Abstract
Background and aims: This study aimed to evaluate the efficacy of ibuprofen, bite wafer and low power red and infrared lasers in orthodontic pain management.
Subjects and methods: One hundred subjects were randomly assigned to 5 groups of 20 each. The patients in each group received one of the following treatments after the placement of fixed orthodontic appliances: 1. placebo medication, 2. ibuprofen, 3. bite wafer, 4. irradiation from a low level red laser (LLRL; 660 nm, 200 mW, 1 J/point, 6 points), 5. irradiation from a low level infrared laser (LLIL; 810 nm, 200 mW, 1 J/point, 6 points). A Visual Analogue Scale (VAS) was used to record pain intensity while chewing, biting, fitting front teeth, and fitting back teeth at 2 hours, 6 hours, bedtime, 24 hours, 2 days, 3 days and 7 days following arch wire placement.
Results: Significant between-group differences were found in pain at chewing, biting, fitting front teeth and fitting back teeth at all time points (p<0.001). Generally, VAS scores in the LLIL, ibuprofen and bite wafer groups were close to each other and significantly lower than those in the LLRL and control groups (p<0.05), which showed comparable pain level at most intervals. The infrared laser group (LLIL) showed significantly lower pain than all other groups at some points over the experiment (p<0.05).
Conclusions: A single irradiation from a low level infrared laser proved to be the best strategy for orthodontic pain control. Alternatively, chewing on a bite wafer could be recommended. These methods should be considered as suitable alternatives for ibuprofen in orthodontic patients.
Keywords: laser, Pain, low level laser, low power laser, therapy, ibuprofen, bite wafer, orthodontic treatment, arch wire
Introduction
Pain/discomfort is a common experience in subjects wearing fixed orthodontic appliances. Pain usually affects routine activities such as sleep, eating and chewing, and may even encourage some patients to undergo early termination of therapy 1). Most orthodontic procedures such as separator placement, insertion and activation of arch wires and debonding could be perceived painful by the patients 2). Pain usually begins at 2 to 4 hours after application of orthodontic forces and increases until 24 hours; then fades gradually over the next 7 days 3–6). It is believed that a combination of pressure, ischemia, inflammation and edema in the compressed periodontal ligament (PDL) are responsive for pain induced following force application 7).
Traditionally, prescription of non-steroidal anti-inflammatory drugs (NSAIDs) has been considered as the most effective strategy for controlling pain resulted from orthodontic forces. NSAIDs inhibit the synthesis of prostaglandins which are important mediators in the process of pain induction 4). The use of these drugs, however, may be associated with some systemic side effects such as gastrointestinal problems, thrombocytopenia, skin rushes, renal insufficiency, hypertension, and headache, and has raised health concerns especially for use in children and adolescents 8). For this reason, employing nondrug approaches such as bite wafers or low level laser therapy (LLLT) has been recommended for pain control during orthodontic therapy 1, 2, 4).
Chewing of gum or plastic wafers has been suggested as a method to alleviate pain induced after placement of orthodontic appliances 4, 9, 10). It is believed that chewing allows blood flow in compressed areas of the periodontal ligament and prevents the formation of pain-inducing metabolites, thus attenuating pain perception 10). Some studies 4, 9) demonstrated the effectiveness of bite wafers in controlling pain associated with initial archwire placement and suggested this approach as a suitable alternative for NSAIDs in pain management.
Low level laser therapy (LLLT) has been widely used in dentistry due to its analgesic and anti-inflammatory effects and its great benefits in accelerating the wound healing process 11–15). Previous studies employed LLLT for reducing pain initiated after separator or arch wire placement or during canine retraction, and reported controversial findings. Some authors believed that LLLT was effective for controlling pain in orthodontic patients 1, 16–21), whereas others reported no significant improvement in pain after laser therapy compared to a placebo application 22–24).
There are a few studies regarding the effectiveness of bite wafers and LLLT in alleviating pain and discomfort in orthodontic patients and the efficacy of these strategies has not been compared with together in previous investigations. Furthermore, no study compared the effect of low power red and infrared lasers in orthodontic pain management. Therefore, this clinical trial was conducted to evaluate the effectiveness of ibuprofen, bite wafer and low level red and infrared lasers in relieving pain during the first week after initial arch wire placement.
Subjects and methods
The sample consisted of one hundred subjects who were scheduled to undergo fixed orthodontic therapy at the Department of Orthodontics, School of Dentistry, Kerman University of Medical Sciences, Kerman, Iran. The patients were 66 females and 34 males and ranged in age from 14 to 21 years (mean age 17.6 years). To be included in the study, the patients should have moderate (4–8 mm) crowding according to Little's irregularity index 25), and require extraction of four first/second premolars for orthodontic reasons. The subjects who had systemic or periodontal diseases or underwent previous orthodontic therapy, as well as those using analgesics or medication interrupting tooth movement were excluded from the study. The study protocol was reviewed and approved by the Ethics Committee of Kerman University of Medical Sciences. The patients and their parents were informed about the details of the study and informed consent document was taken before the commencement of the treatment.
The subjects were randomly assigned to 5 groups of 20 each according to a computer-generated random assignment program. The extractions were finished at least 1 week before placing orthodontic appliances, and elastomeric separators were inserted for the first molars to be banded 2 days before appliance placement. In all participants, stainless steel bands and preadjusted edgewise brackets (0.022×0.028 inch slot; Dentaurum, Ispringen, Germany) were placed in upper and lower jaws at one appointment. A 0.014-in nickel titanium arch wire (Dentaurum) was engaged in all brackets using elastomeric modules (Ortho Technology, Tampa, Florida, USA), and the patients were instructed about the oral hygiene measures and care of appliances. The subjects in the study groups underwent specific pain relief strategies as follows:
Group 1 (placebo medication): The participants were instructed to take a vitamin B6 tablet (Pyridoxine HCl, 40 mg, Darou Pakhsh Co., Tehran, Iran) as a placebo immediately after appliance placement and at 8 hour intervals for one week, if pain persisted.
Group 2 (ibuprofen): The subjects were asked to take a 400-mg ibuprofen tablet (Ibuprofen Najo, 400 mg, Iran Najo Co., Tehran, Iran) immediately after insertion of arch wire and at 8 hour intervals for 1 week, if they experienced pain.
Group 3 (bite wafer): The participants were instructed to chew or bite down on a plastic bite wafer (Ortho Organizers. Inc., Carlsbad, CA; Fig. 1) following arch wire placemat and repeat the procedure at 8 hour intervals for 1 week, if pain persisted.
Fig. 1:

The bite wafers used in this study
Group 4 (low level red laser; LLRL): The patients in this group received a single session irradiation from a low power indium-gallium-aluminum-phosphide (InGaAlP) diode laser (wavelength 660 nm; Thor DD2 control unit, Thor, London, UK; Fig. 2) immediately after placement of fixed appliances. The laser emitted a wavelength of 660 nm and operated in continuous wave mode at power of 200 mW. The tip of the apparatus was held at close contact to the apical, middle and cervical areas of the root at both buccal and lingual directions for 5 seconds each (total period of 30 seconds per tooth), delivering 1 J of energy per area. Considering the area of 0.07 cm2 for the probe, the energy density was approximately 14.3 J/cm2. The laser irradiation was performed once during the study period. Both patient and therapist wore safety goggles during laser therapy.
Fig. 2:

The low power gallium-aluminum-arsenide (GaAlAs) and indium-gallium-aluminum-phosphide (InGaAlP) lasers used in this study
Group 5 (low level infrared laser; LLIL): In this group, a low level gallium-aluminum-arsenide (GaAlAs) diode laser (wavelength 810 nm; Thor; Fig. 2) was irradiated immediately after ligation of the arch wire. The laser parameters and sites of irradiations were similar to that described in group 4. Each area received 1 J of laser energy and the energy density at the surface of the probe was calculated to be 3.6 J/cm2 (spot size 0.28 cm2). The laser irradiation was performed once during the study period and eye protection was taken with safety goggles.
Because of the different pain management approaches employed in this study, masking of the subjects or the treating clinician was not possible. However, the subjects assigned to the ibuprofen and placebo medication groups were blinded to their allocation. Furthermore, the investigator who assessed the outcomes and the data analyst were kept blinded to the assignments.
Pain intensity was evaluated with a questionnaire containing 28 copies of a visual analogue scale (VAS). The VAS consisted of a 10-cm horizontal line with 0 (the left side) indicating no pain and 10 (the right side) representing the worst possible pain. Each patient was instructed to put a mark on the line in accordance with the degree of perceived pain. The distance between the mark and the left margin of the scale was then measured with a ruler and recorded as the pain score. Pain level was evaluated at 2 hours, 6 hours, bedtime on the day of arch wire placemen, 24 hours, 2 days, 3 days and 7 days after placement of the arch wire.
At each time point, pain intensity was recorded during four oral functions including chewing, biting, fitting front teeth and fitting back teeth. For chewing and biting functions, the patients were instructed to chew or bite on a slice of a yellow apple and then mark the degree of perceived pain. For fitting front and back teeth, the patients were asked to put the front teeth edge to edge with light force and to fit the back teeth with light force, respectively, and then score the amount of pain experienced at each function.
The patients were encouraged not to consume additional analgesics as much as possible and if they indeed required rescue medication, they should document the number of tablets.
Statistical analysis
The normal distribution of the data was confirmed by the Kolmogorov-Smirnov test. One way analysis of variance (ANOVA) was run to determine any significant differences in pain scores at each function and time point among the study groups, followed by Tukey post hoc analysis for pairwise comparisons. The difference in age of the participants in the study groups was analyzed by ANOVA and that of the sex and frequency of analgesic consumption was assessed by the chisquare test. The statistical calculation was performed by SPSS (Statistical Package for Social Sciences, Version 16.0, SPSS Inc, Chicago, IL) software, and the significance level was set at p<0.05.
Results
The study stared with 100 participants and 90 questionnaires were completed and returned. These 90 subjects therefore formed the data for this clinical trial. There was no significant difference in age or sex of the participants among the study groups (p=0.10 and p=0.85, respectively). The frequency of analgesic consumption was greater in the placebo medication group but the difference between groups was not significant (p=0.09). Figures 3 to 6 present VAS scores in centimeters for the study groups during different oral functions over the course of the experiment. Pain intensity increased from 2 hours after arch wire placement to a peak at 24 hours; then gradually declined until the 7th day. The highest pain intensity was reported by the subjects in the LLRL (low level red laser) group followed by those in the placebo medication group. Generally, the lowest amount of pain was observed in subjects underwent LLLT with infrared diode laser, but at some points, ibuprofen was the most effective strategy for pain reduction.
Fig. 3:
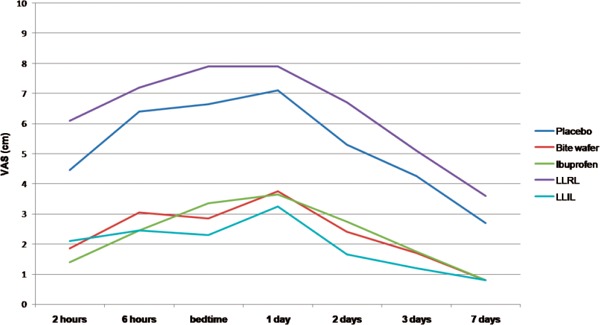
A line chart indicating VAS values at “chewing” function for the study groups (LLRL= low level red laser, LLIL=low level infrared laser).
Fig. 6:
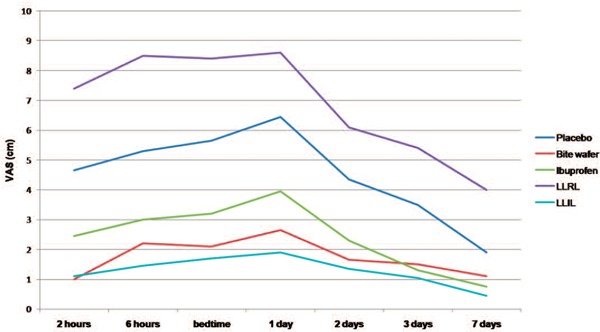
A line chart indicating VAS values at “fitting back teeth” function for the study groups (LLRL= low level red laser, LLIL=low level infrared laser).
Fig. 4:
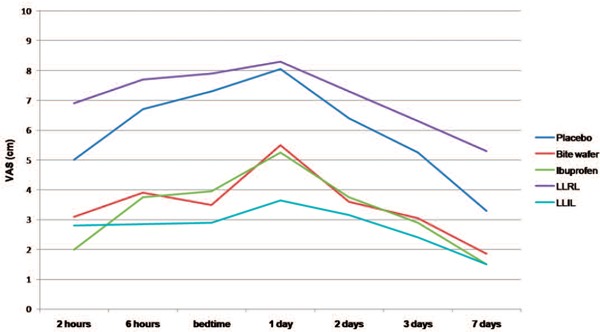
A line chart indicating VAS values at “biting” function for the study groups (LLRL= low level red laser, LLIL=low level infrared laser).
Fig. 5:
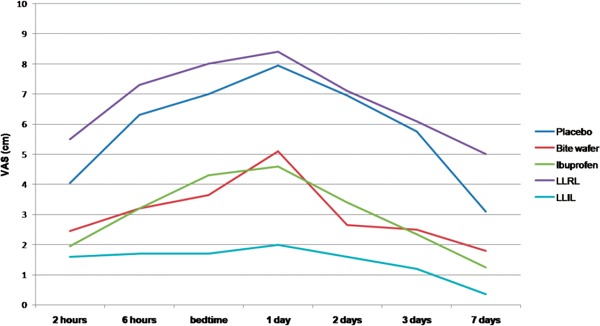
A line chart indicating VAS values at “fitting front teeth” function for the study groups (LLRL= low level red laser, LLIL=low level infrared laser).
ANOVA demonstrated significant between-group differences in pain perceived at chewing, biting, fitting front teeth and fitting back teeth at all time points (p<0.001). The results of the Tukey test revealed that at almost all intervals, pain intensity in the placebo group was comparable to that of the LLRL group (p>0.05), and both groups experienced significantly greater pain than subjects in the bite wafer, ibuprofen and LLIL (low level infrared laser) groups (p<0.05), which exhibited no significant differences to each other (p>0.05). The exceptions were observed in pain at “biting” at 24 hours, and in pain at “fitting front teeth” at bedtime and 24 hours, when the LLIL group showed significantly lower pain level than all other groups (p<0.05). Furthermore, on day 7, there was no significant difference between the placebo and bite wafer groups regarding pain at “biting” and “fitting front teeth” and between the placebo, bite wafer and ibuprofen groups regarding pain at “fitting back teeth”. In addition, LLRL group showed significantly greater pain scores than the placebo group regarding pain at “fitting back teeth” at 2 hours, 6 hours, bedtime, 3 days and 7 days (p<0.05).
Discussion
The present study investigated the effect of an anti-inflammatory drug (ibuprofen), placebo medication, bite wafer and two wavelengths of low power lasers on attenuating pain in subjects underwent orthodontic treatment with fixed appliances. Patients with 4 to 8 mm of crowding were selected in order to allow full engagement of the arch wire in most brackets. It is believed that pain scores in the range of 0 to 35 mm are perceived mild by the patients; whereas those ranging from 36 to 70 mm are categorized as moderate and scores between 71 and 100 mm indicate severe pain 11).
In all groups, pain during the four major oral functions increased 2 hours after fixed appliances were placed and reached the maximum intensity at 24 hours later; then decreased gradually over the rest of the experiment, so that the least amount of pain was reported on the 7th day. This finding confirms the results of other investigators 3–6) who found that pain severity is greatest at 24 hours after insertion of arch wire and returns to the normal level over the first week after appliance placement. In most groups, the maximum pain was somewhat greater during biting compared to other oral functions. This outcome is in agreement with the results of previous authors 4) who found that the peak pain occurs at biting function. In contrast, Polat et al 26) reported that at some time points, the highest pain level was observed while fitting front teeth together.
The effectiveness of ibuprofen and other NSAIDS in reducing pain resulted from the application of orthodontic forces has been demonstrated in previous investigations 26–29). In this study, patients in the ibuprofen group reported significantly lower pain compared to that of the placebo medication and LLRL (low level red laser) groups, but their difference with the bite wafer and LLIL (low level infrared laser) groups was not significant at most intervals. Because of the inflammatory nature of orthodontic pain, NSAIDs have been considered as the golden standard for controlling pain in orthodontic patients 4). The systemic side effects of ibuprofen, however, have deterred from considering this drug as a standard of care for pain management in young orthodontic patients.
In the present study, the use of bite wafer was almost as effective as the ibuprofen and low power infrared laser for orthodontic pain management. According to Furstman and Bernik 7), a combination of pressure, ischemia, inflammation, and edema is responsive for pain perceived after application of orthodontic forces. Proffit et al 10) recommended chewing on gum or plastic wafers to temporarily displace the teeth and establish partial blood circulation in compressed areas of the PDL, thus preventing from the formation of pain-inducing mediators. The outcomes of this study are in agreement with the results of Murdock et al 9) who reported that the use of bite wafers was at least as effective as over-the-counter (OTC) analgesics for pain management during the first week after initial arch wire placement. Farzanegan et al 4) suggested that viscoelastic bite wafers are good substitutes for NSAIDs in orthodontic pain management. In contrast, Otasevic et al 30) concluded that the avoidance of hard food in the first week after appliance placement was a more effective strategy than chewing on masticatory bite wafers for attenuating initial orthodontic pain. In agreement with previous authors 4), patients in the bite wafer group experienced lower pain while fitting back teeth than fitting front teeth. This could be attributed to the same thickness of bite wafer in anterior and posterior areas, so when the back teeth come in touch with the bite wafer, the anterior teeth will not touch the wafer 4).
The exact mechanism of low power lasers in pain release is not yet fully understood, however, their effects on increased local circulation, inhibiting the production of inflammatory mediators, stimulating nerve cell respiration and stabilizing membrane potentials have been indicated by several investigators 21, 31–34). In this study, both low power red and infrared lasers were employed for pain relief in orthodontically treated subjects, and the results showed that the red wavelength was not effective for this application. The degree of pain reported by the patients in the LLRL group was greater than all other groups although the difference with the placebo medication group was small and not statistically significant at most intervals. This may be related to the greater placebo effect of tablets in pain release. It seems that patients conventionally perceive less pain by taking tablets compared to receiving recent technologies such as laser therapy.
LLLT with infrared wavelength was indeed effective in reducing pain resulted from orthodontic treatment. The intensity of pain reported by the subjects in the LLIL group was lower than all other groups at most time points. The difference in pain perception between the LLIL, ibuprofen and bite wafer groups, however, was not statistically significant over the experiment except for pain at “biting” and “fitting front teeth” at some points, when the patients in the LLIL group experienced significantly lower pain than all groups of the study. The outcomes of this study confirmed the results of Tortamano et al 20) who reported that LLLT efficiently controlled pain caused by insertion of the first arch wire. Turhani et al 21) found that LLLT was an effective strategy to decrease the prevalence of pain at 6 and 30 hours after multibanding. Others studies indicated the beneficial effects of laser therapy in controlling pain perceived by the patients during canine retraction 35) or after separation 1, 17–19, 36). In contrast, Esper et al 37) indicated that laser therapy had no significant effect on the reduction of pain level compared to the low-level LED therapy. Several clinical trials reported no significant pain relief by using low-level laser irradiation after applications of orthodontic forces 22–24, 38). A recent systematic review concluded that there is limited evidence to believe that LLLT is capable to delay the onset and reduce the intensity of orthodontic pain 39). The laser parameters such as wavelength, power, energy, irradiation time, frequency of irradiation, power density and energy density could affect the treatment results and these may be the reason for the controversial findings about the analgesic effects of laser therapy on orthodontic pain management.
The laser settings employed in this study allowed each tooth to receive a total energy of 6 J (1 J per area) which was applied over a period of 30 seconds per tooth and thus less than 10 minutes per patient. The differences observed in the therapeutic effects of low power red and infrared lasers could be attributed to the different energy densities employed or to the different penetration depths of these wavelengths in biological tissues. The visible lasers in the range of 400–700 nm penetrate the tissue for about 8 mm, whereas the infrared lasers have approximately 2–3 cm penetration depth 13). It seems that the receptors producing orthodontic pain are located in deep areas and thus the application of infrared wavelength is more suitable for controlling pain resulted from initial arch wire placement. It should be noted that laser therapy was performed once and was not repeated during the study period, but other modalities could be repeated by the patients if pain persisted.
A limitation of laser therapy for pain relief is its relatively long period of application in orthodontic patients. However, LLLT could be performed by a skilled technician in the dental office with less intervention on routine dental activities. The duration of laser therapy could be minimized by using a device with a higher output power such as 400 or 500 mW, although the therapeutic effects of higher powers on orthodontic pain reduction should be clarified in future investigations.
The findings of the present study indicate promising results by a single session of infrared diode laser irradiation for orthodontic pain reduction. It is possible that a more frequent laser application or alterations in laser parameters could lead to a greater efficacy in pain relief in orthodontic patients, but more researches are warranted for verification. Because of the subjective nature of VAS scores which affects the response from patient to patient, further clinical trials are suggested to compare the efficacy of bite wafer and LLLT using objective criteria such as mediators in gingival circular fluids of subjects underwent orthodontic treatment.
Conclusion
Under the conditions used in this study:
A single irradiation from a low power infrared laser was the most effective strategy for pain relief following initial arch wire placement and could be suggested as a suitable alternative for ibuprofen.
Chewing on a bite wafer was also effective for orthodontic pain control and produced results that were comparable to that of the ibuprofen and low power infrared laser at most time points.
Treatment with a low power red laser could not be recommended for pain control following placement of orthodontic appliances.
Conflict of interest
The authors deny any conflict of interest.
Acknowledgements
This work was supported by the research chancellor of Kerman University of Medical Sciences [grant number 207]. The results presented in this paper have been taken from a post graduate student thesis in Orthodontics.
References
- 1: Kim WT, Bayome M, Park JB, Park JH, Baek SH, Kook YA. (2013): Effect of frequent laser irradiation on orthodontic pain. A single-blind randomized clinical trial. Angle Orthodontist, 83:611-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2: Li FJ, Zhang JY, Zeng XT, Guo Y. (2015): Low-level laser therapy for orthodontic pain: a systematic review. Lasers in Medical Science, 30:1789-1803. [DOI] [PubMed] [Google Scholar]
- 3: Erdinc AM, Dincer B. (2004): Perception of pain during orthodontic treatment with fixed appliances. European Journal of Orthodontics, 26:79-85. [DOI] [PubMed] [Google Scholar]
- 4: Farzanegan F, Zebarjad SM, Alizadeh S, Ahrari F. (2012): Pain reduction after initial archwire placement in orthodontic patients: a randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics, 141:169-173. [DOI] [PubMed] [Google Scholar]
- 5: Ngan P, Kess B, Wilson S. (1989): Perception of discomfort by patients undergoing orthodontic treatment. American Journal of Orthodontics and Dentofacial Orthopedics, 96:47-53. [DOI] [PubMed] [Google Scholar]
- 6: Wilson S, Ngan P, Kess B. (1989): Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatric Dentistry, 11:107-110. [PubMed] [Google Scholar]
- 7: Furstman L, Bernick S. (1972): Clinical considerations of the periodontium. American Journal of Orthodontics, 61:138-155. [DOI] [PubMed] [Google Scholar]
- 8: Ecklund CR, Ross MC. (2001): Over-the-counter medication use in preschool children. Journal of Pediatric Health Care, 15:168-72. [DOI] [PubMed] [Google Scholar]
- 9: Murdock S, Phillips C, Khondker Z, Hershey HG. (200): Treatment of pain after initial archwire placement: a noninferiority randomized clinical trial comparing over-the-counter analgesics and bite-wafer use. American Journal of Orthodontics and Dentofacial Orthopedics, 137:316-23. [DOI] [PubMed] [Google Scholar]
- 10: Proffit WR, Fields HW, Jr, Sarver DM. (2013): Contemporary orthodontics. 5th edition, Mosby, Elsevier Health Sciences, St Louis: pp 299-300. [Google Scholar]
- 11: Pakfetrat A, Falaki F, Ahrari F, Bidad S. (2014): Removal of refractory erosive-atrophic lichen planus by the CO2 laser. Oral Health and Dental Management, 13:595-599. [PubMed] [Google Scholar]
- 12: Eshghpour M, Ahrari F, Najjarkar NT, Khajavi MA. (2015). Comparison of the effect of low level laser therapy with alvogyl on the management of alveolar osteitis. Medicina oral, patología oral y cirugía bucal, 20:e386-392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13: Madani AS, Ahrari F, Nasiri F, Abtahi M, Tuner J. (2014): Low-level laser therapy for management of TMJ osteoarthritis. Cranio: the journal of craniomandibular practice, 32:38-44. [DOI] [PubMed] [Google Scholar]
- 14: Moosavi H, Maleknejad F, Sharifi M, Ahrari F. (2015): A randomized clinical trial of the effect of low-level laser therapy before composite placement on postoperative sensitivity in class V restorations. Lasers in medical science, 30:1245-1249. [DOI] [PubMed] [Google Scholar]
- 15: Ahrari F, Madani AS, Ghafouri ZS, Tuner J. (2014): The efficacy of low-level laser therapy for the treatment of myogenous temporomandibular joint disorder. Lasers in Medical Science, 29:551-557. [DOI] [PubMed] [Google Scholar]
- 16: Dominguez A, Velasquez SA. (2013): Effect of low-level laser therapy on pain following activation of orthodontic final archwires: a randomized controlled clinical trial. Photomedicine and laser surgery, 31:36-40. [DOI] [PubMed] [Google Scholar]
- 17: Eslamian L, Borzabadi-Farahani A, Hassanzadeh-Azhiri A, Badiee MR, Fekrazad R. (2014): The effect of 810-nm low-level laser therapy on pain caused by orthodontic elastomeric separators. Lasers in Medical Science, 29:559-564. [DOI] [PubMed] [Google Scholar]
- 18: Marini I, Bartolucci ML, Bortolotti F, Innocenti G, Gatto MR, Alessandri Bonetti G. (2015): The effect of diode superpulsed low-level laser therapy on experimental orthodontic pain caused by elastomeric separators: a randomized controlled clinical trial. Lasers in Medical Science, 30:35-41. [DOI] [PubMed] [Google Scholar]
- 19: Nobrega C, da Silva EM, de Macedo CR. (2013): Low-level laser therapy for treatment of pain associated with orthodontic elastomeric separator placement: a placebo-controlled randomized double-blind clinical trial. Photomedicine and laser surgery, 31:10-16. [DOI] [PubMed] [Google Scholar]
- 20: Tortamano A, Lenzi DC, Haddad AC, Bottino MC, Dominguez GC, Vigorito JW. (2009): Low-level laser therapy for pain caused by placement of the first orthodontic archwire: a randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics, 136:662-667. [DOI] [PubMed] [Google Scholar]
- 21: Turhani D, Scheriau M, Kapral D, Benesch T, Jonke E, Bantleon HP. (2006): Pain relief by single low-level laser irradiation in orthodontic patients undergoing fixed appliance therapy. American Journal of Orthodontics and Dentofacial Orthopedics, 130:371-377. [DOI] [PubMed] [Google Scholar]
- 22: Abtahi SM, Mousavi SA, Shafaee H, Tanbakuchi B. (2013): Effect of low-level laser therapy on dental pain induced by separator force in orthodontic treatment. Dental Research Journal (Isfahan), 10:647-651. [PMC free article] [PubMed] [Google Scholar]
- 23: Dominguez A, Gomez C, Palma JC. (2015): Effects of low-level laser therapy on orthodontics: rate of tooth movement, pain, and release of RANKL and OPG in GCF. Lasers in Medical Science, 30:915-923. [DOI] [PubMed] [Google Scholar]
- 24: Heravi F, Moradi A, Ahrari F. (2014): The effect of low level laser therapy on the rate of tooth movement and pain perception during canine retraction. Oral health and dental management, 13:183-188. [PubMed] [Google Scholar]
- 25: Little RM. (1975): The irregularity index: a quantitative score of mandibular anterior alignment. American Journal of Orthodontics 1975;68:554-563. [DOI] [PubMed] [Google Scholar]
- 26: Polat O, Karaman AI, Durmus E. (2005): Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain. Angle Orthodontist, 75:791-796. [DOI] [PubMed] [Google Scholar]
- 27: Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. (2001): The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. American Journal of Orthodontics and Dentofacial Orthopedics, 120:20-27. [DOI] [PubMed] [Google Scholar]
- 28: Bird SE, Williams K, Kula K. (2007): Preoperative acetaminophen vs ibuprofen for control of pain after orthodontic separator placement. American Journal of Orthodontics and Dentofacial Orthopedics, 132:504-510. [DOI] [PubMed] [Google Scholar]
- 29: Steen Law SL, Southard KA, Law AS, Logan HL, Jakobsen JR. (2000): An evaluation of preoperative ibuprofen for treatment of pain associated with orthodontic separator placement. American Journal of Orthodontics and Dentofacial Orthopedics, 118:629-635. [DOI] [PubMed] [Google Scholar]
- 30: Otasevic M, Naini FB, Gill DS, Lee RT. (2006): Prospective randomized clinical trial comparing the effects of a masticatory bite wafer and avoidance of hard food on pain associated with initial orthodontic tooth movement. American Journal of Orthodontics and Dentofacial Orthopedics, 130:6.e9-e15. [DOI] [PubMed] [Google Scholar]
- 31: Fork RL. (1071): Laser stimulation of nerve cells in Aplysia. Science, 171:907-908. [DOI] [PubMed] [Google Scholar]
- 32: Harris DM. (1991): Editorial comment biomolecular mechanisms of laser biostimulation. Journal of Clinical Laser Medicine & Surgery, 9:277-280. [Google Scholar]
- 33: Ponnudurai RN, Zbuzek VK, Wu WH. (1987): Hypoalgesic effect of laser photobiostimulation shown by rat tail flick test. Acupunct Electrother Res, 12:93-100. [DOI] [PubMed] [Google Scholar]
- 34: Shimizu N, Yamaguchi M, Goseki T, Shibata Y, Takiguchi H, Iwasawa T, et al. (1995): Inhibition of prostaglandin E2 and interleukin 1-beta production by low-power laser irradiation in stretched human periodontal ligament cells. Journal of Dental Research, 74:1382-1388. [DOI] [PubMed] [Google Scholar]
- 35: Doshi-Mehta G, Bhad-Patil WA. (2012): Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. American Journal of Orthodontics and Dentofacial Orthopedics, 141:289-297. [DOI] [PubMed] [Google Scholar]
- 36: Artes-Ribas M, Arnabat-Dominguez J, Puigdollers A. (2013): Analgesic effect of a low-level laser therapy (830 nm) in early orthodontic treatment. Lasers in Medical Science, 28:335-341. [DOI] [PubMed] [Google Scholar]
- 37: Esper MA, Nicolau RA, Arisawa EA. (2011): The effect of two phototherapy protocols on pain control in orthodontic procedure--a preliminary clinical study. Lasers in Medical Science, 26:657-663. [DOI] [PubMed] [Google Scholar]
- 38: Lim HM, Lew KK, Tay DK. (1995): A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain. American Journal of Orthodontics and Dentofacial Orthopedics, 108:614-622. [DOI] [PubMed] [Google Scholar]
- 39: He WL, Li CJ, Liu ZP, Sun JF, Hu ZA, Yin X, et al. (2013): Efficacy of low-level laser therapy in the management of orthodontic pain: a systematic review and meta-analysis. Lasers in Medical Science, 28:1581-1589. [DOI] [PubMed] [Google Scholar]


