Abstract
A strong foundational knowledge of dermatologic disease is crucial for a successful practice in plastic surgery. A plastic surgeon should be able to identify and appreciate common dermatologic diseases that may require medical and/or surgical evaluation and management. In this article, the authors describe epidermal/dermal, infectious, pigmented, and malignant cutaneous lesions that are commonly encountered in practice. Descriptions include the epidemiology, pathogenesis, clinical course, and management options for each type of lesion.
Keywords: dermatology, cutaneous, common, benign, malignant
Epidermal/Dermal Lesions
Seborrheic Keratosis
Seborrheic keratoses (SKs) are common benign skin lesions in adults. Men and women are affected equally, and the frequency and number of lesions appears to directly correspond with age.1 Epidemiological studies from numerous countries have reported prevalence rates approaching 100% in patients over 70 years of age.2 They can be singular or multiple, with lesions throughout the body, excluding the palms, soles, and mucous membranes. Although SKs may be found on nearly any part of the body, the highest rates occur on sun-exposed areas such as the head, neck, and trunk.
The cause of these lesions is unknown, but is believed to involve mutations in genes that regulate cell growth, such as fibroblast growth factor receptor 3.1 Histologically, the epidermis shows proliferation of the basal cells as well as cystic inclusions of keratinaceous material.
Seborrheic keratoses present clinically as hyperpigmented, waxy, verrucous papules with a characteristic “stuck-on” appearance (Fig. 1). The color may range from skin-colored to brown or black. At times, the lesions resemble malignant melanoma or squamous cell carcinoma, and a biopsy is warranted.
Fig. 1.

Seborrheic keratosis. (Photograph courtesy of Dr. Theodore Rosen.)
Treatment, including cryotherapy, shave removal, or dermabrasion, is reserved for symptomatic lesions and those that cause the patient distress from a cosmetic standpoint. It is critical to remember that in darkly pigmented individuals cryotherapy is not an option due to the possibility of postinflammatory hypopigmentation.
Dermatofibroma
Dermatofibromas (DFs), also known as benign fibrous histiocytomas, are common dermal nodular lesions that arise most often on the lower extremity. Women are affected roughly four times more often than men.
The exact cause of DFs is unknown, but they are believed to be associated with trauma from things such as insect bites or shaving. Evidence of clonal expansion in these lesions may support a neoplastic or inflammatory etiology.1
Dermatofibromas present as a solitary, firm, hyperpigmented macule or thin papule on the lower extremity (Fig. 2). They are usually asymptomatic, but may sometimes be painful or pruritic. Lesions exhibit a positive “dimple sign” when lateral pressure is applied.
Fig. 2.

Dermatofibroma. (Photograph courtesy of Dr. Theodore Rosen.)
Except for symptomatic lesions, surgical excision is not usually recommended, as the resulting scar may be more apparent than the lesion itself. Occasionally, lesions may undergo partial or complete regression.
Acrochordon (Skin Tag)
Acrochordon is the most common skin lesion,1 and there is an increased frequency with age. They may arise as a result of repeated irritation to the skin, and are often seen in areas of chronic friction such as the neck, axilla, and groin. The presence of multiple lesions may be associated with obesity, hyperlipidemia, hypertension, and insulin resistance.3 4
Acrochordons present as small, skin-colored, pedunculated papules that may be singular or multiple. They are often asymptomatic, but may become irritated by clothing and jewelry. Occasionally, they may undergo thrombosis, causing pain. The treatment for a symptomatic lesion includes cryotherapy, snip excision, or shave excision.
Lipoma
Lipomas are very common benign tumors that arise in the subcutaneous tissues of the neck, shoulders, trunk, and extremities. Lesions may be solitary or multiple. They may arise at any age, but are seen commonly in middle-aged adults.
Lipomas consist of mature adipocytes surrounded by a thin fibrous capsule. Their cause is unknown; however, familial patterns suggest a genetic association. Similar to acrochordons, lipomas are seen with increased incidence in overweight and diabetic patients.1 They rarely, if ever, undergo malignant transformation.
Lipomas present as soft, rubbery, nontender, slow-growing subcutaneous nodules that are freely movable on palpation. Multiple lipomas may be seen in inherited syndromes such as adiposis dolorosa, Madelung's disease, Cowden's syndrome, and Gardner's syndrome.
When treatment is desired, enucleation via slit incision or excision may be performed. Large lesions may be treated with liposuction.1
Epidermoid/Epidermal Inclusion Cyst
Epidermal inclusion cysts (EICs), also known as infundibular, epidermoid, or sebaceous cysts, comprise the most common class of cutaneous cysts. They occur most often on the head and upper trunk, but may arise anywhere on the body. Lesions may be singular or multiple. They are seen commonly in young to middle-aged adults and are twice as common in men.
Epidermoid cysts arise from the infundibular portion of the hair follicle, often following disruption of the follicle or secondary to trauma. EICs are filled with keratinaceous debris and lined by a stratified squamous epithelium with a granular layer.
Epidermal inclusion cysts present as skin-colored to yellow, firm, movable nodules, often with a visible central punctum. They are usually asymptomatic, but may become inflamed or irritated due to rupture of the cyst wall. Additionally, they may have a foul-smelling discharge and may rarely undergo malignant degeneration.1 Milia are small, superficial epidermoid cysts measuring only 1 to 3 mm in diameter. They can arise at any age and are seen commonly on the face, especially on the cheeks and eyelids.
If bothersome, EICs may be removed via surgical excision. Care must be taken to remove the entire cyst wall to prevent recurrence. If a cyst is acutely inflamed or infected, it should be treated with incision and drainage with or without oral antibiotics and allowed to heal for at least 2 months prior to surgical therapy. Occasionally, intralesional triamcinolone may be used to hasten the resolution of inflammation. Milia may be treated medically with topical retinoids or surgically by making a small incision, often with a needle, and expressing the contents.
Trichilemmal/Pilar Cyst
Also called pilar cysts, trichilemmal cysts are the most common cysts seen in the scalp, with an estimated prevalence of 5 to 10% of the population.5 They appear commonly in middle-aged women and may be inherited in an autosomal dominant pattern.1 Pilar cysts are composed of eosinophilic keratin. In contrast to epidermoid cysts, pilar cysts are lined by a stratified squamous epithelium without a granular layer.
Pilar cysts present as freely movable, smooth nodules that may grow up to several centimeters in size. Lesions may be singular or multiple. The larger they grow the more likely they are to result in hair loss over the cyst. They closely resemble epidermoid cysts, but lack the central punctum seen in the latter.
Noninfected cysts can often be enucleated intact via a small linear incision or elliptical excision. Lesions with evidence of infection may require incision and drainage with or without antibiotic therapy prior to undergoing excision.
Sebaceous Hyperplasia
Sebaceous hyperplasia appears commonly in middle-aged adults and increases in prevalence with age.6 These lesions arise most often on the face; however, lesions may be found anywhere on the skin with the exception of the palms and soles. Sebaceous hyperplasia is more common in renal transplant patients and those on long-term immunosuppressive therapy.
Sebaceous hyperplasia represents proliferation of histologically normal-appearing sebaceous glands. Clinically, it appears as small, skin-colored to yellow papules with a central dell. Lesions are asymptomatic, but may become inflamed after local trauma. Malignant degeneration is rarely if ever seen, but its clinical presentation can sometimes mimic basal cell carcinoma.
Given the benign nature of sebaceous hyperplasia, treatment is not necessary. If treatment is desired, the lesions may be treated with cryotherapy, electrodessication, or laser therapy.
Neurofibroma
Neurofibromas (NFs) may arise at any age. Solitary cutaneous NFs are common in the general population. In patients with multiple NFs and in patients with a plexiform NF, a diagnosis of neurofibromatosis type I (NF1) should be considered.
Neurofibromas are benign tumors of neuromesenchymal origin, which includes Schwann cells and endoneurial fibroblasts. Although NF1 is associated with a mutation in neurofibromin, tumor formation requires a second hit and a loss of heterozygosity.1 The etiology of a solitary NF is unknown.1
Neurofibromas present as soft, compressible, pink or skin-colored papules or nodules. They often exhibit the “button-hole” sign, where they can easily be pushed into the dermis. They may also exhibit a positive Tinel sign, where light percussion of tissue overlying the tumor results in the sensation of pins and needles along the distribution of the affected nerve.7 Plexiform neurofibromas are larger and are classically described as having a “bag of worms” sensation with palpation.
Excision is the treatment of choice for tumors that are symptomatic or causing cosmetic distress. The monitoring of suspicious lesions with magnetic resonance imaging can help rule out malignant transformation.
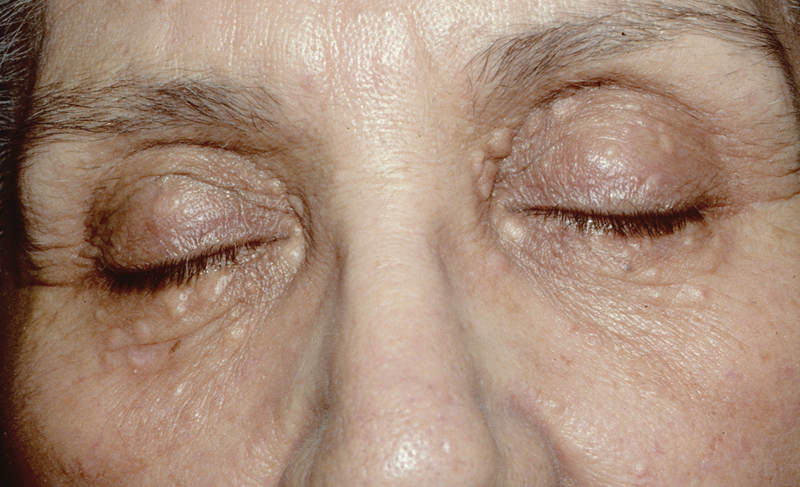
Xanthelasma Palpebrarum
Xanthelasma are common cholesterol-rich lesions that often present in middle-aged adults. These lesions are suggestive of underlying hyperlipidemia, which may be seen in as many as 50 to 60% of people with xanthelasma.1 Earlier onset of lesions is seen more commonly in inherited hyperlipidemias. Xanthelasma may serve as an independent risk factor for atherosclerosis and ischemic heart disease.8 9
Xanthelasma present as asymptomatic yellow-orange papules and plaques, commonly on the medial eyelids. Because of their strong relationship to underlying lipid disorders, appropriate laboratory screening should be performed.
Treatment, typically with surgical excision, is reserved for cosmetic concerns or when the diagnosis is uncertain. Other techniques such as laser therapy, electrodessication, or cryotherapy have also been shown to be effective, but may cause scarring and pigmentary changes.10 Correction of the underlying hyperlipidemia is largely ineffective in treating xanthelasma.
Syringoma
Syringoma is a common benign adnexal neoplasm of sweat duct origin that arises in early adulthood. It is seen with increased incidence in patients with Down's syndrome,10 11 and the clear cell variant is associated with diabetes mellitus.
Syringoma presents as asymptomatic, skin-colored to yellow papules and plaques commonly found on the eyelids and upper cheeks (Fig. 3). However, they may also present on the neck, trunk, or extremities.
Fig. 3.
Syringoma. (Photograph courtesy of Dr. Theodore Rosen.)
Given the asymptomatic nature of syringoma, treatment is usually aimed at addressing cosmetic concerns. Laser ablation therapy has been largely successful in treating cosmetically distressing lesions.10 Other treatment options include cryotherapy, electrodessication, and excision.
Infectious Lesions
Verruca (Wart)
Warts are common skin lesions caused by infection with human papilloma virus (HPV). Human papilloma virus, a highly contagious virus transmitted via direct contact, is the most common sexually transmitted infection throughout the world, including the United States.12 There are various subtypes of warts, including verruca vulgaris (VV; common warts), flat warts, palmoplantar warts, and condyloma acuminata (anogenital warts).
Warts are generally asymptomatic, but may occasionally be associated with pain or pruritus. In addition, they may cause significant psychosocial distress. Verruca vulgaris arises as verrucous, brown, or skin-colored exophytic papules with punctate thrombosed capillaries. In contrast, palmoplantar warts are generally endophytic lesions, and flat warts are smooth, flat-topped, thin papules. Condyloma acuminatum presents as an exophytic or pedunculated smooth papule or plaque in the anogenital area and is commonly associated with HPV types 6 and 11.
Warts are generally considered self-limited; however, treatment can help shorten the duration of symptoms and prevent transmission. In determining how to treat a wart, the type of wart, location, and age of the patient should all be considered. The treatment options include cryotherapy, imiquimod, curettage, scissor or shave excision, and home therapy with salicylic acid covered by silver duct tape. For recalcitrant warts, intralesional bleomycin or Candida antigen may be considered. Patients should be instructed to avoid picking at the lesions to prevent spread, and female patients and female partners of patients with anogenital warts should undergo regular Pap tests to evaluate for cervical neoplasia.
Herpes Simplex
Herpes simplex virus (HSV) is a pervasive virus that can be serologically detected in the majority of the population. Genital herpes alone is estimated to affect more than 50 million people in the United States.13 Infections can be caused by either HSV-1 or HSV-2, with HSV-1 being more common in herpes labialis (cold sores) and HSV-2 more common in genital lesions.
Herpes simplex virus can be transmitted whether lesions are present or not (asymptomatic or active shedding). Once infected, HSV-1 remains dormant in the trigeminal ganglia, whereas HSV-2 remains latent in the lumbosacral ganglion.14
Prodromal flulike symptoms typically occur during primary infection with HSV. Recurrent lesions may be associated with a prodrome of mild paresthesia (burning or tingling) in the hours to days preceding the eruption of lesions. Herpes simplex virus presents as asymptomatic or painful grouped vesicles on an erythematous base with eventual ulceration and crusting, which signals a great reduction in infectivity (Fig. 4). Herpetic whitlow is a variant seen on the digits of children and healthcare workers. Patients with a poor skin barrier, such as those with atopic dermatitis, have an increased risk of eczema herpeticum (Fig. 5), or widespread monomorphic, punched-out erosions due to HSV dissemination.
Fig. 4.

Herpes simplex virus. (Photograph courtesy of Dr. Theodore Rosen.)
Fig. 5.
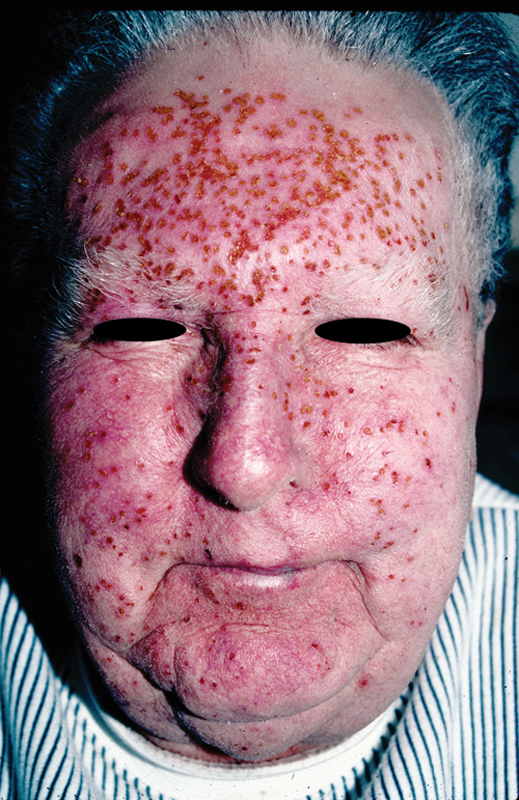
Eczema herpeticum in a transplant patient.
Antivirals such as acyclovir or valacyclovir are the mainstay of therapy. Although they are not curative, antivirals may decrease the frequency, duration, and severity of outbreaks. They also reduce asymptomatic shedding by 95%.1 14 Chronic suppressive therapy is usually reserved for patients who experience at least six outbreaks per year. However, in patients undergoing stressors (emotional or physical, such as a death in the family, laser therapy, or surgery), a short-term prophylaxis with antiviral therapy has been successful in reducing outbreaks.1 A recent international review suggests that the long-term use of oral antivirals in asymptomatic individuals can prevent episodes of herpes labialis, but the small clinical benefit observed may not be great enough to warrant widespread long-term antiviral use.15 There are currently numerous topical antiviral and combination antiviral/steroid creams that are also effective in shortening the duration of the lesions.
Varicella/Shingles
A primary infection by varicella zoster virus (VZV) is known as varicella, or chickenpox, and occurs most often in children. Herpes zoster, or shingles, refers to the reactivation of latent virus following initial exposure and is seen with increasing incidence with age and level of immunosuppression. Varicella zoster virus was present in over 95% of people worldwide prior to the development of the vaccine.1 Since vaccination began, the rates of infection in the United States have decreased by approximately 85%.1
Varicella zoster virus is transmitted by airborne droplets, but may also be transmitted via direct contact. Patients are infectious from 48 hours prior to the onset of lesions until all of the lesions have crusted. Following initial childhood infection, the virus remains dormant in the dorsal root ganglia for the remainder of the person's life. Any disruption of the host's immune system by trauma, stress, illness, medications, or increasing age, can lead to reactivation of the dormant virus.
A diagnosis is made clinically, but a Tzanck smear, viral culture, or a polymerase chain reaction can confirm the diagnosis when there is doubt. Some patients with varicella, adults more often than children, may experience a prodromal flulike illness just prior to the onset of rash. Over the course of several days, successive crops of pruritic vesicles on an erythematous base (“dewdrops on a rose petal”) appear, with all stages of healing present simultaneously (Fig. 6). The reactivation of VZV often presents in a dermatomal distribution with pruritus, pain, or dysesthesia prior to an eruption of grouped vesicles on an erythematous base. Postherpetic neuralgia, the most common complication from shingles, is seen in as many as 20% of patients.1 Ramsay-Hunt syndrome occurs when VZV infection involves the geniculate ganglion and may present as facial palsy and pain or vesicles in the external auditory canal.
Fig. 6.

Varicella zoster virus (shingles).
Antiviral medications given within the first 3 days of cutaneous varicella and the first 3 to 7 days of shingles can help reduce the duration of symptoms and the risk of subsequent development of postherpetic neuralgia.1 A live vaccine is available to prevent primary and recurrent VZV, and varicella zoster immunoglobulin is available for use in high-risk, immunocompromised individuals exposed to VZV. Options for neuropathic pain related to postherpetic neuralgia include analgesics, gabapentin, pregabalin, or tricyclic antidepressants.14 Herpes zoster in the V1 distribution warrants ophthalmologic examination, as ocular involvement is seen in as many as 50% of these patients.1
Scabies
Scabies is a very common mite infestation due to Sarcoptes scabiei and is observed worldwide. It is estimated to affect approximately 300 million people around the world and is strongly associated with overcrowding.16 Infestation can occur anywhere on the body, but commonly affects the interdigital spaces, genital region, or flexural areas such as the wrist and axillae. Scabies often arises as an outbreak within families and communities. Transmission is through direct contact with infected people or clothing. Female mites burrow into the stratum corneum, where they lay eggs that hatch after 7 to 10 days.
Scabies presents as intensely pruritic erythematous papules, nodules, excoriations, and burrows often in the interdigital webspaces, wrists, axilla, groin, and buttock. Infants and immunosuppressed hosts may present with more widespread lesions. A scabies infestation can be confirmed with skin scraping and identification of eggs, mites, or scybala (feces) under light microscopy.
Antiscabetic agents such as topical permethrin or oral ivermectin should be provided to the patient and all household contacts. All clothing and linens should be washed with hot water to ensure the eradication of mites that have been transmitted to them. Repeat therapy as described above should be undertaken 7 to 10 days later to treat the hatching eggs. Patients should be made aware that pruritus often continues for several weeks to months after the elimination of mites. This residual pruritus may be improved with antihistamines.
Tinea/Dermatophytosis
Tinea describes a wide variety of superficial fungal infection due to dermatophytes, a ubiquitous group of fungi. Dermatophyte transmission to humans occurs via other humans, animals, or soil. Infection may occur anywhere on the body and is named based on location. Common types of tinea in adults are tinea corporis (ringworm), tinea cruris (“jock itch”), tinea pedis, and tinea unguium (onychomycosis).
Dermatophytes produce keratinases, which allow them to invade into the stratum corneum, thus producing disease. Risk of infection is increased in patients with skin breakdown or maceration. Diagnosis may be confirmed by KOH (potassium hydroxide) preparation of skin scrapings, skin biopsy, or culture.
Tinea's clinical appearance depends largely on the site of infection and lesions are often pruritic. Tinea capitis appears as scaly erythematous patches or localized alopecia with broken hairs visible at the level of the scalp. Tinea corporis and cruris present as erythematous, scaly, annular lesions with a raised papular or pustular border. There is notable sparing of the scrotum in tinea cruris. All patients with tinea cruris should be inspected for concurrent tinea pedis or tinea unguium, as infection is often spread to the groin via clothing. Tinea pedis often involves the soles and interdigital spaces, with notable scaling or fissuring. Onychomycosis is characterized by nail thickening, nail discoloration, nail dystrophy, and onycholysis.
Topical antifungals, including azoles and allylamines, are the cornerstone of therapy for tinea infections. However, systemic therapy is required for infections that involve the hair or nails and for resistant lesions on the body.
Erythrasma
Erythrasma is a superficial bacterial infection of the stratum corneum due to Corynebacterium minutissimum, a gram-positive rod. Infection arises in warm, moist environments such as the groin, axilla, and interdigital spaces. Risk factors include hyperhidrosis, obesity, and diabetes.
Erythrasma presents as well-demarcated red-brown patches with an overlying fine scale, often in the axilla, groin, or interdigital spaces. Lesions are often asymptomatic, but may be associated with pruritus. Examination with a Wood's lamp reveals coral red fluorescence due to porphyrin production by the bacteria.
Treatment is with topical or oral clindamycin or erythromycin. Other options include aluminum chloride, azole antifungals, Whitfield's ointment, and fusidic acid.1 17
Pigmented Lesions
Melanocytic Nevus
Melanocytic nevi may be present at birth, but the majority of lesions develop during childhood and early adulthood. Peak development occurs during puberty and pregnancy, possibly suggesting a hormonal influence. Both genetic and environmental factors, including sun exposure, play a role in their development. All races may be affected, but nevi are more common in Caucasian individuals. They are the result of melanocytic proliferation in the dermis and/or epidermis.
Clinically, melanocytic nevi present as well-circumscribed skin-colored to brown macules or papules, predominantly on sun-exposed skin (Fig. 7). The clinical appearance varies based on the histologic subtype (junctional, intradermal, or compound) and location. Acral nevi should have pigment in the skin furrows, but not the ridges. All nevi should be evaluated for asymmetry, border irregularity, variable color, diameter > 6 mm, evolution, and a family history of melanoma (the ABCDEFs of melanoma). Benign melanocytic nevi are usually asymptomatic, and symptoms such as pruritus, pain, or bleeding may signal atypia.
Fig. 7.

Multiple melanocytic nevi.
Treatment is not necessary for clinically benign-appearing nevi. However, for lesions that are clinically atypical or are symptomatic, biopsy is recommended. If there is a strong suspicion for melanoma, an excisional biopsy should be performed. For biopsy-proven severely dysplastic nevus or melanoma, wide local excision is the treatment of choice.
Halo Nevus
Halo nevi are benign pigmented lesions occurring in approximately 1% of the general population, most often in teenagers.1 Halo nevi present as single lesions, but there may be multiple lesions. They can be seen in patients with malignant melanoma, multiple dysplastic nevi, and vitiligo. Therefore, the identification of a halo nevus should prompt a thorough skin examination for these additional lesions.
Depigmentation results from an immune attack against the nevus. Although the underlying etiology of this immune response is unknown, the destruction of melanocytes has been postulated.
Halo nevi are often asymptomatic. They present with a central pigmented nevus surrounded by a rim of depigmentation at the periphery; the majority of lesions regress over months to years, leaving a residual depigmented macule (Fig. 8). Some macules may later demonstrate repigmentation.
Fig. 8.
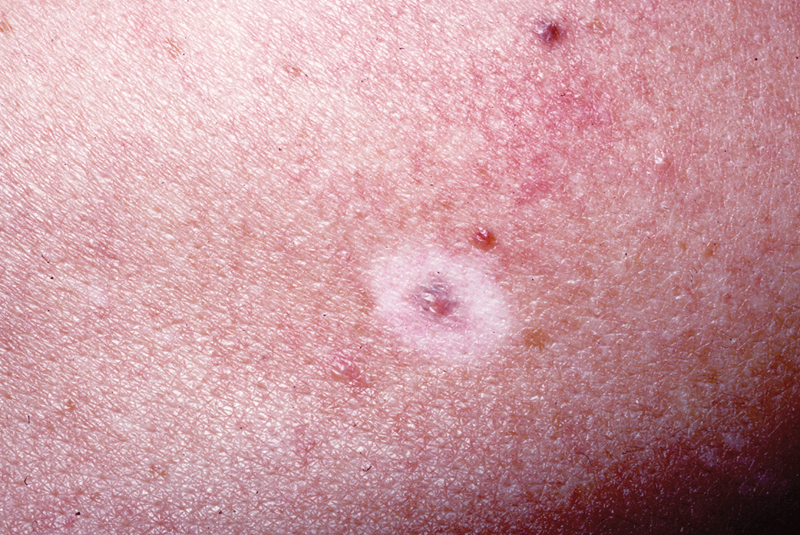
Halo nevus. (Photograph courtesy of Dr. Theodore Rosen.)
Halo nevi with an atypical appearing central nevus should be excised. Benign appearing nevi can be followed clinically. As previously mentioned, patients, especially adults, with halo nevi should undergo a full skin examination to assess for melanoma.
Becker's Melanosis/Nevus
Becker's melanosis may be seen in all races. Onset is usually in adolescence, and men are affected six times more often than women.1 These lesions are benign hamartomas with an unknown pathogenesis. Given their usual onset around puberty, they may respond to androgens.
Becker's melanosis presents as a unilateral, pigmented macule, papule, patch, or plaque on the upper trunk or shoulder, often associated with hypertrichosis, smooth muscle hyperplasia, and a pseudo-Darier's sign. There is no malignant transformation.1
Treatment is not necessary, as they are benign. However, if bothersome to the patient, waxing, electrolysis, and laser therapy may be used to treat the hypertrichosis.
Lentigo
Solar lentigines are seen in the vast majority of elderly patients, affecting lightly pigmented individuals more often than darkly pigmented individuals. In contrast to solar lentigines, lentigo simplex develops at an earlier age and is seen in all races.1
Solar lentigines are associated with chronic sun exposure, which leads to ultraviolet- (UV-) induced epidermal hyperplasia and increased melanin content within keratinocytes.1 Although the pathogenesis of lentigo simplex has not been elucidated, there is a known increase in basal melanocytes and melanin production within these lesions.
Both solar lentigo and lentigo simplex present as well demarcated, evenly pigmented, brown macules. Whereas solar lentigo has a predilection for sun-exposed areas, lentigo simplex may be found throughout the skin, including on the mucosa. Some people believe solar lentigines may be a precursor to seborrheic keratoses. Rarely, lentigines may be associated with genetic diseases, including LEOPARD (lentigines [multiple], electrocardiographic conduction abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of genitalia, retardation of growth, deafness) syndrome, Carney's complex, Peutz-Jeghers syndrome, and xeroderma pigmentosum.
Although treatment of lentigines is not necessary, laser surgery and cryotherapy have been used with variable success. As solar lentigines are an indicator of sun damage and sun exposure, patients should be monitored for the development of skin cancer. Additionally, the importance of strict photoprotection should be emphasized to patients.
Vitiligo
Vitiligo affects less than 2% of the population. Although it may appear at any age, vitiligo often first appears around age 20.1 The exact etiology of vitiligo is unknown; however, it is believed to be a type of autoimmune disease leading to the destruction of melanocytes in affected skin.
Vitiligo is characterized by the development of well-demarcated macules and patches of depigmented skin. There is a predilection for sites that normally have relative hyperpigmentation, such as the perioral and periocular areas, the dorsal hands, the extensor surfaces, and the anogenital area. Affected hair-bearing sites often exhibit poliosis. The clinical course is varied, with some patients experiencing complete remission and others showing gradual progression. Although rare, vitiligo may be associated with other autoimmune diseases, most often autoimmune thyroid disease.
Although treatment is not necessary, it is often desired, as vitiligo can cause psychological distress when there is a significant difference in appearance between affected and unaffected skin. Treatment options include topical corticosteroids, topical calcineurin inhibitors, phototherapy (narrowband UVB or psoralen and UVA- PUVA [photochemotherapy]), and excimer laser therapy.
Premalignant and Malignant Lesions
Premalignant and malignant skin lesions are often asymptomatic at presentation. However, when present, pruritus is usually the presenting symptom. Other symptoms, which more often present later in the disease course, include pain, bleeding, ulceration, inability to heal, rapid growth, and overlying scale. Although there are a wide variety of cutaneous premalignant and malignant lesions, in this section we will focus on the commonly found lesions, including actinic keratosis (AK), basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and malignant melanoma.
Actinic Keratosis
Actinic keratosis is a premalignant lesion composed of atypical keratinocytes confined to the epidermis. This lesion, which is the most common premalignant skin lesion, develops on sun-damaged areas of the body, including the scalp, ears, face, neck, dorsal hands, and dorsal extremities, with relative sparing of photoprotected areas. There is a higher incidence of AKs in lighter skinned individuals, in males, in middle-aged adults, and in those individuals with chronic sun exposure.
Actinic keratoses arise on sun-exposed skin as a result keratinocyte damage following exposure to UV light, with UVB sunlight believed to cause more significant damage than UVA. A higher cumulative amount of UV exposure and an increased frequency of sunburns in childhood increase the risk of formation of AKs and SCCs.
Actinic keratoses present as erythematous, scaly papules, with a sandpaper or rough texture. These lesions may lack the characteristic erythema, making palpation, in addition to visual inspection, an important aspect of skin examination. Variations of AKs include hypertrophic AKs and actinic cheilitis. Hypertrophic AKs have a characteristic hyperkeratotic scale-crust and may occasionally develop into cutaneous horns. The presence of a cutaneous horn warrants biopsy, as this can be the manifestation of an underlying premalignant or malignant lesion in as many as 39 to 58% of cases18 19 (Fig. 9). Actinic cheilitis refers to the presence of actinic keratoses and sun damage on the vermilion lip.
Fig. 9.

Cutaneous horn.
Treatment of actinic keratoses depends on the size, location, and number of lesions present. When few lesions are present, focused therapy, including cryotherapy or curettage, is performed. When there are numerous lesions or if there is more extensive sun damage, field therapy with 5-fluorouracil, diclofenac, imiquimod 5%, ingenol mebutate, or photodynamic therapy should be considered. If left untreated, actinic keratoses have a 10 to 20% risk of transformation to SCC over a 10-year period.1
Basal Cell Carcinoma
Basal cell carcinoma is the most common primary malignant skin tumor seen in dermatology. Basal cell carcinoma arises on sun-damaged skin of the head, neck, and upper extremities, with an increasing incidence with age, fair skin, chronic sun exposure, and a history of tanning bed use.
As with actinic keratoses, BCCs are associated with UVB-induced keratinocyte damage. However, BCCs are believed to be associated more with intermittent, intense UV exposure and sunburn at any age. The development of basal cell skin cancer is associated with inactivation in patched or activation of smoothened or sonic hedgehog. Genetic syndromes that predispose individuals to BCC include basal cell nevus syndrome (BCNS; Gorlin syndrome), Bazex syndrome, and Rombo syndrome.
Basal cell carcinoma presents as a pink, pearly papule with overlying telangiectasia and rolled borders. Ulceration may be present, giving a characteristic “rodent bite” ulcer (Fig. 10). The nodular subtype comprises approximately 50% of BCCs,1 with other less common subtypes including superficial and morpheaform. Superficial BCC presents as a well-circumscribed erythematous, thin papule or plaque with overlying scale and is often multifocal with subclinical spread. Morpheaform BCC is a more aggressive subtype that presents as an ill-defined hypopigmented to light pink indurated plaque, resembling a scar. Basal cell carcinomas are very dependent on the stroma for survival, making metastasis extremely rare.
Fig. 10.

Ulcerated basal cell carcinoma.
Treatment is based on size, location, histologic subtype, and the health status of the patient. Treatment options include electrodessication and curettage (ED&C) with or without cryotherapy, wide local excision, and Mohs micrographic surgery. Radiation may be considered in patients who are poor surgical candidates. Medical therapy with vismodegib, a smoothened inhibitor, may be used in locally advanced or metastatic BCCs or in BCNS.
Squamous Cell Carcinoma
Squamous cell carcinoma is the second most common skin cancer in the general population, and the most common skin cancer in transplant patients. As with BCCs, these lesions are associated with chronic sun exposure and are more commonly seen with lighter skin, increasing age, and tanning bed use. There have been reports of increasing incidence in patients exposed to arsenic, tar, and radiation. Also there is a reversal of the BCC to SCC ratio seen in the normal immunocompetent population compared with the immunodeficient or transplant population.
The development of SCC is associated with UV-induced keratinocyte damage and inactivating mutations in the p53 tumor suppressor gene. Other risk factors include chronic inflammation (Marjolin's ulcer), arsenic exposure, more than 350 PUVA treatments,20 and immunosuppression following transplantation.
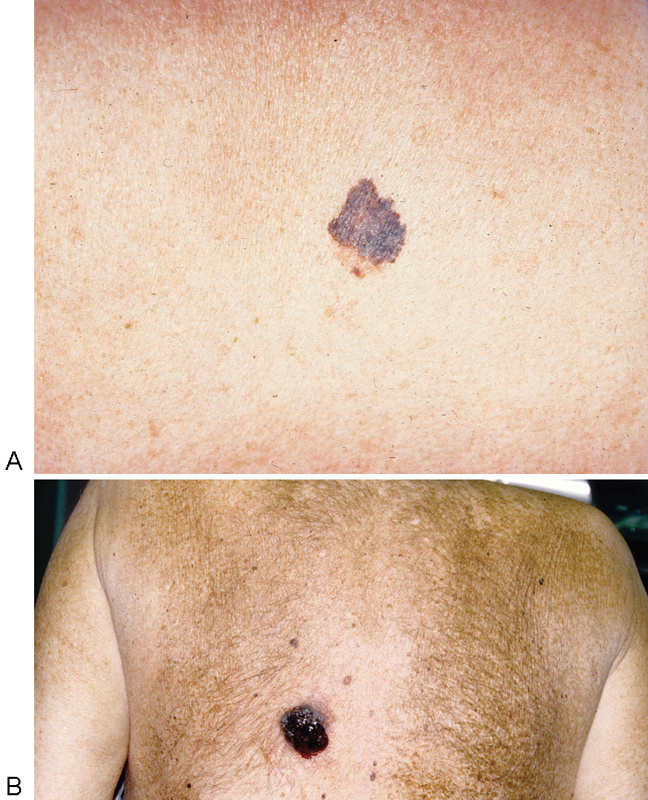
Squamous cell carcinoma presents as an erythematous, scaly or verrucous papule or plaque (Fig. 11A). Squamous cell carcinoma in situ (SCC-IS; Bowen's disease) refers to full-thickness epidermal atypia that presents as a thin eczematous, erythematous plaque. In contrast to SCC-IS, invasive SCC extends into the dermis and may metastasize (most often with lesions on the ear or lip, lesions > 2 cm in size, and in the immunosuppressed population). Keratoacanthoma, considered to be a variant of SCC, is a rapidly growing crateriform nodule with a keratotic core (Fig. 11B).
Fig. 11.
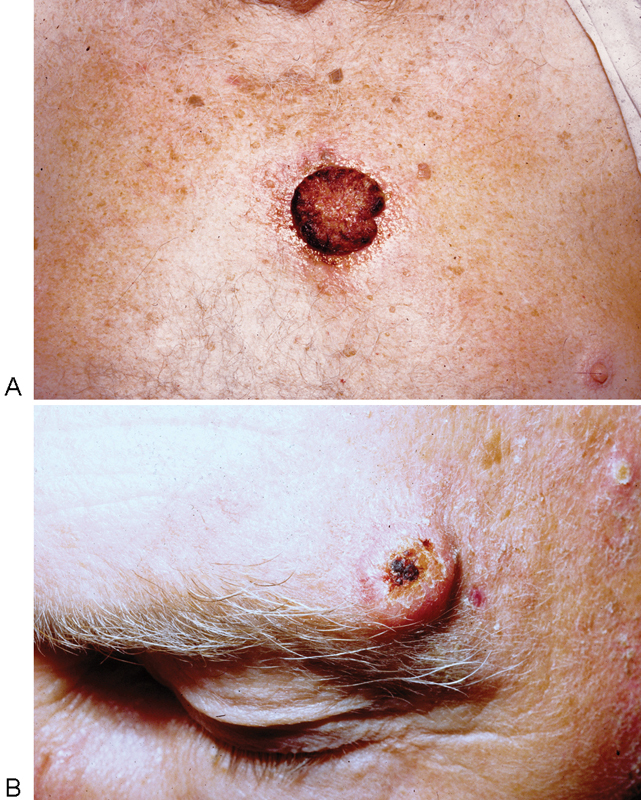
(A) Squamous cell carcinoma. (B) Squamous cell carcinoma, keratoacanthoma type.
Treatment is based on several factors that include location, size, histologic type, and if there is perineural or angiolymphatic involvement. Treatment includes ED&C with or without cryotherapy, wide local excision, and Mohs micrographic surgery. Medical therapy with imiquimod 5% may be used for SCC-IS. In patients who are poor surgical candidates, radiation therapy may be considered. Low-dose retinoids may be used as prophylaxis in solid organ transplant patients with multiple nonmelanoma skin cancers.
Melanoma
Melanoma is found in Caucasian individuals, and its incidence continues to increase, with a predicted doubling every 10 to 20 years.1 Despite the increase in incidence, mortality from melanoma has slowed due to improved surveillance. Though rare, melanomas can be seen in darkly pigmented individuals, but commonly occur in non-sun-exposed areas such as the sole of the foot or on mucosal surfaces.
The development of melanoma depends on both environmental and genetic factors, including intermittent, intense sun exposure, number of sunburns, tanning bed use, fair skin, red hair, and a prior history of dysplastic nevi or melanoma. Familial melanomas are associated with mutations in CDKN2A.
Surveillance for melanoma involves monitoring for asymmetry, an irregular border, multiple colors, diameter > 6 mm, evolution, and a family history (ABCDEFs of melanoma). Superficial spreading melanoma is the most common subtype, accounting for 60 to 70% of all melanomas1 (Fig. 12A). This subtype, which is characterized by slow radial growth followed by more rapid vertical growth, presents as an irregular macule or patch on men's trunk and women's legs. Nodular melanoma, a more aggressive subtype, comprises 15 to 30% of melanomas1 (Fig. 12B). In contrast to the other types of melanoma, the nodular subtype bypasses the radial growth phase and tends to be diagnosed at a later stage. Other less common forms of melanoma include lentigo maligna melanoma (melanoma in situ), which arises on chronically sun-damaged skin; acral lentiginous melanoma, which is more common in African Americans and Asians; amelanotic melanoma; and desmoplastic melanoma, which is a highly infiltrative and aggressive form. The greatest prognostic indicator for melanoma is the depth (Breslow's thickness) at the time of diagnosis. New histologic and clinical criteria that also seem to factor in prognosis include ulceration and number of mitoses.
Fig. 12.
(A) Superficial spreading malignant melanoma. (B) Nodular malignant melanoma.
Wide local excision is the mainstay of treatment for melanoma, although Mohs surgery by an experienced surgeon may also be performed. Depending on the Breslow's thickness and stage, sentinel lymph node biopsy (SLNB) may be warranted. Although SLNB has been shown to improve disease-free survival, it does not improve overall survival.1 Adjunctive therapy with radiation, chemotherapy, or immunotherapy (BRAF inhibitors, CTLA-4 inhibitors) has improved the survival rate of patients who are poor surgical candidates and of those with advanced disease and metastasis.
Conclusion
A large number of dermatologic lesions are encountered by plastic surgeons. Although diagnosis may often present a challenge, proper identification and an understanding of the natural history of these lesions are essential for appropriate management. In this article, we have presented a baseline differential for epidermal/dermal, infectious, pigmented, and malignant cutaneous lesions that are commonly encountered in practice. Diagnosis relies on the history of the lesion, clinical appearance, associated signs and symptoms, and occasionally its histopathology. Evaluation of these clues will help guide treatment, both medical and surgical, and ultimately lead to successful medical and cosmetic outcomes.
References
- 1.Bolognia J L, Jorizzo J L, Schaffer J V. Philadelphia: Elsevier Saunders; 2012. Dermatology. 3rd ed. [Google Scholar]
- 2.Hafner C, Vogt T. Seborrheic keratosis. J Dtsch Dermatol Ges. 2008;6(8):664–677. doi: 10.1111/j.1610-0387.2008.06788.x. [DOI] [PubMed] [Google Scholar]
- 3.Sari R, Akman A, Alpsoy E, Balci M K. The metabolic profile in patients with skin tags. Clin Exp Med. 2010;10(3):193–197. doi: 10.1007/s10238-009-0086-5. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick T B, Wolff K, Johnson R A, Suurmond D. New York: McGraw-Hill; 2005. Fitzpatrick's Color Atlas and Synopsis of Clinical Dermatology. 5th ed. [Google Scholar]
- 5.Thomas V D, Snavely N R, Lee K K, Swanson N A. New York: McGraw-Hill; 2012. Benign epithelial tumors, hamartomas, and hyperplasias; p. 1334. [Google Scholar]
- 6.Pochi P E, Strauss J S, Downing D T. Age-related changes in sebaceous gland activity. J Invest Dermatol. 1979;73(1):108–111. doi: 10.1111/1523-1747.ep12532792. [DOI] [PubMed] [Google Scholar]
- 7.Ramcharan R, Midha R. Clinical presentation and physical examination. Neurosurg Clin N Am. 2004;15(2):125–132. doi: 10.1016/j.nec.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Christoffersen M, Frikke-Schmidt R, Schnohr P, Jensen G B, Nordestgaard B G, Tybjærg-Hansen A. Xanthelasmata, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ. 2011;343:d5497. doi: 10.1136/bmj.d5497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noël B. Premature atherosclerosis in patients with xanthelasma. J Eur Acad Dermatol Venereol. 2007;21(9):1244–1248. doi: 10.1111/j.1468-3083.2007.02252.x. [DOI] [PubMed] [Google Scholar]
- 10.Yates B, Que S K, D'Souza L, Suchecki J, Finch J J. Laser treatment of periocular skin conditions. Clin Dermatol. 2015;33(2):197–206. doi: 10.1016/j.clindermatol.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 11.Urban C D, Cannon J R, Cole R D. Eruptive syringomas in Down's syndrome. Arch Dermatol. 1981;117(6):374–375. [PubMed] [Google Scholar]
- 12.Pahud B A, Ault K A. The expanded impact of human papillomavirus vaccine. Infect Dis Clin North Am. 2015;29(4):715–724. doi: 10.1016/j.idc.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Smith L, Angarone M P. Sexually transmitted infections. Urol Clin North Am. 2015;42(4):507–518. doi: 10.1016/j.ucl.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Ramdass P, Mullick S, Farber H F. Viral skin diseases. Prim Care. 2015;42(4):517–567. doi: 10.1016/j.pop.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Chi C C, Wang S H, Delamere F M, Wojnarowska F, Peters M C, Kanjirath P P. Interventions for prevention of herpes simplex labialis (cold sores on the lips) Cochrane Database Syst Rev. 2015;8(8):CD010095. doi: 10.1002/14651858.CD010095.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dadabhoy I, Butts J F. Parasitic skin infections for primary care physicians. Prim Care. 2015;42(4):661–675. doi: 10.1016/j.pop.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Avci O, Tanyildizi T, Kusku E. A comparison between the effectiveness of erythromycin, single-dose clarithromycin and topical fusidic acid in the treatment of erythrasma. J Dermatolog Treat. 2013;24(1):70–74. doi: 10.3109/09546634.2011.594870. [DOI] [PubMed] [Google Scholar]
- 18.Akram H, Jing S S, Murahari S, David K. Cutaneous horn: case report. Br J Oral Maxillofac Surg. 2011;49(1):73–75. doi: 10.1016/j.bjoms.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 19.Xu P, Gu L, Yao X, Wu X, Chen X. A giant cutaneous horn on the eyebrow. JAAD Case Rep. 2015;1(5):295–297. doi: 10.1016/j.jdcr.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stern R S; PUVA Follow-Up Study. The risk of squamous cell and basal cell cancer associated with psoralen and ultraviolet A therapy: a 30-year prospective study J Am Acad Dermatol 2012664553–562. [DOI] [PubMed] [Google Scholar]


