Abstract
The development of sensitive methods for alloantibody detection has been a significant advance in clinical transplantation. However, the complexity of the data from solid phase and crossmatch assays has led to potential confusion about how to use the results for clinical decision making. The goal of this review is to provide a practical guide for transplant physicians for the interpretation of antibody data to supplement consultation with local tissue typing experts. Sources of variability in both the solid phase and crossmatch assay are discussed as are recent data regarding C1q binding antibodies and IgG subclass testing. While definitive approaches to alloantibody testing are not possible with our current knowledge, we outline a pragmatic approach that we hope will enhance clinical management in this area.
Introduction
Despite improvements in patient selection and management, every transplant carries some risk of graft loss. Donor-specific alloantibody (DSA) either present at the time of transplantation or arising de novo posttransplant is a risk factor for antibody mediated rejection (AMR) and potentially allograft loss in almost all types of organ transplants (1-6). Ideally all DSA would be avoided, but this is often impractical in the setting of organ scarcity and recipient sensitization. Instead the clinician must estimate the risk of AMR in each situation, while considering the consequences of remaining on dialysis. Understanding the complexities and limitations of DSA detection techniques is key for making an accurate risk assessment while improving access to transplantation.
The goal of this overview is to provide a practical guide for using solid phase assays and crossmatch (XM) testing. We also provide possible explanations for ambiguous test results and recommendations for further investigation. This guide is not a substitute for meaningful interaction with your local tissue typing laboratory experts because their guidance remains crucial for proper decision making. Our major emphasis is on pretransplant alloantibody assessment in kidney transplant candidates, but the basic principles apply posttransplantation and to other solid organ transplants - particularly heart, lung, and pancreas.
General Principles: The Initial Evaluation
The initial assessment of a potential renal transplant candidate involves HLA typing of the donor and recipient, screening for alloantibody against HLA, and obtaining a history of sensitizing events (previous transplant, blood transfusion, and/or pregnancy). HLA typing ideally includes A; B; C; DRB1; DRB3,4,5; DQB1; DQA; DPB1; and DPA; but this is not always the performed(7). The single antigen bead (SAB) solid-phase [LAB screen (One Lambda) or LifeScreen (LifeCodes-Immucor)] assay are most commonly used as the first line of screening for alloantibody, but multi-antigen screening beads can be used.
Fortunately, many renal transplant candidates—especially in the absence of a sensitizing event—have little or no alloantibody detected on the solid phase assay. These patients usually require no further investigation. However, if the solid phase assay is positive suggesting the presence of alloantibody, further evaluation is necessary. A basic understanding of the technical aspects of the solid phase and XM assays is essential for optimal interpretation.
The solid phase single antigen bead (SAB) assays
The current fluorescent based solid phase assay is able to concurrently distinguish up to 100 different micro particles or beads. Phenotypic or multi-antigen beads contain Class I and Class II antigens from a single cell line, while each SAB contains a single HLA antigen(8). In both cases, the beads contain a unique ratio of different fluorochromes that provide a distinctive signal that is recognized by Luminex® technology(8). The patient's serum is incubated with the solid phase platform (beads) and a fluorescent-conjugated anti-human IgG, which binds to alloantibody bound to its antigenic target. If the multi-antigen beads used for screening are positive, we suggest doing SABs to precisely identify the HLA-antigen to which the patient has alloantibody. For the purposes of this overview, we will mostly discuss SAB testing. The SAB output is a semiquantitative measure of the amount of antibody (total IgG – all subclasses combined) referred to as mean fluorescence intensity (MFI). However, the assay is only FDA approved as a qualitative assay (negative or positive). Determining a negative SAB result is often the single most important aspect of alloantibody testing because it is used for donor selection and calculated panel reactive antibody (cPRA) assignment, yet this can be difficult because results are not dichotomous and depend on laboratory conditions. The MFI threshold to distinguish negative and positive also depends on a particular center's risk tolerance for AMR and clinical context. This MFI cutoff also differs depending on the organ to be transplanted. An MFI of less than 2000 is usually considered negative at our kidney transplant center. We recognize that DSA may be present using this cutoff, but it also increases our patients' access to transplantation. Regardless, an MFI < 1000 in a patient who has not had a sensitizing event is considered negative at most kidney transplant centers.
Crossmatch Testing (9-11)
The XM is considered the final test to determine the safety of moving forward with transplantation, but now sensitive SAB assays have made the virtual crossmatch possible. When SAB testing is completely negative in a patient who has not had a sensitizing event, XM testing is unlikely to add to the AMR risk assessment. The XM is most valuable whenever there is SAB positivity. Different XM techniques exist and each has its own set of limitations and varied sensitivity.
The complement-dependent cytotoxicity crossmatch (CDC-XM) was historically performed routinely. For this test, donor lymphocytes and recipient serum are mixed with complement. The membrane attack complex forms when alloantibody is cell bound leading to cell lysis. This testing is not sensitive for non-complement binding DSA of low affinity/avidity and therefore the modified T-cell anti-human globulin-enhanced cytotoxicity XM (T-cell AHG CDC) was developed. The addition of AHG to the cytotoxic assay improved its sensitivity, yet its sensitivity is variable. It also does not detect DSA against class II (T cells do not express Class II HLA). The CDC-XM with enriched B cells can be used to detect Class II DSA, but this technique can be technically difficult and AHG treatment is not recommended.
The flow cytometric crossmatch (Flow XM) has improved sensitivity for the detection of both complement and non-complement binding class I and Class II DSA as compared to the gold-standard CDC-XM(10). This method also reduces the subjectivity and inter-observer variability associated with the CDC-XM because it is reported as mean channel shift rather than positive or negative result based on visual interpretation. Therefore to best estimate a patient's risk for AMR, we suggest using the flow XM as adjunct to SAB, as opposed to other methods. This is our personal recommendation. The international Antibody Consensus Group supported by the Transplantation Society has not made recommendations for or against the use of CDC versus flow XM (11).
The flow XM is performed by incubating donor lymphocytes, recipient serum, and a fluorescent labelled anti-human immunoglobulin together and running them through a flow cytometer (9). The level of fluorescence is proportional to the amount of antibody bound to the cell. Markers with different fluorochromes are also added to separate T and B cell reactivity. This is important because class I anti-HLA antibodies bind both T and B cells, while antibodies against Class II antigens usually bind only B cells. Activated donor T cells express class II antigen in the presence of certain cytokines, which is a consideration in some cases (12).
Identifying a transplant that is low risk for AMR
With every transplant comes some risk, but when the SABs are completely negative, especially if the patient has not had a sensitizing event; the risk for AMR is exceedingly low. However, it is important to recognize that not uncommonly either the SAB or XM are falsely positive for anti-HLA alloantibody. In these situations, the risk of AMR is also low Table 1.
Table 1. Risk Stratification of Antibody Mediated Rejection based on the Combination of Single Antigen Beads and Flow Cytometric Crossmatch.
| Risk for AMR | Considerations | SAB results | Flow XM results | Further evaluation |
|---|---|---|---|---|
| Low | No DSA present | Negative | Negative T/B Cell | None |
| Alloantibody towards denatured HLA | Positive | Negative T/B Cell | Acid Treatment of SAB. If still positive – the alloantibody is towards denatured HLA | |
| Laboratory factors | Positive | Negative T/B Cell | Consult with HLA laboratory | |
| Recent anti-CD 20 treatment | Negative | Positive T and/or B-cell | Pronase treatment of donor lymphocytes | |
| Auto-antibodies | Negative | Positive T and/or B–cell | Flow auto-crossmatch | |
| High | DSA present | Positive | Positive B-cell | Consider testing for further risk stratification* |
| Prozone effect | Weakly positive | Strongly Positive B-cell | Repeat SAB with 1:8 serum dilution to identify possible prozone | |
| Incomplete donor/recipient HLA typing | Negative | Positive B-Cell | Be sure that the donor and recipient have been typed for DQ alpha and DP | |
| SAB does not include donor HLA antigen | Negative | Positive B-Cell | If SAB does not include donor antigen, use supplemental SAB kit or another SAB vendor | |
| Alloantibody to shared epitope | Weakly positive | Positive B-Cell | Review SAB epitope binding patterns with HLA expert | |
| Uncertain | Low HLA expression on donor cells (ex. Cw) | Positive | Negative B-Cell | Consult with HLA laboratory |
| DSA with low affinity/avidity | Positive | Negative B-cell | None | |
| Non-HLA antibody | Weakly positive or negative | Positive T and/or B-cell | Consider checking for non-HLA antibody |
The risk of AMR depends on several factors, but mostly depends on SAB and XM testing in clinical context. Ancillary testing including acid treatment of SAB, auto-flow XM, and serum dilution among others can provide additional information for risk stratification. Key: AMR: antibody mediated rejection, SAB: single antigen beads, DSA: donor specific antibody, Flow XM: Flow cytometric crossmatch, HLA: Human leukocyte antigen.
Further risk stratification includes DSA quantification, C1q binding ability, and IgG subclass identification if indicated.
Alloantibody to denatured HLA
The SAB assay does not measure antibody directly, but rather measures the binding of antibody towards an antigen, which is made up of multiple epitopes. This is essential to conceptualize when interpreting SAB results. When the HLA antigen is attached to the bead, a conformational change can expose cryptic binding sites that are otherwise not accessible on donor cells (13-17) (15, 16). Alloantibody binding to these denatured rather than intact HLA antigens leads to SAB positivity, yet the flow XM will be negative. Recognizing this phenomenon is valuable because antibodies toward denatured antigen alone are not clinically relevant and by making the corresponding HLA antigen acceptable for organ offers increases a patient's access to transplantation. One way of detecting these antibodies is to treat the SABs with acid to denature all HLA antigens. If the antibody only binds denatured antigen, the SAB result will remain positive despite acid-treatment (16). Few studies have been done on this subject, but 21-39% of patients are thought to have at least 1antibody towards a denatured antigen (14, 17). These antibodies have only been reported to be directed towards class I HLA and are not associated with previous sensitization (14). Transplant recipients with alloantibody exclusively towards denatured antigen appear to have similar long term allograft survival as compared to transplant recipients no DSA (13, 17).
Laboratory factors
Occasionally the SAB test is mildly positive to multiple antigen specificities, yet the patient has not had a sensitizing event. Likewise, the MFI may be 800 on 1 occasion and 1200 the next. These results to do not necessary indicate that the patient has alloantibody or even that there has been an increase in alloantibody. Inter and intra laboratory variability and background SAB fluorescence can sometimes lead to these results. The SAB assay is only semi-quantitative, and the variation in MFI has been reported as high as 62%, especially when the MFI is relatively low (1000-3000) (18).
Laboratory variability exists because of differences in the SAB product itself depending on the bead manufacturer, batch, or lot (19-21). Manufacturers have different antigen sources, distinctive specificity representation, and varied antigen density on the beads [18]. Even with identical product; intra-laboratory variability can occur depending on laboratory personnel, reagents, equipment, and conditions (19, 20, 22). As with any test using flow fluorescent technology there is also background fluorescence. Laboratories validate their assays with clearly defined positive and negative controls to compensate for this, yet it is important to at least consider. Whenever it is suspected that laboratory factors are contributing to positive SAB results, it is important to consult with your local tissue typing expert for advice.
Nonspecific binding on donor lymphocytes: Recent anti-CD20 treatment or “auto-antibodies”
A false positive flow XM can occur with nonspecific binding of IgG to Fc receptors by factors in recipient serum. Anti-CD20 monoclonal antibody (rituximab) has most commonly been implicated. Pre-treatment of donor lymphocytes with pronase can be helpful in removing the effect of CD 20 binding (23). Treatment of donor cells with pronase is only recommended when needed because it can interfere with the donor HLA expression, which can lead to unreliable results(24). Other unidentified substances or “auto-antibodies” in recipient serum can also occasionally lead to nonspecific binding to Fc receptors, and an auto-flow XM (recipient lymphocytes and serum) can provide clues to this phenomenon (25). The long term significance of an isolated auto-flow XM has not been thoroughly studied in the era of sensitive testing for anti-HLA antibody. Our unpublished single center experience has been that non-sensitized patients with negative SAB tests and positive donor/recipient flow XM thought secondary to auto-antibody (positive auto flow XM) have short-term outcomes comparable to recipients who have a pretransplant negative B flow XM.
Identifying a transplant that is high risk for AMR
When a patient has a history of a sensitizing event, SAB testing is positive for DSA, and the flow XM is positive; it is obvious the patient is at higher risk for AMR. But there are also high risk situations that are not as apparent when looking at SAB tests alone Table 1. Whenever a patient is sensitized (especially highly sensitized ex. cPRA >80%) you need to have a heightened concern for AMR, and it is important to consider situations in which the virtual crossmatch is falsely negative to avoid an unanticipated positive final flow XM. For this reason, we suggest consulting with the HLA laboratory whenever your patient is highly sensitized.
Prozone effect
High levels of anti- HLA antibody with strong affinity and avidity can saturate the solid phase platform or interfere with alloantibody binding to the beads leading to SAB results that are lower than expected for a particular antigenic specificity. This is referred at the prozone or hook effect. External substances such as IgM antibody(26), intravenous immunoglobulin, antithymocyte globulin (27), immune complexes, and complement (28, 29) can interfere with antibody binding to the bead or the secondary detection agent and lead to this phenomenon(30, 31). This effect does not necessarily affect all antigen specificities for a particular patient and is mainly a consideration for highly sensitized patients (cPRA >80%). In 1 highly sensitized cohort studied, 71% had at least 1 anti-HLA antibody specificity demonstrating a prozone(31). However, this amounted to only 0.5% of the total SAB tested.
Serum treatment with EDTA/dithiothreitol, heat, or hypotonic dialysis treatment (29, 30) can mitigate the prozone effect somewhat. These treatments are not part of the SAB manufacturer's standard operating procedure, and are therefore not routinely recommended. These treatments can also non-uniformly dilute the sample making the MFI results less reproducible.
The most reliable way to recognize this effect is to do a serum dilution. If the MFI does not decrease linearly as expected, the prozone effect should be suspected. For example, a patient with a cPRA of 95% has an MFI of 800 to B44, but repeat SAB testing after a 1:8 serum dilution demonstrates an MFI result of 3000. We routinely do a 1:8 serum dilution in all patients with cPRA of greater than 80% who are eligible for a deceased donor transplant. We then consider antigens to which a prozone effect exists unacceptable for transplantation. We recognize that further serum dilution is needed to obtain the antibody titer, which is optimal to determine the level of antibody. However, in most instances the detection of prozone alone (not antibody titer) is sufficient to consider the transplant high risk.
Incomplete donor/recipient HLA typing
An unexpected final positive crossmatch can occur if the donor and/or recipient are not completely typed for HLA. This is especially a consideration for highly sensitized transplant candidates. As mentioned above, UNOS does not currently require the reporting of DQA or DP typing, yet 1.6%-21.6% of transplant candidates have alloantibody towards DQA and 6.6-33.7% have alloantibody towards DP antigens(7) according to a survey of the UNOS Histocompatibility Committee members. The international Antibody Consensus Group supported by the Transplantation Society recommends that donor typing for HLA-A,B,C, DRB1,DRB3,DRB4,DRB5, DQA,DQB, DPA, and DPB be performed for all potential recipients enrolled in paired exchange registries(11). This group also recommends that DSA be consistently negative against the above antigens to rely on a virtual cross-match alone(11).
SABs do not include donor HLA antigen
Although the beads in the SAB assay include most potential donor HLA antigens, it is not entirely comprehensive. Just as it is important to ensure that donor typing is accurate, it is important that the donor antigen is represented on the SABs. If the donor antigen is not represented in the particular kit used, then it may be worthwhile using a different vendor for that particular patient. Supplemental kits are also available if needed.
Shared epitopes
Alloantibody can bind a shared epitope on multiple antigens resulting in the positivity of more than 1 bead (19, 32-34). The strength of this antibody would be diluted and underrepresent its clinical importance if the donor cell only has 1 of these antigens. This is most relevant for alloantibody towards public epitopes present such as those on HLA Bw4 or Bw6 (11, 20). The HLA laboratory can identify whether it appears that an antibody is present towards a shared epitope. The flow XM would also be positive in this scenario.
Uncertain risk for AMR
Historical Alloantibody
Careful attention to the patient's sensitization history can provide clues about previous HLA antigen exposure, specifically donor typing from a previous transplant or paternal HLA typing in the setting of pregnancy. Furthermore, many sensitized patients have historically positive SAB results. Notably, the peak MFI of a particular DSA is most predictive of AMR and graft loss, even if it is a historical measurement (35). The risk of AMR in the setting of historically positive DSA, yet negative crossmatch is not known. To minimize the risk of AMR many transplant centers avoid HLA antigens to which the patient has been previously exposed or has had historical alloantibody.
Low HLA expression on donor cells
Regardless of the strength of alloantibody, without an antigenic target; the risk of AMR is generally low. Occasionally, the HLA expression on donor cells is low or at least different than that represented on the beads. Low expression of HLA Cw and DP is very common, but occasionally other HLA antigens have low expression(20). Although the risk to undergo transplantation is generally low, it is unclear whether the HLA expression could change during an inflammatory event, for example. Low HLA expression should be considered when the SABs are positive, but flow XM and testing for alloantibody towards denatured antigen is negative. Although there are not readily available tests to determine HLA expression on the intended donor cells, occasionally a XM can be done with a surrogate donor (a different donor with same HLA), which would be positive.
DSA with low affinity/avidity
Even if donor HLA is expressed, sometimes DSA is of low enough affinity and avidity that it does not produce a positive flow XM. Although ideally all DSA would be avoided, it is not always possible. Although the presence of DSA in the setting of positive CDC or T-cell AHG is associated with AMR and allograft loss, the significance of DSA with low affinity/avidity with a corresponding negative flow XM is not as clear. If transplantation is performed in this setting, frequent early posttransplant DSA monitoring may be helpful.
Non-HLA antibodies
Sensitized transplant recipients of kidney transplants from HLA identical siblings have inferior 10-year allograft survival as compared to non-sensitized recipients(36) and specific cases of AMR after donation from an HLA identical sibling have been reported(37). Although these reports suggest a role of non-HLA antibodies in AMR, the significance of these antibodies completely independent of alloantibody towards HLA remains unclear.
Testing for non- HLA antibodies has historically been labor intensive and not validated. Most non-HLA antibodies are expressed on endothelial cells and not lymphocytes. Some of the antigenic targets on the endothelial cell that have been studied includes: anti-vimentin, anti-major histocompatibility I related chain A, anti-major histocompatibility I related chain B, perlecan, Kα-tubulin, protein kinase C, and anti-angiotensin A1 receptor among others (38, 39) (40-42) (43) (44-47) . An endothelial XM has also been developed recently (XM-ONE®; AbSorber AB, Stockholm, Sweden)(48, 49). Antigen targets other than those present on the endothelial cell are less well studied and include anti-myosin, anti-nuclear, anti-smooth muscle, anti-nucleoprotein, anti-DNA, anti-cytoplasmic, and anti-mitochondrial among others(38, 50).
The study of non-HLA antibody was previously limited by the lack of concurrent sensitive testing for anti-HLA antibodies and small numbers of patients. The true prevalence of non-HLA antibodies, their relationship to allograft pathology in the absence of anti-HLA antibody, and their mechanism of action remains unclear; thus routine testing for them cannot be recommended currently. That being said, if a sensitized patient has AMR without detectable anti-HLA DSA, testing for non-HLA antibodies using the few commercially available assays is a consideration.
Not all DSA is the same: Risk stratification in the setting of known DSA
Although it is advantageous to completely avoid DSA, it is not always possible given a patient's sensitization. Patient survival has been shown to be improved with positive XM transplantation and desensitization as compared to waiting on dialysis for a negative XM transplant (51). For this reason, some programs accept the potential risk for AMR and proceed to transplantation in the setting of known DSA. Not all DSA is the same and its pathogenicity remains difficult to predict. Understanding DSA characteristics beyond positive and negative can help further stratify the risk of AMR.
Alloantibody quantification
Although the current SAB assay is FDA approved as a qualitative assay for alloantibody (positive versus negative) detection, it has been used clinically as a semiquantitative assay to estimate the amount (strength and avidity) of anti-HLA antibody (52, 53) and attempt to assess posttransplant risk. Numerous groups have shown that a higher DSA MFI and/or XM has been associated with increased AMR and allograft loss (35, 52, 53)but the correlation between MFI and these outcomes is far from precise. Another way of determining the strength and avidity of alloantibody is by obtaining the antibody titer. This is especially important in patients with prozone as described above, but may be helpful in any patient with alloantibody. The antibody titer is determined by doing serial dilutions. The dilution at which antibody is no longer detected is considered its titer (31). Figure 1 shows a comparison between neat MFI, serum dilutions, C1q MFI, and the MFI of EDTA treated samples in a cohort of sensitized patients. Obtaining the antibody titer is clearly a more reliable means of quantifying antibody strength and avidity as compared to MFI alone in highly sensitized transplant candidates because of the limitations of the SAB assay (31), yet it remains unclear whether a higher antibody titer is more strongly correlated with AMR and allograft loss than MFI alone.
Figure 1. Comparison of the strength of DSA using serial dilutions, C1q binding, and EDTA Treatment.
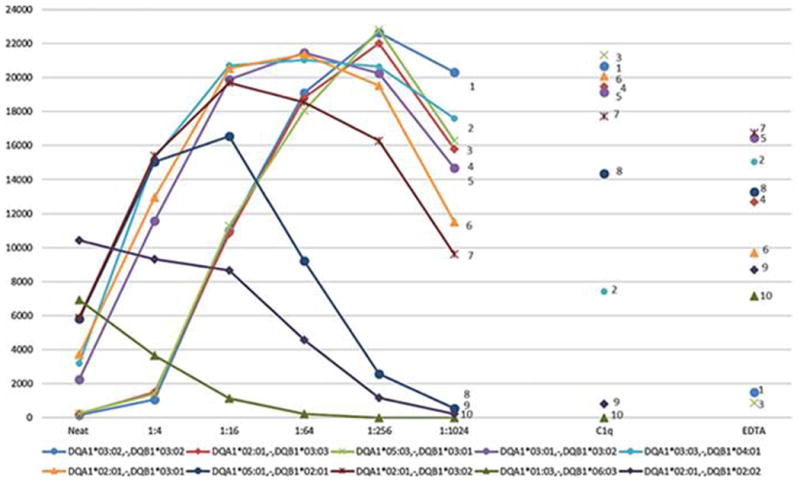
The disadvantage of determining antibody titer is the increased cost and labor involved with doing multiple tests, but this is not always needed. Our personal recommendation is to perform only one serum dilution in highly sensitized patients at baseline and as needed to detect prozone. The information can be used when assigning unacceptable antigens and for future reference because the mere presence of prozone indicates high risk for transplantation. Serial serum dilutions and antibody titer determination can often be reserved to assess the response to antibody depletion therapy in clinical practice or research.
Single versus Multiple DSA
It remains unclear whether there is a difference in long term outcomes depending on the number of DSA the patient has at the time of transplant, independent of the DSA MFI or crossmatch results. Several groups have reported outcomes based on the immunodominant (highest MFI) at the time of transplantation (54, 55), but this approach is complicated because a DSA that appears immunodominant pretransplant may not be immunodominant posttransplant. Other groups have correlated the MFI sum with long term outcomes (52, 56). That approach is also problematic because the SAB is only semi-quantitative. Clearly further study is needed in this area. For now, we suggest using the B flow XM to guide decision making as it provides a summation of the effect of the DSA on the donor cell.
Complement binding DSA
Recent studies have suggested that assessing antibodies for the ability to bind C1q can help differentiate pathogenic from non-pathogenic DSA (57). Complement activation is an important mechanism by which DSA leads to allograft damage, and this activation begins by antibody binding of C1q (58). Downstream, C3 is cleaved leaving C3d. Commercially available modified SAB tests have been developed to specifically detect C1q and C3d binding. C1q or C3d binding positivity represents the presence of DSA that is a complement fixing subtype of IgG at a high enough level to bind complement (59, 60). DSA with C1q and/or C3d binding positivity is associated with the development of AMR and allograft loss (57, 60, 61) and some groups routinely use these tests to distinguish the most deleterious DSA. However, the presence of C1q binding antibodies is also associated with DSA MFI and antibody titer (62, 63). It remains unknown whether C1q positivity is any more predictive of AMR or graft loss than MFI or antibody titer (31, 62, 64) and thus testing for C1q or C3d binding is not yet universally performed.
Immunoglobulin Subclasses
SABs provide a semiquantitative measure of total immunoglobulin G (IgG) rather than IgG subclasses. This is relevant because each subclass has a differing role in the immune response and varied ability to bind the Fc receptor or activate complement(65). Specific subclass profiles may have a stronger association with the development of chronic AMR or allograft loss than total IgG. IgG subclass characterization is now performed in the research setting using a modified SAB assay in which the conventional phycoerythrin-conjugated anti-human IgG is replaced with an IgG subclass-specific anti-human IgG(66).
Of the 4 subclasses, IgG1/IgG3 has the strongest ability to bind complement. Emerging evidence suggests that DSA of the IgG 3 subclass is particularly deleterious to the renal and liver allografts (54, 66-72). However, studies of IgG subclasses in transplantation are limited because few groups have examined complete IgG subclass characterization [IgG1-IgG4] serially. The complexity of studying IgG subclasses is overwhelming, but provides clues about the pathogenicity of certain DSA and the immune response, and thus it will likely become an important aspect in donor selection in highly sensitized patients. More study of the significance of DSA subclass characterization and testing methods are needed before routine clinical use.
Practical approach to alloantibody testing
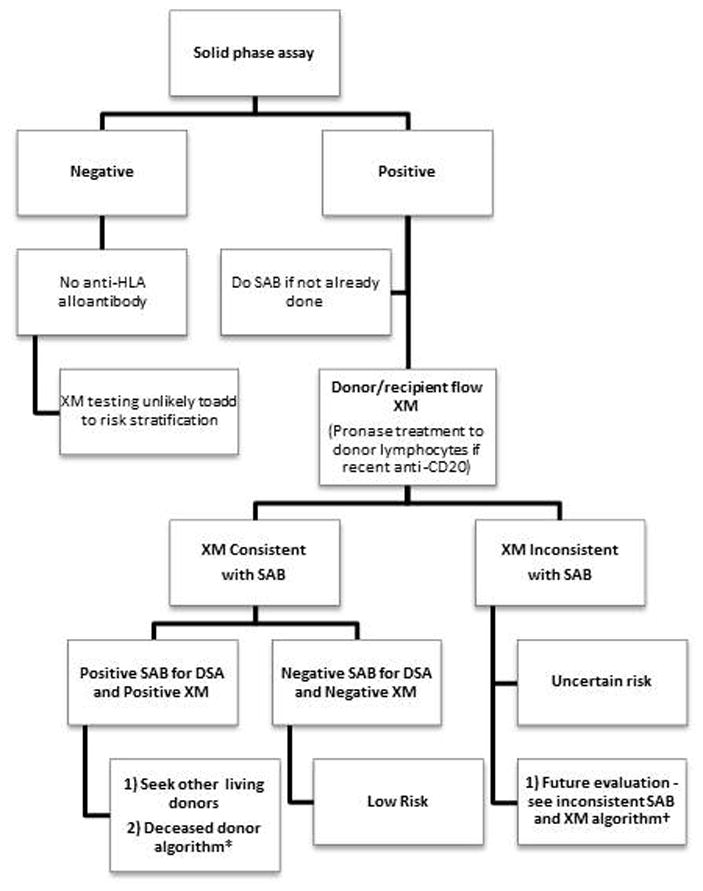
In an ideal world, comprehensive DSA testing would be performed for each patient including antibody titer, non-HLA antibody, auto-flow XM etc; but this is not practical given time constraints and is not cost-effective. We suggest the evaluation be tailored based on type of donor (deceased versus living) and the patient's sensitization Figures 2 and 3. Additionally, we always recommend consultation with local tissue typing experts and consideration of clinical context. These algorithms are based on our personal recommendations and apply to renal transplant recipients only. These algorithms may differ depending on the organ transplanted.
Figure 2. Algorithm for DSA testing for Candidate on Deceased Donor Waiting List.

Figure 3. Algorithm for DSA testing for Candidate with Potential Living Donor.
For transplant candidates awaiting a deceased donor, the goal is to optimize access to transplantation, while avoiding an unexpected final XM. Time constraints limit the ability to do further testing after an unexpected positive final XM, and thus we recommend as much testing as possible before or at the time of the final XM.
If the patient has completely negative solid phase testing (single antigen bead or multi-antigen beads), their risk for AMR is low. Crossmatch testing does not add considerably to risk stratification and in that case, one could argue that it is not needed. However, for patients with SAB positivity or history of sensitizing event, unacceptable antigens (or acceptable mismatch) must be assigned and a final XM is valuable. Because highly sensitized transplant candidates (cPRA >80%) have the least access to transplantation and are the most likely to have an unexpected positive XM, we recommend testing for prozone and alloantibody towards denatured HLA prior to unacceptable antigen assignment. The assignment of unacceptable antigens is variable among centers and is dependent on center preferences and underlying patient characteristics (age, sensitization, historical alloantibody, and waiting time). Inter and intra-laboratory variability and background positivity of the single antigen bead assay should also be taken into consideration. For the most part, if alloantibody is present with MFI of > 1000 or prozone is present, the corresponding antigen is considered unacceptable. Conversely, if the SAB is only positive because alloantibody is toward denatured HLA, it can be considered acceptable.
When an organ is offered, we also recommend obtaining an auto-flow XM at the time of final crossmatch and treating donor lymphocytes with pronase if the potential recipient has had recent exposure to anti-CD20. Usually all XM testing is negative, and transplantation can proceed. However, occasionally the final crossmatch is positive in which case the auto-flow XM is helpful. If the auto-flow XM is positive, and you have confirmed that the patient has not had any recent sensitization and the donor typing is complete, you can proceed to transplant. If the final XM is unexpectedly positive, but the auto-XM is negative, the risk of transplantation is uncertain. The potential considerations include recent sensitization (previous SAB testing is not current), incomplete donor/recipient HLA typing, SAB non-inclusive of donor HLA, alloantibody toward a public epitope, or alloantibody towards non-HLA Figure 2.
When a potential living donor has been identified, the timing of DSA testing is somewhat modified as shown in Figure 3. Again, if the solid phase assay is completely negative, the risk for AMR is low, and the XM does not add considerably to the evaluation. However, in other cases, we recommend a flow XM at the time of donor identification. Further testing is only done if the flow XM result is not consistent with the SAB – whether it is a positive SAB suggestive of DSA and negative XM or negative SAB and positive XM Figure 4. The risk of AMR in the setting of positive SAB and a negative XM is generally low, but we recommend consulting with the HLA laboratory and sometimes testing for alloantibody towards denatured antigen. The risk of transplantation in the setting of a positive XM and negative DSA is less certain. Although the XM is often falsely positive from non-specific binding of donor lymphocytes (auto-flow XM positivity); prozone effect, incomplete donor typing, SAB non-inclusive of donor HLA, alloantibody towards a shared epitope, and non-HLA alloantibody should be considered especially if the patient has a cPRA of greater than 80%.
Figure 4. Evaluation when the Single Antigen Beads and Flow Crossmatch are Inconsistent.

Although we provide a framework for DSA testing, it does not substitute clinical judgement. Consultation with the HLA laboratory is crucial to accurately estimate your patient's risk for AMR. Consideration of the underlying clinical context is also critical. We optimally avoid DSA in the setting of a young nonsensitized patient who is not yet on dialysis, yet consider positive XM transplantation with known DSA in a highly sensitized candidate with prolonged waiting time. Although beyond the scope of this article, it is also always important to have a protocol to manage AMR because AMR can unexpectedly occur even in presumably low risk situations.
Conclusion
Our understanding of DSA has advanced overtime, and sensitive techniques for DSA detection are now available, but the interpretation remains difficult. Optimal patient management involves experts from the HLA laboratory and careful interpretation of alloantibody testing while considering the clinical context. Recent modifications of the SAB assay to determine particular DSA characteristics including complement binding and IgG subclass will complicate alloantibody interpretation, but likely provide clarity about the prognostic significance of particular DSA. An efficient and cost-effective approach to alloantibody testing can minimize the risk of AMR for patients, yet optimize access to transplantation.
Acknowledgments
We thank Adriana Zeevi PhD, ABHI for her critical review of the manuscript and suggestions for improvement.
Funding: This publication was made possible by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Abbreviations
- AMR
antibody mediated rejection
- CDC XM
complement-dependent cytotoxicity crossmatch
- cPRA
calculated panel reactive antibody
- DSA
donor specific antibody
- HLA
human leukocyte antigen
- MFI
mean fluorescence intensity
- SAB
single antigen bead
- XM
crossmatch
Footnotes
Authorship: Carrie A. Schinstock MD, Design and drafting of manuscript, Final approval of version to be published, No conflicts of interest.
Manish J. Gandhi MD, Helped with the design of the work and critical revision, Final approval of version to be published, No conflicts of interest.
Mark D. Stegall MD, Helped with the design of the work and critical revision, Final approval of version to be published, No conflicts of interest
References
- 1.Gloor JM, Sethi S, Stegall MD, et al. Transplant glomerulopathy: subclinical incidence and association with alloantibody. Am J Transplant. 2007;7(9):2124. doi: 10.1111/j.1600-6143.2007.01895.x. [DOI] [PubMed] [Google Scholar]
- 2.Issa N, Cosio FG, Gloor JM, et al. Transplant glomerulopathy: risk and prognosis related to anti-human leukocyte antigen class II antibody levels. Transplantation. 2008;86(5):681. doi: 10.1097/TP.0b013e3181837626. [DOI] [PubMed] [Google Scholar]
- 3.Hidalgo LG, Campbell PM, Sis B, et al. De novo donor-specific antibody at the time of kidney transplant biopsy associates with microvascular pathology and late graft failure. Am J Transplant. 2009;9(11):2532. doi: 10.1111/j.1600-6143.2009.02800.x. [DOI] [PubMed] [Google Scholar]
- 4.Hodges AM, Lyster H, McDermott A, et al. Late antibody-mediated rejection after heart transplantation following the development of de novo donor-specific human leukocyte antigen antibody. Transplantation. 2012;93(6):650. doi: 10.1097/TP.0b013e318244f7b8. [DOI] [PubMed] [Google Scholar]
- 5.Taner T, Stegall MD, Heimbach JK. Antibody-mediated rejection in liver transplantation: Current controversies and future directions. Liver Transpl. 2014;20:514–527. doi: 10.1002/lt.23826. [DOI] [PubMed] [Google Scholar]
- 6.Niederhaus SV, Leverson GE, Lorentzen DF, et al. Acute cellular and antibody-mediated rejection of the pancreas allograft: incidence, risk factors and outcomes. Am J Transplant. 2013;13(11):2945. doi: 10.1111/ajt.12443. [DOI] [PubMed] [Google Scholar]
- 7.OPTN/UNOS. Greater Consistency in Candidate and Deceased Donor HLA Typing Requirements Across Organ Types. [January 22, 2016];U S Department of Health & Human Services. 2014 https://optn.transplant.hrsa.gov/PublicComment/pubcommentPropSub_335.pdf.
- 8.Lachmann N, Todorova K, Schulze H, Schonemann C. Luminex((R)) and its applications for solid organ transplantation, hematopoietic stem cell transplantation, and transfusion. Transfusion medicine and hemotherapy : offizielles Organ der Deutschen Gesellschaft fur Transfusionsmedizin und Immunhamatologie. 2013;40(3):182. doi: 10.1159/000351459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bray R. Transplantation Immunology: Methods and Protocols. In: Zachary AL, Leffell M, editors. Lymphocyte Crossmatching by Flow Cytometry. Vol. 103. Springer; 2013. pp. 285–296. [DOI] [PubMed] [Google Scholar]
- 10.Taylor CJ, Kosmoliaptsis V, Summers DM, Bradley JA. Back to the future: application of contemporary technology to long-standing questions about the clinical relevance of human leukocyte antigen-specific alloantibodies in renal transplantation. Hum Immunol. 2009;70(8):563. doi: 10.1016/j.humimm.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Tait BD, Susal C, Gebel HM, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation. 2013;95(1):19. doi: 10.1097/TP.0b013e31827a19cc. [DOI] [PubMed] [Google Scholar]
- 12.Heo WB, Kim CD, Won DI. HLA Class II-specific antibodies can react with T cells in flow cytometry crossmatch: a case report. Transplant Proc. 2007;39(10):3485. doi: 10.1016/j.transproceed.2007.06.078. [DOI] [PubMed] [Google Scholar]
- 13.Otten HG, Verhaar MC, Borst HP, et al. The significance of pretransplant donor-specific antibodies reactive with intact or denatured human leucocyte antigen in kidney transplantation. Clin Exp Immmunol. 2013;173(3):536. doi: 10.1111/cei.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Visentin J, Guidicelli G, Bachelet T, et al. Denatured class I human leukocyte antigen antibodies in sensitized kidney recipients: prevalence, relevance, and impact on organ allocation. Transplantation. 2014;98(7):738. doi: 10.1097/TP.0000000000000229. [DOI] [PubMed] [Google Scholar]
- 15.Pereira S, Perkins S, Lee JH, et al. Donor-specific antibody against denatured HLA-A1: clinically nonsignificant? Hum Immunol. 2011;72(6):492. doi: 10.1016/j.humimm.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 16.Jacob EK, De Goey SR, Gandhi MJ. Positive virtual crossmatch with negative flow crossmatch results in two cases. Transplant Immunol. 2011;25(1):77. doi: 10.1016/j.trim.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Oaks M, Michel K, Sulemanjee NZ, Thohan V, Downey FX. Practical value of identifying antibodies to cryptic HLA epitopes in cardiac transplantation. J Heart Lung Transplant. 2014;33(7):713. doi: 10.1016/j.healun.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 18.Reed EF, Rao P, Zhang Z, et al. Comprehensive assessment and standardization of solid phase multiplex-bead arrays for the detection of antibodies to HLA-drilling down on key sources of variation. Am J Transplant. 2013;13(11):3050. doi: 10.1111/ajt.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Konvalinka A, Tinckam K. Utility of HLA Antibody Testing in Kidney Transplantation. J Am Soc Nephrol. 2015;26(7):1489. doi: 10.1681/ASN.2014080837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gebel HM, Bray RA. HLA antibody detection with solid phase assays: great expectations or expectations too great? Am J Transplant. 2014;14(9):1964. doi: 10.1111/ajt.12807. [DOI] [PubMed] [Google Scholar]
- 21.Gandhi MJ, Carrick DM, Jenkins S, et al. Lot-to-lot variability in HLA antibody screening using a multiplexed bead-based assay. Transfusion. 2013;53(9):1940. doi: 10.1111/trf.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gandhi MJ, Degoey S, Falbo D, et al. Inter and intra laboratory concordance of HLA antibody results obtained by single antigen bead based assay. Hum Immunol. 2013;74(3):310. doi: 10.1016/j.humimm.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Vaidya S, Cooper TY, Avandsalehi J, et al. Improved flow cytometric detection of HLA alloantibodies using pronase: potential implications in renal transplantation. Transplantation. 2001;71(3):422. doi: 10.1097/00007890-200102150-00015. [DOI] [PubMed] [Google Scholar]
- 24.Hetrick SJ, Schillinger KP, Zachary AA, Jackson AM. Impact of pronase on flow cytometric crossmatch outcome. Hum Immunol. 2011;72(4):330. doi: 10.1016/j.humimm.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Le Bas-Bernardet S, Hourmant M, Valentin N, et al. Identification of the antibodies involved in B-cell crossmatch positivity in renal transplantation. Transplantation. 2003;75(4):477. doi: 10.1097/01.TP.0000047311.77702.59. [DOI] [PubMed] [Google Scholar]
- 26.Kosmoliaptsis V, Bradley JA, Peacock S, Chaudhry AN, Taylor CJ. Detection of immunoglobulin G human leukocyte antigen-specific alloantibodies in renal transplant patients using single-antigen-beads is compromised by the presence of immunoglobulin M human leukocyte antigen-specific alloantibodies. Transplantation. 2009;87(6):813. doi: 10.1097/TP.0b013e318199c581. [DOI] [PubMed] [Google Scholar]
- 27.Gloor JM, Moore SB, Schneider BA, Degoey SR, Stegall MD. The effect of antithymocyte globulin on anti-human leukocyte antigen antibody detection assays. Transplantation. 2007;84(2):258. doi: 10.1097/01.tp.0000269615.91036.52. [DOI] [PubMed] [Google Scholar]
- 28.Visentin J, Vigata M, Daburon S, et al. Deciphering complement interference in anti-human leukocyte antigen antibody detection with flow beads assays. Transplantation. 2014;98(6):625. doi: 10.1097/TP.0000000000000315. [DOI] [PubMed] [Google Scholar]
- 29.Schnaidt M, Weinstock C, Jurisic M, Schmid-Horch B, Ender A, Wernet D. HLA antibody specification using single-antigen beads--a technical solution for the prozone effect. Transplantation. 2011;92(5):510. doi: 10.1097/TP.0b013e31822872dd. [DOI] [PubMed] [Google Scholar]
- 30.Zachary AA, Lucas DP, Detrick B, Leffell MS. Naturally occurring interference in Luminex assays for HLA-specific antibodies: characteristics and resolution. Hum Immunol. 2009;70(7):496. doi: 10.1016/j.humimm.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Tambur AR, Herrera ND, Haarberg KM, et al. Assessing Antibody Strength: Comparison of MFI, C1q, and Titer Information. Am J Transplant. 2015;15(9):2421–30. doi: 10.1111/ajt.13295. [DOI] [PubMed] [Google Scholar]
- 32.Ellis TM. Interpretation of HLA single antigen bead assays. Transplantation reviews. 2013;27(4):108. doi: 10.1016/j.trre.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 33.Tait BD, Hudson F, Brewin G, Cantwell L, Holdsworth R. Solid phase HLA antibody detection technology--challenges in interpretation. Tissue Antigens. 2010;76(2):87. doi: 10.1111/j.1399-0039.2010.01486.x. [DOI] [PubMed] [Google Scholar]
- 34.Duquesnoy RJ, Marrari M. Correlations between Terasaki's HLA class I epitopes and HLAMatchmaker-defined eplets on HLA-A, -B and -C antigens. Tissue Antigens. 2009;74(2):117. doi: 10.1111/j.1399-0039.2009.01271.x. [DOI] [PubMed] [Google Scholar]
- 35.Lefaucheur C, Loupy A, Hill GS, et al. Preexisting donor-specific HLA antibodies predict outcome in kidney transplantation. J Am Soc Nephrol. 2010;21(8):1398. doi: 10.1681/ASN.2009101065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Opelz G. Non-HLA transplantation immunity revealed by lymphocytotoxic antibodies. Lancet. 2005;365(9470):1570. doi: 10.1016/S0140-6736(05)66458-6. [DOI] [PubMed] [Google Scholar]
- 37.Grafft CA, Cornell LD, Gloor JM, et al. Antibody-mediated rejection following transplantation from an HLA-identical sibling. Nephrol Dial Transplant. 2010;25(1):307. doi: 10.1093/ndt/gfp526. [DOI] [PubMed] [Google Scholar]
- 38.Sigdel TK, Sarwal MM. Moving beyond HLA: a review of nHLA antibodies in organ transplantation. Hum Immunol. 2013;74(11):1486. doi: 10.1016/j.humimm.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dinavahi R, George A, Tretin A, et al. Antibodies reactive to non-HLA antigens in transplant glomerulopathy. J Am Soc Nephrol. 2011;22(6):1168. doi: 10.1681/ASN.2010111183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cerilli J, Clarke J, Doolin T, Cerilli G, Brasile L. The significance of a donor-specific vessel crossmatch in renal transplantation. Transplantation. 1988;46(3):359. doi: 10.1097/00007890-198809000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Paul LC, Claas FH, van Es LA, Kalff MW, de Graeff J. Accelerated rejection of a renal allograft associated with pretransplantation antibodies directed against donor antigens on endothelium and monocytes. N Engl J Med. 1979;300(22):1258. doi: 10.1056/NEJM197905313002206. [DOI] [PubMed] [Google Scholar]
- 42.Fredrich R, Toyoda M, Czer LS, et al. The clinical significance of antibodies to human vascular endothelial cells after cardiac transplantation. Transplantation. 1999;67(3):385. doi: 10.1097/00007890-199902150-00008. [DOI] [PubMed] [Google Scholar]
- 43.Glotz D, Lucchiari N, Pegaz-Fiornet B, Suberbielle-Boissel C. Endothelial cells as targets of allograft rejection. Transplantation. 2006;82(1 Suppl):S19. doi: 10.1097/01.tp.0000231348.55262.5a. [DOI] [PubMed] [Google Scholar]
- 44.Mizutani K, Terasaki PI, Shih RN, Pei R, Ozawa M, Lee J. Frequency of MIC antibody in rejected renal transplant patients without HLA antibody. Hum Immunol. 2006;67(3):223. doi: 10.1016/j.humimm.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 45.Mizutani K, Terasaki P, Rosen A, et al. Serial ten-year follow-up of HLA and MICA antibody production prior to kidney graft failure. Am J Transplant. 2005;5(9):2265. doi: 10.1111/j.1600-6143.2005.01016.x. [DOI] [PubMed] [Google Scholar]
- 46.Terasaki PI, Ozawa M, Castro R. Four-year follow-up of a prospective trial of HLA and MICA antibodies on kidney graft survival. Am J Transplant. 2007;7(2):408. doi: 10.1111/j.1600-6143.2006.01644.x. [DOI] [PubMed] [Google Scholar]
- 47.Zou Y, Stastny P, Susal C, Dohler B, Opelz G. Antibodies against MICA antigens and kidney-transplant rejection. N Engl J Med. 2007;357(13):1293. doi: 10.1056/NEJMoa067160. [DOI] [PubMed] [Google Scholar]
- 48.Jackson AM, Sigdel TK, Delville M, et al. Endothelial cell antibodies associated with novel targets and increased rejection. J Am Soc Nephrol. 2015;26(5):1161. doi: 10.1681/ASN.2013121277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jackson AM, Lucas DP, Melancon JK, Desai NM. Clinical relevance and IgG subclass determination of non-HLA antibodies identified using endothelial cell precursors isolated from donor blood. Transplantation. 2011;92(1):54. doi: 10.1097/TP.0b013e31821b60e9. [DOI] [PubMed] [Google Scholar]
- 50.Valenzuela NM, Reed EF. Antibodies in transplantation: the effects of HLA and non-HLA antibody binding and mechanisms of injury. Methods Mol Bio. 2013;1034:41. doi: 10.1007/978-1-62703-493-7_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Montgomery RA, Lonze BE, King KE, et al. Desensitization in HLA-incompatible kidney recipients and survival. N Engl J Med. 2011;365(4):318. doi: 10.1056/NEJMoa1012376. [DOI] [PubMed] [Google Scholar]
- 52.Gloor JM, Winters JL, Cornell LD, et al. Baseline donor-specific antibody levels and outcomes in positive crossmatch kidney transplantation. Am J Transplant. 2010;10(3):582. doi: 10.1111/j.1600-6143.2009.02985.x. [DOI] [PubMed] [Google Scholar]
- 53.Burns JM, Cornell LD, Perry DK, et al. Alloantibody levels and acute humoral rejection early after positive crossmatch kidney transplantation. Am J Transplant. 2008;8(12):2684. doi: 10.1111/j.1600-6143.2008.02441.x. [DOI] [PubMed] [Google Scholar]
- 54.Lefaucheur C, Viglietti D, Bentlejewski C, et al. IgG Donor-Specific Anti-Human HLA Antibody Subclasses and Kidney Allograft Antibody-Mediated Injury. J Am Soc Nephrol. 2015 doi: 10.1681/ASN.2014111120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Woodle ES, Shields AR, Ejaz NS, et al. Prospective iterative trial of proteasome inhibitor-based desensitization. Am J Transplant. 2015;15(1):101. doi: 10.1111/ajt.13050. [DOI] [PubMed] [Google Scholar]
- 56.Kannabhiran D, Lee J, Schwartz JE, et al. Characteristics of Circulating Donor Human Leukocyte Antigen-specific Immunoglobulin G Antibodies Predictive of Acute Antibody-mediated Rejection and Kidney Allograft Failure. Transplantation. 2015;99(6):1156. doi: 10.1097/TP.0000000000000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Loupy A, Lefaucheur C, Vernerey D, et al. Complement-binding anti-HLA antibodies and kidney-allograft survival. N Engl J Med. 2013;369(13):1215. doi: 10.1056/NEJMoa1302506. [DOI] [PubMed] [Google Scholar]
- 58.Stegall MD, Chedid MF, Cornell LD. The role of complement in antibody-mediated rejection in kidney transplantation. NatureRev Nephrol. 2012;8(11):670. doi: 10.1038/nrneph.2012.212. [DOI] [PubMed] [Google Scholar]
- 59.Chen G, Sequeira F, Tyan DB. Novel C1q assay reveals a clinically relevant subset of human leukocyte antigen antibodies independent of immunoglobulin G strength on single antigen beads. Hum Immunol. 2011;72(10):849. doi: 10.1016/j.humimm.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 60.Sicard A, Ducreux S, Rabeyrin M, et al. Detection of C3d-binding donor-specific anti-HLA antibodies at diagnosis of humoral rejection predicts renal graft loss. J Am Soc Nephrol. 2015;26(2):457. doi: 10.1681/ASN.2013101144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baid-Agrawal S, Lachmann N, Budde K. Complement-binding anti-HLA antibodies and kidney transplantation. N Engl J Med. 2014;370(1):84. doi: 10.1056/NEJMc1313506. [DOI] [PubMed] [Google Scholar]
- 62.Zeevi A, Lunz J, Feingold B, et al. Persistent strong anti-HLA antibody at high titer is complement binding and associated with increased risk of antibody-mediated rejection in heart transplant recipients. J Heart Lung Transplant. 2013;32(1):98. doi: 10.1016/j.healun.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schaub S, Honger G, Koller MT, Liwski R, Amico P. Determinants of C1q binding in the single antigen bead assay. Transplantation. 2014;98(4):387. doi: 10.1097/TP.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 64.Gandhi M, Degoey S, Henderson N, Voit L, Krueter J. C1q single antigen bead assay only detects high titer/avidity class-I anti HLA antibodies detected by single antigen beads. Hum Immunol. 2014;75:73. [Google Scholar]
- 65.Nimmerjahn F, Ravetch JV. Divergent immunoglobulin g subclass activity through selective Fc receptor binding. Science. 2005;310(5753):1510. doi: 10.1126/science.1118948. [DOI] [PubMed] [Google Scholar]
- 66.Kaneku H, O'Leary JG, Taniguchi M, Susskind BM, Terasaki PI, Klintmalm GB. Donor-specific human leukocyte antigen antibodies of the immunoglobulin G3 subclass are associated with chronic rejection and graft loss after liver transplantation. Liver Transpl. 2012;18(8):984. doi: 10.1002/lt.23451. [DOI] [PubMed] [Google Scholar]
- 67.Taner T, Gandhi MJ, Sanderson SO, et al. Prevalence, course and impact of HLA donor-specific antibodies in liver transplantation in the first year. Am J Transplant. 2012;12(6):1504. doi: 10.1111/j.1600-6143.2012.03995.x. [DOI] [PubMed] [Google Scholar]
- 68.O'Leary JG, Klintmalm GB. Impact of donor-specific antibodies on results of liver transplantation. Curr Opin Organ Transplant. 2013;18(3):279. doi: 10.1097/MOT.0b013e3283614a10. [DOI] [PubMed] [Google Scholar]
- 69.O'Leary JG, Demetris AJ, Friedman LS, et al. The role of donor-specific HLA alloantibodies in liver transplantation. Am J Transplant. 2014;14(4):779. doi: 10.1111/ajt.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Everly MJ, Rebellato LM, Haisch CE, et al. Impact of IgM and IgG3 anti-HLA alloantibodies in primary renal allograft recipients. Transplantation. 2014;97(5):494. doi: 10.1097/01.TP.0000441362.11232.48. [DOI] [PubMed] [Google Scholar]
- 71.Schinstock CRS, Cosio F, Cornell L, Everly M, Gandhi M, Stegall M. Donor-Specific Alloantibody after Positive Crossmatch Kidney Transplant with Eculizumab: Correlation with Transplant Glomerulopathy and Graft Failure. 2015 Abstract. [Google Scholar]
- 72.Freitas MC, Rebellato LM, Ozawa M, et al. The role of immunoglobulin-G subclasses and C1q in de novo HLA-DQ donor-specific antibody kidney transplantation outcomes. Transplantation. 2013;95(9):1113. doi: 10.1097/TP.0b013e3182888db6. [DOI] [PubMed] [Google Scholar]


