Abstract
Objective
To determine whether baseline dimensions of adult insecure attachment (avoidant and anxious) moderated outcome in a secondary analysis of a randomized controlled trial comparing cognitive–behavioral therapy (CBT) plus supportive listening (CBT + SL) versus CBT plus interpersonal and emotional processing therapy (CBT + I/EP).
Method
Eighty-three participants diagnosed with generalized anxiety disorder (GAD) were recruited from the community and assigned randomly to CBT + SL (n = 40) or to CBT + I/EP (n = 43) within a study using an additive design. PhD-level psychologists treated participants. Blind assessors evaluated participants at pretreatment, posttreatment, 6-month, 12-month, and 2-year follow-up with a composite of self-report and assessor-rated GAD symptom measures (Penn State Worry Questionnaire, Hamilton Anxiety Rating Scale, Clinician’s Severity Rating). Avoidant and anxious attachment were assessed using self-reported dismissing and angry states of mind, respectively, on the Perceptions of Adult Attachment Questionnaire.
Results
Consistent with our prediction, at all assessments higher levels of dismissing styles in those who received CBT + I/EP predicted greater change in GAD symptoms compared with those who received CBT + SL for whom dismissiveness was unrelated to the change. At postassessment, higher angry attachment was associated with less change in GAD symptoms for those receiving CBT + I/EP, compared with CBT + SL, for whom anger was unrelated to change in GAD symptoms. Pretreatment attachment-related anger failed to moderate outcome at other time points and therefore, these moderation effects were more short-lived than the ones for dismissing attachment.
Conclusions
When compared with CBT + SL, CBT + I/EP may be better for individuals with GAD who have relatively higher dismissing styles of attachment.
Keywords: GAD, emotional processing, attachment, interpersonal problems, CBT
According to attachment theory, children’s experiences with care-givers are internalized as cognitive–affective models of interpersonal relationships (e.g., Ainsworth, Blehar, Waters, & Wall, 1978). Such internal working models are carried forward into adulthood and influence the quality of close relationships (e.g., parent–child, romantic relationships; Bowlby, 1973; Bowlby, 1969; Hazan & Shaver, 1994), including the therapeutic relationship (e.g., Dozier, Cue, & Barnett, 1994; Skourteli & Lennie, 2011). Insecure attachment has been linked theoretically and empirically to interpersonal problems and difficulties regulating emotion (e.g., Cassidy & Berlin, 1994; Moutsiana et al., 2015). Although attachment has been conceptualized as a typology, dimensions better characterize the quality of attachment in both childhood and adulthood (Fraley & Spieker, 2003; Fraley & Waller, 1998). In adulthood, insecure attachment has been characterized along two primary dimensions (Brennan, Clark, & Shaver, 1998; Fraley & Shaver, 2000): avoidance and anxiety. These dimensions specify behavioral response styles in close relationships, and therefore, may be useful in guiding predictions about interpersonal behavior within the therapeutic relationship and thus, treatment response (e.g., Bowlby, 1973; Mikulincer & Shaver, 2008).1
Attachment-related avoidance is thought to develop in response to caregivers who are rejecting or unaccepting (Ainsworth et al., 1978) and, when carried into adulthood is characterized by tendencies to be overly autonomous, avoid disappointment or frustration by others’ failure to provide support (Dozier, 1990; Lavy, Mikulincer, & Shaver, 2010), hide feelings, disclose less to others, deal with rejection by maintaining distance (Davis, Shaver, & Vernon, 2003; Kobak & Sceery, 1988), detach oneself from and avoid emotions (Feeney, 1995; Mikulincer & Orbach, 1995), and cope with threat via increasingly pessimistic appraisals (Berant, Mikulincer, & Shaver, 2008; Williams & Riskind, 2004).
Attachment-related anxiety is thought to develop as a result of unresponsive or inconsistently available caretakers (Ainsworth et al., 1978). When carried into adulthood, it is characterized by tendencies to: desire extreme closeness, become overly dependent on significant others for support (Feeney & Noller, 1990), be intrusive with romantic partners (Lavy et al., 2010), feel unable to cope alone (Birnbaum, Orr, Mikulincer, & Florian, 1997; Mikulincer & Florian, 1995), and intensely fear rejection (Feeney, 1995; Mikulincer & Orbach, 1995). Those higher on attachment-related anxiety react to relationship breakups with angry protests, intense preoccupation with former partners, and damaged sense of personal identity (Davis et al., 2003; Sbarra, 2006). They have easy access to emotional memories and negative emotions (Mikulincer & Orbach, 1995), and are prone to distress-intensifying appraisals and coping strategies (Feeney, 1995; Mikulincer & Orbach, 1995). Thus, insecure attachment appears to confer risk through relational styles of emotionally avoidant and dismissing behaviors with inappropriate autonomy from others (avoidant), or of excessive negative emotions (anger and fear) and inappropriate dependence on others (anxious).
Anxious and avoidant attachment have been theorized as possible contributing factors to the development of GAD and its core symptom of worry. Although most of the data in support of this theory is based on cross-sectional studies, worry severity was associated with both avoidant and anxious attachment in children (Brown & Whiteside, 2008) and preadolescents (Muris, Meesters, Merckelbach, & Hülsenbeck, 2000). Furthermore, a diagnosis of GAD was correlated positively with avoidant and anxious attachment and negatively with secure attachment in the National Comorbidity Study (Mickelson, Kessler, & Shaver, 1997). In addition, severity of GAD discriminated those with anxious attachment from those with secure attachment (Muris, Mayer, & Meesters, 2000) and compared with the number of infants classified as secure or avoidant, twice as many infants who were classified as anxious later received a diagnosis of GAD or social phobia in late adolescence (Warren, Huston, Egeland, & Sroufe, 1997). In other studies, however, severity of GAD discriminated those with avoidant attachment from those with secure attachment (Muris, Meesters, van Melick, & Zwambag, 2001). Similarly, avoidant attachment was most robustly associated with new occurrences of GAD in adults compared with anxious attachment, which longitudinally predicted new diagnoses of depression or social phobia (Bifulco et al., 2006). Therefore, whereas the same number of studies point to both avoidant and anxious attachment in the development of GAD, data does not always support both types consistently, possibly due to varying sample characteristics or methods for measuring attachment.
Higher levels of attachment-related avoidance and anxiety in those with GAD may explain the heightened levels of interpersonal problems (Newman & Erickson, 2010) and emotion-regulation difficulties (Mennin, Heimberg, Turk, & Fresco, 2002; Newman & Llera, 2011) to which these individuals are prone. People with GAD have more marital conflict (Whisman, Sheldon, & Goering, 2000), and are more likely to be separated or divorced (Afifi, Cox, & Enns, 2006) compared with those with other psychiatric disorders and to nonanxious participants. They also exhibit poorer relationship quality, interpersonal skills deficits, and habitual maladaptive ways of relating to others (Priest, 2013; Przeworski et al., 2011). Emotionally, they are prone to increasingly pessimistic and distress intensifying appraisals (Newman & Llera, 2011), heightened intensity of emotions (Llera & Newman, 2010; Mennin, Holaway, Fresco, Moore, & Heimberg, 2007), and are more reactive than nonanxious participants to expression of negative emotions in others (Erickson & Newman, 2007). At the same time, they are uncomfortable with and avoid processing negative emotions (Llera & Newman, 2010, 2014; Newman, Llera, Erickson, Przeworski, & Castonguay, 2013; Turk, Heimberg, Luterek, Mennin, & Fresco, 2005).
In addition to explaining interpersonal problems and emotion regulation difficulties, insecure attachment, especially when characterized by avoidant, dismissing styles, might explain why CBT does not work well for everybody with GAD. Following CBT, on average, only 50% of those with GAD exhibit high endstate functioning (Borkovec & Ruscio, 2001). At the same time, compared with those with secure attachment, avoidant attachment, with its associated dismissive style, has been found to predict greater rejection of treatment providers, less willingness to seek psychotherapy, less self-disclosure to therapists, and poorer compliance with and use of treatment (Dozier, 1990; Vogel & Wei, 2005). Avoidant attachment also predicts poor psychotherapy outcome (Byrd, Patterson, & Turchik, 2010; Horowitz, Rosenberg, & Bartholomew, 1993) as well as dropping out of therapy (Tasca et al., 2006; Tasca, Taylor, Bissada, Ritchie, & Balfour, 2004). In contrast, individuals with anxious attachment and associated over-emotional and dependent attachment style are more likely to seek help, admit their distress, and to be more compliant with treatment than those with avoidant attachment (Dozier, 1990; Vogel & Wei, 2005). Thus, although both attachment-related avoidance and anxiety may contribute to risk for GAD, their respective response styles, dismissing or emotionally fearful and angry, may function as individual differences that predict which treatments work best for particular individuals with GAD.
Newman and colleagues developed an integrative treatment that combined cognitive–behavioral therapy (CBT) for GAD with techniques designed to address interpersonal problems and emotional processing avoidance (Newman, Castonguay, Borkovec, & Molnar, 2004). In an initial open trial, the combination of CBT with interpersonal and emotional processing (I/EP) techniques generated promising results (Newman, Castonguay, Borkovec, Fisher, & Nordberg, 2008). However, a subsequent randomized controlled trial found no significant difference between a treatment that added techniques to address emotional processing avoidance and interpersonal problems (CBT + I/EP) compared with standard CBT plus supportive listening (CBT + SL) on GAD symptoms (Newman et al., 2011).
As the first secondary analysis of this outcome trial, the goal of the current study was to examine whether dimensional levels of avoidance and anxiety, measured by self-reports of dismissing and angry states of mind with respect to current relationships with caregivers, would differentially predict responses to compared treatments. We hypothesized that higher levels of self-reported dismissing styles (i.e., avoidance) at baseline would predict a better response to our combined CBT plus interpersonal emotional processing therapy than CBT plus supportive listening. Although we are not aware of any studies that have examined the predictive or moderating impact of attachment on the outcome of psychotherapy for GAD, we based this prediction on the assumption that outcome would be superior if there were a match between an individuals’ initial attachment style and deficits that a particular psychotherapy was designed to address. In this case, receiving a psychotherapy that was focused on providing corrective emotional and interpersonal experiences in addition to CBT might be optimal for individuals with higher avoidance who are dismissing, uncomfortable with intimacy, distrustful of others, and tend to avoid emotional processing. However, we suspected that the addition of I/EP might interfere with the outcome of individuals with higher attachment-related anxiety, who have an angry-fearful style, by amplifying emotional reactivity. Such possible negative effects, we reasoned, might provide one explanation for our failure to find a difference between the two compared treatments, that is, that the incremental benefit obtained by one group of clients might have been hidden by a possible negative impact experienced by another group. Specifically, we tentatively expected that clients who reported higher levels of angry states of mind regarding attachment relationships might do better in the control condition (CBT + SL) than in the integrative condition. Since these individuals are overemotional and focusing on anger often triggers rumination, we thought that the addition of emotional-processing techniques might amplify their existing emotional overreactivity and make things worse as opposed to better.
Method
We compared 50-min of CBT, followed by 50-min of interpersonal/emotional processing therapy (I/EP) to 50-min of CBT, followed by 50 min of supportive listening (SL). Controlling for common factors, such a between-groups additive design is a method to examine whether I/EP leads to a significant increment in efficacy beyond CBT (see Behar & Borkovec, 2003).
Participants
Admission criteria included agreement from two separate diagnostic interviews on: a principal diagnosis of DSM–IV GAD, a Clinician’s Severity Rating for GAD (part of the Anxiety Disorders Interview Schedule for DSM–IV; Brown, Di Nardo, & Barlow, 1994) of 4 (moderate) or greater, absence of concurrent psychotherapy or past adequate dosage of CBT, current stable dose of psychotropic medication or medication-free, willingness to maintain stability in medication use during the 14-week therapy period, absence of substance abuse, psychosis, and organic brain syndrome, and be between 18 and 65 years of age. Eighty-three participants were randomly assigned to treatment condition (CBT–SL n = 40, CBT-I/EP n = 43) but 13 people dropped out at early stages of treatment (4 in CBT–SL and 9 in CBT–I/EP, χ2(1, N = 83) = 1.87, p = .17. No pretreatment demographic traits were significantly different across conditions. All participants consented to the study, and IRB approval was attained.
Three experienced PhD-level psychologists conducted therapy at an outpatient clinic. Equal numbers of clients from each condition were assigned randomly to each therapist. Therapists received extensive training. Ongoing supervision was provided throughout the trial.
Measures
Clinician-administered measures
The Anxiety Disorders Interview Schedule for DSM–IV (Brown et al., 1994) has well-established reliability (Brown, Di Nardo, Lehman, & Campbell, 2001). For our interviewers, kappa agreement for GAD was .78. Interviewers assigned a 0−8 Clinicians’ Severity Rating (CSR) to reflect degree of distress and impairment of each disorder. Reliability of CSRs for GAD was .74. The Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959) is a 14-item clinician administered measure of severity of anxious symptomatology. Internal consistency was α = .87 in the current study and interrater reliability was ICC = .89.
Self-report measures
The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990) has high internal consistency (Meyer et al., 1990; .84 in the current sample), retest reliability ranging from .74–.93, as well as strong convergent and discriminant validity (Molina & Borkovec, 1994). Perceptions of Adult Attachment Questionnaire (PAAQ; Lichtenstein & Cassidy, 1991) is a 60-item measure of adult attachment dimensions. Items are based on Main and Goldwyn’s (1998) system for scoring the Adult Attachment Interview (George, Kaplan, & Main, 1985/1996) and on Bowlby’s (1969) attachment theory. It contains eight subscales, tapping three superordinate dimensions: experiences with the primary caregiver, current state of mind/attitudes toward the primary caregiver, and accessibility of childhood memories. Advantages of this measure are that it is faster and easier to implement than an interview; it provides a dimensional rating system as opposed to a categorical system; and it is the only attachment measure of which we are aware that has been used in a clinical GAD sample in a published study. A logistic regression using the PAAQ to predict GAD versus control status found an overall classification accuracy of 73.9% (Cassidy et al., 2009). Participants rated a 5-point Likert-type scale, ranging from 1 = strongly disagree to 5 = strongly agree. Three subscales tapping childhood relationship with the primary caregiver include (a) rejection/neglect (11 items), (b) loved (6 items), and (c) role-reversal/enmeshment (10 items). Four subscales tapping current attitude toward the primary caregiver include (a) vulnerable (5 items), (b) balancing-forgiving (7 items), (c) angry (5 items), and (d) dismissing/derogating (4 items). The third dimension, accessibility of childhood memories, has one subscale labeled no memory (4 items). Factor analysis supported the theory-based scales (Lichtenstein & Cassidy, 1991). Convergent validity was also demonstrated (for details, see Cassidy, Lichtenstein-Phelps, Sibrava, Thomas, & Borkovec, 2009). The subscales were fairly internally consistent in a sample of 247 college students (coefficient alphas: ranging from .62 to .90) and in a sample of 123 mothers (ranging from .51 to .94) (Lichtenstein & Cassidy, 1991). In the current study, coefficient alphas were as follows: entire scale = .77, rejected/neglected = .90, loved = .90, enmeshed = .77, vulnerable = .85, balancing/forgiving = .60, angry = .81, dismissing/derogating = .54, no memory = .93. The primary scales of interest were the dismissing/derogating and the angry scales, which map onto the two-dimensional model of insecure attachment in adults (Brennan et al., 1998; Fraley & Shaver, 2000). In the current sample, the dismissing subscale was correlated significantly with the overly cold subscale of the Inventory of Interpersonal Problems (IIP; Alden, Wiggins, & Pincus, 1990; r = .307, p = .000) and the angry subscale was correlated significantly with the overly expressive subscale of the IIP (r = .239, p = .006) providing convergent validity. The scale also had good retest reliability over a 3-week interval (e.g., dismissing: r = .78; angry: r = .83; Lichtenstein & Cassidy, 1991).
Procedure
Selection and assessor outcome ratings
For those not ruled out during the phone screen, interviewers administered the ADIS, which included the HARS, and CSRs. For post-, 6-month, and 12-month assessment, a briefer version of the ADIS (assessing only those diagnoses identified at pretherapy) was readministered; the complete ADIS and rating scales were given at 24-month follow-up. All interview and self-report measures were administered at every assessment point except the PAAQ. Assessors were uninformed of therapy condition.
Therapy
CBT
All clients received CBT during the first 50-min segment of 14 2-hr sessions (each of two 50-min segments took place sequentially at each session). Targeting intrapersonal aspects of anxious experience, these techniques were part of a CBT protocol previously developed and tested (Borkovec, Newman, Pincus, & Lytle, 2002). These techniques included self-monitoring of anxiety cues, relaxation methods, self-control desensitization, and cognitive restructuring. During CBT, therapists were allowed to address only the learning and application of these methods as they related to intrapersonal anxious experience (see Newman et al., 2011 for more details). However, the therapist could not work on developmental origins, the deepening of affective experience, analysis of how client behavior may have been contributing to relationship difficulties, and behavioral interpersonal skill training.
Interpersonal/emotional processing segment
This segment was informed by Safran and Segal’s (1990) model of interpersonal schema. However, in contrast to Safran’s model, for the purpose of tailoring the treatment to GAD, the segment was designed to address interpersonal problems and to facilitate emotional processing without the direct integration of cognitive techniques. The goals of I/EP were as follows: (a) identification of interpersonal needs, past and current patterns of interpersonal behavior that attempt to satisfy those needs, and emotional experience that underlies these; (b) generation of more effective interpersonal behavior to better satisfy needs; and (c) identification and processing of avoided emotion associated with all therapeutic content. The interventions were based on the following principles: emphasis on phenomenological experience; therapists’ use of their own emotional experience to identify interpersonal markers; use of the therapeutic relationship to explore affective processes and interpersonal patterns, with therapists’ assuming responsibility for their role in the interactions; promotion of generalization via exploration of between-session events and provision of homework experiments; detection of alliance ruptures and provision of emotionally corrective experiences in their resolution; processing of patient’s affective experiencing in relation to past, current, and in-session interpersonal relationships using emotion-focused techniques (e.g., empty-chair and two-chair; Greenberg, 2002); and skill training methods to provide more effective interpersonal behaviors to satisfy identified needs.
Supportive listening segment
This was adopted directly from the SL manual of Borkovec and colleagues (see Borkovec et al., 2002). Therapists were not allowed to use any methods to deepen clients’ emotional experience. Provision of any direct suggestions, advice, or coping methods, were also prohibited.
Adherence and quality checks
Protocols met high levels of adherence and quality based on independent ratings (see Newman et al., 2011).
Planned Analyses
Similar to other treatment studies (e.g., Newman et al., 2011), we created a single continuous variable to represent GAD severity. A composite provides a more valid measure of psychopathology, and one means of reducing experiment-wise error rate (Horowitz, Inouye, & Siegelman, 1979). The three measures used for this composite, the PSWQ, HARS, and CSRs for GAD, were significantly correlated with one another (ranging from .62 to .84). Raw scores for these measures were converted to standardized z scores and averaged for each participant.
The moderator analyses used multilevel models. For each analysis, time, condition, and the attachment subscales were treated as fixed effects and time was treated as a random effect (by nesting time within persons) to predict the composite outcome measure. Because of the dimensional nature of the PAAQ subscales, each subscale was used as a continuous predictor in the results. Each of the pre-post and pre-follow-up analyses used separate models, as including piecewise coefficients in the model would introduce substantial multicollinearity. Mundry and Nunn (2009) suggest that stepwise, forward, and backward selection methods lead to biased results. On the basis of their recommendations, each analysis included all attachment subscale variables in the model. Subsequently, a parsimonious model was obtained after removing all attachment subscales except the two subscales with the largest effects in the model, and the model was run again. Also, there were three follow-up assessments: 6-month, 1-year, and 2-years, and accordingly, all three time points were included as a continuous predictor in the follow-up model. As recommended by Dunlap, Cortina, Vaslow, and Burke (1996), Cohen’s d was calculated using the between-groups t test value, d = t(2/n)1/2. All significant three-way interactions were investigated for slope differences between CBT + I/EP and CBT + SL. Also, simple slopes for CBT + I/EP and CBT + SL were investigated for these interactions. All post hoc analyses were analyzed in a dimensional way, using the R package, phia (Rosario-Martinez, 2013). For the chi-square statistics reported in the interaction contrasts, Cohen’s d values were calculated from, d = (4 χ2)/(N− χ2)1/2 based on Dunst and colleagues, (2004).
Results
Pretreatment Attachment and GAD Symptoms
Table 1 provides descriptive statistics and correlations between the subscales of the PAAQ at baseline. There were pretreatment differences between the compared treatments on the PAAQ angry subscale, F(2, 79) = 3.57, p = .033, . Those assigned to CBT + SL (M = 2.81, SD = 0.96) had more current anger at their primary caretakers than those assigned to CBT + I/EP (M = 2.14, SD = 0.94). There were no significant pretreatment differences for balancing/forgiving, F(2, 79) = .207, p = .813, ; dismissing, F(2, 79) = .085, p = .919, ,; enmeshed, F(2, 79) = .833, p = .439, ; loved, F(2, 79) = 2.05, p = .127, ; no memory, F(2, 79) = 1.181, p = .312, ; rejection, F(2, 79) = 2.12, p = .127, ; and vulnerable, F(2, 79) = 2.74, p = .071, . There were also no significant differences between therapy conditions at baseline on the composite of GAD symptom outcome measures, F(1, 81) = 0.03, p = .864.
Table 1.
Correlations and Descriptive Statistics of Perceptions of Adult Attachment Questionnaire at Baseline
| Perception | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Reject | — | |||||||
| 2. Loved | 0.88* | — | ||||||
| 3. Enmesh | −0.24* | −0.35* | — | |||||
| 4. Vuln | 0.31* | 0.22* | 0.25* | — | ||||
| 5. Bal | −0.13 | −0.14 | 0.25* | −0.01 | — | |||
| 6. Angry | 0.59* | 0.55* | −0.05 | 0.55* | −0.03 | — | ||
| 7. Dis | 0.21 | 0.21 | −0.21 | −0.10 | −0.17 | 0.26* | — | |
| 8. Mem | 0.28* | 0.32* | −0.10 | 0.10 | −0.17 | 0.17 | 0.38* | — |
| M | 2.19 | 3.25 | 2.39 | 3.00 | 3.66 | 2.45 | 2.53 | 2.87 |
| SD | 0.94 | 0.92 | 0.69 | 0.92 | 0.59 | 1.00 | 0.72 | 1.25 |
| Range | 1.0−4.3 | 1.3−4.7 | 1.0−4.6 | 1.2−4.6 | 2.3−4.9 | 1.0−4.4 | 1.0−4.3 | 1.0−5.0 |
Note. Reject = rejection/neglect; Enmesh = role-reversal/enmeshment; Vuln = vulnerable; Bal = balancing/forgiving; Dis = dismissing/derogating; Mem = no memory.
p < .05.
Pre-Post Attachment Moderation
In the full model for the moderating effect of baseline attachment style on pre-post change in GAD symptoms, the two strongest effects were for dismissing and angry PAAQ subscales. Due to multicollinearity, all other effects were removed and the model was reanalyzed (see planned analyses). Because dismissing and angry subscales were present in the same model, results associated with the dismissing subscale controlled for effects of the angry subscale, and results for the angry subscale controlled for effects of the dismissing subscale.
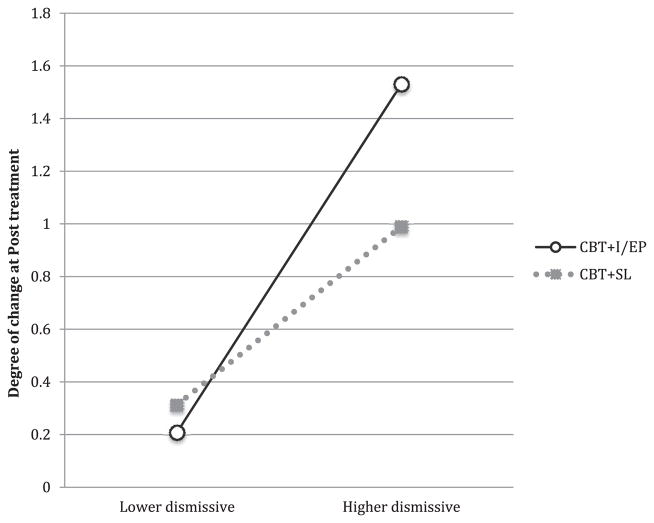
There was a three-way interaction among the dismissing subscale, time, and condition (B = −0.013, SE = 0.007, t(83) = −2.06, p = .043, d = −0.32; see Figure 1). The slopes of change demonstrated significant differences between the two treatments with dismissing predicting greater change in GAD symptoms from CBT + I/EP than from CBT + SL (ΔB = 0.014, χ2 = 4.64, p = .031, d = 0.49). According to the simple slopes, whereas greater levels of dismissing predicted greater change in response to CBT + I/EP (B = −0.011, χ2 = 6.07, p = .027, d = −0.56), levels of dismissing did not predict change from CBT + SL (B = 0.002, χ2 = 0.30, p = .584, d = 0.12). Thus as scores on the dismissing subscale increased, those receiving CBT + I/EP had significantly better outcomes at-post treatment, however levels of dismissing did not predict outcome from CBT + SL.
Figure 1.
This graph depicts the interaction between time, condition, and dismissing attachment level when predicting change in generalized anxiety disorder (GAD) symptoms between pretreatment and posttreatment. Higher scores reflect more change at posttreatment. The change scores were produced using model estimates for pre- and posttreatment in each of the conditions. CBT+I/EP = cognitive behavioral therapy plus interpersonal emotional processing; CBT+SL = cognitive behavioral therapy plus supportive listening.
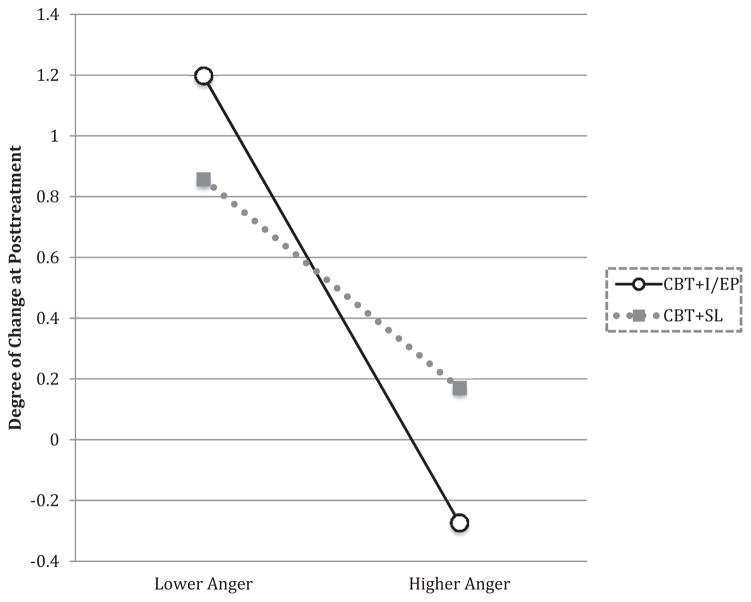
There was also a significant three-way interaction among the angry subscale, time, and condition (B = .010, SE = 0.004, t(83) = 2.48, p = .015, d = .38; see Figure 2). The slopes of change demonstrated significant differences between the two treatments, with the angry subscale predicting less change from CBT + I/EP than from CBT + SL (ΔB = −0.009, χ2 = 6.50, p = .010, d = −0.58). Within the simple slopes, dimensionally higher anger predicted marginally less change from CBT + I/EP (B = 0.005, χ2 = 3.93, p = .094, d = 0.44), however, anger did not significantly predict change from CBT + SL (B = −0.004, χ2 = 2.63, p = .107, d = −0.36). Thus, as attachment-related anger increased, those in CBT + I/EP had worse outcomes at posttreatment; however, anger did not predict change in response to CBT + SL.
Figure 2.
This graph depicts the interaction between time, condition, and anger when predicting change in generalized anxiety disorder (GAD) symptoms between pretreatment and posttreatment. Higher scores reflect more change. The change scores were produced using model estimates for pretreatment and posttreatment in each of the conditions. CBT+I/EP = cognitive behavioral therapy plus interpersonal emotional processing; CBT+SL = cognitive behavioral therapy plus supportive listening.
Pre-Follow-Up Attachment Moderation
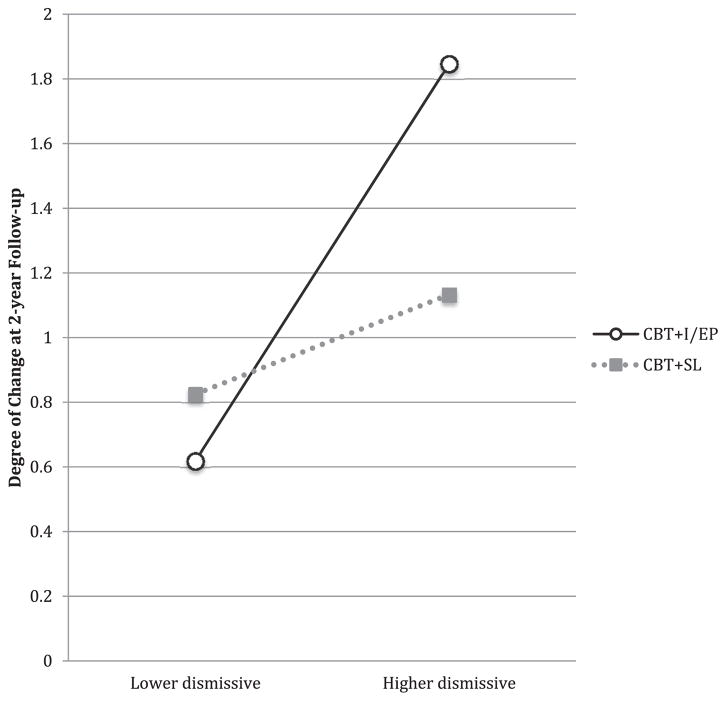
At 2-year follow-up, the dismissing and no memory subscales had the two strongest effects in the full model. All other variables were removed for the parsimonious model to follow. Because dismissing and no memory subscales were present in the same model, results of the dismissing subscale controlled for the effects of no memory, and results of the no memory subscale controlled for the effects of dismissing. There was a significant main effect of time (B = −0.054, SE = 0.026, t(83) = −2.09, p = .040, d = −0.32), showing that as more time elapsed during the follow-up period, participants tended to decrease further in their GAD symptoms. There was also a three-way interaction between the dismissing subscale, time, and condition (B = −0.008, SE = 0.003, t(83) = −2.37, p = .020, d = −0.37; see Figure 3). Higher scores on the dismissing subscale predicted greater change in GAD symptoms from CBT + I/EP than from CBT + SL (ΔB = 0.008, χ2 = 5.63, p = .018, d = 0.54). The simple slopes showed that whereas higher scores on dismissing predicted greater change in response to CBT + I/EP (B = −0.005, χ2 = 5.47, p = .038, d = −0.53), scores on the dismissing subscale failed to predict change from CBT + SL (B = 0.002, χ2 = 0.81, p = .369, d = 0.20). As with prepost effects, as scores on the dismissing subscale increased there was greater change from pretreatment to follow-up in those receiving CBT + I/EP, whereas there was no significant relationship between the dismissing subscale and change in GAD symptoms in response to CBT + SL.
Figure 3.
This graph depicts the interaction between time, condition, and dismissing when predicting change in generalized anxiety disorder (GAD) symptoms between pretreatment and 2-year follow-up. Higher scores reflect more change at 2-year follow-up. The change scores were produced using model estimates for pre- and posttreatment in each of the conditions. CBT + I/EP = cognitive behavioral therapy plus interpersonal emotional processing; CBT + SL = cognitive behavioral therapy plus supportive listening.
The main effect of no memory was not significant (B = −0.024, SE = 0.020, t(83) = −1.20, p = .233, d = −0.19), the interaction of no memory and time was not significant (B = −0.001, SE = 0.001, t(83) = −0.77, p = .443, d = −0.12), and the interaction among time, condition, and no memory was not significant (B =0.003, SE = 0.002, t(83) = 1.45, p = .152, d = 0.22). These results suggest that there was no impact of no memory on follow-up outcomes.2
Discussion
The goal of this study was to examine cognitive-affective styles related to insecure attachment as moderators of treatment outcome at postassessment, 6-month, 1-year, and 2-year follow-up. Consistent with our prediction, at all assessments relatively higher levels of avoidance, as measured by self-reported dismissing states of mind with respect to current attachment figures, predicted more change in GAD symptoms for those who received CBT + I/EP (and lower levels of dismissing styles were associated with less change from CBT + I/EP), whereas dismissing was unrelated to symptom change in CBT + SL at any assessment. Higher anxiety, as measured by self-reported angry states of mind with respect to current attachment figures was associated with less change in GAD symptoms at posttreatment in CBT + I/EP, but was unrelated to symptom change for those in CBT + SL. However, pretreatment anger failed to moderate outcome at 2-year follow-up and therefore, any moderation effects were more short-lived than the ones for dismissing styles. Interestingly, these short term effects were also in contrast with the main effect of time found in the pre-follow-up analyses, which revealed that greater time between the end of treatment and follow-up assessment was associated with greater symptom reductions in both treatment groups. These effects also contrasted with the marginally significant interaction between anger and time showing that higher levels of baseline anger predicted follow-up change in both treatments. Thus, in the long run, higher anger predicted benefits from both treatments. Even though we used a measure that has not been used much in the attachment literature, it is also important to note that of the seven subscales of the PAAQ, the most robust results came from the dismissing and angry subscales, which map onto the dimensions most often assessed in other self-report measures of attachment. These two subscales also load onto the PAAQ superordinate dimension that assesses current (adult) attachment to the caregiver, which may be closest in nature to the attachment bond that may be activated within the therapeutic relationship (compared with adult models of childhood attachment or adult models of romantic relationships).
Our findings that CBT + I/EP enhanced treatment for GAD individuals higher in dismissing states of mind is distinguished from several prior findings suggesting that avoidant attachment, which is characterized by a dismissing style, is associated with less response to treatment in general. For example, in university students with mixed diagnoses treated with interpersonal, cognitive– behavioral, psychodynamic, or eclectic therapies, avoidant attachment predicted poor outcome (Byrd et al., 2010). Similarly, Horowitz and colleagues (1993) found that patients with mixed diagnoses and avoidant attachment treated with brief psychodynamic therapy fared least well compared with other attachment styles. A slight variation of this result was obtained by Tasca and colleagues (2004) who found that whereas avoidant attachment predicted dropping out of group cognitive– behavioral therapy for eating disorders, it did not predict dropping out of group psychodynamic-interpersonal treatment.
In contrast to these prior studies (which either did not examine differential prediction across various treatment approaches or compared two entirely different treatments), we examined attachment style as a moderator of treatment within an additive design. Our findings suggested that adding techniques developed in humanistic, interpersonal, and psychodynamic treatments to CBT could improve its efficacy for clients with GAD who were higher on avoidance. By addressing emotional avoidance and interpersonal difficulties (i.e., excessive autonomy) characterizing GAD individuals with higher levels of dismissing styles, the interventions used in I/EP (emotional deepening, exploration of past and current relationship, repair of alliance ruptures) appear to have bolstered CBT’s ability to reduce symptoms for these individuals. It is also possible that the very structured 2-hr format (requiring 1 hr of intensive focus on CBT, followed by 1 hr exclusively devoted to emotional processing and interpersonal processes) may have contributed to our greater success with these individuals. Perhaps individuals who tend to be emotionally and interpersonally avoidant might do best with a structured and intense treatment protocol that specifically and systematically focuses on emotion and relationship issues, including with the therapist. Although higher levels of dismissiveness dimensionally predicted greater change from CBT + I/EP than from CBT + SL, adding I/EP to CBT does not appear to confer any additional benefit for those relatively lower in avoidant and dismissing attachment for whom CBT + SL worked at least as well.
The process by which I/EP might have had a specific complementary and additive effect on the CBT protocol may be exemplified by an intense qualitative analysis that was conducted for one client who received CBT + I/EP in the present trial (Castonguay et al., 2012). Consistent with findings of the present study, whereas the client successfully responded to therapy (in terms of GAD symptom reduction at the end of treatment and follow-up), his pretreatment self-reported dismissing attachment score (4.25) was a little less than twice the average of study participants (2.53; SD = 0.72). The client was a 50-year-old Caucasian male experiencing high levels of GAD symptoms, as well as work-related stress and marital conflict. He reported a long history of interpersonal problems, including physical abuse from his father and lack of protection from his mother, as well as a traumatic divorce (involving the removal of his children from his care). He viewed his current marital problems to be a result of conflicts between his needs and those of his wife. He admitted to feeling distrust toward women in general. Whereas the logical analysis and skill-oriented focus of CBT appeared to fit with the client’s problem-solving approach as a scientist, the I/EP segment raised considerable concerns for him. Immediately upon presentation of the I/EP rationale (in the first session), he stated that showing emotions would be painful because of previously hurtful experiences and that it would be uncomfortable for him to talk about feelings that might emerge in the relationship with the therapist. And although he showed progressive involvement in and benefits from CBT, he displayed repeated reluctance toward being engaged in I/EP tasks (e.g., expressing his feelings toward his wife). These clear signs of alliance rupture were systematically addressed during the I/EP segment when the therapist disclosed to him the frustrating impact that he had on her when he repeatedly avoided her questions about emotion and anything else related to the I/EP treatment focus. The client recognized that he was indeed evading her questions as a way to control the therapy, and that he was doing this in order to avoid being emotionally vulnerable. Using a skillful balance of challenge and support (as described by Linehan, 1993), the therapist then fostered a corrective experience “by exploring (in an emotionally immediate way) his fear of being criticized and his need for control, while neither controlling nor criticizing him—and in fact, doing quite the opposite” (Castonguay et al., p. 266). During this and subsequent sessions, the therapist’s use of metacommunication (including her contribution to relationship strains), exploratory (e.g., drawing connections between what was taking place in the session and the client’s interactions with others), and experiential (e.g., two-chair exercise) interventions led to a number of meaningful changes, including experiencing in the here-and-now emotions related to needs and fears toward the therapist and others, recognition of similar maladaptive and unfulfilling patterns of behaviors with others (where being emotionally distant and controlling neither prevented him from being hurt nor allowed him to get what he wanted), and exploration of developmental issues related to his interpersonal fears and behaviors. The continued exploration of alliance ruptures and their resolution, as well as reinforcement of new ways of being and interacting with the therapist in the session (open to experience, emotionally present) also served as a stepping stone to help the client to engage in genuine (as opposed to controlling) and emotionally vulnerable ways with both his wife and a close friend. Similar to what happened during therapy, these new ways of relating with important others appeared to have led to increased fulfillment of his interpersonal needs (acceptance and affirmation) and likely contributed to reduced interpersonal anxiety and worries. (See Castonguay et al., 2012 and Newman et al., 2004 for more details about technical and relational interventions used by therapists in both CBT and I/EP, as well as complementary and synergistic aspects of the client engagement [emotional, cognitive, behavioral, and interpersonal] and change in the each of these segments.)
In line with our tentative prediction, findings also indicated that clients with higher levels of anger showed higher levels of symptoms at posttreatment in CBT + I/EP than in CBT + SL. This result, however, should be considered with caution since the two treatments failed to differ at any follow-up assessment. In fact, as noted earlier, higher baseline angry attachment marginally predicted greater change from both treatments at follow-up. Thus, whereas the addition of I/EP techniques did not appear to improve the efficacy of CBT for GAD for clients with higher levels of anger, it may not have been detrimental either—at least in the long run. Our tentative prediction was based on the concern that an exploration of emotion (particularly anger) in those who were higher in emotional reactivity might make things worse in I/EP. Assuming that this concern was valid, it may be that therapists did not always focus extensively or systematically on anger with clients who had higher levels of anger toward current attachment figures. If this was the case, then it makes sense that level of angry attachment did not moderate long-term outcome. Interestingly, this is what was observed in the client described in the case reported above who, in addition to a high level of dismissing attachment, showed a high level of angry attachment at pretreatment. Early in the I/EP segment, for example, the client stated that in addition to “stuffing away” his painful feelings, he also coped with stress by reacting in an impulsive and hostile manner. Later in therapy, he described being angry with others most of the time and expecting others to be angry at him. In these instances, the therapist did not attempt to deepen the client’s hostile feelings. Rather, she and the client focused on the impact that his anger and deception had on others (including the therapist), a developmental source of his anger, and new ways he could relate to others in order to fulfill his interpersonal needs. Afterward, the client took a risk and disclosed to a close friend his feeling of being rejected by him, which contrary to his fear of being criticized, led to a strengthening of their relationship. In light of the manner that hostility was addressed with this successful case, and because the angry subscale did not discriminate the two treatments (and was associated with marginally greater change from both treatments at follow-up), we would suggest that CBT + I/EP is likely to be an effective treatment with individuals with both avoidant and anxious attachment.
Several limitations of this study should be mentioned. First, on average, those who received CBT + SL had higher pretreatment levels of angry attachment, which may have impacted our results. On the one hand, we have some confidence in the moderator findings for this variable because the outcome measure for this analysis (GAD symptoms) showed no pretreatment differences across treatment conditions. On the other hand, it is possible that fewer participants with angry attachment in CBT + I/EP led to the posttreatment findings, which did not hold up at follow-up. However, this possibility seems to be offset by the finding that higher levels of angry attachment styles predicted greater gains during follow-up across both treatments. Another limitation is that other attachment measures have been more widely used than the PAAQ. At the same time, the most robust effects in the current study were found with the dismissing and angry dimensions, which are most commonly assessed in other self-report measures. Furthermore, the internal consistency of the dismissing subscale was less than optimal. Nonetheless, the retest reliability of this subscale was very good and it is also important that its moderation of outcome was replicated across all time-points. Also, although we examined the data dimensionally, the significance of the analyses relied on relative extremes in our data and it is unclear whether these results will replicate across different samples. Further, study participants were mostly White and a large proportion had some college education. It is unclear therefore, whether our results would generalize to other groups.
Future studies should of course be conducted to replicate this study to increase our confidence in the moderating effects that we obtained. At this point in time, however, the moderating impact does suggest that not all but some GAD clients may benefit from interpersonal and emotional processing treatment aimed at improving the efficacy of CBT. Considering that CBT has been shown to be highly effective for about 50% of GAD clients who receive it (Borkovec & Ruscio, 2001), finding out who will benefit from “pure” CBT and who may require additional interventions may be preferable to searching for one treatment (integrative or not) that is better than CBT across GAD clients.
What is the public health significance of this article?
When choosing a treatment for individuals with generalized anxiety disorder, this study suggests the potential importance of taking adult attachment into account.
Acknowledgments
A National Institute of Mental Health Research Grant RO1 MH58593-02 supported this study. We thank Thomas D. Borkovec for his crucial collaboration on the original RCT.
Footnotes
Numerous terms are used in the attachment literature depending on the ages of individuals studied and methods for assessing attachment. For readability, we adopt Brennan’s (Brennan et al., 1998) dimensional model of adult attachment and use the terms avoidance (or avoidant) and anxiety (or anxious). These map onto categorical patterns of insecure attachment and are functionally equivalent across development (Fraley & Spieker, 2003; Fraley & Shaver, 2000). Avoidant and anxious dimensions respectively also map onto the dismissing and angry current states of mind subscales of the Perceptions of Adult Attachment Questionnaire (PAAQ) used in this study. Thus, we use the terms dismissing (or dismissiveness) and angry (or anger) to refer to the analogous current states of mind assessed dimensionally in the current study.
Note that because the angry subscale was included in the prepost model, we also tested a model with anger and dismissing in the pre-follow-up model (in addition to the model with dismissing and no memory). As in the other pre-follow-up model, there was a significant three-way interaction between dismissing, time, and condition (B = −0.007, SE = 0.002, t(83) = −3.01, p = .003, d = −0.47). Each of the simple slopes and the contrasts between the slopes showed identical patterns to when the no memory subscale was included (rather than the angry subscale) in the pre-follow-up model (see text for the results). There was, however, a marginally significant interaction between anger and time (B = 0.002, SE = 0.001, t(83) = −1.79, p = .077, d = 0.28), suggesting that higher anger predicted marginally more change across both treatments as more time elapsed during the 2-year follow-up. The interaction among time, condition, and anger was not significant (B = 0.001, SE = 0.001, t(83) = 0.83, p = .407, d = 0.12), suggesting that anger failed to predict differential outcomes across the two treatments at follow-up. Also, controlling for anger in the model did not change the effect of the dismissing subscale on outcome at follow-up.
References
- Afifi TO, Cox BJ, Enns MW. Mental health profiles among married, never-married, and separated/divorced mothers in a nationally representative sample. Social Psychiatry and Psychiatric Epidemiology. 2006;41:122–129. doi: 10.1007/s00127-005-0005-3. http://dx.doi.org/10.1007/s00127-005-0005-3. [DOI] [PubMed] [Google Scholar]
- Ainsworth BE, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Lawrence Erlbaum; 1978. [Google Scholar]
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. http://dx.doi.org/10.1207/s15327752jpa5503&4_10. [DOI] [PubMed] [Google Scholar]
- Behar ES, Borkovec TD. Psychotherapy outcome research. In: Schinka JA, Velicer WF, editors. Handbook of psychology: Research methods in psychology. Vol. 2. New York: Wiley; 2003. pp. 213–240. http://dx.doi.org/10.1002/0471264385.wei0209. [Google Scholar]
- Berant E, Mikulincer M, Shaver PR. Mothers’ attachment style, their mental health, and their children’s emotional vulnerabilities: A 7-year study of children with congenital heart disease. Journal of Personality. 2008;76:31–65. doi: 10.1111/j.1467-6494.2007.00479.x. http://dx.doi.org/10.1111/j.1467-6494.2007.00479.x. [DOI] [PubMed] [Google Scholar]
- Bifulco A, Kwon J, Jacobs C, Moran PM, Bunn A, Beer N. Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Social Psychiatry and Psychiatric Epidemiology. 2006;41:796–805. doi: 10.1007/s00127-006-0101-z. http://dx.doi.org/10.1007/s00127-006-0101-z. [DOI] [PubMed] [Google Scholar]
- Birnbaum GE, Orr I, Mikulincer M, Florian V. When marriage breaks up: Does attachment style contribute to coping and mental health? Journal of Social and Personal Relationships. 1997;14:643–654. http://dx.doi.org/10.1177/0265407597145004. [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. http://dx.doi.org/10.1037/0022-006X.70.2.288. [PubMed] [Google Scholar]
- Borkovec TD, Ruscio AM. Psychotherapy for generalized anxiety disorder. The Journal of Clinical Psychiatry. 2001;62(Suppl 11):37–42. [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 1. Attachment. Vol. 2. New York: Basic Books; 1969. [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 2. Separation. New York: Basic Books; 1973. [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. New York: Guilford Press; 1998. pp. 46–76. [Google Scholar]
- Brown AM, Whiteside SP. Relations among perceived parental rearing behaviors, attachment style, and worry in anxious children. Journal of Anxiety Disorders. 2008;22:263–272. doi: 10.1016/j.janxdis.2007.02.002. http://dx.doi.org/10.1016/j.janxdis.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM–IV. New York: Oxford University Press; 1994. [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM–IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. http://dx.doi.org/10.1037/0021-843X.110.1.49. [DOI] [PubMed] [Google Scholar]
- Byrd KR, Patterson CL, Turchik JA. Working alliance as a mediator of client attachment dimensions and psychotherapy outcome. Psychotherapy: Theory, Research, & Practice. 2010;47:631–636. doi: 10.1037/a0022080. http://dx.doi.org/10.1037/a0022080. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Berlin LJ. The insecure/ambivalent pattern of attachment: Theory and research. Child Development. 1994;65:971–991. http://dx.doi.org/10.2307/1131298. [PubMed] [Google Scholar]
- Cassidy J, Lichtenstein-Phelps J, Sibrava NJ, Thomas CL, Jr, Borkovec TD. Generalized anxiety disorder: Connections with self-reported attachment. Behavior Therapy. 2009;40:23–38. doi: 10.1016/j.beth.2007.12.004. http://dx.doi.org/10.1016/j.beth.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Nelson DL, Boswell JF, Nordberg SS, McAleavey AA, Newman MG, Borkovec TD. Corrective experiences in cognitive behavior and interpersonal–emotional processing therapies: A qualitative analysis of a single case. In: Castonguay LG, Hill CE, editors. Transformation in psychotherapy: Corrective experiences across cognitive behavioral, humanistic, and psychodynamic approaches. Washington, DC: American Psychological Association; 2012. pp. 245–279. http://dx.doi.org/10.1037/13747-013. [Google Scholar]
- Davis D, Shaver PR, Vernon ML. Physical, emotional, and behavioral reactions to breaking up: The roles of gender, age, emotional involvement, and attachment style. Personality and Social Psychology Bulletin. 2003;29:871–884. doi: 10.1177/0146167203029007006. http://dx.doi.org/10.1177/0146167203029007006. [DOI] [PubMed] [Google Scholar]
- Dozier M. Attachment organization and treatment use for adults with serious psychopathological disorders. Development and Psychopathology. 1990;2:47–60. http://dx.doi.org/10.1017/S0954579400000584. [Google Scholar]
- Dozier M, Cue KL, Barnett L. Clinicians as caregivers: Role of attachment organization in treatment. Journal of Consulting and Clinical Psychology. 1994;62:793–800. doi: 10.1037//0022-006x.62.4.793. http://dx.doi.org/10.1037/0022-006X.62.4.793. [DOI] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. http://dx.doi.org/10.1037/1082-989X.1.2.170. [Google Scholar]
- Dunst CJ, Hamby DW, Trivette CM. Guidelines for calculating effect sizes for practice-based research syntheses. Centerscope. 2004;3:1–10. [Google Scholar]
- Erickson TM, Newman MG. Interpersonal and emotional processes in generalized anxiety disorder analogues during social interaction tasks. Behavior Therapy. 2007;38:364–377. doi: 10.1016/j.beth.2006.10.005. http://dx.doi.org/10.1016/j.beth.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Feeney JA. Adult attachment and emotional control. Personal Relationships. 1995;2:143–159. http://dx.doi.org/10.1111/j.1475-6811.1995.tb00082.x. [Google Scholar]
- Feeney JA, Noller P. Attachment style as a predictor of adult romantic relationships. Journal of Personality and Social Psychology. 1990;58:281–291. http://dx.doi.org/10.1037/0022-3514.58.2.281. [Google Scholar]
- Fraley RC, Shaver PR. Adult romantic attachment: Theoretical developments, emerging controversies, and unanswered questions. Review of General Psychology. 2000;4:132–154. http://dx.doi.org/10.1037/1089-2680.4.2.132. [Google Scholar]
- Fraley RC, Spieker SJ. Are infant attachment patterns continuously or categorically distributed? A taxometric analysis of strange situation behavior. Developmental Psychology. 2003;39:387–404. doi: 10.1037/0012-1649.39.3.387. http://dx.doi.org/10.1037/0012-1649.39.3.387. [DOI] [PubMed] [Google Scholar]
- Fraley RC, Waller NG. Adult attachment patterns: A test of the typological model. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. New York: Guilford Press; 1998. pp. 77–114. [Google Scholar]
- George C, Kaplan N, Main M. The Berkeley Adult Attachment Interview. Department of Psychology, University of California; Berkeley: 1985/1996. Unpublished manuscript. [Google Scholar]
- Greenberg LS. Emotion-focused therapy: Coaching clients to work through their feelings. Washington, DC: American Psychological Association; 2002. http://dx.doi.org/10.1037/10447-000. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. The British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. http://dx.doi.org/10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hazan C, Shaver PR. Attachment as an organizational framework for research on close relationships. Psychological Inquiry. 1994;5:1–22. http://dx.doi.org/10.1207/s15327965pli0501_1. [Google Scholar]
- Horowitz LM, Inouye D, Siegelman EY. On averaging judges’ ratings to increase their correlation with an external criterion. Journal of Consulting and Clinical Psychology. 1979;47:453–458. doi: 10.1037//0022-006x.47.3.453. http://dx.doi.org/10.1037/0022-006X.47.3.453. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Bartholomew K. Interpersonal problems, attachment styles, and outcome in brief dynamic psychotherapy. Journal of Consulting and Clinical Psychology. 1993;61:549–560. doi: 10.1037//0022-006x.61.4.549. http://dx.doi.org/10.1037/0022-006X.61.4.549. [DOI] [PubMed] [Google Scholar]
- Kobak RR, Sceery A. Attachment in late adolescence: Working models, affect regulation, and representations of self and others. Child Development. 1988;59:135–146. doi: 10.1111/j.1467-8624.1988.tb03201.x. http://dx.doi.org/10.2307/1130395. [DOI] [PubMed] [Google Scholar]
- Lavy S, Mikulincer M, Shaver PR. Autonomy–proximity imbalance: An attachment theory perspective on intrusiveness in romantic relationships. Personality and Individual Differences. 2010;48:552–556. http://dx.doi.org/10.1016/j.paid.2009.12.004. [Google Scholar]
- Lichtenstein J, Cassidy J. The Inventory of Adult Attachment: Validation of a new measure. Paper presented at the annual meeting of the Society for Research in Child Development; Seattle, WA. 1991. Mar, [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Llera SJ, Newman MG. Effects of worry on physiological and subjective reactivity to emotional stimuli in generalized anxiety disorder and nonanxious control participants. Emotion. 2010;10:640–650. doi: 10.1037/a0019351. http://dx.doi.org/10.1037/a0019351. [DOI] [PubMed] [Google Scholar]
- Llera SJ, Newman MG. Rethinking the role of worry in generalized anxiety disorder: Evidence supporting a model of emotional contrast avoidance. Behavior Therapy. 2014;45:283–299. doi: 10.1016/j.beth.2013.12.011. http://dx.doi.org/10.1016/j.beth.2013.12.011. [DOI] [PubMed] [Google Scholar]
- Main M, Goldwyn R. Adult attachment scoring and classification system. Department of Psychology, University of California; Berkeley: 1998. Unpublished manuscript. [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Applying an emotion regulation framework to integrative approaches to generalized anxiety disorder. Clinical Psychology: Science and Practice. 2002;9:85–90. http://dx.doi.org/10.1093/clipsy.9.1.85. [Google Scholar]
- Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behavior Therapy. 2007;38:284–302. doi: 10.1016/j.beth.2006.09.001. http://dx.doi.org/10.1016/j.beth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. http://dx.doi.org/10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mickelson KD, Kessler RC, Shaver PR. Adult attachment in a nationally representative sample. Journal of Personality and Social Psychology. 1997;73:1092–1106. doi: 10.1037//0022-3514.73.5.1092. http://dx.doi.org/10.1037/0022-3514.73.5.1092. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Florian V. Appraisal of and coping with a real-life stressful situation: The contribution of attachment styles. Personality and Social Psychology Bulletin. 1995;21:406–414. http://dx.doi.org/10.1177/0146167295214011. [Google Scholar]
- Mikulincer M, Orbach I. Attachment styles and repressive defensiveness: The accessibility and architecture of affective memories. Journal of Personality and Social Psychology. 1995;68:917–925. doi: 10.1037//0022-3514.68.5.917. http://dx.doi.org/10.1037/0022-3514.68.5.917. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. Adult attachment and affect regulation. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 2. New York: Guilford Press; 2008. pp. 503–531. [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: Wiley; 1994. pp. 265–283. [Google Scholar]
- Moutsiana C, Johnstone T, Murray L, Fearon P, Cooper PJ, Pliatsikas C, … Halligan SL. Insecure attachment during infancy predicts greater amygdala volumes in early adulthood. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2015;56:540–548. doi: 10.1111/jcpp.12317. http://dx.doi.org/10.1111/jcpp.12317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundry R, Nunn CL. Stepwise model fitting and statistical inference: Turning noise into signal pollution. American Naturalist. 2009;173:119–123. doi: 10.1086/593303. http://dx.doi.org/10.1086/593303. [DOI] [PubMed] [Google Scholar]
- Muris P, Mayer B, Meesters C. Self-reported attachment style, anxiety, and depression in children. Social Behavior and Personality. 2000;28:157–162. http://dx.doi.org/10.2224/sbp.2000.28.2.157. [Google Scholar]
- Muris P, Meesters C, Merckelbach H, Hülsenbeck P. Worry in children is related to perceived parental rearing and attachment. Behaviour Research and Therapy. 2000;38:487–497. doi: 10.1016/s0005-7967(99)00072-8. http://dx.doi.org/10.1016/S0005-7967(99)00072-8. [DOI] [PubMed] [Google Scholar]
- Muris P, Meesters C, van Melick M, Zwambag L. Self-reported attachment style, attachment quality, and symptoms of anxiety and depression in young adolescents. Personality and Individual Differences. 2001;30:809–818. http://dx.doi.org/10.1016/S0191-8869(00)00074-X. [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Boswell JF, Szkodny LE, Nordberg SS. A randomized controlled trial of cognitive-behavioral therapy for generalized anxiety disorder with integrated techniques from emotion-focused and interpersonal therapies. Journal of Consulting and Clinical Psychology. 2011;79:171–181. doi: 10.1037/a0022489. http://dx.doi.org/10.1037/a0022489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Nordberg SS. An open trial of integrative therapy for generalized anxiety disorder. Psychotherapy: Theory, Research, & Practice. 2008;45:135–147. doi: 10.1037/0033-3204.45.2.135. http://dx.doi.org/10.1037/0033-3204.45.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Molnar C. Integrative psychotherapy. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guilford Press; 2004. pp. 320–350. [Google Scholar]
- Newman MG, Erickson TM. Generalized anxiety disorder. In: Beck JG, editor. Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment. Washington, DC: American Psychological Association; 2010. pp. 235–259. http://dx.doi.org/10.1037/12084-009. [Google Scholar]
- Newman MG, Llera SJ. A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry. Clinical Psychology Review. 2011;31:371–382. doi: 10.1016/j.cpr.2011.01.008. http://dx.doi.org/10.1016/j.cpr.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, Castonguay LG. Worry and generalized anxiety disorder: A review and theoretical synthesis of research on nature, etiology, and treatment. Annual Review of Clinical Psychology. 2013;9:275–297. doi: 10.1146/annurev-clinpsy-050212-185544. http://dx.doi.org/10.1146/annurev-clinpsy-050212-185544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priest JB. Anxiety disorders and the quality of relationships with friends, relatives, and romantic partners. Journal of Clinical Psychology. 2013;69:78–88. doi: 10.1002/jclp.21925. http://dx.doi.org/10.1002/jclp.21925. [DOI] [PubMed] [Google Scholar]
- Przeworski A, Newman MG, Pincus AL, Kasoff MB, Yamasaki AS, Castonguay LG, Berlin KS. Interpersonal pathoplasticity in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2011;120:286–298. doi: 10.1037/a0023334. http://dx.doi.org/10.1037/a0023334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario-Martinez H. Phia: Post-hoc interaction analysis. R package version 0.1–3. 2013 Retrieved from http://CRAN.R-project.org/packagephia.
- Safran JD, Segal ZV. Interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]
- Sbarra DA. Predicting the onset of emotional recovery following nonmarital relationship dissolution: Survival analyses of sadness and anger. Personality and Social Psychology Bulletin. 2006;32:298–312. doi: 10.1177/0146167205280913. http://dx.doi.org/10.1177/0146167205280913. [DOI] [PubMed] [Google Scholar]
- Skourteli MC, Lennie C. The therapeutic relationship from an attachment theory perspective. Counselling Psychology Review. 2011;26:20–33. [Google Scholar]
- Tasca GA, Ritchie K, Conrad G, Balfour L, Gayton J, Lybanon V, Bissada H. Attachment scales predict outcome in a randomized controlled trial of two group therapies for binge eating disorder: An aptitude by treatment interaction. Psychotherapy Research. 2006;16:106–121. http://dx.doi.org/10.1080/10503300500090928. [Google Scholar]
- Tasca GA, Taylor D, Bissada H, Ritchie K, Balfour L. Attachment predicts treatment completion in an eating disorders partial hospital program among women with anorexia nervosa. Journal of Personality Assessment. 2004;83:201–212. doi: 10.1207/s15327752jpa8303_04. http://dx.doi.org/10.1207/s15327752jpa8303_04. [DOI] [PubMed] [Google Scholar]
- Turk CL, Heimberg RG, Luterek JA, Mennin DS, Fresco DM. Emotion dysregulation in generalized anxiety disorder: A comparison with social anxiety disorder. Cognitive Therapy and Research. 2005;5:89–106. http://dx.doi.org/10.1007/s10608-005-1651-1. [Google Scholar]
- Vogel DL, Wei M. Adult attachment and help-seeking intent: The mediating roles of psychological distress and perceived social support. Journal of Counseling Psychology. 2005;52:347–357. http://dx.doi.org/10.1037/0022-0167.52.3.347. [Google Scholar]
- Warren SL, Huston L, Egeland B, Sroufe LA. Child and adolescent anxiety disorders and early attachment. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:637–644. doi: 10.1097/00004583-199705000-00014. http://dx.doi.org/10.1097/00004583-199705000-00014. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: Does type of relationship matter? Journal of Abnormal Psychology. 2000;109:803–808. doi: 10.1037//0021-843x.109.4.803. http://dx.doi.org/10.1037/0021-843X.109.4.803. [DOI] [PubMed] [Google Scholar]
- Williams NL, Riskind JH. Cognitive vulnerability and attachment. Journal of Cognitive Psychotherapy. 2004;18:3–6. http://dx.doi.org/10.1891/jcop.18.1.3.28052. [Google Scholar]