Abstract
Background and aims: Recently novel picosecond duration lasers (ps-lasers) have been developed for the treatment of multicolored and recalcitrant tattoos, and safety and efficacy have been reported. We therefore hypothesized that the ps-laser could be an alternative treatment for dermal pigmented lesions and performed a retrospective review to evaluate the efficacy and safety of the ps-laser.
Subjects and methods: A retrospective photographic review of 10 patients with dermal pigmented lesions was performed (ages from 4 months to 52 yr), 6 nevus of Ota, 3 ectopic Mongolian spots and 1 Mongolian spots. The patients were treated in the Ohshiro Clinic with picosecond 755 nm alexandrite laser (ps-Alex laser) and picosecond 1064 nm Nd:YAG laser (ps-Nd:YAG laser) from April 2014 to December 2015 (ps-Alex laser, 7 patients; ps-Nd:YAG laser, 3 patients, 1 to 3 treatment sessions). Improvement was evaluated as percentage of pigmentation clearance comparing the baseline findings with those at 3 months after the final treatment using a five category grading scale: Poor, 0–24%; Fair, 25–49%; Good, 50–74%; Excellent, 75–94%; and Complete, 95–100% improvement. Adverse events were also assessed.
Results: All ten patients obtained clinical improvement ranging from fair to excellent. Treatment with the ps-Alex laser caused transient hyperpigmentation followed by improvement to complete resolution at 3 months follow-up. The ps-Nd:YAG laser caused severe transient erythema and swelling but no post-inflammatory hyperpigmentation.
Conclusions: Our results suggest that the 755 nm and 1064 nm ps-lasers are efficacious for the treatment of dermal pigment lesions, with minimum adverse events.
Keywords: picosecond laser, alexandrite laser, Nd:YAG laser, dermal melanocytosis, nevus of Ota, Mongolian spot
Introduction
The introduction of selective tissue destruction by pulsed lasers 1), so called selective photothermolysis 2), consolidated the landmark for laser treatment for dermatological disorders by allowing for precise tissue targeting, thus avoiding the risk of hyperpigmentation, hypopigmentation, and scarring associated with earlier treatment approaches such as continuous wave lasers, cryotherapy, dermabrasion and skin grafting.
The introduction of Q-switched lasers (lasers with pulse-widths in the nanosecond [ns] domain) to dermatological practice in the 1980s was viewed as a major breakthrough in the treatment of cutaneous pigmented lesions 3). Following Q-switched ns-domain laser treatment of dermal melanocytosis (dermal pigmented lesions) such as nevus of Ota, and Mongolian spots/ectopic Mongolian spots, the characteristic blue-grey color could be resolved completely with the Q-switched ruby, Q-switched alexandrite and Q-switched Nd:YAG lasers 4–9).
Recently, novel picosecond duration lasers (ps-lasers) have been developed for the treatment of unwanted tattoos. Since 2013, ps-lasers have become commercially available and the subsequent clinical trials have reported the safety and efficacy in treating multicolored and recalcitrant tattoos 10–14). It is considered that irradiation of targets with the ultra-short picosecond pulses can induce almost instantaneous heating of chromophores in the skin and greater fragmentation of the targets in an almost nonlinear fashion, with even less damage to adjacent structures than was achieved with the ns-domain lasers.
Application of the ps-laser for the treatment of unwanted tattoos was started in the Ohshiro clinic from December 2013. From our experience of the great success of tattoo removal with the ps-laser, we hypothesized that the ps-laser could be an alternative treatment for dermal pigmented lesions. In this study we performed a retrospective photographic review to evaluate the efficacy and safety in treating dermal pigmented lesions in the Asian skin using ps-domain lasers.
Subjects and methods
The present study was a retrospective photographic review of patients attending the Ohshiro Clinic, Shinanomachi, Tokyo, a long-established specialist medical laser practice, for the treatment of dermal melanocytosis during the period from April 2014 to December 2015. Patients were screened for inclusion in the retrospective study. Exclusion criteria included any hyperphotosensitivity, active or systemic infections, taking any medication for which sunlight is a contraindication, history of skin cancer, history of keloid scarring and history of immunosuppression. Pregnant woman and lactating woman were excluded. In addition, patients who had received another laser irradiation on the same pigmented lesion in the 12-month period before treatment were also excluded.
Patient medical information was extracted from the patient records, which included the age of patients at time of treatment, irradiation settings of each treatment, duration and number of treatment sessions, complications and clinical photographs. Clinical photographs were taken before, immediate after, 1 week after, 1 month after and 3 months after each treatment.
Ten patients met the inclusion criteria, 8 females, 2 males, ages ranging from 4 months to 52 years, mean 32.0 yr, who had dermal pigmented lesions. Fitzpatrick skin types were type III/IV, with the majority of patients type IV. Among the patients, Six had nevus of Ota, three had ectopic Mongolian spots (1 shoulder, 1 arm and 1 leg), and one patient had a Mongolian spot. Seven patients were treated with the picosecond 755 nm alexandrite laser (ps-Alex laser) (Picosure®, Cynosure, Westford, MA) and 3 with the picosecond 1064 nm Nd:YAG laser (ps-Nd:YAG laser) (Enlighten®, Cutera, Brisbane CA; PicoWay®, Syneron-Candela, Wayland, MA). Treatment sessions ranged from 1 to 3, with an average of 1.6. The parameters used for each individual patient are given in Table 1.
Table 1: Subject demographics, treatment parameters and clinical results.
Pre-treatment: Cryo: Cryotherapy
- QR: Q-switched ruby laser
Results: Clinical outcome was evaluated according to the following five category grading scale on the percentage of pigment clearance
- Poor, 0–24% improvement
- Fair, 25–49% improvement
- Good, 50–74% improvement
- Excellent, 75–94% improvement
- Complete, 95–100% improvement or complete clearance
IWP: immediate whitening phenomenon
| No. | Age | Gender | Skin type | Pre-treatment: No. of sessions | No.of treatment (Total=16) | Wavelength | Pulse duration | Fluence (J/cm2) | Spot size (mm) | Results | IWP | Adverse events | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 45 | F | IV | nevus of Ota | None | 3 | 755 | 750 | 4.07 | 2.5 | − | erythema(+) | |
| 755 | 750 | 4.07 | 2.5 | − | erythema(+) | ||||||||
| 755 | 750 | 4.07 | 2.5 | Good | − | erythema(+) | |||||||
| 2 | 48 | F | IV | recalcitrant nevus of Ota | Cryo: 4 QR:4 | 2 | 755 | 750 | 2.83 | 3 | − | erythema(+) | |
| 755 | 750 | 4.07 | 2.5 | Fair | + | erythema(+), crust(+),PIH(+) | |||||||
| 3 | 50 | F | III | recalcitrant nevus of Ota | QR:5 | 1 | 5 | 750 | 2.83 | 3 | Good | − | erythema(+) |
| 4 | 52 | F | IV | nevus of Ota | QR:3 | 3 | 755 | 750 | 2.83 | 3 | − | erythema(+) | |
| 755 | 750 | 3.49 | 2.7 | − | erythema(+) | ||||||||
| 755 | 750 | 4.07 | 2.5 | Good | + | erythema(+), crust(+),PIH(+) | |||||||
| 5 | 53 | F | IV | nevus of Ota | None | 2 | 755 | 750 | 2.83 | 3 | − | erythema(+) | |
| 755 | 750 | 5.26 | 2.2 | Exellent | + | erythema(+), crust(+),PIH(+) | |||||||
| 6 | 3 | M | III | nevus of Ota | QR:1 | 1 | 1064 | 450 | 2 | 4 | Exellent | − | erythema(++), swelling(+) |
| 9 | 51 | F | IV | ectopic Mongolian spot: shoulder | QR:1 | 1 | 755 | 750 | 4.07 | 2.5 | Good | − | erythema(+) |
| 8 | 0 | F | IV | ectopic Mongolian spot : arm | None | 1 | 1064 | 750 | 1 | 6 | Good | − | erythema(++), swelling(+) |
| 7 | 5 | M | IV | ectopic Mongolian spot : leg | None | 1 | 1064 | 750 | 2 | 4 | Good | − | erythema(++), swelling(+) |
| 10 | 13 | F | IV | persistent Mongolian spot | None | 1 | 755 | 750 | 2.83 | 3 | Good | ± | erythema(+), crust(+) |
The clinical outcome was evaluated by comparing the clinical photography at baseline and at 3 month after the final session. The clinical photography was assessed by two blinded independent plastic surgeons using a five category grading scale based on the pigment clearance and treatment response according to the percentage of skin lightening with Poor, 0–24%; Fair, 25–49%; Good, 50–74%; Excellent, 75–94%; and Complete, 95–100% improvement. Adverse events including the occurrence of crusting, blister formation, erythema, erosion, infection, hyperpigmentation and hypopigmentation, and these were assessed every treatment session.
Results
All ten patients obtained clinical improvement with varying degrees of clearance. In patients of nevus of Ota (n=6), two had excellent (75–95%), three had good (50–74%), and one had fair (25–49%) responses. In patients with ectopic Mongolian spots / Mongolian spots (n=4), all experienced a good (50-74%) response after only one treatment session. No patient was rated as Poor.
Anticipated complications were mild in severity and included transient erythema, swelling, pain and crust formation. All resolved completely within two weeks after treatment. In patients who were treated with the ps-Alex laser, transient hyperpigmentation was followed by improvement to complete resolution at 3 months follow-up in three patients. On the contrary, in patients who were treated with the ps-Nd:YAG laser, transient erythema and swelling were severe compared to the ps-Alex laser group, but no pigmentary adverse events were noted.
Representative results in two patients are shown for a nevus of Ota in a 52-year-old woman treated with the ps-Alex laser in 3 sessions (Figure 1), and an ectopic Mongolian spot in a 6-month-old female infant treated with one treatment of the ps-Nd:YAG laser (Figure 2). The independent grading in both patients was Good.
Figure 1: Case 5:
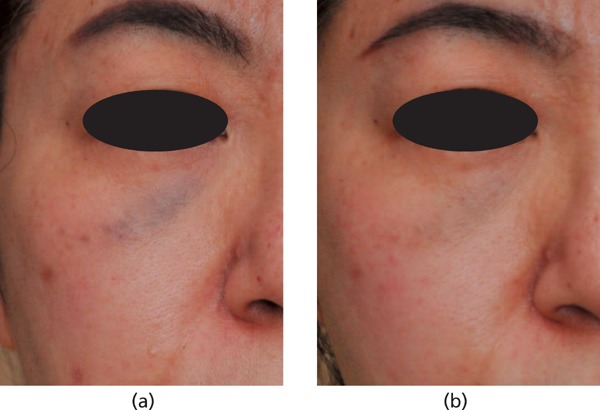
A 52-year-old woman with Fitzpatrick skin type IV who underwent treatment for nevus of Ota in the right periorbital region is seen at (a) pretreatment; (b) 3-month follow up after three treatments with the 755 nm picosecond alexandrite laser demonstrating good pigmentary clearance.
Figure 2: Case 8.
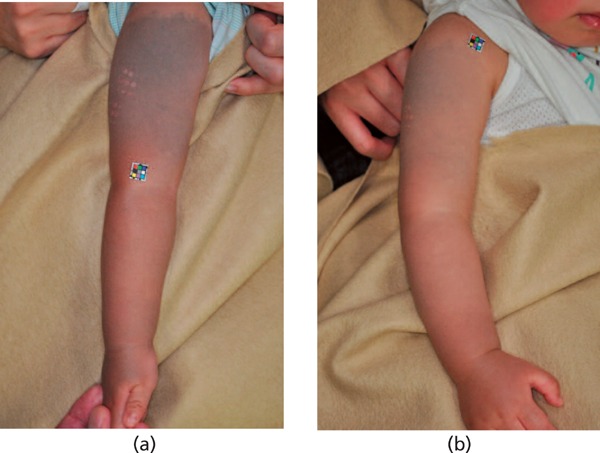
A 6-months-old baby with Fitzpatrick skin type IV with an ectopic Mongolian spot on her right arm is seen at (a) pretreatment; (b) 3-month follow-up after only one treatment with the 1064 nm picosecond Nd:YAG laser demonstrating good pigmentary clearance.
Discussion
To the best of our knowledge, this is the first retrospective study to demonstrate the efficacy of 755 nm and 1064 nm picosecond lasers for the treatment of dermal melanocytosis in Asians. Significant pigmentary reduction with minimum adverse events were achieved with few treatment sessions in the treatment of nevus of Ota, ectopic Mongolian spots, and Mongolian spot.
Only for the treatment of nevus of Ota, have Chestnuts et al. 15), Levin et al. 16) and Chan et al. 17) also reported the successful application of a ps-Alex laser. In our study, satisfactory responses (>50% clearance) were observed in five of our six patients with nevus of Ota. One patient with the recalcitrant type of Nevus Ota, who had undergone cryotherapy previously, obtained only a fair response. In this case, hard-to-see scar formations existed on the surface of the treated area, caused by the previous cryotherapy sessions. It was thought this scar tissue had interfered with the penetration of the laser energy into the dermis, and thus reduced the clinical efficacy. Though there was only one case, the application of the ps-Nd:YAG laser has also been found effective to achieve good clearance with minimum adverse events. Although limited to our study and current reports, the ps-domain laser appears efficacious for the treatment for nevus of Ota. Despite being sparse, the present data are however encouraging and further large prospective studies are warranted.
Mongolian spots are most common in Asians. They are found most frequently in the sacral region in infants and typically disappear during childhood. Ectopic Mongolian spots located in areas distal from the lumbosacral region may persist. We treated three ectopic Mongolian spots and one persistent Mongolian spot. In the treatment of ectopic Mongolian spots and Mongolian spot with picosecond lasers, in all cases (n=4) satisfactory responses (>50%) were obtained with only one treatment session, using both the ps-Alex and the ps-Nd:YAG lasers. When treating Mongolian spots, including the ectopic type, with the ns-domain Q-switched lasers, more than 3 treatment sessions with a 3 to 6-month interval has usually been required to resolve the lesions clinically, normally accompanied by prolonged post-inflammatory hyperpigmentation (PIH). The total treatment period thus tended to be extended. In our study, following both the ps-Alex and ps-Nd:YAG laser treatments, PIH was not noted and remarkable reduction of pigmentation was observed in all patients. Though our patient number was small, the uniformity of the findings suggests that picosecond laser treatment for Mongolian spots is expeditious, and patients can obtain good results in a short time with minimal side effects.
Concerning the irradiation end point in the treatment of dermal melanocytosis with the ns-domain Q-switched lasers in Asians, the immediate whitening phenomenon (IWP), caused by epidermal damage after laser irradiation, is usually used as one of the indices in order to obtain the reduction of pigmentation. In Asians, excessive epidermal injury, particularly involving damage at the dermoepidermal junction, usually induces PIH lasting 3 to 12 months. A minimum but adequate laser-tissue interaction is desirable to obtain the optimum clinical results. According to the results of our study, in 12 of all 16 treatments, patients obtained successful lightening without IWP and PIH. It implies the immediate whitening, which is usually followed by PIH in Asians, does not need to be obtained achieve clinical clearance in ps-laser treatment of dermal pigmented lesions. However, the optimal endpoints after a variety of ps-laser protocols should be defined through further large prospective studies.
To conclude, our results suggest that the novel picosecond lasers, both the 755 nm alexandrite and the 1064 nm Nd:YAG are efficacious for the treatment of dermal pigmented lesions such as nevus of Ota, and Mongolian spots of both the ectopic and persistent types. We recognize that ps-lasers could be one of the most important therapeutic options in laser treatment for dermal pigmented lesions. Our study is only a retrospective evaluation, and is limited in the number of patients. Well designed, large prospective clinical trials on non-treated individual pigmented lesions are needed to confirm our optimistic findings.
Disclosure of conflict of interest
The authers declare that they have no competing interests.
References
- 1: Ohshiro T. Laser treatment for nevi. 1980, Medical Laser Research Co. Ltd. Tokyo: pp17-52. [Google Scholar]
- 2: Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983; 220(4596):524-527. [DOI] [PubMed] [Google Scholar]
- 3: Anderson RR, Margolis RJ, Watanabe S, Flotte T, Hruza GJ, Dover JS. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd:YAG laser pulses at 1064, 532 and 355 nm. J Invest Dermatol. 1989; 93: 28-32. [DOI] [PubMed] [Google Scholar]
- 4: Watanabe S, Takahashi H. Treatment of nevus of Ota with Q-switched ruby laser. N Engl J Med. 1994; 331: 1745-50. [DOI] [PubMed] [Google Scholar]
- 5: Chang CJ, Nelson JS, Achauer BM. Q-switched ruby laser treatment of oculodermal melanosis (Nevus of Ota). Plast Reconstr Surg. 1996; 98:784-90. [DOI] [PubMed] [Google Scholar]
- 6: Chan HH, Leung RS, Ying SY, Lai CF, Kono T, Chua JK, Ho WS. A retrospective analysis of complications in the treatment of nevus of Ota with the Q-switched alexandrite and Q switched Nd:YAG lasers. Dermatol Surg. 2000; 26(11): 1000-6. [DOI] [PubMed] [Google Scholar]
- 7: Chang CJ, Kou CS. Comparing the effectiveness of Q-switched ruby laser treatment with that of Q switched Nd:YAG laser for occulodermal melanosis (Nevus of Ota). J Plast Reconst Aesthet Surg. 2011; 64: 339-45. [DOI] [PubMed] [Google Scholar]
- 8: Kagami S, Asahina A, Watanabe R, Mimura Y, Shirai A, Hattori N, Watanabe T, Tamaki K. Laser treatment of 26 Japanese patients with Mongolian spots. Dermatol Surg. 2008; 34(12): 1689-94. [DOI] [PubMed] [Google Scholar]
- 9: Shirakawa M, Ozawa T, Ohasi N, Ishii M, Harada T. Comparison of regional efficacy and complications in the treatment of aberrant Mongolian spots with the Q-switched ruby laser. J Cosmet Laser Ther. 2010; 12(3): 138-42. [DOI] [PubMed] [Google Scholar]
- 10: Ross V, Naseef G, Lin G, Kelly M, Michaud N, Flotte TJ, Raythen J, Anderson RR. Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol. 1998; 134(2): 167-71. [DOI] [PubMed] [Google Scholar]
- 11: Brauer JA, Reddy KK, Anolik R, Weiss ET, Karen JK, Hale EK, Brightman LA, Bernstein L, Geronemus RG. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol. 2012; 148(7): 820-3. [DOI] [PubMed] [Google Scholar]
- 12: Saedi N, Metelitsa A, Petrell K, Arndt KA, Dover JS. Treatment of tattoos with a picosecond alexandrite laser: a prospective trial. Arch Dermatol. 2012; 148(12): 1360-3. [DOI] [PubMed] [Google Scholar]
- 13: Alabdulrazzaq H, Brauer JA, Bae YS, Geronemus RG. Clearance of yellow tattoo ink with a novel 532-nm picosecond laser. Lasers Surg Med. 2015; 47(4): 285-8. [DOI] [PubMed] [Google Scholar]
- 14: Bernstein EF, Schomacker KT, Basilavecchio LD, Plugis JM, Bhawalkar JD. A novel dual-wavelength, Nd:YAG, picosecond-domain laser safely and effectively removes multicolor tattoos. Lasers Surg Med. 2015: 47; 542-548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15: Chesnut C, Diehl J, Lask G. Treatment of nevus of ota with a picosecond 755-nm alexandrite laser. Dermatol Surg. 2015; 41(4): 508-10. [DOI] [PubMed] [Google Scholar]
- 16: Levin MK, Ng E, Bae YS, Brauer JA, Geronemus RG. Treatment of pigmentary disorders in patients with skin of color with a novel 755 nm picosecond, Q-switched ruby, and Q-switched Nd:YAG nanosecond lasers: A retrospective photographic review. Lasers Surg Med. 2016; 48(2): 181-7. [DOI] [PubMed] [Google Scholar]
- 17: Chan JC, Shek SY, Kono T, Yeung CK, Chan HH. A retrospective analysis on the management of pigmented lesions using a picosecond 755-nm alexandrite laser in Asians. Lasers Surg Med. 2016; 48(1): 23-9. [DOI] [PubMed] [Google Scholar]


