Abstract
Background
Following a landmark study showing decreased morbidity and mortality after implementation of the surgical safety checklist (SSC), it has been widely adopted into perioperative policy. We explored the impact of attitudes and beliefs surrounding the SSC on its uptake in Calgary.
Methods
We used qualitative methodology to examine factors influencing SSC use. We performed semistructured interviews based on Rogers’ theory of diffusion of innovation. Purposive and snowball sampling were used to identify surgeons, anesthesiologists and operating room nurses from hospitals in Calgary. Data collection and analysis were based on grounded theory. Two individuals jointly analyzed data and achieved consensus on emerging themes.
Results
Generated themes included 1) the SSC has brought organization to previous informal perioperative checks, 2) the SSC is most helpful when it is simple, and 3) the 3 current components of the checklist are redundant. The briefing was considered the most important aspect and the debriefing the least important. Initially the SSC was difficult to implement owing to a shift in time management and perioperative culture; however, it has now assimilated into perioperative routine. Finally, though most participants agreed that the SSC might avoid some delays and complications, only a few believe there have been observable improvements to morbidity and mortality.
Conclusion
Although the SSC has been integrated into perioperative practice in Calgary, participants believe that previous informal checkpoints were able to circumvent most perioperative issues. Although the SSC may help with flow and equipment, participants believe it fails to show a subjective, clinically important improvement.
Abstract
Contexte
Après une étude charnière ayant montré une baisse de la morbidité et de la mortalité après la mise en œuvre de la liste de contrôle de la sécurité chirurgicale, cette dernière a été largement intégrée aux politiques périopératoires. Nous avons examiné l’effet des attitudes et des croyances entourant la liste sur son adoption à Calgary.
Méthodes
À l’aide d’une méthode qualitative, nous nous sommes penchés sur les facteurs influençant l’utilisation de la liste. Pour ce faire, nous avons effectué des entrevues semi-dirigées fondées sur la théorie de la diffusion de l’innovation de Rogers. Nous avons utilisé l’échantillonnage dirigé et le sondage en boule de neige pour cibler des chirurgiens, des anesthésiologistes et des membres du personnel infirmier de salle d’opération des hôpitaux de Calgary. La collecte et l’analyse des données étaient fondées sur la théorie ancrée. Deux personnes ont analysé ensemble les données et se sont entendues sur les thèmes émergents.
Résultats
Voici les principales conclusions dégagées : 1) la liste a permis de structurer les contrôles périopératoires non officiels du passé, 2) la liste est surtout utile quand elle est simple et 3) les 3 composantes actuelles de la liste de contrôle sont redondantes. Le breffage était considéré comme étant l’aspect le plus important et le débreffage, le moins important. Au départ, la liste a été difficile à mettre en œuvre en raison des changements à apporter à la gestion du temps et à la culture périopératoire; cependant, elle est maintenant bien intégrée dans la routine périopératoire. Enfin, bien que la plupart des participants conviennent que la liste peut éviter des retards et des complications, seuls quelques-uns croient qu’il y a eu une amélioration observable de la morbidité et de la mortalité.
Conclusion
Si la liste de contrôle de la sécurité chirurgicale a été intégrée dans la pratique périopératoire à Calgary, les participants croient que les points de contrôle non officiels du passé pouvaient prévenir la plupart des problèmes périopératoires. La liste est utile pour ce qui est du processus et de l’équipement, mais les participants croient qu’elle n’apporte pas d’amélioration subjective importante d’un point de vue clinique.
Adverse events (AEs) are unintended injuries caused by medical management rather than disease processes.1 A Canadian audit revealed an incidence of 7.5 AEs per 100 hospital admissions,2 which is concordant with other national AE rates.1,3–5 Nearly half of these occur in surgical patients, and 36%–51% of them are retrospectively judged to be preventable. Additionally, a substantial portion of these AEs are “never events,” such as wrong site surgery and retained foreign objects. Often, the etiology of these AEs is attributed to a failure of communication.
The World Health Organization (WHO) Surgical Safety Checklist (SSC) was developed to improve communication in the perioperative care of patients. A landmark study published in 2009 illustrated that the implementation of the WHO SSC in varied socioeconomic settings worldwide was associated with marked improvements in surgical outcomes, including significant reductions in morbidity and mortality.6 Numerous studies published since then have shown similar results,7–10 and consequently the SSC has seen rapid and widespread adoption.11 Many of these studies have shown compliance to be the most important factor for improved mortality and morbidity.
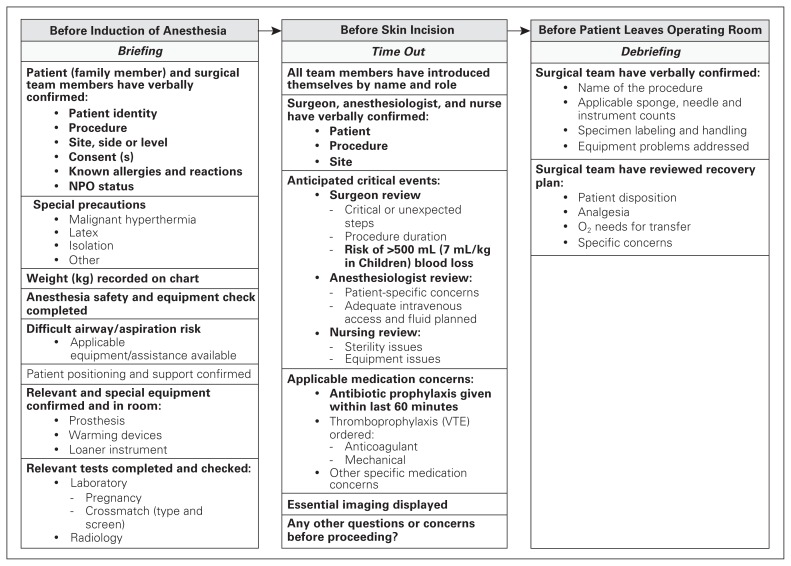
A modified version of the WHO SSC has been adopted by Alberta Health Services (AHS), the single health authority for the province of Alberta, Canada. The AHS governs operations of individual institutions within the province and often introduces policies for clinical practice. In 2009 a modified version of the SSC was formally implemented across Alberta. This checklist has 3 components, as outlined in Figure 1: a “briefing” before induction of anesthesia, a “time out” before skin incision and a “debriefing” before the patient leaves the operating room. All 3 components require the attending surgeon, anesthesiologist and an OR nurse to be present. Residents and other trainees are not permitted to perform any component of the SSC. A prior study from our institution, including hospitals associated with the University of Calgary, illustrated an overall 62.1% compliance across all 3 components.12 A growing body of literature illustrates there are a variety of objective and subjective barriers contributing to a lack of implementation and compliance.13–17 A common factor affecting compliance has been the attitudes of health care providers toward the SSC. Therefore, the objective of this qualitative study was to determine the attitudes of health care providers toward the SSC that may impact its adoption and compliance in Calgary, Canada.
Fig. 1.
Modified version of the World Health Organization surgical safety checklist adopted by Alberta Health Services.
Methods
Theoretical framework
We used an exploratory approach using qualitative methodology to examine the attitudes and beliefs regarding the SSC in Calgary, Canada. A framework based on Rogers’ theory of diffusion of innovation was used to guide the outline of the semistructured interviews.18 This theory describes how a new idea or technology, such as the SSC, is integrated into practice. This theoretical framework has previously been used to determine the adoption of clinical innovations19,20 and was selected to better understand how specific factors contribute to the overall implementation of the SSC. The specific factors influencing adoption are outlined in Table 1: awareness, relative advantage, compatibility, complexity, trialability and observability. Questions in the semistructured interviews were aimed at specifically addressing these factors. We obtained ethics approval from the Research Ethics Board of the University of Calgary.
Table 1.
Factors of Rogers’ theory of diffusion of innovation
| Factor | Description | Questions | Quotes |
|---|---|---|---|
| Awareness | Whether or not users are aware of the innovation | What do you know about the SSC and the evidence supporting its use? | “[AHS] told us [nurses] that it helps with patient safety.” |
| Relative advantage | The degree to which an innovation is perceived as being an improvement on the idea that preceded it | Was there anything similar to the SSC before its implementation? How is the SSC different? | “We were looking for history, consent, whether a side needed to be marked; so [the SSC] just took it a little bit further.” |
| Compatibility | The degree to which an innovation is consistent with existing values | What are your thoughts on the value of the SSC? | “Even if we improve things a small amount it’s worth it.” |
| Complexity | How difficult an innovation is to understand and use | How easy or difficult is it to incorporate the SSC into your perioperative routine? | “Sometimes it feels like we nurses spend a lot of time lassoing [physicians] to get them to participate.” |
| Trialability | How easily an innovation may be experimented with | How often do you use the SSC? What facilitates and prevents you from using it? How easily does the SSC fit into your previous perioperative practice? | “[Surgeons were] the biggest challenge in the process.” |
| Observability | The degree to which the results of an innovation are perceptible to others | Have you noticed any advantages or disadvantages of the SSC? What is the feedback from your OR team? | “I know it’s supposed to save lives and reduce morbidity; I’m not sure it does that. I think that it improves the efficiency of my OR.” |
AHS = Alberta Health Services; OR = operating room; SSC = surgical safety checklist.
Data collection
The theoretical basis of data collection was guided by grounded theory. A single interviewer (N.D.) conducted a single pilot interview in person. This interview was audio-recorded, transcribed verbatim and then discussed among the research team (N.D., M.L.Q.) to confirm that all topics of interest were addressed. The questions of the semistructured interview guide were subsequently adjusted to reflect the discussion. All subsequent interviews were conducted by a single interviewer (N.D.) in person, audio-recorded, and transcribed verbatim. We obtained informed consent from all interviewees before initiation of the interview. Interviewees were informed that interviews could be aborted at anytime and were reassured that responses were confidential and would not be attached to any identifying data.
Sampling and recruitment
We identified potential participants through a snowball sampling strategy, and they were purposively sampled to obtain a variety of perspectives. Initial health care providers were identified based on nominations from clinical leads or division heads. Using the snowball sampling approach, each interviewee was then asked to recommend additional health care providers who could participate in our study. We then approached the recommended providers in person for potential inclusion. Finally, each potential participant was asked to further recommend other potential participants.
Our goal was to interview a minium of 10 surgeons, 10 anesthesiologists and 10 operating room nurses within Calgary or to interview participants until we reached the point of saturation (i.e., until no new information was obtained as per the snowball sampling approach). We selected 3 acute care hospitals to provide different perspectives, as surgical services are regionalized to various hospitals in Calgary. While all 3 hospitals are university-affiliated teaching centres, 1 is home to the only trauma and cancer centre, as well as vascular and cardiac surgery; 1 is a general hospital providing vascular surgery, and the 1 is a pediatric centre. The AHS implementation strategy was delivered to all sites at the same time.
Data analysis
The qualitative analysis of the interview transcripts was conducted with an inductive approach, which involved repeated reading of transcripts, development of a coding scheme to reflect unique ideas within interviews, application of the novel coding scheme to the transcript text, and grouping of coded text. These themes were then tabulated. To improve the reliability of the codes, 2 investigators (N.D., C.C.) analyzed the transcripts. Findings were then compared with discrepancies resolved through discussion.
Results
A total of 31 health care providers were interviewed between October 2012 and August 2013: 12 surgeons, 10 anesthesiologists and 9 operating room nurses; at this point, saturation was reached. As mentioned, these health care providers work at 3 main hospitals within Calgary: 2 adult acute care centres and 1 pediatric centre. All 3 institutions are tertiary-care, academic centres. All 3 hospitals were equally represented within the sample group. Despite a variety of hospital settings, we found that the themes were similar across health care providers and did not differ among the sites. As such, they are presented together.
Themes
Awareness of innovation
All participants were aware of the SSC. Surgeons and anesthesiologists were knowledgeable of the WHO study supporting the implementation and, thus, understood the goal of the SSC was to improve perioperative morbidity and mortality through improved communication. One major concern expressed by physicians regarding the implementation of the SSC was “the improvement in morbidity and mortality evidence appear to be more supportive in less resource-rich health care systems.” Nurses had become aware of the SSC through the AHS implementation process. One nurse noted,
We were told that this is what we were going to do, but were not informed of the evidence other than its potential role in perioperative patient safety. Instead, [AHS] told us [nurses] that it helps with patient safety.
Relative advantage
An informal checklist existed before the province-wide implementation of the SSC; however, most participants observed the AHS SSC to be more structured, formal and comprehensive. Health care providers “were looking for history, consent, whether a side needed to be marked; so [the SSC] just took it a little bit further.” The formality of the SSC was found to translate into a consistent safety checkpoint and “hasn’t added much to what [health care providers] were already doing, but it has standardized it.” The participants noted that the endorsed implementation of the SSC led to improved patient perception of safety. For example, a surgeon noted, “my patients have told me they feel more comfortable knowing what is going on and that we have these safety checkpoints in place.”
Compatibility
All participants believed that the intention of the SSC was to improve perioperative patient care in some capacity. As all interviewees were invested in patient safety, the SSC was consistent with their goals and ideals. An anesthesiologist commented, “even if we improve things a small amount, it’s worth it.” There was concern from several participants that the SSC was not necessarily functioning in the capacity intended. As items not included in the original WHO SSC, such as medical reconciliation of outpatient medications, were added, health care providers objected quite strongly. A participant noted, “you need to study whether the changes have had an unanticipated negative impact or makes no positive impact.” However, the SSC’s role in improving communication as an attempt to improve patient safety resonated with all health care providers, as they use it to communicate.
Complexity
The complexities of adoption were varied among the 3 groups interviewed. The main complexity of adopting the SSC from a nursing point of view was coordinating all 3 parties: nursing, anesthesiologists and surgeons. Nurses expressed their frustration as “sometimes it feels like we nurses spend a lot of time lassoing people to get them to participate.” Nurses often perceived they needed to ensure the completion of the SSC by organizing the surgeons and anesthesiologists, and they hoped “the physicians would take more responsibility for the process.”
The main complexity perceived by the surgeons was the additional burden of completing the SSC while managing their busy days in the operating room. Surgeons were used to having time between cases to take care of other tasks, such as ward issues, administrative work and teaching. The SSC can be viewed as “a hassle because [surgeons] don’t have as much time between cases for multitasking.” Completing all 3 portions of the SSC was found to be cumbersome, particularly for numerous, similar, repetitive procedures, such as tonsillectomies and lumpectomies. One surgeon noted the SSC is “harder during those quick little cases that [health care providers] do, and it would be nice if we could do an abbreviated version in those situations.”
For all parties, the briefing and time out aspects of the SSC were the easiest to use, whereas the debriefing was most difficult to implement. There were many reasons postulated by the interviewees as to why the debriefing had such poor compliance. Nurses found that attending surgeons had “often left the room by the time [nurses] can do the debriefing because [surgeons] have an important responsibility to speak with the family of the patient postoperatively.”
From the surgeons’ perspective, briefing is less of an issue if the case has gone as planned, and when other health care providers “don’t have any concerns you sometimes just move on; sometimes it’s because the nurses are busy at the end of the case getting ready for the next case.”
Anesthesiologists found they were occupied with waking a patient at the end of a case when the debriefing is meant to be completed. This is an important component of perioperative care, and anesthesiologists “are very concerned with the emergence and are not really focused on the debrief because [they] have conflicting priorities at that time.” Most interviewees commented the debriefing was more likely to be completed for procedures that had an unexpected course and also for patients who were being transferred to the intensive care unit (ICU). Of note, the anesthesiologist and nursing staff usually carried out this debriefing with the ICU staff “because of carry through of care.”
Trialability
The SSC was overall feasible to trial within hospitals. There was no new equipment, training or expertise required. The most difficult aspect of trialing the SSC within Calgary operating rooms was to change the current framework of how health care providers manage their time between cases. As mentioned, surgeons often multitask between cases, and having to attend the 3 aspects of the SSC can interfere with their other clinical roles. As such, it was most difficult to ask surgeons to further divide their time by using the SSC, and their cooperation “was the biggest challenge in the process.” However, as the SSC continued to be used, most health care providers felt that it was integrated into routine perioperative care in Calgary.
Observability
Most health care providers were able to observe a change in perioperative culture with the implementation of the SSC. However, differences of opinion existed regarding the main changes observed with the SSC. Most interviewees found themselves more aware of patient and operating room issues and processes, particularly special equipment that may be required for the procedure and confirming the need for and availability of blood products. There also appeared to be an improved awareness of patient allergies among the entire team. The change in communication was noticed by all 3 subgroups of health care providers. Nurses were better informed about tasks that needed to be completed for upcoming procedures. Surgeons noted that the SSC provided an opportunity to confirm that all necessary equipment for a procedure would be present for the case before it started: “the SSC reduces the number of questions from the team because [the surgeons] state it up front and there is lots of clarity about equipment and how things will be done.” This was thought to improve operative efficiency; however, most health care providers subjectively did not notice a change in morbidity or mortality. One participant expressed, “I know it’s supposed to save lives and reduce morbidity; I’m not sure it does that. I think that it improves the efficiency of my OR.”
Discussion
In this qualitative study, we found that the SSC has been successfully accepted and adopted; however, there are mixed attitudes regarding its utility in completing its purported objective of reducing perioperative morbidity and mortality. The adoption and subsequent barriers to adoption of the SSC can be described by factors defined by Rogers’ theory of diffusion of innovation. The utilization of the SSC in Calgary was enabled by ubiquitous awareness, perceived relative advantage and compatibility with existing ideals. The barriers of adoption, however, include complexity of integration into the current perioperative workflow, difficult trialability and lack of observability of the desired effect (i.e., decreased morbidity and mortality).
Our findings parallel those of previous studies that showed high levels of awareness of the SSC in institutions that had mandated its usage. For example, Abdel-Galil21 reported 100% awareness at his institution, and Hurtado and colleagues22 noted 93.8% awareness; both institutions had mandated the use of the SSC.21,22 Awareness of the SSC is integral in its successful adoption; however, it is not sufficient to stop there; it is important to explain the rationale for using the SSC as well as outlining the anticipated benefits.23 An explicit implementation strategy had been carried out in Calgary, including formal presentation at clinical rounds and web-based resources, which likely contributed to widespread awareness. A large driver of implementation was the introduction of its use via the nursing staff, who were less autonomous in their scope of practice and were mandated by their clinical managers to use the SSC.
Prior to the implementation of the SSC, an informal checklist or “time out” was in place. However, its use was inconsistent and was far from comprehensive. The health care providers who participated in our study noted that the modified WHO SSC had added value, likely owing to its structured and formal nature. Furthermore, the consistent and collaborative use of the SSC provided a platform for improved communication and patient safety. This opinion echoes the sentiment noted in another study in which participants strongly disagreed with the statement “[the SCC] brings no added value to existing safety procedures.”24 The ability of the SSC to have benefits beyond improved morbidity and mortality has been established within the literature. Health care providers included in the qualitative study by Thomassen and colleagues25 evaluating nurses’ and physicians’ acceptance of the SSC felt that it was able to reveal insufficient equipment standardization and improve physician–nurse cooperation. They concluded that the checklist could further be used in situations for which it was not originally intended. In addition, we found subjective improvement in OR communication, which was also found by Papaconstantinou and colleagues.16 They administered a pre- and post-SSC implementation questionnaire and found that implementation of the SSC led to overall significant improvement in the perceptions of effective communication regarding equipment needs and availability, critical events or anticipated difficulties during the operation, and surgical team debriefing for patient recovery and postoperative management.
Most studies report an overall compliance with the SSC between 38% and 96% in developed countries.21,26–29 These rates are concordant with the qualitative experience in Calgary, as interviewees reported using some version of the SSC for almost all procedures. However, these rates fail to capture the adherence to the 3 components specifically. Our study found Calgary health care providers were least invested in the debriefing component of the SSC, with some providers commenting the debriefing is likely used for 15%–40% of cases. Levy and colleagues30 noted that despite 100% documentation of SSC completion, not all components of the SSC were completed as defined.30 Cullati and colleagues24 found similar results in university hospitals in Switzerland. The “briefing” and “time out” were completed 90% and 83% of the time, respectively; however the “debriefing” was completed only 47% of the time. Another study noted that poor compliance with “debriefing” may be because of ambiguity of the item or the need to dispel interdisciplinary tension that may arise from detection of errors.31 Our study, however, identified alternative barriers to compliance with the “debrief”: mainly health care providers are concerned about the utility and feasibility of carrying out another checklist item at the end of a procedure, particularly if the procedure went as planned. The SSC was viewed as being disruptive to previous perioperative workflow, which was considered a barrier to adoption from a complexity and trialability perspective. In the study by Thomassen and colleagues,25 health care providers in Norway found their version of the SSC disrupted their established workflow and, consequently, caused stress to both providers and patients. These disruptions dissipated over time as the SSC assimilated into the perioperative culture; this was reflected in the attitudes of the health care providers in our study as well. In a qualitative study by Gagliardi and colleagues17 evaluating factors that influence SSC adherence, health care providers commented that the quality of completion of the SSC was suboptimal. Even when operating room staff complied with the components of the SSC, other staff members were sometimes obstructive, inattentive and preoccupied with other tasks, which may reflect a lack of belief in the utility of the SSC.
One of the most striking results from our study was the belief of health care providers, particularly surgeons and anesthesiologists, that the SSC is unlikely to have a role in decreasing morbidity and mortality in their patient population. This perception is discordant with the findings of multiple studies showing a decrease in perioperative morbidity and mortality with the implementation of the WHO SSC. The reasons are likely multifactorial. A study by Haynes and colleagues6 showed improved rates of morbidity and mortality with specific modification of the WHO SSC. The AHS modified version of the SSC is very similar to the WHO SSC; however, it has not specifically been validated to have similar benefits. Second, the rates of AEs in Calgary may not be equal to reported rates elsewhere, as there was an informal checklist previously in place (preop “time out”). As such, the relative reduction in AE rates may be less significant, given that 1 of the 3 main components of the SSC had already been in place and operational before SSC implementation. Interestingly, a multicentre observational study carried out in Ontario, Canada, confirmed this lack of decreased morbidity and mortality with the implementation of the SSC in a similar Canadian population.11 The postulated reasons for this unexpected finding include a potential Hawthorne effect in studies showing an improvement, the lower likelihood of negative studies being published and poor rates of real-life compliance (despite high rates of documented compliance). The mismatch of documentation and actual compliance has been established in a study by Levy and colleagues.30 In this prospective observational study, despite 100% documented completion of the briefing phase of the SSC, they found that most tasks were not executed as designed or were not executed at all. This poor implementation fidelity may also be an issue in Calgary. A previous study by our group noted equal documented compliance to all components of the SSC, but this equal level of compliance was not reflected in this qualitative study, particularly for the debriefing section of the SSC.12 This may be a result of our documentation practice of checking a box on the operative record when each component of the checklist is complete; anecdotal reports of all 3 boxes being checked before the cases starting have been reported, and may account for the discrepancy between reported compliance and our findings.
This study also highlights similarities and differences in attitudes toward the SSC based on the category of health care providers. Each provider group felt at least somewhat burdened by the task of completing the SSC. In particular, each provider group felt the SSC had the potential to distract from their own clinical duties. Furthermore, each provider group expected other groups to take more ownership of completing the SSC. The motivation for completing the SSC appeared to differ for nurses and physicians. The nurses interviewed emphasized the SSC was a mandated protocol and, thus, needed to be completed. The physicians were more concerned with the potential safety and communication benefits of the SSC. This may explain why nurses voiced they needed to “lasso” physicians into completing the SSC.
Strengths and limitations
There are multiple strengths of this study. Its qualitative nature allowed further depth into the attitudes and beliefs of health care providers in Calgary than a quantitative study would yield. The face-to-face semistructured interview process captured more information than a formally structured interview or survey method would have captured. The analysis of themes by 2 independent researchers provides additional validation of our results. There are also several limitations of this study. This study interviewed health care providers only in Calgary. This collective opinion may be reflective of other similar populations; however, these results may not be completely generalizable. The attitudes of health care providers may differ substantially owing to differing baseline perioperative procedures before implementation of the SSC and to low incidence of AEs. Owing to the face-to-face interview design, this study is susceptible to a social desirability bias. We attempted to circumvent this potential bias by assuring confidentiality of participants and by asking pointed questions prompting reporting of both positive and negative opinions.
Conclusion
This qualitative study shows there are both positive and negative attitudes and beliefs regarding the SSC as implemented and mandated by AHS. Health care providers are motivated to use the SSC owing to high rates of awareness, perceived improvement in communications and efficiency, and high stakes in improved patient care. The SSC has, however, caused disruptions in workflow, and the prevailing belief among heatlh care providers challenges its efficacy in its original intent of improving perioperative morbidity and mortality. Irrespective of this failing, most believe it is a useful tool that improves the perioperative process. The WHO recommends the SSC be modified in order to suit the setting in which it will be used. This study highlights the usefulness of the SSC for improving communication. As the AHS SSC continues to evolve, it will be important to emphasize communication rather than create “another tick box.”
Footnotes
Poster presentation at the Canadian Surgery Forum, Vancouver, B.C., 2014. Podium presentation at the Clinical Congress for American College of Surgery, San Francisco, Calif., 2014
Funding: This study received funding from the MSI Foundation.
Competing interests: None declared.
Contributors: All authors designed the study. N. Dharampal and M. Quan acquired and analyzed the data, which C. Cameron also analyzed. N. Dharampal and M. Quan wrote the article, which all authors reviewed and approved for publication.
References
- 1.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ. 2001;322:517–9. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker GR, Norton PG. Adverse events and patient safety in Canadian health care. CMAJ. 2004;170:353–4. [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. N Engl J Med. 1991;324:370–6. doi: 10.1056/NEJM199102073240604. [DOI] [PubMed] [Google Scholar]
- 4.Gawande AA, Thomas EJ, Zinner MJ, et al. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126:66–75. doi: 10.1067/msy.1999.98664. [DOI] [PubMed] [Google Scholar]
- 5.Kable AK, Gibberd RW, Spigelman AD. Adverse events in surgical patients in Australia. Int J Qual Health Care. 2002;14:269–76. doi: 10.1093/intqhc/14.4.269. [DOI] [PubMed] [Google Scholar]
- 6.Haynes AB, Weiser TG, Berry WR, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360:491–9. doi: 10.1056/NEJMsa0810119. [DOI] [PubMed] [Google Scholar]
- 7.Bliss LA, Ross-Richardson CB, Sanzari LJ, et al. Thirty-day outcomes support implementation of a surgical safety checklist. J Am Coll Surg. 2012;215:766–76. doi: 10.1016/j.jamcollsurg.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 8.Fudickar A, Hörle K, Wiltfang J, et al. The effect of the WHO surgical safety checklist on complication rate and communication. Dtsch Arztebl Int. 2012;109:695–701. doi: 10.3238/arztebl.2012.0695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodrigo-Rincon I, Martin-Vizcaino MP, Tirapu-Leon B, et al. The effects of surgical checklists on morbidity and mortality: a pre- and post-intervention study: effect of surgical checklists. Acta Anaesthesiol Scand. 2015;59:205–14. doi: 10.1111/aas.12443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Klei WA, Hoff RG, van Aarnhem EEHL, et al. Effects of the introduction of the WHO “surgical safety checklist” on in-hospital mortality: a cohort study. Ann Surg. 2012;255:44–9. doi: 10.1097/SLA.0b013e31823779ae. [DOI] [PubMed] [Google Scholar]
- 11.Urbach DR, Govindarajan A, Saskin R, et al. Introduction of surgical safety checklists in Ontario, Canada. N Engl J Med. 2014;370:1029–38. doi: 10.1056/NEJMsa1308261. [DOI] [PubMed] [Google Scholar]
- 12.Laffin MR, Shaheen AA, Dixon E, et al. Surgical safety checklist: Missing when needed the most? J Am Coll Surg. 2013;217:S108. [Google Scholar]
- 13.Haynes AB, Weiser TG, Berry WR, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf. 2011;20:102–7. doi: 10.1136/bmjqs.2009.040022. [DOI] [PubMed] [Google Scholar]
- 14.Fourcade A, Blache J-L, Grenier C, et al. Barriers to staff adoption of a surgical safety checklist. BMJ Qual Saf. 2012;21:191–7. doi: 10.1136/bmjqs-2011-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Russ S, Rout S, Caris J, et al. Measuring variation in use of the WHO surgical safety checklist in the operating room: a multicenter prospective cross-sectional study. J Am Coll Surg. 2015;220:1–11. doi: 10.1016/j.jamcollsurg.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 16.Papaconstantinou HT, Jo C, Reznik SI, et al. Implementation of a surgical safety checklist: impact on surgical team perspectives. Ochsner J. 2013;13:299–309. [PMC free article] [PubMed] [Google Scholar]
- 17.Gagliardi AR, Straus SE, Shojania KG, et al. Multiple interacting factors influence adherence, and outcomes associated with surgical safety checklists: a qualitative study. PLoS One. 2014;9:e108585. doi: 10.1371/journal.pone.0108585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rogers EM. Diffusion of innovations. 4th edition. Simon and Schuster; 2010. [Google Scholar]
- 19.Kaminski J. Diffusion of innovation theory. Canadian Journal of Nursing Informatics. [accessed 2016 Apr. 11]. Available: http://cjni.net/journal/?p=1444.
- 20.Sanson-Fisher RW. Diffusion of innovation theory for clinical change. Med J Aust. 2004;180:S55–6. doi: 10.5694/j.1326-5377.2004.tb05947.x. [DOI] [PubMed] [Google Scholar]
- 21.Abdel-Galil K. The WHO surgical safety checklist: Are we measuring up? Br J Oral Maxillofac Surg. 2010;48:397–8. doi: 10.1016/j.bjoms.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Hurtado JJ, Jiménez X, Peñalonzo MA, et al. Acceptance of the WHO surgical safety checklist among surgical personnel in hospitals in Guatemala city. BMC Health Serv Res. 2012;12:169. doi: 10.1186/1472-6963-12-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conley DM, Singer SJ, Edmondson L, et al. Effective surgical safety checklist implementation. J Am Coll Surg. 2011;212:873–9. doi: 10.1016/j.jamcollsurg.2011.01.052. [DOI] [PubMed] [Google Scholar]
- 24.Cullati S, Licker M-J, Francis P, et al. Implementation of the surgical safety checklist in Switzerland and perceptions of its benefits: cross-sectional survey. PLoS One. 2014;9:e101915. doi: 10.1371/journal.pone.0101915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomassen Ø, Brattebø G, Heltne J-K, et al. Checklists in the operating room: Help or hurdle? A qualitative study on health workers’ experiences. BMC Health Serv Res. 2010;10:342. doi: 10.1186/1472-6963-10-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gueguen T, Coevoet V, Mougeot M, et al. Deployment of the checklist “Patient safety in the operating room” in two Lorraine hospitals. Performances and difficulties. Ann Fr Anesth Reanim. 2011;30:489–94. doi: 10.1016/j.annfar.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 27.Spence J, Goodwin B, Enns C, et al. Student-observed surgical safety practices across an urban regional health authority. BMJ Qual Saf. 2011;20:580–6. doi: 10.1136/bmjqs.2010.044826. [DOI] [PubMed] [Google Scholar]
- 28.Kearns RJ, Uppal V, Bonner J, et al. The introduction of a surgical safety checklist in a tertiary referral obstetric centre. BMJ Qual Saf. 2011;20:818–22. doi: 10.1136/bmjqs.2010.050179. [DOI] [PubMed] [Google Scholar]
- 29.Makary MA, Mukherjee A, Sexton JB, et al. Operating room briefings and wrong-site surgery. J Am Coll Surg. 2007;204:236–43. doi: 10.1016/j.jamcollsurg.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 30.Levy SM, Senter CE, Hawkins RB, et al. Implementing a surgical checklist: more than checking a box. Surgery. 2012;152:331–6. doi: 10.1016/j.surg.2012.05.034. [DOI] [PubMed] [Google Scholar]
- 31.Cullati S, Du SL, Raë A-C, et al. Is the surgical safety checklist successfully conducted? An observational study of social interactions in the operating rooms of a tertiary hospital. BMJ Qual Saf. 2013;22:639–46. doi: 10.1136/bmjqs-2012-001634. [DOI] [PubMed] [Google Scholar]