that the relationship between levels of first year use and past year frequency was stronger for males than for females (see Table 4 and Figure 1).
Table 4.
Multiple linear regression analysis in predicting past year crack cocaine use frequency from baseline levels of crack cocaine use, childhood abuse history, and trait stress reactivity by sex.
| Variable | B | SE B | β | R2 |
|---|---|---|---|---|
| Step One | ||||
| Sex | −.99 | .49 | −.22 * | |
| .05* | ||||
| Step Two | ||||
| Year 1 Crack Use | .83 | .08 | .76*** | |
| Emotional Abuse | −.02 | .03 | −.05 | |
| Physical Abuse | −.06 | .03 | −.18 | |
| Sexual Abuse | .06 | .03 | .15† | |
| Trait Stress Reactivity | .07 | .04 | .14† | |
| .67*** | ||||
| Step Three | ||||
| Year 1 Crack Use × Sex | .36 | .18 | .28* | |
| .69* |
Note: N = 85.
Abbreviations: B = unstandardized regression coefficient; SE = standard error; β = standardized regression coefficient; R2 = explained variance.
<.10;
p < .05;
p < .01;
p < .001
Figure 1.
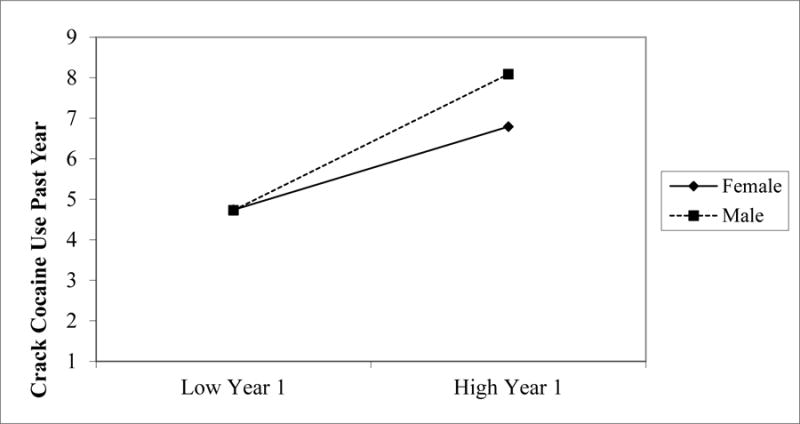
The moderating effect of sex on the predictive relationship between baseline crack cocaine use frequency and past year crack cocaine use frequency.
DISCUSSION
The adverse health consequences of frequent crack and cocaine use have been well documented (Carey, 2006; Muniz et al., 2001; NIDA, 2010; Palha et al., 2008; Pozner et al., 2005; Riezzo et al., 2012; Treadwell et al., 2007; Valente et al., 2012). Moreover, the increased use of cocaine among the African American community, especially African American women, is of great concern. Though risk factors related to cocaine use are known more broadly (e.g., Ball et al., 1995), far less is understood about risk factors specific to African American crack and cocaine users, much less as a function of sex (e.g., Lejuez et al., 2007). The aims of the current study were to examine the relationship between three well-documented risk factors – frequency of use, childhood trauma, and trait stress reactivity – on past year cocaine and crack use among African Americans users and to test whether the relationships varied as a function of sex.
First, we were able to find partial support for the predictive validity of the three risk factors on cocaine and crack cocaine use. Frequency of first year use and stress reactivity were found to be significant predictors of past year cocaine use. Pertaining to childhood trauma, only childhood sexual abuse was found to be a significant predictor in the regression model. Similar results were found in predicting past year crack cocaine use. Although frequency of first year use was the only statistically significant predictor in the regression analysis, both childhood sexual abuse and stress reactivity trended towards statistical significance.
Our findings provide important information on the need to assess childhood maltreatment by type of trauma rather than using an aggregated childhood trauma risk factor. Among our sample of low-income African American users, childhood sexual abuse appeared to be the most important childhood trauma factor when assessing risk for crack/cocaine use. However, different trauma factors may be important to consider when assessing risk for other substance use outcomes (Hyman, Garcia, & Sinha, 2006).
Our findings also highlighted interesting sex differences in the prevalence of and risk for recent cocaine and crack cocaine use. Consistent with previous literature, African American women reported more frequent past year crack and cocaine use, although baseline levels of crack and cocaine use were similar across groups. Women also reported significantly higher rates of childhood sexual abuse, emotional abuse, and stress reactivity. Despite women experienced greater exposure to risk for cocaine use, there were no sex differences in predicting past year cocaine use based on the risk factors observed. However, a significant sex difference was found in crack cocaine use, such that the relationship between frequency of use during the first year and past year was stronger for males than for females.
These findings suggest that treatment interventions for African American crack and cocaine users should focus on incorporating distress tolerance skills and more adaptive stress management skills, while also considering the possible influence of childhood trauma. One such mode of treatment might be Cocaine-Specific Coping Skills Training (CST), an evidence-based intervention that targets emotions – such as frustration and anger – and social and internal pressures to use, while also teaching coping skills and cognitive restructuring to avoid trigger situations and prevent relapse (Rohsenow, Monti, Martin, Michalec, & Abrams, 2000). More generally, Dialectical Behavioral Therapy (DBT) has been demonstrated as an efficacious treatment for individuals with substance use disorders and co-occurring sexual abuse histories (Dimeff & Linehan, 2008). For, African American males in particular, preventative interventions that focus on delaying onset and frequency of use appear to be most appropriate. Early preventative EBIs such as SAFEChildren – an evidence-based preventative intervention focused on decreasing the risk of later drug use, academic problems, and low social competence in inner-city 1st-grade children and their families – has demonstrated efficacy in reducing child problems that typically precede substance use (Tolan, Gorman-Smith, & Henry, 2004).
This paper has some limitations that must be acknowledged when interpreting the results. First, although obtaining a sample of 270 African American treatment seeking cocaine users is noteworthy, increasing the sample size may have allowed for more power to observe sex differences given that 70% of the sample was male. Additionally, only a subset of cocaine users also used crack cocaine (N=85), thus a larger sample would allow for more power in observing potential sex differences. However, even with the current sample, significant results were observed and important implications can be drawn from this study on risk for cocaine use, specifically for African Americans. Second, the childhood trauma data, as well as early drug use, were collected retrospectively. As mentioned by Lejuez and colleagues (2007), this method of measurement may limit the accuracy of reporting, given the chronic pharmacological effects (e.g., brain damage) of drug use. Additionally, childhood abuse data were collected without reference to a specific time period of abuse, which may be an important factor to consider. More frequent data collection, which tracks frequency of crack/cocaine use on an annual bases beginning close to initiation through present day use, would provide a fuller/more accurate understanding of the patterns of cocaine use. It is possible that the intensity of use is exponential for some, yet curvilinear for others. Finally, we did not include information regarding other well-documented risk factors for substance use, which may also be important risk factors for frequent cocaine use. Such risk factors include family history of substance dependence, poly drug use, impulsivity traits, family or peer use of drugs, childhood disorders, other psychiatric problems, and cultural factors, such as racial discrimination.
Despite these limitations, the current study provides a clearer understanding of risk for crack and cocaine use among lower income African Americans, which is vital due to the high prevalence of use and problems among this population. Given that participants recruited for this study were entering a residential treatment facility for substance abuse, these findings can be informative in intervention programming for cocaine-dependent adults. They can also inform prevention programming aimed at reducing racial disparities in crack/cocaine use and addiction.
Footnotes
Declaration of Interest
The authors report no declaration of interest.
Contributor Information
Tamika C. B. Zapolski, Indiana University Purdue University at Indianapolis
Patrick D. Baldwin, Indiana University Purdue University at Indianapolis
Carl W. Lejuez, University of Maryland
References
- Ahmadi J, Kampman KM, Oslin DM, Pettinati HM, Dackis C, Sparkman T. Predictors of treatment outcome in outpatient cocaine and alcohol dependence treatment. The American Journal On Addictions. 2009;18(1):81–86. doi: 10.1080/10550490802545174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications, Inc; 1991. [Google Scholar]
- Arias F, Szerman N, Vega P, Mesias B, Basurte I, Morant C, Babin F. Cocaine abuse or dependency and other pyschiatric disorders. Madrid study on dual pathology. Revista de Psiquiatría y Salud Mental (English Edition) 2013;6(3):121–128. doi: 10.1016/j.rpsm.2012.09.002. [DOI] [PubMed] [Google Scholar]
- Armour C, Shorter GW, Elhai JD, Elklit A, Christoffersen MN. Polydrug use typologies and childhood maltreatment in a nationally representative survey of Danish young adults. Journal of Studies on Alcohol and Drugs. 2014;75(1):170–178. doi: 10.15288/jsad.2014.75.170. doi: http://dx.doi.org/10.15288/jsad.2014.75.170. [DOI] [PubMed] [Google Scholar]
- Babor TF, Del Boca FK. Treatment matching in alcoholism. Cambridge University Press; 2003. [Google Scholar]
- Back SE, Hartwell K, DeSantis SM, Saladin M, McRae-Clark AL, Price KL, Brady KT. Reactivity to laboratory stress provocation predicts relapse to cocaine. Drug and Alcohol Dependence. 2010;106(1):21–27. doi: 10.1016/j.drugalcdep.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Carroll KM, Babor TF, Rounsaville BJ. Subtypes of cocaine abusers: support for a type A-type B distinction. Journal of Consulting and Clinical Psychology. 1995;63(1):115–124. doi: 10.1037//0022-006x.63.1.115. [DOI] [PubMed] [Google Scholar]
- Banducci AN, Hoffman E, Lejuez CW, Koenen KC. The relationship between child abuse and negative outcomes among substance users: psychopathology, health, and comorbidities. Addictive Behaviors. 2014;39(10):1522–1527. doi: 10.1016/j.addbeh.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Bernstein KT, Bucciarelli A, Piper TM, Gross C, Tardiff K, Galea S. Cocaine-and opiate-related fatal overdose in New York City, 1990–2000. BMC Public Health. 2007;7(1):31. doi: 10.1186/1471-2458-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Blumstein A. The notorious 100: 1 Crack: Powder disparity-The data tell us that it is time to restore the balance. Federal Sentencing Reporter. 2003;16:87–92. [Google Scholar]
- Bornovalova MA, Lejuez CW, Daughters SB, Zachary Rosenthal M, Lynch TR. Impulsivity as a common process across borderline personality and substance use disorders. Clinical Psychology Review. 2005;25(6):790–812. doi: 10.1016/j.cpr.2005.05.005. [DOI] [PubMed] [Google Scholar]
- Brems C, Johnson ME, Neal D, Freemon M. Childhood abuse history and substance use among men and women receiving detoxification services. The American Journal of Drug and Alcohol Abuse. 2004;30(4):799–821. doi: 10.1081/ada-200037546. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Proctor SL, Reynolds E, Kopetz C, Lejuez CW. Cocaine dependence and anxiety sensitivity among patients presenting for residential drug use treatment. Journal of Cognitive Psychotherapy. 2011;25(1):22–30. doi: http://dx.doi.org/10.1891/0889-8391.25.1.22. [Google Scholar]
- Cardoso JB, Goldbach JT, Cervantes RC, Swank P. Stress and multiple substance use behaviors among hispanic adolescents. Prevention Science. 2015 doi: 10.1007/s11121-015-0603-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey JC. Pharmacological effects on sexual function. Obstetrics and Gynecology Clinics of North America. 2006;33(4):599–620. doi: 10.1016/j.ogc.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Chen K, Kandel D. Relationship between extent of cocaine use and dependence among adolescents and adults in the United States. Drug and Alcohol Dependence. 2002;68(1):65–85. doi: 10.1016/s0376-8716(02)00086-8. [DOI] [PubMed] [Google Scholar]
- Chung T, Kim KH, Hipwell AE, Stepp SD. White and black adolescent females differ in profiles and longitudinal patterns of alcohol, cigarette, and marijuana use. Psychology of Addictive Behaviors. 2013;27(4):1110–1121. doi: 10.1037/a0031173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990–98. Addiction. 2003;98(6):739–747. doi: 10.1046/j.1360-0443.2003.00376.x. [DOI] [PubMed] [Google Scholar]
- Compton WM, Cottler LB, Ben Abdallah A, Phelps DL, Spitznagel EL, Horton JC. Substance dependence and other psychiatric disorders among drug dependent subjects: race and gender correlates. The American Journal on Addictions. 2000;9(2):113–125. doi: 10.1080/10550490050173181. [DOI] [PubMed] [Google Scholar]
- Cornelius J, Kirisci L, Reynolds M, Tarter R. Does stress mediate the development of substance use disorders among youth transitioning to young adulthood? The American Journal of Drug and Alcohol Abuse. 2014;40(3):225–229. doi: 10.3109/00952990.2014.895833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Patricia Chou S, June Ruan W, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcoholism: Clinical and Experimental Research. 2008;32(12):2149–2160. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. Am J Psychiatry. 2000;157(5):745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Linehan MM. Dialectical behavior therapy for substance abusers. Addiction Science and Clinical Practice. 2008;4(2):39–47. doi: 10.1151/ascp084239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan E, Boshoven W, Harenski K, Fiallos A, Tracy H, Jovanovic T, Kilts C. An fMRI study of the interaction of stress and cocaine cues on cocaine craving in cocaine-dependent men. The American Journal On Addictions. 2007;16(3):174–182. doi: 10.1080/10550490701375285. [DOI] [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Scherrer JF, Grant JD, Heath AC, Nelson EC, Bucholz KK. The association between cannabis abuse and dependence and childhood physical and sexual abuse: evidence from an offspring of twins design. Addiction. 2008;103(6):990–997. doi: 10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easton CJ, Swan S, Sinha R. Prevalence of family violence in clients entering substance abuse treatment. Journal of Substance Abuse Treatment. 2000;18(1):23–28. doi: 10.1016/s0740-5472(99)00019-7. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: prospective links from adolescence to young adulthood. Journal of Abnormal Psychology. 2006;115(1):26. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology. 2011;214(1):17–31. doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falck RS, Wang J, Carlson RG. Crack cocaine trajectories among users in a midwestern American city. Addiction. 2007;102(9):1421–1431. doi: 10.1111/j.1360-0443.2007.01915.x. [DOI] [PubMed] [Google Scholar]
- First Michael B, Spitzer Robert L, Gibbon Miriam, Williams Janet BW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) Washington, DC: American Psychiatric Press, Inc; 1996. [Google Scholar]
- Freeman RC, Collier K, Parillo KM. Early life sexual abuse as a risk factor for crack cocaine use in a sample of community-recruited women at high risk for illicit drug use. The American Journal of Drug and Alcohol Abuse. 2002;28(1):109–131. doi: 10.1081/ada-120001284. [DOI] [PubMed] [Google Scholar]
- Fox HC, Talih M, Malison R, Anderson G, Kreek M, Sinha R. Frequency of recent cocaine and alcohol use affects drug craving and associated responses to stress and drug-related cues. Psychoneuroendocrinology. 2005;30:880–891. doi: 10.1016/j.psyneuen.2005.05.002. [DOI] [PubMed] [Google Scholar]
- González-Sáiz F, Domingo-Salvany A, Barrio G, Sánchez-Niubó A, Brugal MT, de la Fuente L, Alonso J. Severity of Dependence Scale as a diagnostic tool for heroin and cocaine dependence. European Addiction Research. 2009;15(2):87–93. doi: 10.1159/000189787. [DOI] [PubMed] [Google Scholar]
- Halley Grigsby TJ, Forster M, Soto DW, Baezconde-Garbanati L, Unger JB. Problematic Substance Use Among Hispanic Adolescents and Young Adults: Implications for Prevention Efforts. Substance Use & Misuse. 2014;49(8):1025–1038. doi: 10.3109/10826084.2013.852585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Sinha R. Gender specific associations between types of childhood maltreatment and the onset, escalation and severity of substance use in cocaine dependent adults. The American Journal of Drug and Alcohol Abuse. 2006;32(4):655–664. doi: 10.1080/10623320600919193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ. Alcohol use disorders and psychological distress: a prospective state-trait analysis. Journal of Abnormal Psychology. 2003;112(4):599–613. doi: 10.1037/0021-843X.112.4.599. [DOI] [PubMed] [Google Scholar]
- Karlsgodt KH, Lukas SE, Elman I. Psychosocial Stress and the Duration of Cocaine Use in Non-treatment Seeking Individuals with Cocaine Dependence. The American Journal of Drug And Alcohol Abuse. 2003;29(3):539–551. doi: 10.1081/ADA-120023457. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Nich C, Witkiewitz K, Babuscio TA, Carroll KM. What happens in treatment doesn’t stay in treatment: Cocaine abstinence during treatment is associated with fewer problems at follow-up. Journal of Consulting And Clinical Psychology. 2014;82(4):619–627. doi: 10.1037/a0036245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Ahmed SH, Boutrel B, Chen SA, Kenny PJ, Markou A, Sanna PP. Neurobiological mechanisms in the transition from drug use to drug dependence. Neuroscience & Biobehavioral Reviews. 2004;27(8):739–749. doi: 10.1016/j.neubiorev.2003.11.007. [DOI] [PubMed] [Google Scholar]
- Krueger RF. Personality traits in late adolescence predict mental disorders in early adulthood: a prospective-epidemiological study. Journal of Personality. 1999;67(1):39–65. doi: 10.1111/1467-6494.00047. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Reynolds EK, Daughters SB, Curtin JJ. Risk factors in the relationship between gender and crack/cocaine. Experimental and Clinical Psychopharmacology. 2007;15(2):165–175. doi: 10.1037/1064-1297.15.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Daughters SB, Curtin JJ. Differences in impulsivity and sexual risk behavior among inner-city crack/cocaine users and heroin users. Drug and Alcohol Dependence. 2005;77(2):169–175. doi: 10.1016/j.drugalcdep.2004.08.013. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive S. A comparative analysis of perceived risks and substance abuse among ethnic groups. Addictive Behaviors. 2000;25(3):361–371. doi: 10.1016/S0306-4603(99)00070-2. [DOI] [PubMed] [Google Scholar]
- Mantsch JR, Ho A, Schlussman SD, Kreek M. Predictable individual differences in the initiation of cocaine self-administration by rats under extended-access conditions are dose-dependent. Psychopharmacology. 2001;157(1):31–39. doi: 10.1007/s002130100744. [DOI] [PubMed] [Google Scholar]
- Moss HB, Chen CM, Yi H. Measures of substance consumption among substance users, DSM-IV abusers, and those with DSM-IV dependence disorders in a nationally representative sample. Journal of Studies on Alcohol and Drugs. 2012;73(5):820–828. doi: 10.15288/jsad.2012.73.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muniz AE, Evans T. Acute gastrointestinal manifestations associated with use of crack. The American Journal of Emergency Medicine. 2001;19(1):61–63. doi: 10.1053/ajem.2001.20010. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA) Cocaine: Abuse and addiction. Research Report Series. 2010;10-4166:1–8. [Google Scholar]
- O’Brien MS, Anthony JC. Risk of becoming cocaine dependent: epidemiological estimates for the United States, 2000–2001. Neuropsychopharmacology. 2005;30(5):1006–1018. doi: 10.1038/sj.npp.1300681. [DOI] [PubMed] [Google Scholar]
- Ompad DC, Ikeda RM, Shah N, Fuller CM, Bailey S, Morse E, Strathdee SA. Childhood sexual abuse and age at initiation of injection drug use. American Journal of Public Health. 2005;95(4):703–709. doi: 10.2105/AJPH.2003.019372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palha AP, Esteves M. Drugs of abuse and sexual functioning. Advances in Psychosomatic Medicine. 2008;29:131–149. doi: 10.1159/000126628. [DOI] [PubMed] [Google Scholar]
- Palamar JJ, Davies S, Ompad DC, Cleland CM, Weitzman M. Powder cocaine and crack use in the United States: An examination of risk for arrest and socioeconomic disparities in use. Drug and Alcohol Dependence. 2015;149:108–116. doi: 10.1016/j.drugalcdep.2015.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychoogical Assessessment. 2002;14(2):150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Pozner CN, Levine M, Zane R. The cardiovascular effects of cocaine. Journal of Emergency Medicine. 2005;29(2):173–178. doi: 10.1016/j.jemermed.2005.01.019. [DOI] [PubMed] [Google Scholar]
- Prisciandaro JJ, Korte JE, McRae-Clark AL, Brady KT. Associations between behavioral disinhibition and cocaine use history in individuals with cocaine dependence. Addictive Behaviors. 2012;37(10):1185–1188. doi: 10.1016/j.addbeh.2012.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riezzo I, Fiore C, De Carlo D, Pascale N, Neri M, Turillazzi E, Fineschi V. Side effects of cocaine abuse: multiorgan toxicity and pathological consequences. Current Medicinal Chemistry. 2012;19(33):5624–5646. doi: 10.2174/092986712803988893. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. Journal of Consulting and Clinical Psychology. 2000;68(3):515–520. doi: 10.1037//0022-006x.68.3.515. [DOI] [PubMed] [Google Scholar]
- Roy A. Self-rated childhood emotional neglect and CSF monoamine indices in abstinent cocaine-abusing adults: possible implications for suicidal behavior. Psychiatry Research. 2002;112(1):69–75. doi: 10.1016/s0165-1781(02)00176-2. [DOI] [PubMed] [Google Scholar]
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Annals of the New York Academy of Sciences. 2008;1141(1):105–130. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Archives of General Psychiatry. 2006;63(3):324–331. doi: 10.1001/archpsyc.63.3.324. [DOI] [PubMed] [Google Scholar]
- Sinha R, Talih M, Malison R, Cooney N, Anderson GM, Kreek MJ. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berl) 2003;170(1):62–72. doi: 10.1007/s00213-003-1525-8. [DOI] [PubMed] [Google Scholar]
- Sterk CE, Theall KP, Elifson KW, Kidder D. HIV risk reduction among African-American women who inject drugs: a randomized controlled trial. AIDS and Behavior. 2003;7(1):73–86. doi: 10.1023/a:1022565524508. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration[SAMHSA] Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. (NSDUH Series H-41, HHS Publication No. (SMA) 11-4658). [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS) 1999 – 2009. 2009 Retrieved from www.samhsa.gov.
- Tolan P, Gorman-Smith D, Henry D. Supporting families in a high-risk setting: proximal effects of the SAFEChildren preventive intervention. Ournal of Consulting and Clinical Psychology. 2004;72(5):855–869. doi: 10.1037/0022-006x.72.5.855. [DOI] [PubMed] [Google Scholar]
- Treadwell SD, Robinson TG. Cocaine use and stroke. Postgradruate Medicine Journal. 2007;83(980):389–394. doi: 10.1136/pgmj.2006.055970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. National Survey on Drug Use and Health, 2013. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2014-11-18; 2013. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. ICPSR35509-v1. http://doi.org/10.3886/ICPSR35509.v1. [Google Scholar]
- Unterwald EM, Kreek MJ, Cuntapay M. The frequency of cocaine administration impacts cocaine-induced receptor alterations. Brain research. 2001;900(1):103–109. doi: 10.1016/S0006-8993(01)02269-7. [DOI] [PubMed] [Google Scholar]
- Valente MJ, Carvalho F, Bastos M, de Pinho PG, Carvalho M. Contribution of oxidative metabolism to cocaine-induced liver and kidney damage. Current Medicinal Chemistry. 2012;19(33):5601–5606. doi: 10.2174/092986712803988938. [DOI] [PubMed] [Google Scholar]
- Wagner FA, Anthony JC. From first drug use to drug dependence: developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26:479–488. doi: 10.1038/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]
- Waldrop AE, Back SE, Brady KT, Upadhyaya HP, McRae AL, Saladin ME. Daily stressor sensitivity, abuse effects, and cocaine use in cocaine dependence. Addictive Behaviors. 2007;32(12):3015–3025. doi: 10.1016/j.addbeh.2007.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


