Abstract
Background
Previous studies on end-of-life (EOL) care among patients with chronic kidney disease (CKD) have been largely limited to White hemodialysis patients. In this study we sought to explore racial variability in EOL communication, care preferences and advance care planning among patients with advanced CKD prior to decisions regarding initiation of dialysis.
Methods
We performed a cross-sectional study between 2013 and 2015 of Black and White patients with Stage IV or V CKD (per the Modified Diet in Renal Disease estimation of GFR < 30 ml/min/1.73m2) from two academic centers in Boston. We assessed experiences with EOL communication, advance care planning, EOL care preferences, hospice knowledge, spiritual/religious and cultural beliefs, and distrust of providers.
Results
Among 152 participants, 41% were Black. Black patients were younger, had less education, and lower income than White patients (all p < 0.01). Black patients also had less knowledge of hospice compared to White patients (17% vs. 61%, p < 0.01). A small fraction of patients (8%) reported having EOL discussions with their nephrologists and the majority had no advance directives. In multivariable analyses, Blacks were more likely to have not communicated EOL preferences (adjusted Odds Ratio aOR, [95% Confidence Interval CI] 2.70 [1.08, 6.76]) and more likely to prefer life-extending treatments (aOR, 3.06 [1.23, 7.60]) versus Whites.
Conclusions
As Black and White patients with advanced CKD differ on EOL communication, preferences, and hospice knowledge, future efforts should aim to improve patient understanding and promote informed decision-making.
Keywords: Racial disparities, end-of-life, chronic kidney disease
Introduction
Although survival rates for patients with chronic kidney disease (CKD) and end-stage renal disease (ESRD) initiating hemodialysis (HD) have slightly improved, only 54% of people who start HD are alive within three years.[1] Furthermore, patients with ESRD typically experience intensive patterns of health care utilization at the end of life as opposed to comfort care.[2] For instance, many who choose dialysis also receive other life-sustaining treatments such as cardiopulmonary resuscitation and mechanical ventilation despite a poor likelihood of survival.[3-5] As communication about care desired at the end of life is one of the best ways for people to preserve their wishes, early goals of care discussions are especially salient in this population.[6-9]
Previous literature on end-of-life (EOL) conversations and preferences for care among patients with CKD has largely been limited to patients on maintenance HD.[6,10-12] Despite national guidelines and initiatives to improve EOL care for nephrology patients, recent studies have demonstrated that patients infrequently engage in prognostic and EOL discussions with their nephrologists.[6,7,13] Furthermore, studies of advance care planning (ACP), defined as the process where individuals plan ahead for care desired if they were to become incapacitated, and patients with kidney disease have been conducted almost exclusively among White patients.[6,14-16] Several disciplines of healthcare have demonstrated how minority racial-ethnic groups typically experience less access to palliative care services, receive more life-sustaining therapies and are less likely to use hospice during the final months of life compared to other racial-ethnic groups.[17-21] While poor education, spirituality, and trust of the healthcare system likely contribute to disparities in patterns of care at the end of life, such relationships have not been evaluated in CKD patients.[21,22] In this study we sought to explore whether racial variability exists with regards to EOL communication, care preferences, and ACP among patients with advanced CKD prior to initiation of dialysis.
Methods
Setting and study participants
We performed a cross-sectional study between August 2013 and February 2015 among patients with Stage IV or V CKD (as defined by the Modified Diet in Renal Diseases[23] estimation of GFR < 30 ml/min/1.73m2). Patients were recruited from outpatient nephrology clinics associated with two academic centers in Boston, Massachusetts. Eligibility included age 45 years or older, English-speaking and self-report of Black or White race. Patients were excluded if they had a known history of dementia or were found to have severe cognitive deficit (as determined by eight or more errors on the Short Portable Mental Status Questionnaire).[24] Patients were also excluded if they were listed for kidney transplantation as the illness trajectory and prognoses for such patients differs significantly from those without this treatment option. The Institutional Review Boards at Partner's Healthcare and Boston Medical Center approved this study.
Data collection
All study personnel underwent training in conducting structured patient interviews using study questionnaires. All interviews were performed in a quiet and private room in the outpatient clinic at a scheduled routine visit. Patient demographic information including age, gender, race, ethnicity, formal level of education, annual income, and health insurance status were ascertained through study questionnaires. We reviewed electronic medical records for comorbid conditions and the Charlson Comorbidity Index (CCI) score was calculated.[25]
Outcomes
The primary outcome was prior EOL communication with any providers (yes versus no). Additional outcomes included, EOL communication with nephrologists (yes versus no), EOL communication with family members or friends (yes versus no), ACP (possession of healthcare proxy [HCP] and Do-Not-Rescusitate [DNR] forms or living wills; yes versus no) and EOL preferences. As previously done in research investigating EOL care in seriously ill patients [26], we ascertained EOL preference for resuscitation (yes versus no) as well as life-extending care (comfort versus life-extending) and site of death (hospital versus home) at the end of life. Using the outpatient electronic medical record (EMR), we verified whether DNR orders, living wills, and HCP forms had been completed for all patients. For patients who had evidence of these forms in the EMR, they were given credit for having such documentation even if this had not been reported. For any missing information in the EMR, we deferred to the patient's response as confirmation.
We collected secondary outcomes including spiritual/religious beliefs, cultural beliefs, and distrust of healthcare providers and their influence on EOL preferences using single item measures (yes versus no) during patient interviews. In addition, hospice knowledge was determined by content analysis of an open-ended follow-up item for participants who had heard of the term ‘hospice’ (“Since you have heard of hospice, what does this mean to you in your own words?”). Three members of the study staff subsequently and independently categorized responses into “poor knowledge”, “partial knowledge”, or “good knowledge”.[27] The third study staff member was also used to adjudicate any disagreements in categorization.
Statistical analyses
Descriptive participant characteristics are presented using proportions for categorical variables and means (standard deviations) for continuous variables. We tabulated the proportions of participants who had a history of EOL discussion with their healthcare providers/families, preference for resuscitation, EOL care and site of care, and possession of HCP form, DNR order or living will. We also ascertained whether culture, religion/spirituality and distrust of healthcare providers had an impact on preferences. Hospice knowledge response categories were dichotomized into poor or partial knowledge versus good knowledge.
We used univariate logistic regression analysis to identify statistically significant racial differences in EOL preferences and communication. Models were examined for each of five outcomes where statistically significant racial differences existed in univariate analysis including: 1) No communication of EOL preferences with family; 2) No possession of a HCP form; 3) No possession of DNR order or living will; 4) Preference for EOL life-extending care; and 5) Preference for site of death. Collinearity for demographic variables, hospice knowledge, and study site with race were tested using the variance inflation factor. Multivariable logistic regression analyses were then performed to identify significant predictors of each of the five outcomes. As the distribution of elderly patients differed among racial groups, we stratified the final analyses by age (< 65 years versus ≥ 65 years). In addition, we stratified the final analysis of hospice knowledge by level of education. All analyses were performed using SAS version 9.2 (Cary, NC). Statistical significance was determined by p-values < 0.05.
Results
Patient characteristics
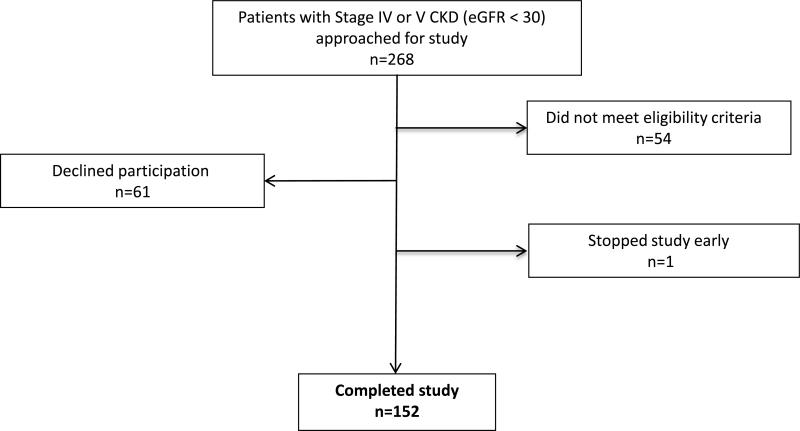
A total of 268 patients were approached for study enrollment. Fifty-four patients were ineligible, 61 patients declined participation, and one patient stopped the study early (Figure 1). Among 57% of patients who enrolled and completed the study, 41% were Black. Black patients were younger compared to White patients with a mean age (± SD) of 66 (± 11) years versus 70 (± 10) years (p = 0.01) (Table 1). A higher proportion of Black patients had an annual income < $30,000 and a lower level of education attainment (both p < 0.01). There was no significant difference in mean CCI score between the two racial groups.
Figure 1.
Study Enrollment
Table 1.
Patient characteristics
| Total (N=152) | Black (N=63) | White (N=89) | P-Value | |
|---|---|---|---|---|
| Age, years1 | 69 (11) | 66 (11) | 70 (10) | 0.01 |
| Age ≥ 65, years (%) | 68 | 56 | 78 | < 0.01 |
| Hispanic ethnicity (%) | 2 | 3 | 1 | 0.16 |
| Male (%) | 61 | 52 | 66 | 0.08 |
| Less than high school education (%) | 16 | 32 | 4 | < 0.01 |
| Income less than $30,000 (%) | 47 | 68 | 31 | < 0.01 |
| Health insured (%) | 98 | 97 | 99 | 0.36 |
| Charlson comorbidity index score1 | 7 (2) | 7 (2) | 7 (2) | 0.96 |
| EOL2 Communication | ||||
| No communication of EOL preferences with any healthcare provider EOL (%) | 77 | 76 | 78 | 0.85 |
| No communication of EOL preferences with kidney doctor (%) | 92 | 87 | 96 | 0.06 |
| No communication of EOL preferences with family members or friends (%) | 38 | 54 | 27 | < 0.01 |
| Advance Care Planning | ||||
| No completion of healthcare proxy form (%) | 39 | 51 | 30 | 0.01 |
| No completion of DNR3 form or living will (%) | 68 | 78 | 62 | 0.04 |
| EOL Preferences | ||||
| Prefer to be resuscitated in current health state (%) | 89 | 90 | 87 | 0.57 |
| Prefer to extend life versus comfort care if critically ill (%) | 38 | 56 | 25 | < 0.01 |
| Prefer to stay in the hospital versus go home if critically ill (%) | 29 | 43 | 20 | < 0.01 |
Presented as mean (± SD)
EOL = End-of-Life
DNR = Do Not Resuscitate
Hospice knowledge
All White patients (n = 89) and 75% of Black patients (n = 47) reported that they had heard of “hospice” and responded to the query about the meaning of hospice. Examples of these patients’ verbatim descriptions of the meaning of hospice are listed in Table 2. We determined 17% (8/47) of Black patients’ and 61% (54/89) of White patients’ responses as exhibiting good knowledge of hospice (p < 0.01). In addition, when stratified by level of education, we observed that among those who graduated high school (n = 128), racial differences persisted (p < 0.01), but these differences were not significant among those who had not graduated high school (n = 24, p = 0.42).
Table 2.
| Poor Knowledge | Partial Knowledge | Good Knowledge |
|---|---|---|
| “It's a place where people who can't take care of their activities of daily living are taken care of.” | “It means that you are seriously ill.” | “It's final care at home or in a suitable setting. It's palliative care.” |
| “The preface to hospital - a type of hospital.” | “You usually have a 6 month window of dying.” | “Hospice is care that people get when they are dying.” |
| “It's where people go to be taken care of after an operation.” | “I don't know what it means. Nothing can be done about the person's situation so they go home and die.” | “It means that its giving care to someone in the end stages of life. It's compassionate care among family that helps someone ease into death without pain. It can be at home if desired.” |
Patient responses to “Since you have heard of hospice, what does this mean to you in your own words?”
17% of Black patients had good knowledge versus 61% of White patients (p < 0.01)
Previous EOL communication
Overall, 77% percent of patients reported never having a prior EOL discussion with any healthcare provider (Table 1). Specifically, 92% of patients reported never having such conversations with a nephrologist. Significantly more Black patients reported not having discussions about EOL preferences with their family members or friends compared to White patients (54% versus 27%, p = 0.01, Table 1). After adjusting for age, education, income, study site, CCI score and hospice knowledge, Black patients were still more likely to not communicate EOL preferences with family members and friends (adjusted Odds Ratio aOR, [95% Confidence Interval CI] 2.70 [1.08, 6.76], Table 3) compared to White patients.
Advance care planning
Two patients reported that they did not have a living will and 14 patients reported having no HCP despite record of these documents in the EMR. There were no differences in patient characteristics between those with and without EMR evidence of ACP documentation. A higher proportion of the Black patients reported that they had not completed DNR orders or living wills and had no evidence of such documentation in the EMR compared to White patients (78% versus 62%, p = 0.04, Table 1). More Black patients also had not completed HCP forms and had no evidence of such documentation in the EMR compared to White patients (50% versus 30%, p = 0.01). In adjusted analyses, there were no significant racial differences.
EOL care preferences
A total of 89% of patients preferred to be resuscitated and there was no difference between Blacks and Whites. At the same time, a higher proportion of Black patients preferred to extend life as opposed to focusing on comfort care compared to White patients (56% vs. 25%, p < 0.01, Table 1). Similarly, Blacks were more likely to prefer spending their final moments of life in a hospital versus Whites (41% vs. 19% p < 0.01). In adjusted analyses, Black patients were more likely to prefer to extend life if critically ill (3.06 [1.23, 7.60], Table 3); however, there was no difference in preference for site of death.
Table 3.
End-of-life life communication, advance care planning, and preferences for Black versus White patients
| End-of-life Preference | Unadjusted OR (95% CI) | Adjusted OR1 (95% CI) | Adjusted OR2 (95% CI) < 65 years | Adjusted OR2 (95% CI) ≥ 65 years |
|---|---|---|---|---|
| No communication of end-of-life preferences with family members of friends | 3.18 (1.61, 6.28)** | 2.70 (1.08, 6.76)** | 3.93 (0.72, 21.61) | 1.91 (0.61, 5.95) |
| No completion of healthcare proxy form | 2.16 (1.04, 4.50)** | 1.03 (0.39, 2.71) | 1.14 (0.22, 5.91) | 0.81 (0.23, 2.79) |
| No completion of living will or DNR3 form | 2.37 (1.21, 4.63)** | 2.13 (0.77, 5.90) | 4.05 (0.27, 59.63) | 1.68 (0.53, 5.33) |
| Prefer to extend life versus comfort care if critically ill | 3.66 (1.85, 7.26)** | 3.06 (1.23, 7.60)** | 9.15 (1.48, 56.74)** | 2.40 (0.74, 7.76) |
| Prefer to stay in the hospital versus go home if critically ill | 2.66 (1.31, 5.40)** | 1.87 (0.71, 4.75) | 6.49 (0.78, 54.15) | 1.45 (0.45, 4.74) |
OR, odds ratio; CI, 95% confidence interval.
Multivariable analyses adjusted for age, education, income, study site, Charlson comorbidity index score, and hospice knowledge
Multivariable analyses adjusted for education income, study site, Charlson comorbidity score, and hospice knowledge, stratified by age of 65
DNR = Do Not Resuscitate
Statistically significant, p < 0.05
In the final models, additional significant predictors included: income (p= 0.03; for EOL communication), study site (p = 0.02; for completion of HCP form), Charlson comorbidity score (p < 0.01; for completion of HCP form) and education (p = 0.01; for site of death). In multivariable analyses stratified by age, younger (< 65 years) Black patients were more likely to prefer life-extending care (9.15 [1.48, 56.74], Table 3) than White patients. However, there were no racial differences in preference for EOL communication, ACP or EOL care preferences among patients ≥ 65 years of age (Table 3).
There were no significant racial differences with regards to the influence of religious/spiritual beliefs, cultural beliefs, and distrust of healthcare providers on preferences for care at the end of life (not displayed).
Discussion
Among patients with advanced CKD not yet on dialysis, few patients reported having discussions about EOL preferences and many had not completed any form of ACP. Black patients were less likely to understand the meaning of hospice compared to White patients. Furthermore, independent of age, education, income, comorbidities, study site and hospice knowledge, Black patients were less likely to communicate EOL preferences with family members and more likely to desire treatment intended to extend life if they were to become critically ill compared to White patients. In particular, younger Black patients were more likely to prefer life-extending care compared to younger White patients.
Our study confirms very low rates of ACP and EOL discussions for patients with CKD with their nephrologists and their other health care providers. Davison et al. showed that 44% of CKD patients had completed a health care proxy or enduring power of attorney and 38% reported having a personal directive; however, most of this cohort had already begun dialysis and was almost exclusively White.[7] Furthermore, despite patients feeling somewhat comfortable discussing EOL issues with family members and healthcare providers, only 33% had spoken with family member/health care proxies and 10% had spoken with nephrologists within the past year about EOL issues. Our findings build upon this knowledge by enrolling a mixed race cohort of patients who had not yet begun dialysis, and by identifying the fact that Black patients in our study were less likely to communicate EOL preferences with their families and more likely to prefer life-extending treatment at the end of life compared to White patients. Factors such as lack of awareness of illness trajectory and prognosis in addition to unrealistic expectations of health statuses likely contribute to poor communication between patients with kidney disease and their families.[28,29] For example, a recent randomized controlled trial of a communication intervention geared specifically toward Black patients with ESRD and their surrogates was particularly effective in improving patient-surrogate congruence and decisional confidence in goals of care.[30] This approach elucidated the complex relationships of health awareness and subsequent emotional burden that often occurs within families. As medical decision-making at the end of life for seriously ill patients can be difficult to predict and lead to traumatic experiences for patients’ families and healthcare providers, the promotion of clear prognostic and ACP communication early in the course of CKD becomes a key strategy for improving delivery of EOL care while simultaneously reducing racial disparities.[31-33]
Differences in EOL treatment preferences and practice patterns between different racial and ethnic groups have been confirmed across several disciplines of healthcare.[34-37] Such differences are inherently a problem if they are driven by misinformation. Fewer Black patients understood the meaning of hospice compared to White patients. Our data also demonstrated the important interplay between hospice knowledge, racial differences, and EOL preferences – a notion that could contribute to subsequent discrepant hospice utilization at the end of life.[34,38] Through treatment of emotional and physical symptoms, hospice care has been proven to significantly improve the transition to death for patients and their families. Less understanding of the benefits of hospice has been associated with more aggressive care at end of life and a lower quality of death.[31] Educational programs for CKD patients and their families have the potential to promote more informed decision-making regarding treatment options at the end of life, better satisfaction with care, and decreased disparities.[15]
We did not find substantial racial differences with regards to all aspects of care desired at the end of life. In adjusted analyses, Blacks and Whites had similar likelihood of completing HCP forms, DNR forms or living wills, and preference for site of death. Differences in nephrology clinic practices as well as illness severity could impact completion of advance directives. For instance, despite national guidelines that recommend the incorporation of ACP into routine clinical practice,[13] none of the study sites had formal protocols for EOL communication or documentation. Factors such as education and income that remained significant predictors of certain EOL outcomes after adjustment may indeed represent social determinants of health that are fixed and unequal between the two races within the CKD population.[39,40] Historically, similar socioeconomic factors have been linked to racial differences in CKD development and progression. Our findings reinforce the need for more awareness in this arena with regards to disparate EOL care. Black patients were also younger than White patients in this cohort and our analyses revealed that racial differences in the outcomes examined were isolated to the younger patients. These findings could reflect ACP efforts traditionally targeted towards frail and older patients and highlight the need for interventions that reach a broader patient population.[2,14,41]
Our study has some limitations. The study population was comprised of Black and White English-speaking patients from two academic centers in the Boston metro area which reduces generalizability. We did not verify documentation of EOL discussions in the EMR as all patients enrolled in the study were cognitively intact without dementia. While it is possible that patients may have misunderstood or not remembered previous EOL discussions, it is unlikely that this phenomenon explained the racial differences we observed. Also, previous work has cited strong religious/spiritual beliefs, culture, and healthcare distrust as catalysts for differences in preferences and between Black and White patients.[21] However, our findings showed no significant racial differences among these factors. We did not collect data on specific religion affiliation and therefore could not determine any overarching themes that would affect EOL preferences or communication relating to this factor. Also, due to the limited diversity of our cohort, we were unable to determine the effect of ethnicity on outcomes. Future research is needed to understand the divergence of our findings from prior work on racial disparities in religion/spiritual beliefs, culture, and healthcare distrust. While this may reflect limitations in the generalizability of our cohort, these observations may also reflect true changes that have transpired over time and/or the possibility that racial disparities in these factors may not be present among CKD patients or in general for patients who have had stable access to medical care (as has been the case in Massachusetts). Additionally, we explored the concept of hospice as a follow-up question only with patients who reported that they were familiar with the term. This could have potentially excluded patients who may have been knowledgeable about the concept despite unfamiliarity with the word hospice. Furthermore, sociocultural factors such as education level could have affected patients’ likelihood of answering a question phrased as ‘Have you heard of...?’ with a ‘yes’ or ‘no’ response. Independent of actual understanding of the meaning of ‘hospice,’ it might be harder for people with a higher level of education to say that they have never heard of this word. Another limitation relates to the cross-sectional study design, which blocks our ability to make stronger causal inferences.
Despite these limitations, this study is the first to our knowledge to investigate and describe racial differences in EOL communication and preferences among pre-dialysis patients with chronic kidney disease. In conclusion, EOL discussions with providers and the rate of ACP are very low for patients with CKD. Black patients are less likely to have had any EOL communication with their families and prefer more aggressive care at the end of life than White patients. At the same time, Black patients in our study have lower hospice knowledge compared to White patients. This may have a large influence on the racial disparities in EOL preferences we observe. These differences have important implications in designing research and clinical care interventions that improve patient understanding, promote better informed decision-making and reduce racial disparities for patients with advanced CKD.
Acknowledgments
We thank Sarah M. Doughtery for her assistance with patient recruitment and data entry. This study was supported by a grant from the American Society of Nephrology Foundation for Kidney Research Ben J. Lipps Research Fellowship Program (PI – Eneanya) and a mentorship grant from the National Institute of Diabetes and Digestive and Kidney Diseases K24-DK094872 (PI - Thadhani).
Footnotes
Conflict of interest: All authors have approved this manuscript for submission. To the best of our knowledge, no conflict of interest, financial or other, exists.
References
- 1.Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, Chen JT, Cope E, Gipson D, He K, Herman W, Heung M, Hirth RA, Jacobsen SS, Kalantar-Zadeh K, Kovesdy CP, Leichtman AB, Lu Y, Molnar MZ, Morgenstern H, Nallamothu B, O'Hare AM, Pisoni R, Plattner B, Port FK, Rao P, Rhee CM, Schaubel DE, Selewski DT, Shahinian V, Sim JJ, Song P, Streja E, Kurella Tamura M, Tentori F, Eggers PW, Agodoa LY, Abbott KC. Us renal data system 2014 annual data report: Epidemiology of kidney disease in the united states. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2015;65:A7. doi: 10.1053/j.ajkd.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wong SP, Kreuter W, O'Hare AM. Treatment intensity at the end of life in older adults receiving long-term dialysis. Archives of internal medicine. 2012;172:661–663. doi: 10.1001/archinternmed.2012.268. discussion 663-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moss AH, Holley JL, Upton MB. Outcomes of cardiopulmonary resuscitation in dialysis patients. Journal of the American Society of Nephrology : JASN. 1992;3:1238–1243. doi: 10.1681/ASN.V361238. [DOI] [PubMed] [Google Scholar]
- 4.Wong SP, Kreuter W, Curtis JR, Hall YN, O'Hare AM. Trends in in-hospital cardiopulmonary resuscitation and survival in adults receiving maintenance dialysis. JAMA internal medicine. 2015;175:1028–1035. doi: 10.1001/jamainternmed.2015.0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saeed F, Adil MM, Malik AA, Schold JD, Holley JL. Outcomes of in-hospital cardiopulmonary resuscitation in maintenance dialysis patients. Journal of the American Society of Nephrology : JASN. 2015 doi: 10.1681/ASN.2014080766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goff SL, Eneanya ND, Feinberg R, Germain MJ, Marr L, Berzoff J, Cohen LM, Unruh M. Advance care planning: A qualitative study of dialysis patients and families. Clinical journal of the American Society of Nephrology : CJASN. 2015 doi: 10.2215/CJN.07490714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davison SN. End-of-life care preferences and needs: Perceptions of patients with chronic kidney disease. Clinical journal of the American Society of Nephrology : CJASN. 2010;5:195–204. doi: 10.2215/CJN.05960809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ (Clinical research ed) 2010;340:c1345. doi: 10.1136/bmj.c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schonwetter RS, Walker RM, Solomon M, Indurkhya A, Robinson BE. Life values, resuscitation preferences, and the applicability of living wills in an older population. Journal of the American Geriatrics Society. 1996;44:954–958. doi: 10.1111/j.1532-5415.1996.tb01867.x. [DOI] [PubMed] [Google Scholar]
- 10.Song MK, Ward SE, Fine JP, Hanson LC, Lin FC, Hladik GA, Hamilton JB, Bridgman JC. Advance care planning and end-of-life decision making in dialysis: A randomized controlled trial targeting patients and their surrogates. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2015 doi: 10.1053/j.ajkd.2015.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bristowe K, Horsley HL, Shepherd K, Brown H, Carey I, Matthews B, O'Donoghue D, Vinen K, Murtagh FE. Thinking ahead--the need for early advance care planning for people on haemodialysis: A qualitative interview study. Palliative medicine. 2015;29:443–450. doi: 10.1177/0269216314560209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tong A, Cheung KL, Nair SS, Kurella Tamura M, Craig JC, Winkelmayer WC. Thematic synthesis of qualitative studies on patient and caregiver perspectives on end-of-life care in ckd. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2014;63:913–927. doi: 10.1053/j.ajkd.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 13.Davison SN, Levin A, Moss AH, Jha V, Brown EA, Brennan F, Murtagh FE, Naicker S, Germain MJ, O'Donoghue DJ, Morton RL, Obrador GT. Executive summary of the kdigo controversies conference on supportive care in chronic kidney disease: Developing a roadmap to improving quality care. Kidney international. 2015;88:447–459. doi: 10.1038/ki.2015.110. [DOI] [PubMed] [Google Scholar]
- 14.Kurella Tamura M, Goldstein MK, Perez-Stable EJ. Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2010;25:237–242. doi: 10.1093/ndt/gfp430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davison SN, Jhangri GS, Koffman J. Knowledge of and attitudes towards palliative care and hospice services among patients with advanced chronic kidney disease. BMJ supportive & palliative care. 2014 doi: 10.1136/bmjspcare-2013-000610. [DOI] [PubMed] [Google Scholar]
- 16.Fried TR, Redding CA, Robbins ML, Paiva AL, O'Leary JR, Iannone L. Development of personalized health messages to promote engagement in advance care planning. Journal of the American Geriatrics Society. 2016 doi: 10.1111/jgs.13934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas BA, Rodriguez RA, Boyko EJ, Robinson-Cohen C, Fitzpatrick AL, O'Hare AM. Geographic variation in black-white differences in end-of-life care for patients with esrd. Clinical journal of the American Society of Nephrology : CJASN. 2013;8:1171–1178. doi: 10.2215/CJN.06780712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnato AE, Chang CC, Saynina O, Garber AM. Influence of race on inpatient treatment intensity at the end of life. Journal of general internal medicine. 2007;22:338–345. doi: 10.1007/s11606-006-0088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jennings B, Ryndes T, D'Onofrio C, Baily MA. Access to hospice care. Expanding boundaries, overcoming barriers. The Hastings Center report. 2003;(Suppl:S3-7):S9–13. S15–21. passim. [PubMed] [Google Scholar]
- 20.Nhpco facts and figures: Hospice care in america. National hospice and palliative care organization; Alexandria, va: Oct, 2014. [Google Scholar]
- 21.Crawley L, Payne R, Bolden J, Payne T, Washington P, Williams S. Palliative and end-of-life care in the african american community. JAMA : the journal of the American Medical Association. 2000;284:2518–2521. doi: 10.1001/jama.284.19.2518. [DOI] [PubMed] [Google Scholar]
- 22.Volandes AE, Paasche-Orlow M, Gillick MR, Cook EF, Shaykevich S, Abbo ED, Lehmann L. Health literacy not race predicts end-of-life care preferences. Journal of palliative medicine. 2008;11:754–762. doi: 10.1089/jpm.2007.0224. For Peer Review. [DOI] [PubMed] [Google Scholar]
- 23.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of diet in renal disease study group. Annals of internal medicine. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 24.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 25.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of chronic diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 26.A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (support). The support principal investigators. JAMA : the journal of the American Medical Association. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 27.Shelkowitz E, Vessella SL, O'Reilly P, Tucker R, Lechner BE. Counseling for personal care options at neonatal end of life: A quantitative and qualitative parent survey. BMC palliative care. 2015;14:70. doi: 10.1186/s12904-015-0063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wachterman MW, Marcantonio ER, Davis RB, Cohen RA, Waikar SS, Phillips RS, McCarthy EP. Relationship between the prognostic expectations of seriously ill patients undergoing hemodialysis and their nephrologists. JAMA internal medicine. 2013;173:1206–1214. doi: 10.1001/jamainternmed.2013.6036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paterson BL. The shifting perspectives model of chronic illness. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2001;33:21–26. doi: 10.1111/j.1547-5069.2001.00021.x. [DOI] [PubMed] [Google Scholar]
- 30.Song MK, Ward SE, Happ MB, Piraino B, Donovan HS, Shields AM, Connolly MC. Randomized controlled trial of spirit: An effective approach to preparing african-american dialysis patients and families for end of life. Research in nursing & health. 2009;32:260–273. doi: 10.1002/nur.20320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. JAMA : the journal of the American Medical Association. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 32.Uhlmann RF, Pearlman RA, Cain KC. Physicians' and spouses' predictions of elderly patients' resuscitation preferences. Journal of gerontology. 1988;43:M115–121. doi: 10.1093/geronj/43.5.m115. [DOI] [PubMed] [Google Scholar]
- 33.Mack JW, Paulk ME, Viswanath K, Prigerson HG. Racial disparities in the outcomes of communication on medical care received near death. Archives of internal medicine. 2010;170:1533–1540. doi: 10.1001/archinternmed.2010.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zheng NT, Mukamel DB, Caprio T, Cai S, Temkin-Greener H. Racial disparities in in-hospital death and hospice use among nursing home residents at the end of life. Medical care. 2011;49:992–998. doi: 10.1097/MLR.0b013e318236384e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loggers ET, Maciejewski PK, Jimenez R, Nilsson M, Paulk E, Stieglitz H, Prigerson HG. Predictors of intensive end-of-life and hospice care in latino and white advanced cancer patients. Journal of palliative medicine. 2013;16:1249–1254. doi: 10.1089/jpm.2013.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hernandez RA, Hevelone ND, Lopez L, Finlayson SR, Chittenden E, Cooper Z. Racial variation in the use of life-sustaining treatments among patients who die after major elective surgery. American journal of surgery. 2015;210:52–58. doi: 10.1016/j.amjsurg.2014.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dillon PJ, Roscoe LA. African americans and hospice care: A narrative analysis. Narrative inquiry in bioethics. 2015;5:151–165. doi: 10.1353/nib.2015.0049. [DOI] [PubMed] [Google Scholar]
- 38.Cagle JG, LaMantia MA, Williams SW, Pek J, Edwards LJ. Predictors of preference for hospice care among diverse older adults. The American journal of hospice & palliative care. 2015 doi: 10.1177/1049909115593936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nicholas SB, Kalantar-Zadeh K, Norris KC. Socioeconomic disparities in chronic kidney disease. Advances in chronic kidney disease. 2015;22:6–15. doi: 10.1053/j.ackd.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruce MA, Beech BM, Sims M, Brown TN, Wyatt SB, Taylor HA, Williams DR, Crook E. Social environmental stressors, psychological factors, and kidney disease. Journal of investigative medicine : the official publication of the American Federation for Clinical Research. 2009;57:583–589. doi: 10.231/JIM.0b013e31819dbb91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the united states. Annals of internal medicine. 2007;146:177–183. doi: 10.7326/0003-4819-146-3-200702060-00006. [DOI] [PubMed] [Google Scholar]