Abstract
Purpose
This study was aimed to evaluate the effect of time of surgery for acute appendicitis on surgical outcomes to optimize the timing of appendectomies.
Methods
Medical records of patients who underwent an appendectomy were reviewed to obtain data on time of symptom onset, time of hospital presentation, and start times of surgery. Surgical findings were used to define appendicitis as either uncomplicated or complicated. The uncomplicated group included patients with simple, focal, or suppurative appendicitis, and the complicated group included patients with gangrenous, perforated appendicitis or periappendiceal abscess formation. The 2 groups were analyzed by age, sex, and time.
Results
A total of 192 patients were analyzed. The mean time from symptom onset to start of operation showed a significant difference between both groups (1,652.9 minutes vs. 3,383.8 minutes, P < 0.001). The mean time from hospital visit to start of operation showed no difference between both groups (398.7 minutes vs. 402.0 minutes, P = 0.895). Operating within 24 hours of symptom onset had a relative risk of 1.738 (95% confidence interval, 1.319–2.425) for complications. Operating more than 36 hours after symptom onset was associated with an increased risk of postoperative ileus and a longer hospital stay.
Conclusion
Complicated appendicitis is associated with a delay in surgery from symptom onset rather than a delay at hospital arrival. Surgeons should take into account the time from symptom onset when deciding on the timing of appendectomy. We recommend that appendectomy be performed within 36 hours from symptom onset.
Keywords: Appendectomy, Appendicitis, Treatment outcome
INTRODUCTION
Appendicitis has been known to require emergency management [1]. Without immediate surgery, appendicitis may progress to perforation of the appendix. Therefore, an appendectomy should be performed urgently, irrespective of the time of day. Many studies support emergency appendectomy [2,3,4,5]. However, there is evidence that delayed appendectomy is acceptable and some studies have reported that it is not associated with a higher rate of complications [6,7,8].
Therefore, the optimal timing for appendectomy remains controversial. The overall time (OT) between symptom onset and surgery for treatment of appendicitis comprises pre-hospital time (PT), the time from symptom onset to visiting the hospital, and in-hospital time (IT), the time from visiting the hospital to the start of the operation. The aim of the present study was to evaluate the relationship between variables of time and outcomes based on appendicitis severity. In addition, as a secondary outcome, postoperative outcomes were evaluated in regards to surgical timing. Accordingly, the authors sought to determine recommendations for appendectomy timing relative to disease severity.
METHODS
The present study was based on a retrospective review of medical records. The Institutional Review Board approved the study and waived informed consent. Patients undergoing surgery for appendicitis between 1 January 2013 and 31 December 2013 were included in the study.
Patients treated by drainage procedure, not by resection, were excluded. In our center, conservative treatment for appendicitis with antibiotics alone was not adopted. Medical records were reviewed to identify the following factors: gender, age, time of symptom onset, when the patient presented at the hospital, when the operation started, surgical findings, postoperative complications, and length of hospital stay. The time when nausea, vomiting, dyspepsia, epigastric pain, or any other abdominal pain was reported by the patients was defined as the time of symptom onset. Surgical findings were divided into either uncomplicated appendicitis or complicated appendicitis. Simple, focal, or suppurative appendicitis were regarded as uncomplicated appendicitis, and gangrenous, perforated appendicitis, and periappendiceal abscess formation were regarded as complicated appendicitis.
The result of the operation, based on surgical findings, was the primary outcome, and was analyzed with respect to PT and IT. The postoperative outcomes of ileus and length of hospitalization stay were also analyzed. Patients with postoperative nausea, vomiting or absence of gas passage were checked via simple abdominal X-ray to diagnose ileus.
SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Independent t-tests were used for quantitative comparison of data and chi-square and Fisher exact tests were used for qualitative comparison. A P-value of <0.05 was considered statistically significant.
RESULTS
A total of 192 consecutive patients over a period of 1 year were included in the study. The overall mean age was 33.6 ± 19.5 years (range, 3–86 years). Male patients accounted for 51.6% (n = 99) of total patients. The mean duration of hospital stay was 4.1 ± 1.6 days (range, 2–14 days). Patients with complicated appendicitis accounted for 51.0% (n = 99) of individuals. Every patient was treated by appendectomy. Every enrolled patient was treated by laparoscopic appendectomy. There were no conversions or open appendectomies. Also, there was no case treated by ileocecectomy or right colectomy.
Patient characteristics are shown in Table 1. There was a significant association between patients with complicated appendicitis and age, and longer duration of operation, and hospital stay. There were also associations between complicated appendicitis and delays in PT and OT (1,254.2 ± 1,424.7 minutes vs. 2,986.7 ± 3,980.1 minutes, P < 0.001, 1,652.9 ± 1,445.2 minutes vs. 3,388.8 ± 3,982.2 minutes, P < 0.001, respectively). However, there was no significant association between complicated appendicitis and IT (398.7 ± 154.0 minutes vs. 402.0 ± 194.9 minutes, P = 0.895).
Table 1. Patient characteristics in cases of uncomplicated appendicitis and complicated appendicitis.
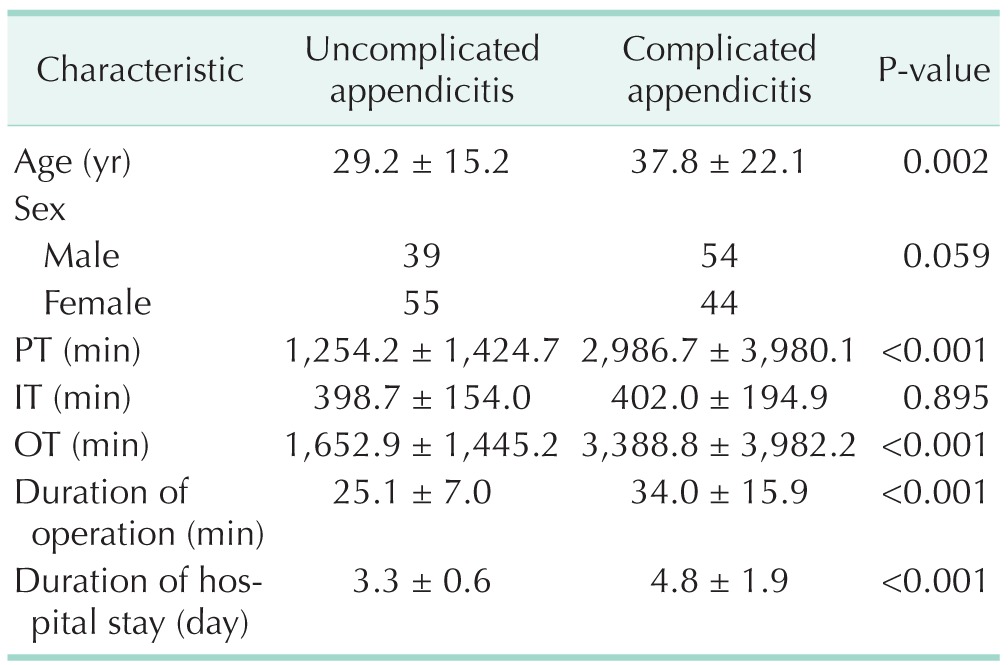
Values are presented as mean ± standard deviation or number.
PT, pre-hospital time (time between onset of symptoms and hospital visit); IT, in-hospital time (time between hospital visit and operation); OT, overall time (time between onset of symptom and operation).
Analysis of OT, a controllable factor, showed there was a significant association between starting the operation 24, 36, and 48 hours after symptom onset and complicated appendicitis (relative risk [95% confidence interval], 1.738 [1.319–2.425], 2.029 [1.366–3.014], 2.061 [1.309–3.244]) (Table 2). In addition, PT had a significant association, although it is an uncontrollable factor. We found that PT, when visiting the hospital 12, 24, and 36 hours after symptom onset had an association with complicated appendicitis (relative risk [95% confidence interval], 1.626 [1.225–2.160], 2.328 [1.576–3.438], and 1.912 [1.251–2.923], respectively). However, IT, the other controllable factor, showed no significant association with the severity of appendicitis.
Table 2. Analysis of type of appendicitis and elapsed time.
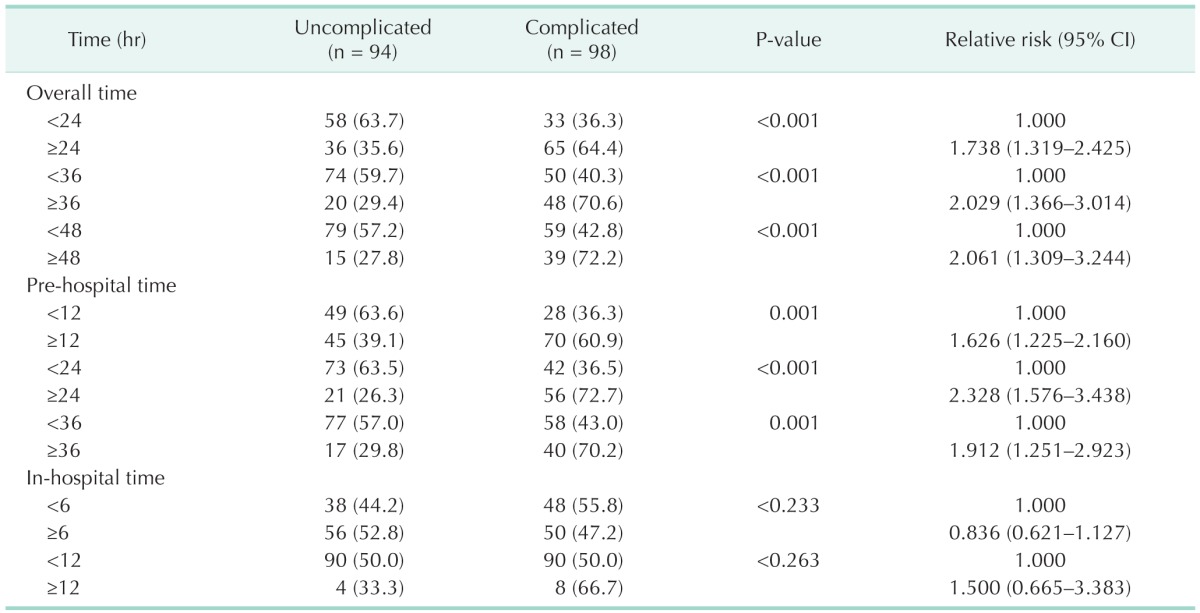
Values are presented as number (%).
CI, confidence interval.
Starting the operation more than 36 hours from symptom onset was associated with a higher risk of postoperative ileus (0% vs. 5.9%, P = 0.0024). This delay also led to longer hospital stays (3.8 ± 1.5 vs. 4.7 ± 1.7, P < 0.001) (Table 3). No significant differences were found for other complications, such as wound infection or postoperative pericecal inflammation [2,4]. Additionally, analysis of postoperative outcome by IT yielded no significant differences.
Table 3. Analysis of postoperative outcome and time between symptom onset and start of operation.
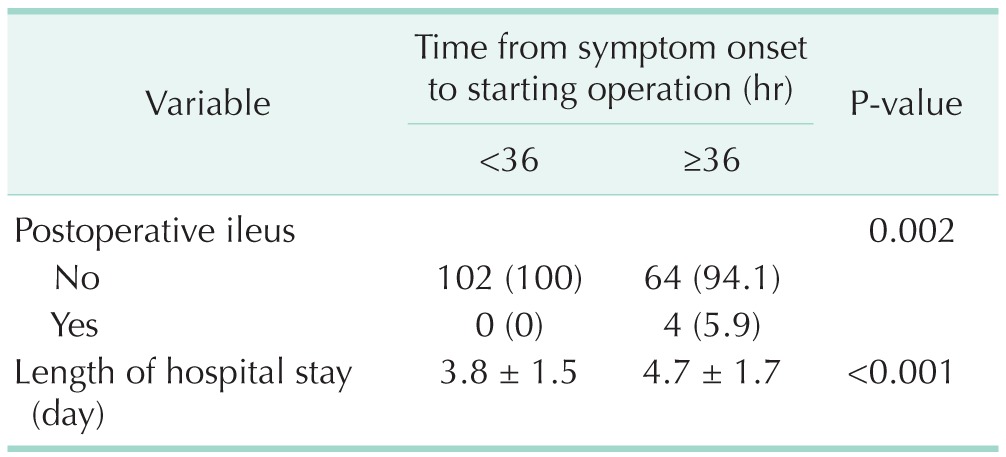
Values are presented as number (%) or mean ± standard deviation.
DISCUSSION
The aim of the present study was to examine whether the variable of appendectomy timing has an effect on outcomes for acute appendicitis. Several studies have shown that delayed appendectomies after hospital presentation are associated with poor outcomes [2,4,9]. Busch et al. [2] reported that an IT delay of more than 12 hours was an independent risk factor for perforation. Giraudo et al. [4] reported that delayed appendectomy, after 24 hours from onset, increases the complication rate. In addition, Papandria et al. [9] reported inpatient delay to be associated with a higher perforation rate. In contrast, results from other studies have supported delays in appendectomies [6,7,8]. Teixeira reported that appendectomy delay did not increase perforation risk [6]. In addition, Abou-Nukta et al. [7] reported that delaying operation 12 to 24 hours after presentation does not increase the risk of perforation. Still, ideal timing of appendectomy is a controversial issue.
Previous studies on the timing of appendectomies have nearly always analyzed IT alone [2,4,6,7,9]. In comparison, the present study evaluated both OT and IT. Evaluating not only IT, but both parameters, might be more rational, considering the pathophysiology of appendicitis. Separation of these variables of time enabled further analysis and identification of the more important variable.
In the present study, patients in the complicated appendicitis group had longer OT and PT periods. However, no significant associations were shown for IT. Although OT and IT are both controllable factors, only OT demonstrated a significant association with outcomes. It showed that reducing IT alone could not improve the results of appendectomies and reducing OT would yield better prognoses. Further analysis of OT showed that operating more than 36 hours after symptom onset had a relative risk of 2.029 compared with operating within 36 hours. Moreover, operating after 36 hours increased the risk of postoperative ileus and a longer hospital stay.
The timing of onset of symptoms of appendicitis is important in deciding when to perform acute care surgery. Delayed surgery from symptom onset is associated with worse outcomes for peptic ulcer perforation [10,11]. Additionally, a similar study on appendicitis reported that a delay in the overall timing of treatment increased the risk of progression of pathology and postoperative complications [3]. Similarly, OT had a significant association in the present study.
Although PT showed statistical significance, it is not easy to shorten this time period directly. Therefore, it is recommended that clinicians focus on shortening OT. Reducing PT might be accomplished through the dissemination of publicity.
In the present study, only 12 appendectomies were performed 12 hours after the patient visited the hospital. The mean IT of both groups was approximately 400 minutes and is much shorter than in previous studies. Inclusion of a larger number of patients with a higher number of delayed appendectomies may yield a different result.
Recently, several studies about nonoperative treatments for appendicitis have been reported [12,13,14]. However, the failure rate of conservative treatment was reported as approximately 10% [15]. Some cases of simple appendicitis could be treated with antibiotics; however, other cases of appendicitis that do not respond to conservative treatment might worsen and result in severe complications [16]. Therefore, nonoperative treatment was not performed in our hospital nor enrolled to the present study.
The mean IT of all patients in this study was about 400 minutes, much shorter than previously reported ITs of 7.1 to 11.8 hours [2,6,17,18]. There might be several reasons for our short IT. One possible reason was that an in-house trauma surgeon participated in emergency surgeries during the study period. Therefore, appendectomy could be performed more promptly [19].
One limitation of this study is that it is retrospective and includes a relatively small sample size. However, this is consistent with several retrospective studies of appendixes that analyzed fewer than 200 subjects [20,21,22]. Another large-scale, multicenter study may yield further outcomes.
The initial symptoms of appendicitis are known to be vague and nonspecific. However, because the symptoms depend on patients' subjective feelings, the investigators had to rely on patients' statements. The time when any known symptoms, such as nausea, vomiting, anorexia, or abdominal pain were reported by the patient was regarded as the onset of appendicitis symptoms [23].
It can be concluded that a delay in OT is associated with complicated appendicitis. An OT longer than 36 hours was associated with a higher risk of postoperative ileus and a longer hospital stay. Surgeons should take into account the time from symptom onset when deciding on the timing of appendectomy. We recommend that appendectomy be performed within 36 hours of symptom onset.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Korner H, Sondenaa K, Soreide JA, Andersen E, Nysted A, Lende TH, et al. Incidence of acute nonperforated and perforated appendicitis: age-specific and sex-specific analysis. World J Surg. 1997;21:313–317. doi: 10.1007/s002689900235. [DOI] [PubMed] [Google Scholar]
- 2.Busch M, Gutzwiller FS, Aellig S, Kuettel R, Metzger U, Zingg U. In-hospital delay increases the risk of perforation in adults with appendicitis. World J Surg. 2011;35:1626–1633. doi: 10.1007/s00268-011-1101-z. [DOI] [PubMed] [Google Scholar]
- 3.Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244:656–660. doi: 10.1097/01.sla.0000231726.53487.dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giraudo G, Baracchi F, Pellegrino L, Dal Corso HM, Borghi F. Prompt or delayed appendectomy? Influence of timing of surgery for acute appendicitis. Surg Today. 2013;43:392–396. doi: 10.1007/s00595-012-0250-5. [DOI] [PubMed] [Google Scholar]
- 5.Omundsen M, Dennett E. Delay to appendicectomy and associated morbidity: a retrospective review. ANZ J Surg. 2006;76:153–155. doi: 10.1111/j.1445-2197.2006.03673.x. [DOI] [PubMed] [Google Scholar]
- 6.Teixeira PG, Sivrikoz E, Inaba K, Talving P, Lam L, Demetriades D. Appendectomy timing: waiting until the next morning increases the risk of surgical site infections. Ann Surg. 2012;256:538–543. doi: 10.1097/SLA.0b013e318265ea13. [DOI] [PubMed] [Google Scholar]
- 7.Abou-Nukta F, Bakhos C, Arroyo K, Koo Y, Martin J, Reinhold R, et al. Effects of delaying appendectomy for acute appendicitis for 12 to 24 hours. Arch Surg. 2006;141:504–506. doi: 10.1001/archsurg.141.5.504. [DOI] [PubMed] [Google Scholar]
- 8.Eko FN, Ryb GE, Drager L, Goldwater E, Wu JJ, Counihan TC. Ideal timing of surgery for acute uncomplicated appendicitis. N Am J Med Sci. 2013;5:22–27. doi: 10.4103/1947-2714.106186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papandria D, Goldstein SD, Rhee D, Salazar JH, Arlikar J, Gorgy A, et al. Risk of perforation increases with delay in recognition and surgery for acute appendicitis. J Surg Res. 2013;184:723–729. doi: 10.1016/j.jss.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Svanes C, Lie RT, Svanes K, Lie SA, Soreide O. Adverse effects of delayed treatment for perforated peptic ulcer. Ann Surg. 1994;220:168–175. doi: 10.1097/00000658-199408000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Surapaneni S, S R, Reddy A VB. The perforation-operation time interval; an important mortality indicator in peptic ulcer perforation. J Clin Diagn Res. 2013;7:880–882. doi: 10.7860/JCDR/2013/4925.2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salminen P, Paajanen H, Rautio T, Nordstrom P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: The APPAC Randomized Clinical Trial. JAMA. 2015;313:2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 13.Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, noninferiority, randomised controlled trial. Lancet. 2011;377:1573–1579. doi: 10.1016/S0140-6736(11)60410-8. [DOI] [PubMed] [Google Scholar]
- 14.Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156. doi: 10.1136/bmj.e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu K, Fogg L. Use of antibiotics alone for treatment of uncomplicated acute appendicitis: a systematic review and metaanalysis. Surgery. 2011;150:673–683. doi: 10.1016/j.surg.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Hua J, Yao L, He ZG, Xu B, Song ZS. Necrotizing fasciitis caused by perforated appendicitis: a case report. Int J Clin Exp Pathol. 2015;8:3334–3338. [PMC free article] [PubMed] [Google Scholar]
- 17.Drake FT, Mottey NE, Farrokhi ET, Florence MG, Johnson MG, Mock C, et al. Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg. 2014;149:837–844. doi: 10.1001/jamasurg.2014.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clyde C, Bax T, Merg A, MacFarlane M, Lin P, Beyersdorf S, et al. Timing of intervention does not affect outcome in acute appendicitis in a large community practice. Am J Surg. 2008;195:590–592. doi: 10.1016/j.amjsurg.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Earley AS, Pryor JP, Kim PK, Hedrick JH, Kurichi JE, Minogue AC, et al. An acute care surgery model improves outcomes in patients with appendicitis. Ann Surg. 2006;244:498–504. doi: 10.1097/01.sla.0000237756.86181.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sandstrom A, Grieve DA. Hyperbilirubinaemia: its utility in non-perforated appendicitis. ANZ J Surg. 2015 Nov 17; doi: 10.1111/ans.13373. [Epub] [DOI] [PubMed] [Google Scholar]
- 21.Foley TA, Earnest F, 4th, Nathan MA, Hough DM, Schiller HJ, Hoskin TL. Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology. 2005;235:89–96. doi: 10.1148/radiol.2351040310. [DOI] [PubMed] [Google Scholar]
- 22.Maroju NK, Robinson Smile S, Sistla SC, Narasimhan R, Sahai A. Delay in surgery for acute appendicitis. ANZ J Surg. 2004;74:773–776. doi: 10.1111/j.1445-1433.2004.02785.x. [DOI] [PubMed] [Google Scholar]
- 23.Liang MK, Andersson RE, Jaffe BM, Berger DH. The appendix. In: Brunicardi FC, Andersen DK, Billiar TR, Dunn DL, Hunter JG, Matthews JB, et al., editors. Schwartz's principles of surgery. 10th ed. New York: McGraw-Hill Education; 2014. pp. 1243–1244. [Google Scholar]


