Abstract
Background
The surgical approach chosen for total hip arthroplasty (THA) may affect the positioning of the acetabular component. The purpose of this study was to examine the accuracy in orienting the acetabular component using the modified Hardinge approach.
Methods
We used our institutional arthroplasty database to identify patients with primary, press-fit, hemispherical acetabular components of a metal-on-polyethylene THA performed between 2003 and 2011. Patients with radiographs obtained 1–3 years after the index procedure were included for measurement of anteversion and inclination angles. Acceptable values of anteversion and abduction angles were defined as 15° ± 10° and 40° ± 10°, respectively.
Results
We identified 1241 patients from the database, and the modified Hardinge approach was used in 1010 of the patients included in our analysis. The acetabular component was anteverted in the acceptable zone in 54.1% of patients. The abduction angle was within the defined range in 79.2% of patients. Combined anteversion and abduction angles within the defined zone were present in 43.6% of patients.
Conclusion
Consistent with studies examining accuracy from other approaches, our study reveals that the modified Hardinge approach was only moderately accurate in positioning the acetabular component in the acceptable zone.
Abstract
Contexte
La voie d’abord choisie pour une arthroplastie totale de la hanche (ATH) pourrait influer sur le positionnement du composant cotyloïdien. La présente étude portait sur la précision de l’orientation du composant dans les interventions empruntant la voie de Hardinge modifiée.
Méthodes
À partir de la base de données sur les arthroplasties de notre établissement, nous avons cherché puis retenu les patients ayant subi une ATH entre 2003 et 2011 et ayant alors reçu une première prothèse métal sur polyéthylène avec composant cotyloïdien hémisphérique ajusté à la presse. Nous avons inclus les patients ayant subi des radiographies de 1 à 3 ans après l’intervention afin de mesurer les angles d’antéversion et d’abduction. Les valeurs jugées acceptables étaient respectivement de 15° ± 10° et de 40° ± 10°.
Résultats
Nous avons retenu 1241 patients sélectionnés à partir de la base de données; la voie employée pour 1010 d’entre eux était la voie de Hardinge modifiée. L’angle d’antéversion du cotyle était dans les limites acceptables chez 54,1 % des patients, l’angle d’abduction se trouvait dans les limites définies dans 79,2 % des cas, et les valeurs cibles étaient respectées pour les 2 paramètres chez 43,6 % des patients.
Conclusion
Nous avons conclu que la précision du positionnement du composant cotyloïdien par la voie de Hardinge modifiée est tout au plus modérée, ce qui concorde avec d’autres études visant à évaluer la précision d’autres techniques.
Acetabular component positioning is paramount for successful total hip arthroplasty (THA). Poor cup positioning affects impingement,1–5 dislocation rates6–10 and edge loading11 and may lead to liner fractures.3 Studies have shown that excess abduction angle is correlated with increased bearing surface wear rates in metal-on-polyethylene and metal-on-metal articulations.12–15 In metal-on-metal hip resurfacing, Hart and colleagues16 showed increased blood metal ion levels in patients with insufficient cup version.16 However, acceptable cup position has been defined only in reference to dislocation rates, and its definition has been largely inconsistent in the literature. Lewinnek and colleagues6 defined a “safe zone” of 15° ± 10° of anteversion and inclination angle of 40° ± 10° based on 9 dislocations. Meanwhile, McCollum and Gray8 suggested the cup to be placed between 20° and 40° of anteversion based on 5 dislocations. Although Lewinnek’s “safe zone” is considered obsolete by many surgeons,17,18 it is often used in the literature to allow consistent comparison of outcomes.
Surgical approach may influence dislocation rates, postoperative function, heterotopic ossification and the possibility of neurovascular damage.19–24 The selection of surgical approach is largely a matter of preference based on prior training of the surgeon. Callanan and colleagues25 identified surgical approach to be an independent risk factor in cup malpositioning. They identified a 68% incidence of cup malpositioning with the use of the direct lateral approach compared with 42.7% when using the posterolateral approach. Barrack and colleagues26 reported only 21% of the cups positioned outside their defined range using the anterolateral approach. Both studies, however, used different acceptable ranges for the cup position, with an emphasis on the posterolateral approach as the most popular surgical approach at their centres. Furthermore, the lateral approaches were being performed by low-volume surgeons in both studies, making it difficult to determine the generalizability of the results.
The modified Hardinge approach is the most common surgical approach used at our institution for total hip replacements. This approach offers good visualization of the acetabulum, facilitating optimal cup positioning as well as excellent stability of the total hip joint. The purpose of this study was to evaluate the accuracy of intraoperative acetabular component positioning with use of the modified Hardinge approach performed by high-volume surgeons at a tertiary centre.
Methods
Ethics approval was obtained from our institutional review board. We used our institutional arthroplasty database to obtain information on patients who underwent THA between 2003 and 2011, including their age, sex, date of their precedure, laterality of the hip, implant information and surgical approach used for the procedure. All THAs were either executed under the guidance of or performed directly by fellowship-trained high-volume surgeons, each of whom perform more than 250 total joint replacements per year. Mean duration of employment of these surgeons was 23.3 ± 13.4 years.
The study cohort consisted of patients with a diagnosis of osteoarthritis who underwent a cementless THA with the use of the modified Hardinge approach. Patients were required to have digital postoperative radiographs collected prospectively, 24–36 months from their index procedure. We excluded patients for whom the surgical approach was not recorded in the database. We also excluded patients who had diagnoses of metastatic cancer, avascular necrosis, inflammatory arthritis, post-traumatic arthritis, acute fracture or developmental hip dysplasia; those who had metal-on-metal articulations or cemented acetabular components; and those who had undergone bipolar hemiarthroplasty, modular neck-stem implants and revision surgeries.
The acetabular components used in our cohort were all press fit, hemispherical shells, and included Reflection (Smith and Nephew), Duraloc (Depuy), R3 (Smith and Nephew), Pinnacle (Depuy) and Trident (Stryker) models.
The modified Hardinge approach has previously been detailed by Frndak and colleagues.27 Patients were positioned in a lateral decubitus position with supporting posts. A lateral skin incision centred over the greater trochanter was used. The access to the hip joint was gained through an abductor muscle split approach. The fibres of the gluteus medius were split longitudinally at the junction of the anterior third to posterior two-thirds of the muscle belly. The gluteus minimus and capsule were then divided vertically along the same incision parallel to the gluteus medius split. Surgeons were attentive to keep the vertical split within 5 cm proximal to the greater trochanter to avoid injury to the superior gluteal nerve. During preoperative templating and the implantation of the cup, surgeons aimed the operative inclination and anteversion angles of the acetabular component to be within the Lewinnek zone. A combination of anatomic landmarks and mechanical guides were used intraoperatively.
Anteroposterior (AP) and lateral radiographs were examined for the purposes of this study. Using the General Electric Centricity Picture Archiving and Communications System (PACS), we measured the radiographic inclination angle and anteversion. Radiographs were analyzed by 2 observers (P.G. and A.L.). A subset of 20 ragiographs was measured by both observers to calculate the concordance correlation coefficient and confirm adequate inter-observer reliability, which was consistently greater than 0.93. Differences were reconciled through mutual agreement. Anteversion was measured using the technique described by Tiberi and colleagues.28 Inclination angle was measured between the face of the acetabular component and the horizontal axis, drawn by connecting the ischial tuberosities.6,29,30
Statistical analysis
We performed statistical analyses using SPSS statistics software version 20 (IBM). Frequency analysis and χ2 tests were performed to determine the accuracy of the modified Hardinge approach at our institution. We performed a univariate analysis with 5 factors: age, sex, body mass index (BMI), head size and outer acetabular component diameter. Multivariate analysis was performed using logistic regression with the same 5 variables. We considered results to be significant at p < 0.05.
Results
A total of 1241 THAs were performed during the study period; of these 1010 patients met our selection criteria and were included in the study.
The mean anteversion was 21.8° ± 11.8°, and the mean inclination was 44.32° ± 7.0°. At the time of the procedure, the mean age of the study population was 71.5 ± 9.6 years. There were 595 women (59%) and 415 men (41%). The majority of the procedures (543 [53.7%]) were performed on the right hip. The average BMI was 29.6 ± 6.1. Only 1 dislocation was identified in the entire cohort.
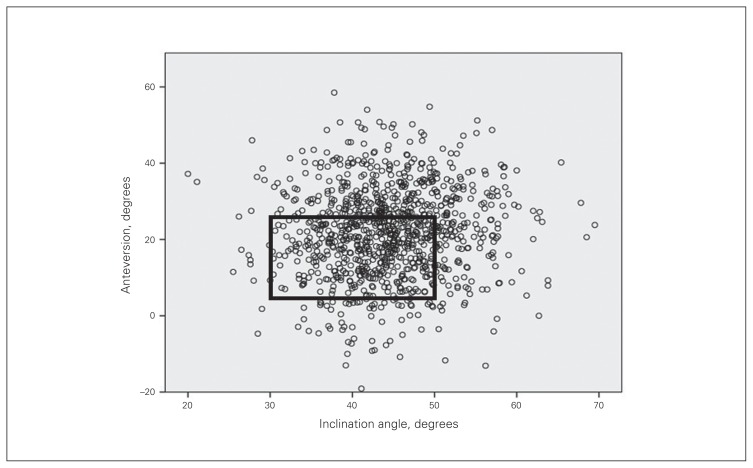
The accuracy of achieving the targeted cup position is reported in Table 1. Accuracy was best for inclination, with 79.2% of the hips meeting the target inclination angle. For anteversion, 54.1% of the hips had the cup in the intended range. Examining combined inclination and anteversion angles, 43.6% of the hips had the acetabular component within the target range. The position of acetabular components in all patients are graphically represented in Figure 1. We found that 47.5% of the hips were within 1 standard deviation of the mean of combined anteversion and inclination angle, while 90.5% were within 2 standard deviations of the mean (Table 2).
Table 1.
Comparison of cup positioning accuracy between different approaches, as demonstrated in previous studies
| Study; approach | No. of hips | Optimal range of inclination angle | Optimal range of anteversion | Components within both ranges, % |
|---|---|---|---|---|
| Callanan et al.25 | 1952 | 30°–45° | 5°–25° | |
|
| ||||
| Direct lateral | 50 | 32.0 | ||
|
| ||||
| Posterolateral | 1170 | 57.3 | ||
|
| ||||
| Anterolateral | 560 | 37.0 | ||
|
| ||||
| Barrack et al.26 | 1549 | 30°–55° | 5°–35° | |
|
| ||||
| Posterolateral | 898 | 88.0 | ||
|
| ||||
| Anterolateral | 154 | 79.0 | ||
|
| ||||
| Present study | 1010 | 30°–50° | 5°–25° | 43.6 |
| Modified Hardinge | ||||
Fig. 1.
Scatter diagram summary of the orientation of the acetabular components in our cohort. Data highlighted within the black box indicate the cups within the Lewinnek’s “safe zone.”
Table 2.
Distribution of the hips within described ranges of anteversion and inclination
| Distribution | Inclination angle | Anteversion | No. (%) of components within both ranges | ||
|---|---|---|---|---|---|
|
|
|
||||
| Range | No. (%) of components within range | Range | No. (%) of components within range | ||
| Total range | 20° to 70° | 1010 (100) | −19° to −59° | 1010 (100) | 100% |
|
| |||||
| Mean ± 1 SD | 37.4° to 51.3° | 705 (69.8) | 10.1° to −33.6° | 685 (67.8) | 480 (47.5) |
|
| |||||
| Mean ± 2 SD | 30.4° to 58.2° | 965 (95.5) | −1.7° to 45.4° | 958 (94.9) | 915 (90.6) |
SD = standard deviation.
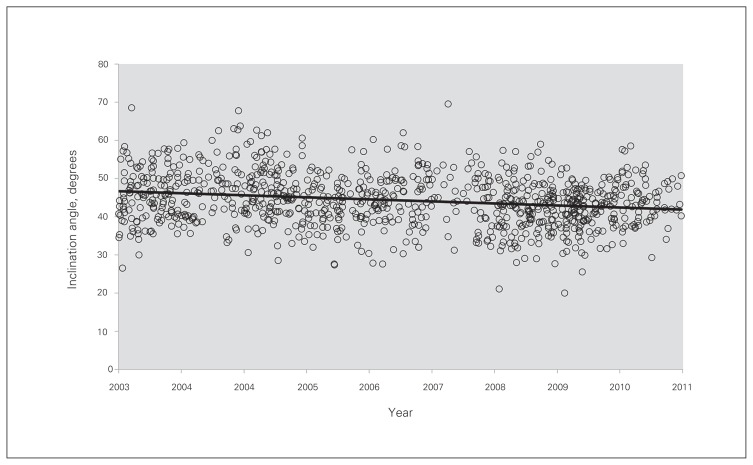
The results of the univariate analysis for age, sex, BMI, head size and outer acetabular component diameter are shown in Table 3. The BMI and sex of the patient had a significant effect on combined position of the acetabular component. Men were more likely than women to have a correctly oriented acetabular component (p < 0.001). Furthermore, patients with lower BMI were more likely to have an acetabular component with inaccurate anteversion and inclination angle (p = 0.020). When acetabular inclination angle was examined separately, sex (p < 0.001) and femoral head size (p < 0.001) had an effect on acetabular inclination. Women and patients with head sizes of 28 mm or smaller were more likely to have an inclination angle outside the target zone. Akin to the combined absolute cup position, anteversion was similarly affected by sex (p = 0.009) and BMI (p = 0.002). Figure 2 graphically illustrates a reduction in inclination angle over time (Spearman rho = −0.19, p < 0.001).
Table 3.
Univariate analysis of various factors for combined acetabular cup position within the Lewinnek’s “safe zone”
| Factor | No. (%) of hips | p value* | ||
|---|---|---|---|---|
| Total | Within Lewinnek’s zone | Outside Lewinnek’s zone | ||
| Age, yr (n = 1010) | 1010 | 440 (43.6) | 570 (56.4) | 0.33 |
| < 50 | 36 | 19 (52.8) | 17 (47.2) | |
| 50–69 | 359 | 148 (41.2) | 211 (58.8) | |
| ≥ 70 | 615 | 273 (44.4) | 342 (55.6) | |
| Sex (n = 1010) | < 0.001 | |||
| Male | 415 | 210 (50.6) | 205 (49.4) | |
| Female | 595 | 230 (38.7) | 365 (61.3) | |
| Body mass index (n = 965) | 0.020 | |||
| ≤ 24.99 | 214 | 71 (33.2) | 143 (66.8) | |
| 25–29.99 | 343 | 165 (48.1) | 178 (51.9) | |
| 30–34.99 | 247 | 111 (44.9) | 136 (55.1) | |
| 35–39.99 | 101 | 50 (49.5) | 51 (50.5) | |
| ≥ 40 | 60 | 20 (33.3) | 40 (66.7) | |
| Head size (n = 1009) | 0.32 | |||
| ≤ 28 mm | 291 | 118 (40.5) | 173 (59.5) | |
| 32 mm | 509 | 222 (43.6) | 287 (56.4) | |
| ≥ 36 mm | 209 | 99 (47.4) | 110 (52.6) | |
| Outer cup diameter (n = 1002) | 0.06 | |||
| < 52 mm | 44 | 16 (36.4) | 28 (63.6) | |
| 52–56 mm | 639 | 266 (41.6) | 373 (58.4) | |
| > 56 mm | 319 | 156 (48.9) | 163 (51.1) | |
χ2 test.
Fig. 2.
A temporal view of inclination angles of all hips from 2003 to 2011. R2 = 0.041, y = −0.0015x + 101.75
Multivariate analysis demonstrated that patients with a BMI between 25 and 40 were more likely to be have correct combined acetabular component position than those with a BMI lower than 25 or higher than 40 (Table 4). Sex, age, head size and outer acetabular diameter were not independent risk factors to cup malpositioning.
Table 4.
Multivariate analysis of factors for predicting accurate component position within Lewinnek’s zone (n = 958)
| Factor | Reference category | OR (95% CI) | p value |
|---|---|---|---|
| Body mass index | ≤ 24.99 | ||
| 25–29.99 | 1.78 (1.24–2.56) | 0.002 | |
| 30–34.99 | 1.53 (1.04–2.26) | 0.033 | |
| 35–39.99 | 2.07 (1.26–3.40) | 0.004 | |
| ≥ 40 | — | 0.87 | |
| Male sex | Female | 1.40 (1.00 – 1.95) | 0.05 |
| Age, yr | ≤ 50 | ||
| 50–70 | — | 0.36 | |
| ≥ 70 | — | 0.55 | |
| Head size, mm | 32mm | ||
| ≤ 28 | — | 0.44 | |
| ≥ 36 | — | 0.96 | |
| Outer cup diameter, mm | 52–56mm | ||
| < 52 | — | 0.89 | |
| > 56 | — | 0.65 |
CI = confidence interval; OR = odds ratio.
Discussion
Using Lewinnek’s “safe zone,” we found that 43.6% of the cups were within the combined inclination and anteversion target using the modified Hardinge approach. There is no consensus in the literature to suggest the ideal position of the acetabular component. Barrack and colleagues26 used the wider ranges of 30°–55° and 5°–35° as their reference ranges for inclination angle and anteversion, respectively. A direct comparison with the study performed by Barrack and colleauges was not possible, as they did not perform any of their surgeries using the modified Hardinge approach.26 Callanan and colleagues25 obtained an accuracy of 32% using the direct lateral approach with a slightly narrower reference range consisting of 30°–45° of inclination and 5°–25° of anteversion.25 Only low-volume surgeons used the direct lateral approach in their study,25 potentially explaining the greater accuracy seen in our study, in which the surgeries were being performed only by high-volume surgeons. Furthermore, the direct lateral group made up only 2.6% of the entire cohort (50/1952) in the study by Callanan and colleagues; therefore, there is more potential for error in their reported results.
Among different studies, cup positioning accuracy varies between 32% and 88% depending on the approach and the target range.25,26 As shown in Table 1, Barrack and colleagues26 had combined accuracy of 79% and 88% mainly due to a wider reference range using the anterolateral and posterolateral approach, respectively. Callanan and colleagues25 used a reference range comparable to the range targeted at our centre. They reported moderate accuracy in attaining cup position in all groups regardless of the approach used, which is comparable to the accuracy we obtained using the modified Hardinge approach.
Our study suggests that women are at risk to have inaccurate anteversion and inclination of their acetabular components. However, we also found that women were more likely to have a lower BMI than men (p < 0.001). The multivariate analysis also highlights this confounding phenomenon, as the significance no longer meets the threshold value to establish sex as a risk factor for cup malpositioning. This suggests that differences in malpositioning seen with sex are confounded by BMI, a factor that was previously identified to affect placement of the cup25,26 and confirmed by our study. These studies demonstrated that patients with a higher BMI are more likely to have an incorrect position of the cup with their chosen reference range of anteversion and inclination. Our study, however, also shows patients who have lower BMI were at risk for acetabular component malpositioning. Potential reasons for cup malposition in these patients include the use of smaller incisions, the potential for patients with lower BMI to have different pelvic obliquity on the operating table and the relatively lower number of patients with low BMI. Analogous to minimally invasive approaches that use smaller incisions, we know that limited exposure is a risk factor for cup malpositioning.25
The size of the acetabular cup was not a significant factor in cup malpositioning, which is consistent with the current literature.25 However, femoral head size was found to be an independent factor affecting inaccuracies in inclination angle. Smaller head sizes were associated with increased inclination angle. However, with further analysis, a temporal factor was demonstrated. Over time, the arthroplasty community has demonstrated an increased tendency to use larger diameter head sizes.31 This widespread tendency was also evident in our data. The literature has demonstrated that increased inclination angle is associated with more polyethylene wear.12,13,15 Concurrent with the trend to increased head size is an increased understanding and acceptance of the effect of inclination and wear, resulting in a tendency toward a decreased inclination angle (Fig. 2). Therefore, the association of smaller head sizes with increased cup inclination has time as a confounding factor.
Previous reports investigating acetabular positioning have relied on a variety of techniques to measure anteversion angles, including edge detection software, computed tomography (CT) and anteroposterior radiographs centred on the hip.25,26,32–35 We used the method outlined by Tiberi and colleagues,28 which is comparatively reliable to edge detection software. Overall, we found the mean inclination angle in our study to be comparable to studies in the literature.25,26,32–35 The mean anteversion angle of 21.82° found in our study, however, is the highest among these studies.
Limitations
Limitations of our study include the lack of a comparison group. A small proportion of total hip replacements were performed using other surgical approaches at our institution. However, these groups were too small to obtain any meaningful comparisons and could not be used (53 hips used a posterior approach, 7 used an anterior approach). The method used for anteversion measurements on routine radiographs is not standardized in literature. It is currently difficult to ascertain the accuracy of radiographic measurements compared with CT scans, as current reports in the literature use variable reference planes to determine anteversion and inclination angles.36 In order to be consistent, we assessed radiographic measurements using the radiographic coronal plane, which is a method currently used and understood by surgeons and is therefore practical. The number of hips operated by trainees was not known in our study. Since only 1 dislocation was identified in this study, an ideal position for the acetabular component could not be determined. The effect of various patient positioning devices on cup positioning could not be determined because all the surgeries were uniformly performed with the use of bolsters.
Conclusion
To our knowledge, our study is the largest to date that attempts to study the accuracy of cup positioning using the modified Hardinge approach performed by high-volume surgeons. Our sample size is comparable to those reported in the literature evaluating the posterolateral approach to establish the accuracy of cup positioning. Consistent with other studies examining other surgical approaches, we showed that a modified Hardinge approach is moderately successful in attaining accurate combined anteversion and inclination angle within a target range.
Footnotes
Funding: Institutional support was received from Stryker, Smith and Nephew, DePuy, Zimmer and Microport.
Competing interests: R. McCalden has been a paid consultant of Smith and Nephew and an employee of Smith and Nephew, and declares speaker fees from Smith and Nephew and travel assistance from Smith and Nephew. J. Howard has been a paid consultant of Depuy an Stryker, and declares speaker fees from Depuy and Stryker, and travel assistance from Depuy and Stryker. B. Lanting has been a paid consultant of Depuy, Stryker, Smith and Nephew and Intellijoint and declares honoraria from Integra, speaker fees from Depuy, Stryker, Smith and Nephew and Intellijoint and travel assistance from Depuy, Stryker, Smith and Nephew and Intellijoint.
Contributors: P. Goyal, M. Teeter, J. Howard and B. Lanting designed the study. P. Goyal and A. Lau acquired the data, which P. Goyal, R. McCalden, M. Teeter, J. Howard and B. Lanting analyzed. P. Goyal, A. Lau, J. Howard and B. Lanting wrote the article, which all authors reviewed and approved for publication.
References
- 1.Shon WY, Baldini T, Peterson M, et al. Impingement in total hip arthroplasty: a study of retrieved acetabular components. J Arthroplasty. 2005;20:427–35. doi: 10.1016/j.arth.2004.09.058. [DOI] [PubMed] [Google Scholar]
- 2.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–21. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi M, Akisue T, Bauer T, et al. The spatial location of impingement in total hip arthroplasty. J Arthroplasty. 2000;15:305–13. doi: 10.1016/s0883-5403(00)90601-6. [DOI] [PubMed] [Google Scholar]
- 4.D’Lima DD, Urquhart A, Buehler K, et al. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–21. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Williams D, Royle M, Norton M. Metal-on-metal hip resurfacing: the effect of cup position and component size on range of motion to impingement. J Arthroplasty. 2009;24:144–51. doi: 10.1016/j.arth.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–20. [PubMed] [Google Scholar]
- 7.Ali Khan MA, Brakenbury P, Reynolds I. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981;63-B:214–8. doi: 10.1302/0301-620X.63B2.7217144. [DOI] [PubMed] [Google Scholar]
- 8.McCollum DE, Gray W. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;(261):159–70. [PubMed] [Google Scholar]
- 9.Robinson M, Bornstein L, Mennear B, et al. Effect of restoration of combined offset on stability of large head THA. Hip Int. 2012;22:248–53. doi: 10.5301/HIP.2012.9283. [DOI] [PubMed] [Google Scholar]
- 10.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–8. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 11.Leslie IJ, Williams S, Isaac G, et al. High cup angle and microseparation increase the wear of hip surface replacements. Clin Orthop Relat Res. 2009;467:2259–65. doi: 10.1007/s11999-009-0830-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patil S, Bergula A, Chen PC, et al. Polyethylene wear and acetabular component orientation. J Bone Joint Surg Am. 2003;85-A:56–63. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 13.Little NJ, Busch C, Gallagher J, et al. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467:2895–900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hart AJ, Ilo K, Underwood R, et al. The relationship between the angle of version and rate of wear of retrieved metal-on-metal resurfacings: a prospective, CT-based study. J Bone Joint Surg Br. 2011;93:315–20. doi: 10.1302/0301-620X.93B3.25545. [DOI] [PubMed] [Google Scholar]
- 15.Schmalzried TP, Guttmann D, Grecula M, et al. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677–88. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Hart AJ, Guttmann D, Grecula M, et al. Insufficient acetabular version increases blood metal ion levels after metal-on-metal hip resurfacing. Clin Orthop Relat Res. 2011;469:2590–7. doi: 10.1007/s11999-011-1930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eilander W, Harris S, Henkus H, et al. Functional acetabular component position with supine total hip replacement. Bone Joint J. 2013;95-B:1326–31. doi: 10.1302/0301-620X.95B10.31446. [DOI] [PubMed] [Google Scholar]
- 18.Murphy WS, Klingenstein G, Murphy S, et al. Pelvic tilt is minimally changed by total hip arthroplasty. Clin Orthop Relat Res. 2013;471:417–21. doi: 10.1007/s11999-012-2581-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arthursson AJ, Furnes O, Espehaug B, et al. Prosthesis survival after total hip arthroplasty–does surgical approach matter? Analysis of 19,304 Charnley and 6,002 Exeter primary total hip arthroplasties reported to the Norwegian Arthroplasty Register. Acta Orthop. 2007;78:719–29. doi: 10.1080/17453670710014482. [DOI] [PubMed] [Google Scholar]
- 20.Colwell J. Instability after total hip arthroplasty. Curr Orthop Pract. 2009;20:8–14. [Google Scholar]
- 21.Enocson A, Tidermark J, Tornkvist H, et al. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008;79:211–7. doi: 10.1080/17453670710014996. [DOI] [PubMed] [Google Scholar]
- 22.Mallory TH, Lombardi A, Jr, Fada R, et al. Dislocation after total hip arthroplasty using the anterolateral abductor split approach. Clin Orthop Relat Res. 1999;(358):166–72. [PubMed] [Google Scholar]
- 23.Abitbol JJ, Gendron D, Laurin C, et al. Gluteal nerve damage following total hip arthroplasty. A prospective analysis. J Arthroplasty. 1990;5:319–22. doi: 10.1016/s0883-5403(08)80090-3. [DOI] [PubMed] [Google Scholar]
- 24.Gore DR, Murray M, Sepic S, et al. Anterolateral compared to posterior approach in total hip arthroplasty: differences in component positioning, hip strength, and hip motion. Clin Orthop Relat Res. 1982;(165):180–7. [PubMed] [Google Scholar]
- 25.Callanan MC, Jarrett B, Bragdon C, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319–29. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barrack RL, Krempec J, Clohisy J, et al. Accuracy of acetabular component position in hip arthroplasty. J Bone Joint Surg Am. 2013;95:1760–8. doi: 10.2106/JBJS.L.01704. [DOI] [PubMed] [Google Scholar]
- 27.Frndak PA, Mallory T, Lombardi A., Jr Translateral surgical approach to the hip. The abductor muscle “split”. Clin Orthop Relat Res. 1993;(295):135–41. [PubMed] [Google Scholar]
- 28.Tiberi JV, Pulos N, Kertzner M, et al. A more reliable method to assess acetabular component position. Clin Orthop Relat Res. 2012;470:471–6. doi: 10.1007/s11999-011-2006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–32. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 30.Woo RY, Morrey B. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–306. [PubMed] [Google Scholar]
- 31.Kostensalo I, Junnila M, Virolainen P, et al. Effect of femoral head size on risk of revision for dislocation after total hip arthroplasty: a population-based analysis of 42,379 primary procedures from the Finnish Arthroplasty Register. Acta Orthop. 2013;84:342–7. doi: 10.3109/17453674.2013.810518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bosker BH, Verheyen C, Horstmann W, et al. Poor accuracy of freehand cup positioning during total hip arthroplasty. Arch Orthop Trauma Surg. 2007;127:375–9. doi: 10.1007/s00402-007-0294-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saxler G, Marx A, Vandevelde D, et al. The accuracy of free-hand cup positioning–a CT based measurement of cup placement in 105 total hip arthroplasties. Int Orthop. 2004;28:198–201. doi: 10.1007/s00264-004-0542-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Todkar M. Obesity does not necessarily affect the accuracy of acetabular cup implantation in total hip replacement. Acta Orthop Belg. 2008;74:206–9. [PubMed] [Google Scholar]
- 35.Mouilhade F, Matsoukis J, Oger P, et al. Component positioning in primary total hip replacement: a prospective comparative study of two anterolateral approaches, minimally invasive versus gluteus medius hemimyotomy. Orthop Traumatol Surg Res. 2011;97:14–21. doi: 10.1016/j.otsr.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 36.Wan Z, Malik A, Jaramaz B, et al. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res. 2009;467:32–42. doi: 10.1007/s11999-008-0597-5. [DOI] [PMC free article] [PubMed] [Google Scholar]