Abstract
Aim
To verify the accuracy of automatic image registration (IR) between the planning kilo voltage computed tomography (kV CT) and megavoltage cone beam computed tomography (MV CBCT) datasets using phantom and patient images.
Background
The automatic IR between MV CBCT and planning kV CT is a fast solution for performing online image guided radiotherapy (IGRT). The IR accuracy has to be verified periodically as it directly affects patient setup accuracy.
Materials and methods
The automatic IR accuracy was evaluated using image quality phantom acquired with different kV CT slice thickness, different MV CBCT acquisition MUs and reconstruction slice size and thickness. The IR accuracy was also evaluated on patient images on different anatomical sites such as brain, head & neck, thorax and pelvis. The uncertainty in the automatic registration was assessed by introducing known offset to kV CT dataset and compared with the registration results.
Results
The result with the phantom images was within 2 mm in all three translational directions. The accuracy in automatic IR using patient images was within 2 mm in most of the cases. 3 mm planning kV CT slice thickness was sufficient to perform automatic IR successfully within 2 mm accuracy. The MV CBCT reconstruction parameters such as slice thickness and slice size had no effect on the registration accuracy.
Conclusion
This study shows that the automatic IR is accurate within 2 mm and provides confidence in performing them between planning kV CT and MV CBCT image datasets for online image guided radiotherapy.
Keywords: Automatic image registration, Cone beam computed tomography (CBCT), Image guided radiotherapy (IGRT)
1. Background
Advanced conformal radiotherapy delivery techniques, like the intensity modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT), have become routine in radiotherapy centres. These techniques require high accuracy in patient treatment positioning and alignment with respect to the treatment fields. Image guidance system utilising cone beam computed tomography reconstruction had contributed to achieve high precision in patient treatment positioning.1, 2, 3, 4 Megavoltage cone-beam computed tomography (MV CBCT) is one of the commercially available IGRT systems5, 6, 7 using megavoltage X-rays of the treatment beam from the linear accelerator (linac). The retractable amorphous silicon flat-panel detector mounted on the linac is used to acquire the 2D projection images at different gantry angles around the patient on the treatment couch and reconstruct 3D volumetric MV CBCT image which provide both soft tissue and bony structure information. The system provides software tools for automatic and manual registration of the MV-CBCT and (kilo Voltage) kV CT images acquired for patient treatment planning and calculate the patient position 3D translation offsets from which couch corrections can be made. Introduction of online image guidance in the patient treatment verification has increased the patient's time on treatment couch, which has the potential to induce patient intra-fraction movement, hence the preference to have a faster image guidance solution. The automatic registration, which uses mutual information to establish correspondence between the two image sets, helps to speed up the alignment process.8 In our radiotherapy department, we perform online image guidance with automatic image registration between the acquired MV CBCT and reference planning kV CT and visually inspect the results before applying the couch correction. The clinical implementation of the automatic image registration requires evaluating the uncertainties associated with it, as registration failures may result in very large errors.
2. Aim
The aim of this study is to verify the accuracy of automatic image registration between the planning kV CT and MV CBCT datasets in phantom with different CBCT acquisition and reconstruction parameters and with different planning CT slice thickness used clinically and in patient images at different sites.
3. Materials and methods
3.1. MV CBCT system
The Medical high energy linear accelerator, Siemens Oncor Expression™ equipped with the retractable imaging guidance (IG) system, (OPTIVUE 1000ST™, Siemens Medical solutions Inc., Concord, CA) used for MV planar and MV CBCT imaging, is attached to the gantry at the counter-part of the head of the linear accelerator, as shown in Fig. 1. The IG system consists of flat panel detectors which have the sensors of amorphous silicon (a-Si) photo diodes that are deposited on a glass substrate with a scintillator coating. The pixels have a pitch of 400 μm and there are 1024 × 1024 pixels covering a 40 × 40 cm2 area. The entire imaging system operates under SYNGO™ based COHERENCE™ therapist workspace, which communicates to the control console, the linear accelerator, and a local patient database. The workspace contains applications allowing for automatic acquisition of projection images, image reconstruction, CT-to-CBCT image registration, and couch position adjustment. Each projection of the CBCT acquisition is corrected for defective pixels, as well as for pixel-to-pixel offset and gain variations before 3D reconstruction.
Fig. 1.

The Siemens Oncor Expression linear accelerator equipped with OPTIVUE imaging system.
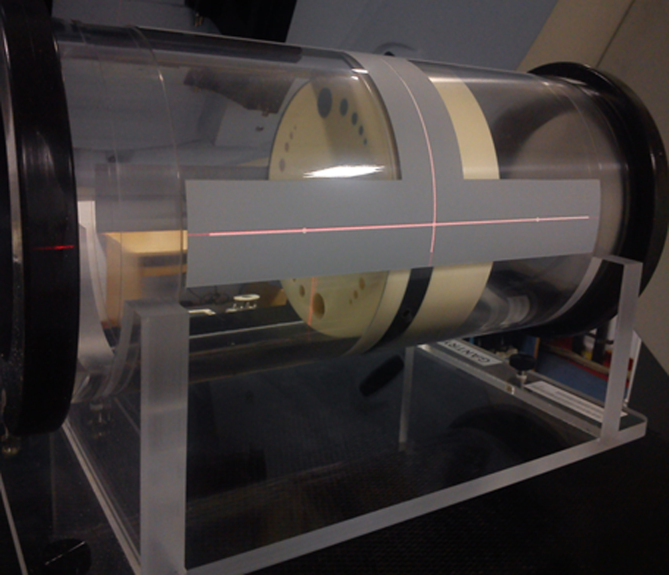
3.2. Phantom
The image quality phantom (Siemens Medical Solutions, Concord, CA), as shown in Fig. 2, is a cylindrical acrylic shell of diameter 20 cm with four solid water sections positioned axially within the shell. These sections are used to assess the MV CBCT image quality and geometric accuracy. Section 1 is purely made of solid water of thickness 4 cm without any inserts and used to check image uniformity, noise and artefacts. Sections 2 and 4 consist of 5 circular inserts of 8 different density materials with diameter 2, 1, 0.7, 0.5 and 0.3 cm used to check low and high contrast resolution. Section 3 contains 11 bar groups and each bar group contains 5 air bars to evaluate spatial resolution. The sections 2 and 4 are of thickness 2 cm each. In the outer shell, three axial planes (at the centre, head and foot of the phantom) have four tungsten beads at each plane, arranged at 12, 3, 6 and 9 o’clock positions to determine the geometric positional accuracy of CBCT image. In this study, we used this phantom to check the automatic image registration accuracy as it has different density material inserts.
Fig. 2.
Image quality phantom.
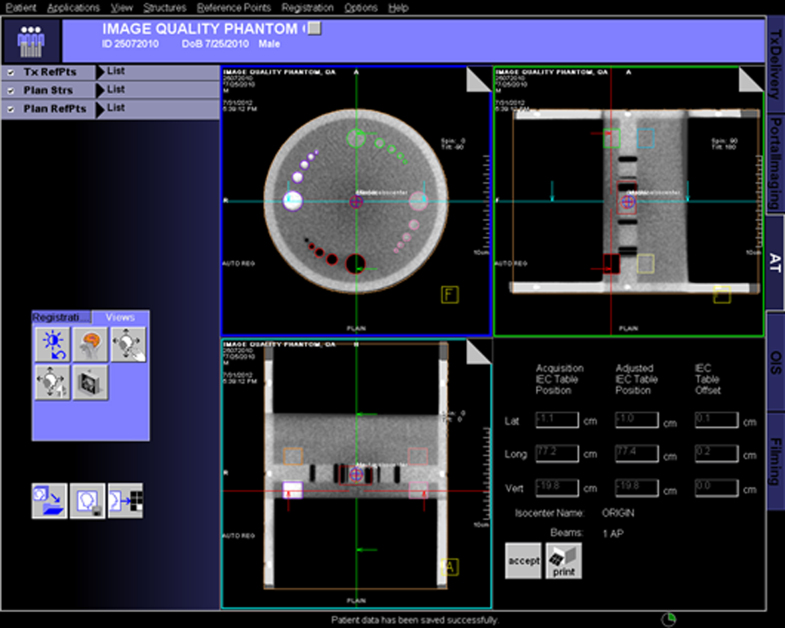
3.3. Adaptive targeting application
The Adaptive targeting (AT) application of Coherence Therapist system (Siemens Medical Solutions, Concord, CA), shown in Fig. 3 is used to register automatically or manually the planning kV CT image data set with the acquired MV CBCT image data set and on acceptance of image registration to display the table offset for correction. The Auto-registration uses the mutual information algorithm to automatically register the datasets by comparing all the voxels intensities for bony anatomy, soft tissue and air. The results of automatic registration are verified visually in the axial, coronal and sagittal planes before accepting the registration. Manual registration enables the user to manually specify a shift to the treatment isocentre such that planning volumes in the kV CT dataset correspond to visible anatomy in the treatment MV CBCT dataset.
Fig. 3.
Adaptive targeting application window.
Reference planning kV CT image dataset of the phantom The image quality phantom was aligned with its tungsten beads at the central plane to the laser system in the CT simulator. The phantom was scanned using Siemens SOMATOM EMOTION CT scanner in a helical scan mode with a matrix size of 512 × 512. Two different planning CT scan series were acquired with slice thickness of 1 mm and 3 mm. These images were transferred to the Oncentra treatment planning system (TPS) and the two image series were imported separately. The intersection of the central fiducial markers on the phantom was called the origin. The external body contour and different density inserts were contoured and a simple plan was created with the treatment isocentre coinciding with the origin. The entire plan along with CT images of the phantom, contours and isocentre information were transferred to the COHERENCE workstation. The imported planning CT image dataset serves as a standard reference to register with the MV-CBCT image dataset.
Uncertainties in phantom and imager positioning and in registration The image quality phantom was set up on the treatment table with its tungsten beads at the central plane aligned with the machine isocentre using room lasers. Standard MV CBCT images of the phantom were acquired with a high MU cone beam protocol of 60 Mus, 512 × 512 pixel image resolution and reconstruction slice thickness of 1 mm. On the MV CBCT axial images displayed on the AT application window, the reference point cursor was placed on each tungsten bead to read the three dimensional position co-ordinates. Since the phantom dimension and each bead position is known, the obtained values were compared with the actual position of each bead. This procedure was done to ensure correct positioning of the phantom with respect to the imaging geometry. Uncertainty due to positioning of the imager was determined by retracting and repositioning the imager each of the five times followed by imaging and registration. Uncertainty due to the acquisition and reconstruction process was determined by repeating the CBCT imaging and registration of these images with the reference image data for five times.
Accuracy of automatic image registration using phantom images Once the accurate positioning of the phantom at the isocentre was verified, MV CBCT images were obtained with clinically used acquisition and reconstruction parameters. The scans were repeated for 5 sets of different known shifts introduced to the CBCT images by offsetting the treatment table in the lateral, longitudinal and vertical directions, as given in Table 1. The acquired MV CBCT images were registered automatically with the reference planning kV CT dataset and the registration results were visually verified. Each time the system computed offset from automatic registration were noted and compared with the applied table offset.
-
(a)
Accuracy with different acquisition parameters (MUs)
Automatic image registrations were performed with CBCT acquired with different MU, such as 6, 8 and 15 Mus, to study the registration accuracy dependency on CBCT image quality.
-
(b)
Accuracy with different reconstruction parameters
The CBCT acquired with 6,8 and 15 MU were again reconstructed offline to vary the reconstruction parameters such as slice thickness of 1 mm and 3 mm and slice size of 512 × 512 pixels and 256 × 256 pixels to study the dependency of image registration accuracy on image resolution.
-
(c)
Accuracy with different planning kV CT slice thickness
Registrations were repeated with different planning CT slice thickness of 1 mm and 3 mm with CBCT acquired with different acquisition and reconstruction parameters to study the registration accuracy with planning CT slice thickness.
Table 1.
3D translational MV CBCT offsets introduced through treatment table.
| S. no. | Translational offsets, mm |
||
|---|---|---|---|
| Lateral (X) | Longitudinal (Y) | Vertical (Z) | |
| Set 1 | 0 | 20 | −10 |
| Set 2 | 5 | −20 | 10 |
| Set 3 | 10 | −10 | 0 |
| Set 4 | −5 | 10 | 5 |
| Set 5 | −10 | 0 | −5 |
Accuracy of automatic image registration using patient images The automatic image registration accuracy was studied for different treatment sites, such as the brain, head and neck, thorax and pelvis on patient images. The registration accuracy was evaluated on planning kV CT and MV CBCT images of 40 patients, (10 Brain, 10 Head & Neck, 10 Thorax and 10 Pelvis) who were previously treated using MV CBCT image guidance. All the 40 patients were scanned with a planning kV CT slice thickness of 3 mm and the MV CBCT acquired with 6 MU for the brain and head & neck, 8 MU for the thorax, 15 MU for the pelvis with 1 mm reconstruction slice thickness and 256 × 256 pixels slice size. For all patients, the MV CBCT image acquired in first week of treatment after initial setup correction was registered with the planning kV CT dataset and residual errors, if any, were noted and their respective corrections were made on the translational isocentre co-ordinates on the TPS so that the planning kV CT dataset exactly match with the acquired MV CBCT dataset. In the planning kV CT dataset on the TPS, 5 sets of known shifts were applied to the isocenter co-ordinates as given in Table 1 in the lateral, longitudinal and vertical directions and each set was exported to the COHERENCE workstation and registered with the acquired MV CBCT images. The registration results were visually verified and the obtained translational offsets were compared with that applied on the planning kV CT patient images.
4. Results
4.1. Uncertainties in phantom and imager positioning and in registration
Table 2 shows the mean and standard deviation of phantom and imager positioning and registration uncertainties in the three translational directions. This shows that the accuracy of imager and phantom positioning was less than 1 mm in any direction and the registration results were consistent.
Table 2.
Results showing mean error with 1σ (standard deviation) of phantom and imager positioning uncertainty and registration uncertainty in lateral (X), longitudinal (Y) and vertical (Z) directions.
| Phantom positioning uncertainty, mm | Imager positioning uncertainty, mm | Registration uncertainty, mm | ||||||
|---|---|---|---|---|---|---|---|---|
| X | Y | Z | X | Y | Z | X | Y | Z |
| 0.1 ± 0.1 | 0.0 ± 0.2 | −0.1 ± 0.2 | 0.0 ± 0.2 | 0.0 ± 0.2 | −0.1 ± 0.3 | 0.0 ± 0.0 | 0.0 ± 0.0 | 0.0 ± 0.0 |
4.2. Accuracy of automatic image registration
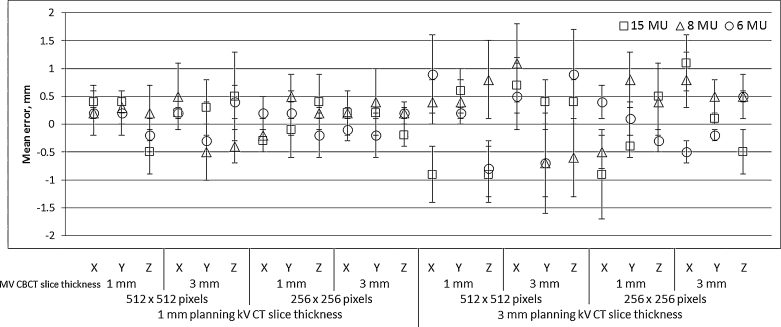
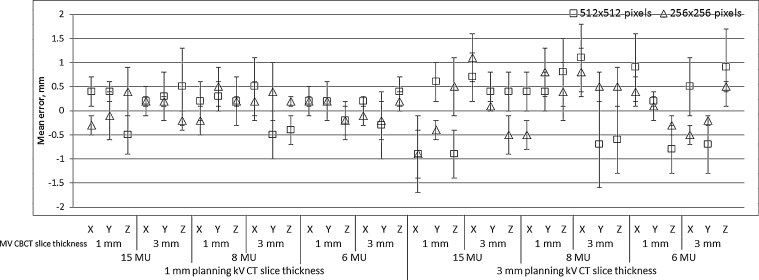
The mean and standard deviation of difference between the applied offset and the system calculated correction with automatic registration were calculated and plotted against different MV CBCT acquisition and reconstruction parameters.
-
(a)
Accuracy with different acquisition parameters (MUs)
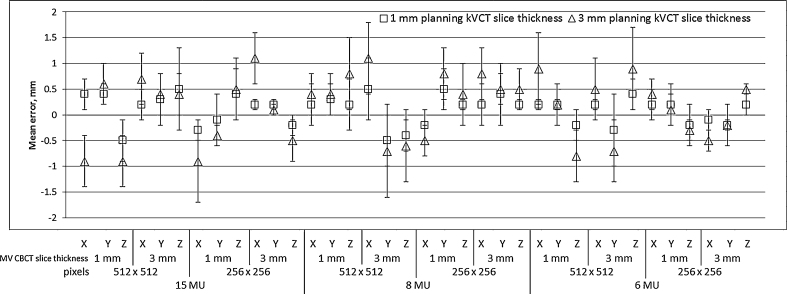
Fig. 4 shows that the offset calculation accuracy of automatic image registration is within 2 mm with different Mus used to acquire the MV CBCT images. The results indicate that there is no difference in the registration accuracy between different imaging Mus. Improving the image quality by increasing the imaging dose have no effect on the accuracy of automatic registration.
-
(b)
Accuracy with different reconstruction parameters
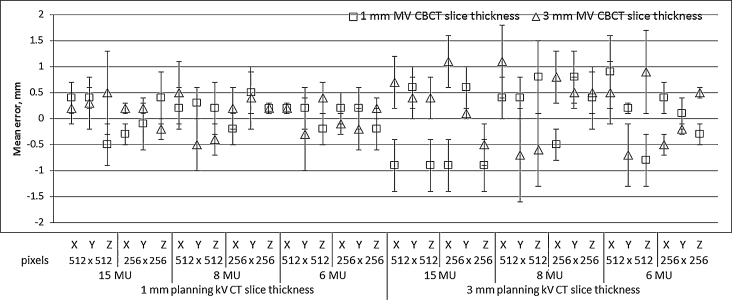
Fig. 5, Fig. 6 show the mean and standard deviation of the error in offset calculation accuracy using automatic image registration of MV CBCT reconstructed with different slice size and slice thickness, respectively. The results indicate that the registration accuracy was within 2 mm with different MV CBCT reconstruction slice thickness of 1 mm and 3 mm and different slice size of 512 and 256 pixels.
-
(c)
Accuracy with different planning CT slice thickness
Fig. 7 shows that the automatic registration accuracy was within 2 mm in both 1 mm and the 3 mm planning CT slice thickness. Also Fig. 4, Fig. 5, Fig. 6 show lesser registration accuracy in the 3 mm planning CT slice thickness than the 1 mm slice thickness, but both within 2 mm accuracy. As the system uses the mutual pixel information algorithm for automatic image registration, with the lesser the slice thickness the better the image resolution, and provides a better registration accuracy. For most of the clinical protocols, the planning CT is acquired with 3 mm slice thickness which is sufficient to achieve 2 mm registration accuracy.
Fig. 4.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration with different MV CBCT acquisition MUs.
Fig. 5.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration with different MV CBCT reconstruction slice size.
Fig. 6.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration with different MV CBCT slice thickness.
Fig. 7.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration with different planning kV CT slice thickness.
4.3. Accuracy of automatic image registration using patient images
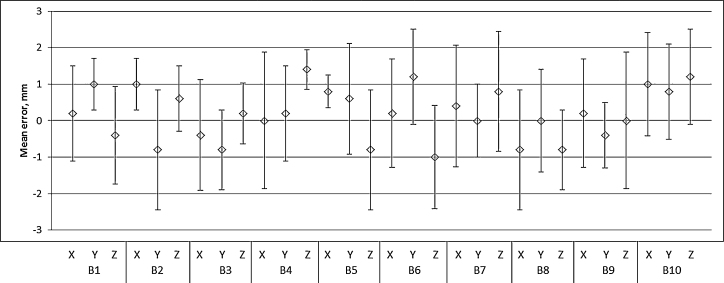
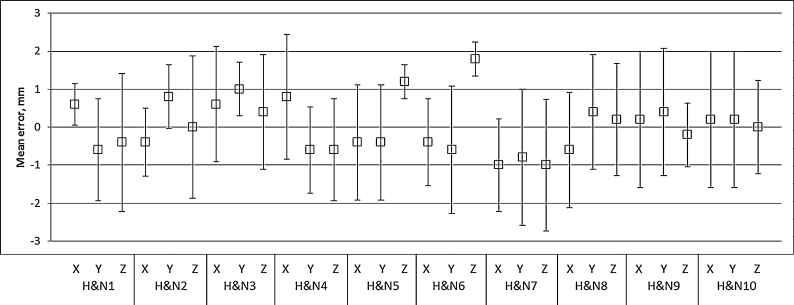
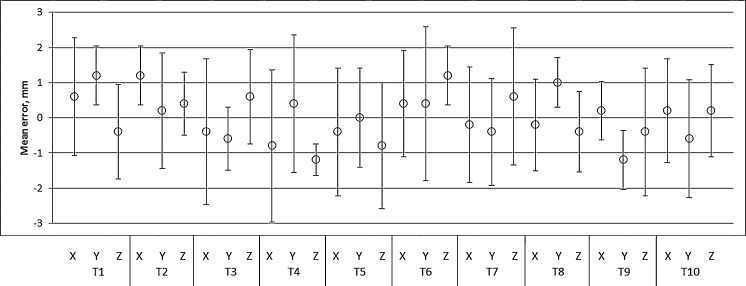
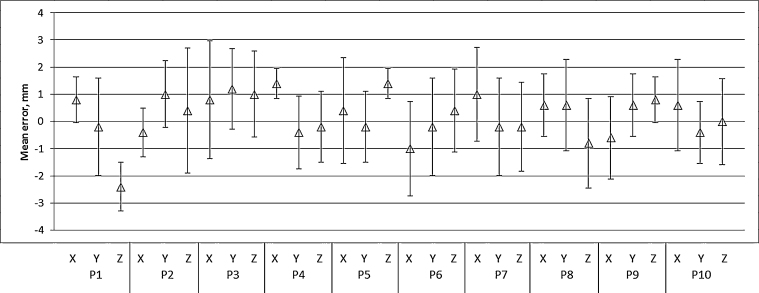
The mean and standard deviation of difference between the applied offset and the system calculated correction with automatic registration for the 5 sets were calculated and plotted for different sites on patient images. Fig. 8, Fig. 9 show that the automatic registration accuracy was within 2 mm for the brain and head & neck sites respectively. Fig. 10, Fig. 11 show that the automatic registration accuracy was within 2 mm for most of the cases in the thorax and pelvis sites, respectively. In these sites, the maximum error calculated was 3 mm in any direction.
Fig. 8.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration using patient images in brain (B1-10) site.
Fig. 9.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration using patient images in head and neck (H&N1-10) site.
Fig. 10.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration using patient images in thorax (T1-10) site.
Fig. 11.
Mean error with 1σ (Standard deviation) in 3D translational offset calculation with automatic image registration using patient images in pelvis (P1-10) site.
4.4. Discussion
In this study, the accuracy of automatic image registration between the MV CBCT and planning kV CT used in image guided radiotherapy was evaluated with different acquisition and reconstruction parameters of MV CBCT and different planning CT slice thickness.
It is required to ensure the safety and accuracy of MV CBCT system for clinical use. The positioning accuracy of the imager with respect to the treatment beam, geometric accuracy of the CBCT system, image quality of the planar and CBCT images were studied through periodic quality assurance programme.9 The accuracy of the isocentre with respect to the gantry was measured to be less than 1 mm. We use the Siemens MV CBCT system routinely for accurate patient positioning for conformal treatment techniques. The automatic image registration tool which helps to register the acquired MV CBCT images with the planning kV CT images allows faster assessment of patient set-up error than manual registration thereby reducing the patient's time on a treatment couch. We studied the accuracy of automatic image registration with respect to the parameters such as planning CT slice thickness, MV CBCT acquisition Mus, reconstruction slice thickness, slice size which may have potential impact on the accuracy of the registration. The image quality phantom, provided by the vendor along with the machine was used to analyse the accuracy of automatic image registration as the phantom had different density materials similar to that of human body.
In our study we found that 3 mm planning kV CT slice thickness was sufficient to perform automatic image registration successfully within 2 mm accuracy, even though 1 mm slice thickness could perform better registration. We found that the parameters such as MV CBCT slice thickness and slice size had no effect on the registration accuracy. With the use of 3 mm slice thickness and 256 × 256 pixels slice resolution the MV CBCT reconstruction time was almost reduced to half the time required to reconstruct 1 mm slice thickness and 512 × 512 pixels slice size.
Our study is unique in evaluating the accuracy of automatic image registration on patient images at different sites such as the brain, head & neck, thorax and pelvis. The automatic registration was accurate enough to register the image data sets within 2 mm accuracy for most of the cases. In a few cases of the thorax and pelvis sites, a difference of 3 mm was noted. This may be because of the changes in the patient anatomy between the acquisition of planning kV CT and MV CBCT image datasets. It may also be due to the limited field of view of the MV CBCT system of 27 × 27 × 27 cm3, unable to provide entire anatomy information in these sites.
MV CBCT system provides only the translational offsets in three directions but does not provide one in the rotational direction. Hence, we did not study the rotational correction accuracy of the system.
5. Conclusions
The accuracy of automatic image registration between the MV CBCT and planning kV CT used in image guided radiotherapy has been evaluated with a different acquisition and reconstruction parameter of MV CBCT and a different planning CT slice thickness. The offset calculation accuracy with the automatic image registration was found to be within 2 mm in all three translational directions when evaluated using a phantom. The results were better with 1 mm planning kV slice thickness compared to 3 mm slice thickness. The accuracy in automatic image registration using patient images was within 2 mm in most of the cases at different sites.
Conflict of interest
None declared.
Financial disclosure
None declared.
Acknowledgements
None declared.
References
- 1.Mosleh-Shirazi M.A., Evans P.M., Swindell W., Webb S., Partridge M. A cone-beam megavoltage CT scanner for treatment verification in conformal radiotherapy. Radiother Oncol. 1998;48(3):319–328. doi: 10.1016/s0167-8140(98)00042-5. [DOI] [PubMed] [Google Scholar]
- 2.Bylund K.C., Bayouth J.E., Smith M.C., Hass A.C., Bhatia S.K., Buatti J.M. Analysis of interfraction prostate motion using megavoltage cone beam computed tomography. Int J Radiat Oncol Biol Phys. 2008;72(3):949–956. doi: 10.1016/j.ijrobp.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Welsh J.S., Bradley K., Ruchala K.J. Megavoltage computed tomography imaging: a potential tool to guide and improve the delivery of thoracic radiation therapy. Clin Lung Cancer. 2004;5(5):303–306. doi: 10.3816/CLC.2004.n.010. [DOI] [PubMed] [Google Scholar]
- 4.Higgins J., Bezjak A., Hope A. Effect of image-guidance frequency on geometric accuracy and setup margins in radiotherapy for locally advanced lung cancer. Int J Radiat Oncol Biol Phys. 2011;80(5):1330–1337. doi: 10.1016/j.ijrobp.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Pouliot J., Bani-Hashemi A., Aubin M. Clinical intergration of a MV cone-beam system for image guided treatment. Med Phys. 2005;32:1938. [Google Scholar]
- 6.Morin O., Gillis A., Chen J. Megavoltage cone-beam CT: system description and clinical applications. Med Dosim. 2006;31(1):51–61. doi: 10.1016/j.meddos.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 7.Pouliot J., Bani-Hashemi A., Chen J. Low-dose megavoltage cone-beam CT for radiation therapy. Int J Radiat Oncol Biol Phys. 2005;61(2):552–560. doi: 10.1016/j.ijrobp.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Smitsmans M.H., de Bois J., Sonke J.J. Automatic prostate localization on cone-beam CT scans for high precision image-guided radiotherapy. Int J Radiat Oncol Biol Phys. 2005;63(4):975–984. doi: 10.1016/j.ijrobp.2005.07.973. [DOI] [PubMed] [Google Scholar]
- 9.Kanakavelu N., Samuel E.J.J. Assessment and evaluation of MV image guidance system performance in radiotherapy. Rep Pract Oncol Radiother. 2015;20(3):188–197. doi: 10.1016/j.rpor.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]