Abstract
Purpose: To determine whether the handheld dynamometer (HHD) is an appropriate tool to assess and quantify peak hip extension strength in prone standing position by (1) evaluating the concurrent validity of the HHD versus an isokinetic dynamometer (IKD), (2) establishing the minimal detectable change (MDC), and (3) determining the validity of single-trial versus multi-trial measures. Method: A convenience sample of 20 healthy adults was recruited for this cross-sectional study. Measures of peak hip extension strength were collected in prone standing position with both the HHD and the IKD and in supine position with the IKD. Results: Values of r were 0.37 for HHD versus IKD prone standing and 0.51 for HHD versus IKD supine. MDC was 14.8 Nm for the HHD, 25.6 Nm for IKD prone standing, and 41.5 Nm for IKD supine. High correlations (r values of 0.92–0.94) were observed between trial 1 and the mean of three trials. Conclusions: The HHD has moderate concurrent validity in measuring peak hip extension strength in the prone standing position in healthy adults. MDC for hip extension strength was lowest using the HHD. Single-trial values showed a high correlation with three-trial mean values.
Key Words: hip, isometric contraction, muscle strength dynamometer, reproducibility of results
Abstract
Déterminer si le dynamomètre manuel (DM) est un outil approprié pour évaluer et quantifier la force d'extension de la hanche maximale en position « pronation debout » en (1) évaluant simultanément la validité du DM par rapport à celle d'un dynamomètre isocinétique (DI), (2) établissant le changement détectable minimal (CDM) et (3) déterminant la validité des mesures découlant d'un essai simple par rapport à des mesures découlant d'essais multiples. Méthode : On a recruté un échantillon de commodité de 20 adultes en bonne santé pour cette étude transversale. On a colligé des mesures de la force d'extension de la hanche maximale en position pronation debout au moyen à la fois du DM et du DI, ainsi qu'en position supination sur le DI. Résultats : Les valeurs r se sont établies à 0,37 dans le cas du DM par rapport au dynamomètre isocinétique en position pronation debout, et à 0,51 dans le cas du DM par rapport au DI en position supination. Le CDM s'est établi à 14,8 Nm pour le DM, à 25,6 Nm pour le DI en pronation debout, et à 41,5 Nm pour le DI en supination. On a observé des liens serrés (r=0,92–0,94) entre l'essai 1 et la moyenne des trois essais. Conclusions : Les DM offrent une validité simultanée modérée lorsqu'il s'agit de mesurer la force d'extension de la hanche maximale en position pronation debout chez les adultes en santé. Le CDM dans le cas de la force d'extension de la hanche est le plus faible lorsqu'on utilise le DM. Les valeurs découlant d'un essai simple montrent qu'il existe un lien important avec les valeurs moyennes de trois essais.
Mots clés : contraction isométrique, dynamomètre de calcul de la force musculaire, hanche, validité
Assessing muscle strength in people with musculoskeletal pathologies as part of physiotherapy assessment allows clinicians to identify muscle weaknesses and provides a baseline to create a treatment plan and assess treatment efficacy via subsequent strength testing.1–5 Hip extension strength is an important measurement in orthopaedic pathologies because it plays a key role in functional mobility such as ambulation and negotiating stairs.6–8 Research has suggested that weak hip extensors are linked to several orthopaedic pathologies, including low back pain9,10 and hip osteoarthritis.11–13 A valid and objective measure to quantify hip extension strength is needed to explore these relationships.
Manual muscle testing (MMT) is commonly used to assess muscle strength, but it is a subjective measure.4 A handheld dynamometer (HHD) gives a more objective measure than MMT and is more portable and affordable than an isokinetic dynamometer (IKD), which is considered the gold standard for muscle strength measurements.3,14,15 Furthermore, clinicians tend to assess muscle strength using a single trial.17,18 It is therefore important to determine whether single-trial measures are correlated with multitrial mean measures to reflect typical use of this device in a clinical setting.
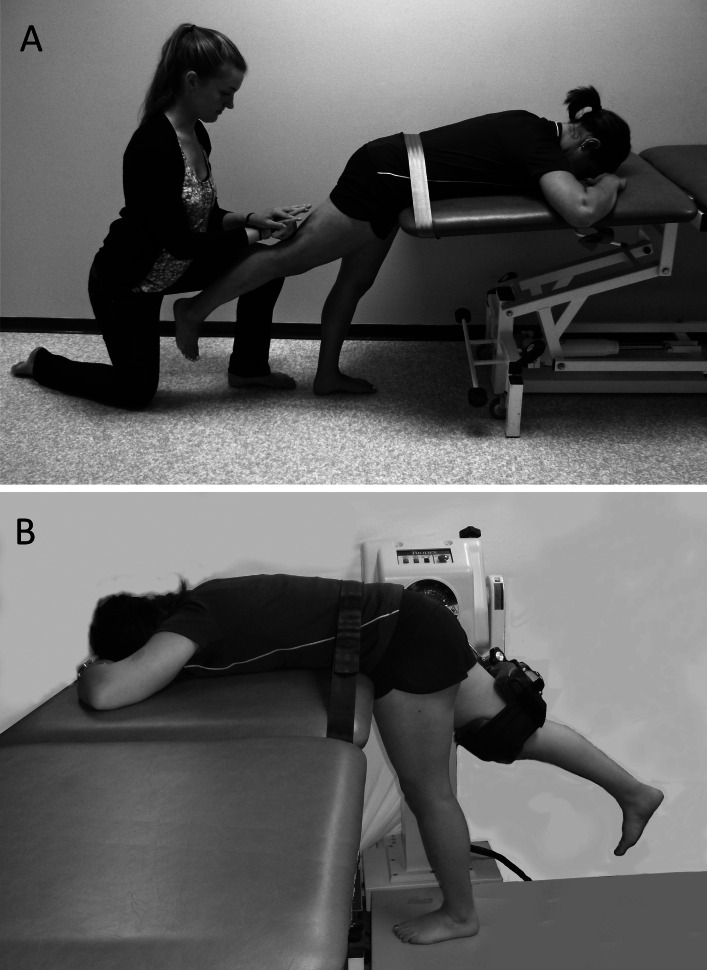
The intertester, intratester, and intrasession reliability of hip extension measurement using an HHD has been well documented in healthy participants in the prone position (intertester intra-class correlation [ICC]=0.65–0.93; intratester ICC=0.77–0.96)4,19,20 and in the standing position (intertester ICC=0.82–0.84; intratester ICC=0.91–0.94).21 Higher intertester (ICC=0.92) and intrasession (ICC=0.94–0.99) reliability values have been reported using a prone standing position6,22 in which the participant is standing but the upper body is supported on a plinth (Figure 1). Studies have suggested that the prone position does not allow as great a muscle contraction as the prone standing position.6,22 In the prone standing position, the hip is flexed and hip extensor muscle fibres and lever arm are lengthened, allowing a favourable length–tension relationship and thus optimizing hip extension torque production.23 Waters and colleagues24 found that in standing, when increasing hip flexion from 0° to 90°, hip extension force production more than doubled. In addition, the prone standing position may be a more functional position for hip extension than the prone or supine position.25
Figure 1.
Participant in prone standing position with the handheld dynamometer (a) and the isokinetic dynamometer (b).
The research examining the validity of the HHD in measuring peak hip extension strength is limited.4,21,26 Previous studies using the prone, prone belted, and standing positions have demonstrated Pearson product–moment correlation coefficients (r) ranging from 0.42 to 0.68.4,21,26 Current literature has not examined the concurrent validity of the prone standing position. Concurrent validity is the extent to which results obtained by one measurement procedure agree with those of the gold-standard procedure.27 Unlike predictive validity (which compares measurements taken at one point with those taken in the future to predict a construct), concurrent validity evaluates measurements taken at approximately the same time.27 Given the clinical use of the HHD to measure hip extension strength, more studies on its concurrent validity are warranted.
In addition, the minimal detectable change (MDC) of the prone standing position has not been tested with the HHD. The MDC is the smallest amount of change, outside of error, that can be assumed to reflect true change between two points rather than a variation in measurement.28 Establishing the MDC allows clinicians to determine whether a difference in performance is real and reliable; at the same time, it tells us whether the measurement tool used is able to detect such a change.28
The overall aim of our study, therefore, was to assess the ability of the HHD to quantify hip extension muscle strength in a prone standing position. The study had three specific objectives: First, to determine whether use of an HHD is a valid method of measuring hip extension strength relative to an IKD in a prone standing position; second, to establish the MDC for hip extension strength using the HHD and IKD; and, third, to examine whether a single-trial measure, as typically used in clinical practice, is representative of multitrial mean measures. We hypothesized that the HHD would provide a valid measure of hip extension strength in the prone standing position relative to the IKD.
Methods
Participants
We recruited a convenience sample of 20 English-speaking participants—9 men (mean age 30.0 [SD 8.3] y, mean weight 84.0 [SD 5.4] kg, mean height 1.82 [SD 0.04] m) and 11 women (mean age 28.0 [SD 9.1] y, mean weight 63.7 [SD 8.2] kg, mean height 1.66 [SD 0.08] m)—from the University of British Columbia and the surrounding community. Potential participants were excluded if they reported a back or lower extremity injury within the previous 3 months; had participated in maximal exercise in the previous 24 hours; or had any existing conditions that would contraindicate a maximal muscle contraction.
The study was approved by the University of British Columbia Research Ethics Board and conforms to the Human and Animal Rights requirements of the February 2006 International Committee of Medical Journal Editors' Uniform Requirements for Manuscripts Submitted to Biomedical Journals. All participants signed an informed consent form before participating.
Instrumentation and testers
The testers were three final-year physical therapy students with no prior experience using either an HHD or an IKD. Before beginning the study, each tester demonstrated the ability to collect five trials on healthy participants with values within 5% of one another. We also compared data across testers to ensure that measures for each single participant were within 5% across testers. Two testers participated in each measurement session, one collecting the IKD data while another used the HHD, and each tester was blinded to the measurements taken with the other tool. To limit the effects of motor learning, testing order was randomized by drawing cards to determine whether the participant's dominant or non-dominant leg was tested first and whether testing began with the IKD or the HHD.6
Handheld dynamometer procedures
The MicroFET2 HHD (Hoggan Health Technologies Inc., Salt Lake City, UT) was used to assess hip extension strength in the prone standing position (see Figure 1a). Using the testing position derived from studies by Wang and colleagues22 and Lue and colleagues,6 participants leaned forward on a plinth to support their trunk, keeping the knee of their non-test leg extended and in a straight line below the hip. Participants were instructed to rest their head on their hands and not to hold onto the plinth. With the test leg in 45° of hip flexion and full knee extension, the tester marked the HHD position perpendicular to the posterior thigh, 5 cm above the midpoint of the knee-joint line.20 The moment arm was measured as the distance from the greater trochanter to the mark and was used to convert the raw data in kilograms to Newton metres. One tester operated the HHD on the marked point, with the participant's pelvis stabilized by a belt to minimize compensatory movements. The tester using the HHD was in a low or a high lunge position, depending on the strength of the participant.
Testers demonstrated the prone standing testing position and conducted one practice trial, which allowed participants to familiarize themselves with the procedure and ensured testers were exerting a static force equal to the participant's. To optimize an isometric hip extension contraction, testers instructed participants to assume the starting position by extending their hip back and up until they reached 45° of hip flexion (relative hip extension) and to maintain this position during the trial using their gluteal muscles. Participants were instructed to gradually increase their effort to maximum to improve movement isolation and minimize compensation. The contraction was held for 5 seconds, with the tester exerting a force equal to that of the participant, to perform an isometric “make” test.22 All testers used a standardized script of encouragement with equal enthusiasm across all participants, and all participants were able to complete five 5-second trials. There was a 30-second rest after each trial to minimize the effects of fatigue.
Isokinetic dynamometer procedures
The Biodex Pro4 IKD (Biodex Medical Systems Inc., Shirley, NY) was used to assess hip extension strength in prone standing position (see Figure 1b). All Biodex tests were performed in isometric mode (i.e., with no gravity correction applied). Participants stood with the greater trochanter within the axis of rotation of the attachment of the IKD. The participant's trunk was supported on a plinth with a belt stabilizing the pelvis, in the same position as for HHD testing. With the test leg in 45° of hip flexion and full knee extension, the tester positioned the dynamometer pad on the posterior thigh, 5 cm above the midpoint of the knee-joint line, and instructed participants to rest their head on their hands and not to hold onto the plinth. The same protocol described above for the HHD was used with the IKD; testers collected five individual trials per leg.
Because prone standing is not the manufacturer-recommended position for measuring hip extension strength with the Biodex Pro4 dynamometer, we also took measurements in the recommended supine position on another test day. The participant was supine, with the test leg strapped in the IKD attachment at 90° of hip flexion and knee flexion, the contralateral leg in neutral hip flexion over the edge of the Biodex chair, and the trunk and pelvis stabilized using the Biodex belts. The rest of the protocol was the same as described earlier.
Statistical analysis
IBM SPSS version 20.0 (IBM Corporation, Armonk, NY) was used for data analysis. Data were excluded for participants unable to maintain the contraction for 5 seconds on the IKD. We analyzed peak torque values for the HHD and IKD testing using trial 1, the mean of all five trials, and the mean of three trials (excluding the highest and lowest of the five trial values). Two-way analyses of variance (ANOVA), with task (HHD, IKD prone standing, IKD supine) and leg (right, left) as factors, were used to look for significant differences across the three strength measurements and between the right and left legs. The data were normally distributed, as confirmed by statistically insignificant values of the Kolmogorov–Smirnov test, and the homogeneity of variance was confirmed by Levene's test for equality of error variances. Because the assumption of sphericity of the data was not satisfied (Mauchly's test for sphericity), we used Greenhouse–Geisser corrections in interpreting the results.
To examine concurrent validity, we used linear regression analyses to compare the three trial means for HHD, IKD prone standing, and IKD supine peak torque measures. Correlations were defined as high for r values greater than 0.70, moderate for 0.50–0.69, low for 0.26–0.49, and little or no correlation for 0.00–0.25.21 MDC was calculated for the 95% CI as , where . Intrasession reliability was assessed using ICC3,1 values, with consistency agreement for three- and five-trial means on the HHD, IKD prone standing, and IKD supine. The ranges used to assess the strength of the ICC values were poor (<0.69), fair (0.70–0.79), good (0.80–0.89), and high (0.90–1.00).21 To compare HHD trial 1 peak torques with three- and five-trial means, we used the Pearson product–moment correlation coefficients (r) and paired t-tests.
Results
Table 1 reports mean values for HHD, IKD prone standing, and IKD supine positions for trial 1 and three- and five-trial means for the left and right limbs. We found no statistically significant differences between limbs across the three positions (F2,1=0.481, p=0.62), but there was a statistically significant difference in torques across the three positions (HHD=58.43 Nm, IKD prone standing=50.40 Nm, IKD supine=174.54 Nm; F2,1=153.6, p=0.001).
Table 1.
Mean Peak Torque and Intrasession Reliability of the Peak Torque Values on the HHD, ID Prone Standing, and ID Supine
| Trial 1 |
3 Trials |
5 Trials |
|||
|---|---|---|---|---|---|
| Measures | Mean (SD) | Mean (SD) | ICC3,1 (95% CI) | Mean (SD) | ICC3,1 (95% CI) |
| HHD, prone standing | |||||
| L | 58.01 (14.00) | 57.73 (11.69) | 0.95* (0.89–0.98) | 57.56 (12.46) | 0.81* (0.67–0.91) |
| R | 59.02 (14.22) | 59.13 (10.97) | 0.93* (0.86–0.97) | 59.10 (11.77) | 0.80* (0.67–0.90) |
| IKD, prone standing | |||||
| L | 48.20 (25.84) | 48.02 (23.98) | 0.96* (0.90–0.98) | 48.71 (24.23) | 0.82* (0.64–0.94) |
| R | 51.34 (24.93) | 52.79 (24.66) | 0.87* (0.75–0.94) | 53.04 (25.95) | 0.91* (0.80–0.97) |
| IKD, supine | |||||
| L | 163.24 (52.78) | 164.44 (52.73) | 0.97* (0.94–0.99) | 164.47 (53.66) | 0.90* (0.83–0.96) |
| R | 184.44 (78.82) | 184.64 (73.58) | 0.99* (0.97–1.00) | 186.89 (72.89) | 0.97* (0.94–0.99) |
*p≤0.001.
ICC=intraclass correlation coefficient; HHD=handheld dynamometer; L=left; R=right; IKD=isokinetic dynamometer.
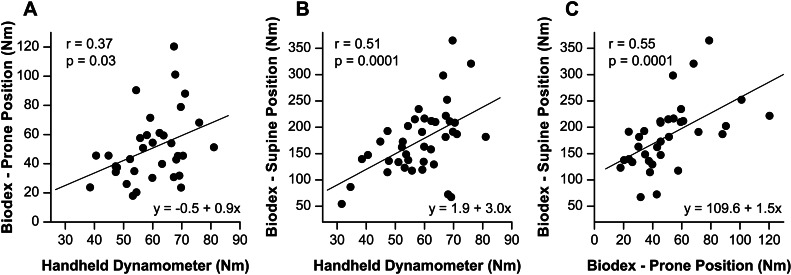
We observed weak to moderate correlations (r values of 0.37–0.51, p≤0.05; see Figures 2a and 2b) between three-trial peak torque values on the HHD and three-trial peak torque values on the IKD, both in prone standing and in supine. Values were moderately correlated (r=0.55, p≤0.001; see Figure 2c) between the IKD in prone standing and supine positions.
Figure 2.
Scatterplot of peak torque values (in Newton metres) for the three-trial means: (a) HHD versus IKD prone standing; (b) HHD versus IKD supine; (c) IKD prone standing versus IKD supine, including the lines of best fit.
HHD=handheld dynamometer; IKD=isokinetic dynamometer.
We calculated MDC and MDC% values for the HHD and for the IKD prone standing and supine positions. MDC was 14.8 Nm (MDC%=25.4%) for the HHD, 25.6 Nm (50.1%) for the IKD prone standing, and 41.5 Nm (23.6%) for the IKD supine. The MDC was lowest for the HHD. Table 1 reports ICC intrasession reliability values, which show good to high intrasession reliability across the three measurement conditions.
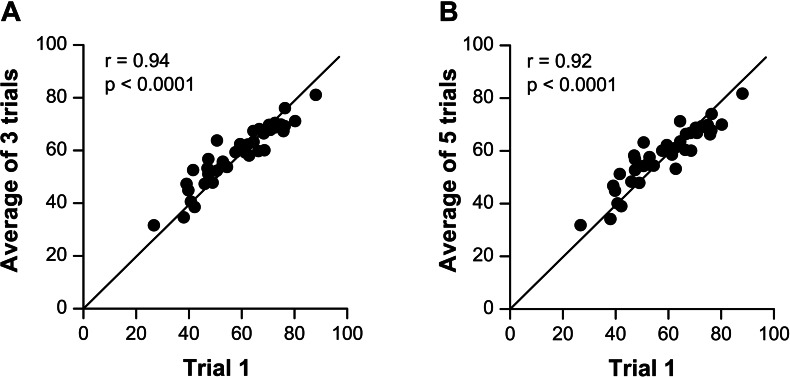
Correlations were high (r=0.94, p<0.001) between HHD trial 1 peak torque values and both three-trial (r=0.94, p<0.001) and five-trial means (r=0.92, p<0.001; see Figure 3). A paired t-test showed no significant differences in HHD peak torque values between trial 1 and either three-trial (p=0.97) or five-trial means (p=0.91).
Figure 3.
Scatterplot of peak torque values (in Newton metres), comparing the handheld dynamometer trial 1 value with the three-trial mean (b) and the five-trial mean (b). The line of unity is included.
Discussion
Our findings show that in healthy adults, hip extensor strength values assessed using an HHD in the prone standing position demonstrated moderate concurrent validity. The HHD showed good to high intrasession reliability across both three- and five-trial averages, and the MDC was lowest using the HHD in the prone standing position compared with the IKD. Values obtained from trial 1, which is typical of the performance of a single trial in clinical practice, demonstrated high validity relative to three-trial means.
Initially, we compared HHD data with data obtained from the IKD in prone standing, so as to standardize the testing position across instruments when assessing the validity of the HHD. Concurrent validity was low (r=0.37) for these two conditions, however, likely as a result of not using the manufacturer-recommended supine position when assessing hip extension strength on the IKD. Testers also encountered difficulties with the IKD in the prone standing position: At times, the machine was unable to read the force production on the pad, and data for these trials had to be excluded as a result. Similarly, Kawaguchi and Babcock4 found that participants had difficulty in isolating their hip extensors and required verbal cues when in the prone standing position on an IKD.
Participants were retested in supine position on the IKD. This position provides more stability and allows participants to recruit other muscles when performing the movement, resulting in higher torque values. Although straps were used to stabilize the participants, the movement was less specific to hip extension, and global recruitment patterns were observed. The prone standing testing was more specific for isolated hip extension measures. Studies have shown that a position similar to prone standing allows for an optimal length–tension relationship of the gluteal muscles because they are lengthened with hip flexion in this position23 but that hamstring activation is minimized.24 It may also be that additional straps and a supported back in the supine position allows greater absolute force production. In addition, the supine position used on the IKD had the hip flexed to 90°, versus 45° of hip flexion in the prone standing position. Waters and colleagues24 found that 90° of hip flexion resulted in higher hip extension force values than 45° of hip flexion.
Despite the difference in magnitudes of strength, peak torque values for the HHD and the IKD supine were moderately correlated (r=0.51), which suggests that although the peak torques measured in these two positions differed, strength measured in prone standing was significantly related to strength measured in supine. As discussed earlier, this may be because the prone standing position predominantly recruited gluteal muscles, whereas the supine position may have allowed for other hip extensors to be activated as well.23,24 We should note, however, that despite cueing, several participants struggled to engage only their gluteal muscles in the prone standing position and exhibited some additional back extension and torsion, which may be the result of the novel test position and the participants' exerting a strong contraction. When participants were retested in supine, testers were unable to gain sufficient mechanical advantage to test the HHD, and therefore it was not feasible to examine hip extension using the HHD in a supine position. Because our study attempted to replicate a typical clinical setting, testers did not use additional straps or belts to fixate the HHD because such a set-up is less clinically feasible.
It is interesting to note that Rasch and colleagues,29 who tested hip extension strength in a modified prone standing position with participants with both uninjured and osteoarthritic hips, found significantly higher absolute hip extension torque values across both populations than we found in our study. However, testing in Rasch and colleagues' study used a much more elaborate and supported position, involving multiple belt straps, a surface for the trunk on a 45° incline, and handlebars; the greater stability resulting from this setup would lend itself to higher torque values,29 but its clinical feasibility is questionable.
We tested participants in the prone standing position to replicate the test position used by Lue and colleagues,6 which has been shown to have high interrater and intrasession reliability in healthy adults. Overall, few studies4,21,26 have examined the validity of the HHD in measuring peak hip extension, and their authors have used both prone and standing positions. Previous research has not examined the concurrent validity of the prone standing position used in our study. Hip extension strength measured with the HHD in our study showed low to moderate correlations (r values of 0.37–0.51) with measurements taken with the IKD; these values are lower than those previously observed in the standing (r values of 0.57–0.63)21 and prone (r values of 0.42–0.68)4,26 positions.
In this study, the HHD demonstrated good to high intrasession reliability. Findings from the three-trial average were consistent with previous reliability studies in the prone standing position.6 They were also comparable to those of another study of occupational therapists with no prior HHD experience, showing that with training, therapists are able to use dynamometers with a high level of reliability.16
Of the three measurements, the HHD had the lowest MDC (14.8 Nm, or 25.4%). Although the HHD had the lowest MDC, the IKD in supine had the lowest MDC% (albeit by only 1.8%), likely because IKD values were much higher in supine than in prone standing. This finding is consistent with those of Thorborg and colleagues,28 who found MDC% values of HHD for hip and knee strength ranging from 14% to 29%.
Because clinicians tend to take only one trial for muscle strength assessments, it is important to establish the validity of single-trial versus multitrial mean measures.18 As a commonly used musculoskeletal textbook states, the therapist should use as few repetitions as possible.17 We found high correlations between the first trial and the mean of three trials with the HHD, and the same trend held for five-trial means, which indicates that it was not a result of rejecting the highest and lowest values. Thus, we can conclude that the first trial is representative of the mean of three trials in healthy populations. Further research on this relationship is warranted to determine whether single-trial measures in pathologic populations also demonstrate high correlations and may be clinically appropriate.
An important contribution of our study is the establishment of moderate levels of concurrent validity of the HHD in measuring peak hip extension strength in prone standing, which has not been investigated in previous studies. This is of interest to clinicians because the testing position used can be easily replicated in a clinic, and thus it was important to ascertain the HHD's feasibility for use in a clinical setting. Future studies should investigate the concurrent validity of the HHD in clinical populations who might present with muscle imbalances at the hip.
Our study has several limitations. First, our sample size was small; although many reliability and validity studies have used similar sample sizes, having more participants would allow for more generalizability. Second, when testing in the prone standing position, participants often struggled to isolate their gluteal muscles without compensating, despite practice trials and cueing. Co-contraction, moving through habitual patterns, and participants' motor control may have had an impact on peak torque produced. Third, tester strength has previously been identified as a potential limitation of HHD use; to minimize the effect of tester strength, however, our testers underwent a training protocol to ensure that results were within 5% both within and between testers. Suggested alternatives to minimize the effects of tester strength require construction of fixed structures, which would decrease the clinical feasibility of the protocol.30 Finally, participants recruited to the study were young and healthy; generalizing our results to a clinical population, therefore, would require further investigation to address variability between trials and muscle recruitment strategies in a pathologic population.
Conclusion
This study demonstrates that in the prone standing position, HHD has moderate concurrent validity in measuring peak hip extension strength in healthy adults aged 20–53 years. With training, therapists are able to use the HHD to measure peak hip extension strength with a high level of reliability, and values are consistent with previous findings using the prone standing position. MDC in the prone standing position was found to be lowest using the HHD. Finally, single-trial HHD measures are highly correlated with three- and five-trial average values and may therefore be clinically appropriate.
Key Messages
What is already known on this topic
Muscle imbalances at the hip have been linked to a variety of musculoskeletal conditions. To objectively assess these imbalances, a valid, cost-effective means of measuring strength is needed. Hip extension strength has previously been assessed in the supine, standing, and prone positions with moderate levels of validity. Recent studies have reported greater reliability using the prone standing position, but the validity of this position has not been tested.
What this study adds
The handheld dynamometer (HHD) was found to have high reliability and moderate validity for assessing peak hip extension strength in the prone standing position. The minimal detectable change for hip extension strength using the HHD was established. Single-trial measures were also investigated because clinicians tend to use only one trial when assessing muscle strength. Single trials with the HHD in the prone standing position demonstrated high correlations with average values in healthy populations.
References
- 1. Deones VL, Wiley SC, Worrell T. Assessment of quadriceps muscle performance by a hand-held dynamometer and an isokinetic dynamometer. J Orthop Sports Phys Ther. 1994;20(6):296–301. http://dx.doi.org/10.2519/jospt.1994.20.6.296. Medline:7849749 [DOI] [PubMed] [Google Scholar]
- 2. Reinking MF, Bockrath-Pugliese K, Worrell T, et al. . Assessment of quadriceps muscle performance by hand-held, isometric, and isokinetic dynamometry in patients with knee dysfunction. J Orthop Sports Phys Ther. 1996;24(3):154–9. http://dx.doi.org/10.2519/jospt.1996.24.3.154. Medline:8866274 [DOI] [PubMed] [Google Scholar]
- 3. Stark T, Walker B, Phillips JK, et al. . Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472–9. http://dx.doi.org/10.1016/j.pmrj.2010.10.025. Medline:21570036 [DOI] [PubMed] [Google Scholar]
- 4. Kawaguchi JK, Babcock G. Validity and reliability of handheld dynametric strength assessment of hip extensors and abductor muscles. Athletic Training Sports Health Care. 2010;2(1):11–7. http://dx.doi.org/10.3928/19425864-20101221-04 [Google Scholar]
- 5. May LA, Burnham RS, Steadward RD. Assessment of isokinetic and hand-held dynamometer measures of shoulder rotator strength among individuals with spinal cord injury. Arch Phys Med Rehabil. 1997;78(3):251–5. http://dx.doi.org/10.1016/S0003-9993(97)90029-0. Medline:9084345 [DOI] [PubMed] [Google Scholar]
- 6. Lue YJ, Hsieh CL, Liu MF, et al. . Influence of testing position on the reliability of hip extensor strength measured by a handheld dynamometer. Kaohsiung J Med Sci. 2009;25(3):126–32. http://dx.doi.org/10.1016/S1607-551X(09)70051-8. Medline:19419917 [DOI] [PubMed] [Google Scholar]
- 7. Lyons K, Perry J, Gronley JK, et al. . Timing and relative intensity of hip extensor and abductor muscle action during level and stair ambulation. An EMG study. Phys Ther. 1983;63(10):1597–605. Medline:6622534 [DOI] [PubMed] [Google Scholar]
- 8. Perry J, Weiss WB, Burnfield JM, et al. . The supine hip extensor manual muscle test: a reliability and validity study. Arch Phys Med Rehabil. 2004;85(8):1345–50. http://dx.doi.org/10.1016/j.apmr.2003.09.019. Medline:15295763 [DOI] [PubMed] [Google Scholar]
- 9. Massoud Arab A, Reza Nourbakhsh M, Mohammadifar A. The relationship between hamstring length and gluteal muscle strength in individuals with sacroiliac joint dysfunction. J Manual Manip Ther. 2011;19(1):5–10. http://dx.doi.org/10.1179/106698110X12804993426848. Medline:22294848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nadler SF, Malanga GA, DePrince M, et al. . The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10(2):89–97. http://dx.doi.org/10.1097/00042752-200004000-00002. Medline:10798789 [DOI] [PubMed] [Google Scholar]
- 11. Pua YH, Wrigley TV, Cowan SM, et al. . Hip flexion range of motion and physical function in hip osteoarthritis: mediating effects of hip extensor strength and pain. Arthritis Rheum. 2009;61(5):633–40. http://dx.doi.org/10.1002/art.24509. Medline:19405017 [DOI] [PubMed] [Google Scholar]
- 12. Rasch A, Byström AH, Dalen N, et al. . Reduced muscle radiological density, cross-sectional area, and strength of major hip and knee muscles in 22 patients with hip osteoarthritis. Acta Orthop. 2007;78(4):505–10. http://dx.doi.org/10.1080/17453670710014158. Medline:17966005 [DOI] [PubMed] [Google Scholar]
- 13. Rossi MD, Brown LE, Whitehurst MA. Assessment of hip extensor and flexor strength two months after unilateral total hip arthroplasty. J Strength Cond Res. 2006;20(2):262–7. Medline:16686551 [DOI] [PubMed] [Google Scholar]
- 14. Drouin JM, Valovich-mcLeod TC, Shultz SJ, et al. . Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91(1):22–9. http://dx.doi.org/10.1007/s00421-003-0933-0. Medline:14508689 [DOI] [PubMed] [Google Scholar]
- 15. Martin HJ, Yule V, Syddall HE, et al. . Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Bodex dynamometry. Gerontology. 2006;52(3):154–9. http://dx.doi.org/10.1159/000091824. Medline:16645295 [DOI] [PubMed] [Google Scholar]
- 17. Clarkson HM. Musculoskeletal assessment: joint range of motion and manual muscle strength. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 18. Magee DJ. Orthopedic physical assessment. 5th ed. St. Louis (MO): Saunders Elsevier; 2008. [Google Scholar]
- 19. Kelln BM, McKeon PO, Gontkof LM, et al. . Hand-held dynamometry: reliability of lower extremity muscle testing in healthy, physically active, young adults. J Sport Rehabil. 2008;17(2):160–70. Medline:18515915 [DOI] [PubMed] [Google Scholar]
- 20. Thorborg K, Petersen J, Magnusson SP, et al. . Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scand J Med Sci Sports. 2010;20(3):493–501. http://dx.doi.org/10.1111/j.1600-0838.2009.00958.x. Medline:19558384 [DOI] [PubMed] [Google Scholar]
- 21. Arnold CM, Warkentin KD, Chilibeck PD, et al. . The reliability and validity of handheld dynamometry for the measurement of lower-extremity muscle strength in older adults. J Strength Cond Res. 2010;24(3):815–24. http://dx.doi.org/10.1519/JSC.0b013e3181aa36b8. Medline:19661831 [DOI] [PubMed] [Google Scholar]
- 22. Wang CY, Olson SL, Protas EJ. Test-retest strength reliability: hand-held dynamometry in community-dwelling elderly fallers. Arch Phys Med Rehabil. 2002;83(6):811–5. http://dx.doi.org/10.1053/apmr.2002.32743. Medline:12048660 [DOI] [PubMed] [Google Scholar]
- 23. Pohtilla JF. Kinesiology of hip extension at selected angles of pelvifemoral extension. Arch Phys Med Rehabil. 1969;50(5):241–50. Medline:5769844 [PubMed] [Google Scholar]
- 24. Waters RL, Perry J, McDaniels JM, et al. . The relative strength of the hamstrings during hip extension. J Bone Joint Surg Am. 1974;56(8):1592–7. Medline:4434027 [PubMed] [Google Scholar]
- 25. Dyball KM, Taylor NF, Dodd KJ. Retest reliability of measuring hip extensor muscle strength in different testing positions in young people with cerebral palsy. BMC Pediatr. 2011;11(1):42–9. http://dx.doi.org/10.1186/1471-2431-11-42. Medline:21609493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Katoh M, Hiiragi Y, Uchida M. Validity of isometric muscle strength measurements of the lower limbs using a handheld dynamometer and belt: a comparison with an isokinetic dynamometer. J Phys Ther Sci. 2011;23(4):553–7. http://dx.doi.org/10.1589/jpts.23.553 [Google Scholar]
- 27. Haynes SN, Richard DCS, Kubany ES. Content validity in psychological assessment: a functional approach to concepts and methods. Psychol Assess. 1995;7(3):238–47. http://dx.doi.org/10.1037/1040-3590.7.3.238 [Google Scholar]
- 28. Thorborg K, Bandholm T, Hölmich P. Hip- and knee-strength assessments using a hand-held dynamometer with external belt-fixation are inter-tester reliable. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):550–5. http://dx.doi.org/10.1007/s00167-012-2115-2. Medline:22773065 [DOI] [PubMed] [Google Scholar]
- 29. Rasch A, Dalén N, Berg HE. Test methods to detect hip and knee muscle weakness and gait disturbance in patients with hip osteoarthritis. Arch Phys Med Rehabil. 2005;86(12):2371–6. http://dx.doi.org/10.1016/j.apmr.2005.05.019. Medline:16344037 [DOI] [PubMed] [Google Scholar]
- 16. Lindstrom-Hazel D, Kratt A, Bix L. Interrater reliability of students using hand and pinch dynamometers. Am J Occup Ther. 2009;63(2):193–7. http://dx.doi.org/10.5014/ajot.63.2.193. Medline:19432057 [DOI] [PubMed] [Google Scholar]
- 30. Stone CA, Nolan B, Lawlor PG, et al. . Hand-held dynamometry: tester strength is paramount, even in frail populations. J Rehabil Med. 2011;43(9):808–11. http://dx.doi.org/10.2340/16501977-0860. Medline:21826388 [DOI] [PubMed] [Google Scholar]