Abstract
The increasing availability of electronic health care records has provided remarkable progress in the field of population health. In particular the identification of disease risk factors has flourished under the surge of available data. Researchers can now access patient data across a broad range of demographics and geographic locations. Utilizing this Big healthcare data researchers have been able to empirically identify specific high-risk conditions found within differing populations. However to date the majority of studies approached the issue from the top down, focusing on the prevalence of specific diseases within a population. Through our work we demonstrate the power of addressing this issue bottom-up by identifying specifically which diseases are higher-risk for a specific population. In this work we demonstrate that network-based analysis can present a foundation to identify pairs of diagnoses that differentiate across population segments. We provide a case study highlighting differences between high and low income individuals in the United States. This work is particularly valuable when addressing population health management within resource-constrained environments such as community health programs where it can be used to provide insight and resource planning into targeted care for the population served.
Today we are witnessing a shift in the landscape of modern healthcare. The rapid emergence and adoption of Electronic Medical Records (EMR) has led to a sundry of analytic technologies. These technologies utilize aggregated EMR’s from numerous individuals in conjunction with machine learning and statistical techniques to provide personalized diagnoses based on a patient’s specific health conditions, clinical decision support systems, and numerous other tools employing secondary uses of EMR data1,2,3,4,5.
While these methods and technologies have provided advancements to both diagnostic accuracy and patient safety, the research thus far has been limited in leveraging data-driven methods to understand population level health dynamics. The EMR data, indeed, provides an exciting opportunity to gain a more complete and holistic understanding of a population segment. This not only offers an understanding of the risks faced by the population at large, but also offer insights into more effective resource management and application.
Traditionally, those studies that do attempt to address the issue at a population level have done so with respect to specific diseases such as diabetes, cardiovascular disease and mental disorders6,7,8. Further these population studies often evaluate attributes outside of an individual’s direct control, such as age, gender, and ethnicity. However, prior population health works have shown these attributes account for only a small portion of an individual’s overall health condition. In fact, the set of factors contributing most notably to an individual’s health have been linked to their socioeconomic “circle,” or as stated by Dahlgren and Whitehead, the set of material and social conditions in which people live and work9.
One factor that has drawn a great deal of attention from population health researchers, is that of income. Two fundamental studies related to population income disparity were performed by Adler and Marmont respectively10,11. In their work Marmot et al. go so far as to claim that “all modern analysis must now ‘control for’ social class as they do for sex”. Since the publication of these works, there have been a number of additional studies investigating the relation of income to health more closely12,13,14. While these studies have provided a detailed evaluation into how socioeconomics can influence a population’s health, they fail to address the major factor of identifying specifically which diseases the population is at risk for.
The methodology presented in this work addresses this exact deficiency, helping to answer the question: what are the distribution of diseases, including comorbidities, of varying subgroups within a population? An understanding of a population’s high-risk diagnoses has been shown to offer substantial benefits at both an administrative and community level. From an administrative perspective, population health can have a direct impact on public policy. A study by Tarlov proposed four frameworks that must be used in conjunction to provide guidance for constructing effective public policy, one of which is constructed from the “determinants of population health”15. Building on ideas similar to Dahlgren, Tarlov believes social/societal factors account for more than half of all influences on a population’s health. He adds to the importance of this understanding by posing that population interventions are unlikely to be successful without social/societal change.
On the community side, diagnosis specific inference can provide a direct impact on individual care. Community healthcare operations often struggle with restricted healthcare budgets or limited resource access, and as a result the allocation of their current resources has become increasingly important. An early study by Birch et al. detailed a need-based healthcare resource allocation system, which like many early works focused on population attributes such as age and sex16. With their work Birch et al. demonstrated that external data could be utilized to improve healthcare allocation, and offered that the next challenge was to “construct indicators of relative need” for a population. Building from this, we believe the ability to identify a population’s specific high-risk diagnoses could provide more effective resource allocation and treatment plans.
Although the quantity and quality of healthcare data is increasing, the analysis needed to obtain the diagnosis specific insights still present some challenges. Just as the complexities of human physiology and the unique nature of individual’s medical history have provided difficulties in the field of personalized medicine, the wide range of ethnicities, genders and ages between individuals offers a similar obstacle to the field of population healthcare. Variations such as these become particularly evident as we analyze populations stratified on attributes such as income, which fall on the outer edge of an individual’s socioeconomic circle.
In an attempt to address these complexities many studies have drawn on the field of network science. One of the first approaches, a study by Hidalgo et al., constructed networks based on disease comorbidities17. In these early works Hidalgo et al. and others demonstrated how diagnosis networks could be used to quantitatively study the properties of comorbid diseases18,19,20,21. Over the past decade network-based techniques have continued to evolve, with applications ranging from the identification of cancer-specific disease comorbidities, to the utilization of diagnostic data to identify the skeletal components that contribute to pathological disequilibrium in dental patients22,23,24,25.
Beyond the macro-level physical interactions found in diagnosis networks, extensive work has also been performed on utilizing networks to model the complex interactions that occur on a molecular-level26,27,28,29. Further, in addition to their diagnostic applications, exciting new work has emerged with a focus on utilizing networks to model human physiology. These networks aim to inform our knowledge of the interdependency among several organs systems, and their function within the complex biological systems of the human body30,31,32.
It has become increasingly clear that population health management can no longer operate under a one-size-fits-all paradigm. In this work we leverage the network based framework, which allows for the analysis of the deviations in comorbidities and specific diagnoses between population subgroups. We introduce a network-focused metric termed fold-change. The fold-change provides a normalized metric of the over-representation for diagnosis comorbidity pairs between two generalized population subgroups. Through the analyses presented we will establish not only the utility of the fold-change metric in identifying high-risk diagnoses targeted for specific population subgroups, but also demonstrate how partitioning the network using the fold-change metric as edge weights can help to uncover new and interesting diagnosis patterns not discernible through naive partitioning techniques. We provide a case study of patients from high and low income populations, based on median household income, within the United States. Additionally, we provide an extended analysis detailing the effects of further stratification based on insurance of the patient, discovering potentially cost saving disease hubs that could be used to guide the preventive actions of healthcare organizations and policy makers.
Results
The evaluation of the network-based technique proposed in this work was broken down into two distinct analysis, each of which investigated a different aspect of the diagnosis variations between the population subgroups. These subgroups represent individuals in the highest and lowest quartiles of median income across the United States. A summary of each analysis and the corresponding results can be found in the respective sections below.
The foundation for each of the following analyses was the creation of a diagnosis network to help standardize a disease intearaction representation as also done in the related works. As such, prior to detailing the analysis results we offer a brief overview of the experimental framework, providing context around the specific attributes of the networks utilized throughout the work.
Network Construction
In the simplest form a network is a relational data representation. This representation is comprised of a set of entities, known as nodes, and connections between pairs of nodes, known as edges. Within the context of the diagnosis networks used in this work, each node represents a unique diagnosis code (provided in the ICD9-CM international standard), and co-morbid diagnoses share an edge. Diagnoses are comorbid if they co-occur in a patient.
Additionally, the edges of the network were assigned a weight corresponding to the frequency at which the diagnosis nodes occurred comorbidly across all patients of the particular subgroup. It should be noted the edge weights of each diagnosis pair were normalized, the complete formalization of this process can be found in the Study Data and Methods section.
Comorbidity Analysis
Our first analysis focused on the identification of over-represented network edges (comorbid diagnoses) for a particular population subgroup. The over-representation of a specific edge was quantified by a normalized ratio of the corresponding edge weights in each of the two subgroup networks, a quantity henceforth referred to as “fold change”. A detailed discussion of the fold change metric can be found in the Study Data and Methods section.
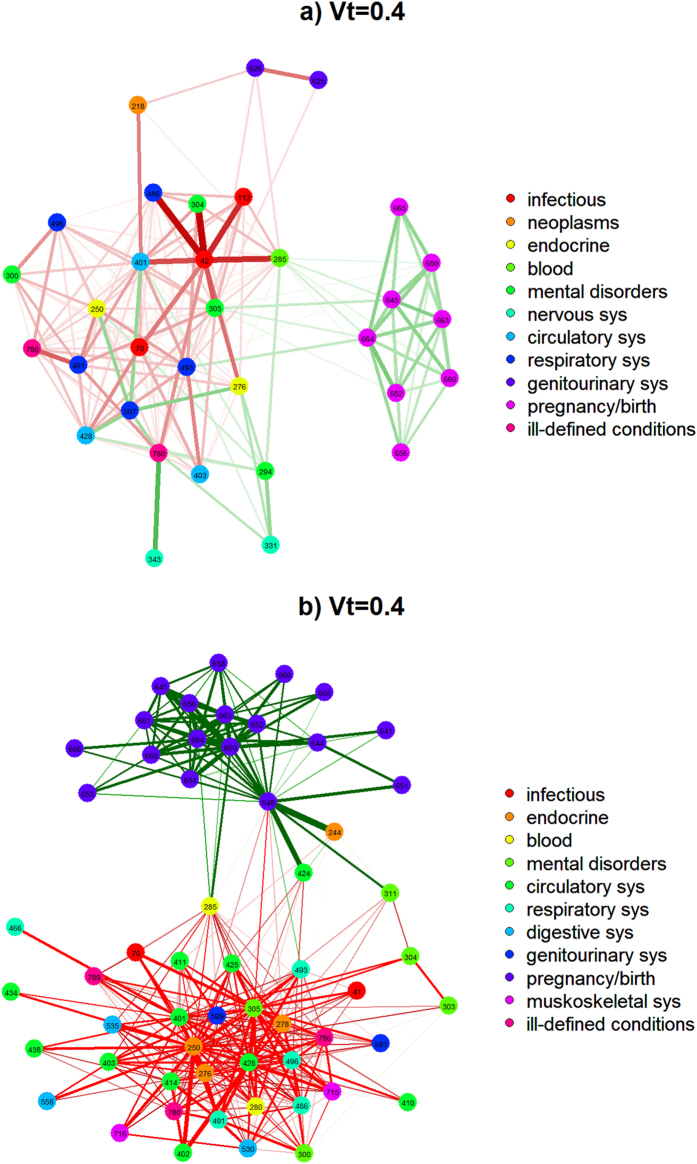
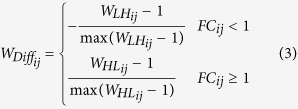
Figure 1a presents a single-network representation of the diagnosis fold-change between the low and high income populations. The numbers within each node represent the respective ICD9-CM diagnosis code, and the edge coloring conveys whether the comorbid diagnoses were over-represented in the high or low income subgroup. Edges where the fold-change ratio was greater than 1 for the high income subgroup were colored green, and those where fold-change ratio was greater than 1 for the low income subgroup were colored red. For clarity a fold-change value over 1 represents the case where the edge weight, representing the normalized comorbidity frequency between two diagnoses, is greater in a particular subgroup.
Figure 1. Presents a visualization detailing the diagnosis fold-change between the low and high income populations in a single network representation.
(a) Complete Network Visualization comparing low income and high income populations. (b) Network Visualization without pregnancy/birth related diagnoses.
One benefit of the network visualization seen in Fig. 1a stems from the ability to quickly identify specific groupings of diagnoses. The figure was generated using what is known as a force-directed layout, where nodes are positioned in an effort to separate groups of adjacent (connected) nodes in a visually interpretable manner. As a result the prevalence of complications for pregnancy and childbirth in a group of high income female patients could be seen with relative ease. To account this an additional visualization is provided in Fig. 1b, which excludes pregnancy/birth related diagnoses, allowing a far more detailed view of the network composition.
A review of the low income population’s over-represented edges revealed a high prevalence of mental disorders (schizophrenia), chronic diseases (obesity, diabetes) and drug related abuse and dependence. Conversely over-represented edges within the high income population were comprised almost entirely of pregnancy related conditions, ranging from labor conditions to delivery trauma. Conditions including obstructed labor represent a risk to the mother while others such as umbilical cord complications, and malposition indicate risk to the fetus.
For reference we have provided the top 10 diagnosis code pairs ranked by highest fold-change in Tables 1 and 2 for the low and high populations respectively. It is important to note that all edges listed in the top 10, as well as all edges shown in Fig. 1, are significantly over-represented at p < 0.001.
Table 1. Ranked list of edges where Low Income (LI) population is over-represented in comparison to High Income (HI) population.
| Rank | Edge Pair | Count |
Normalized |
Fold-change | ||
|---|---|---|---|---|---|---|
| HI | LI | HI | LI | |||
| 1 | 295 - Schizophrenic disorders | 26,603 | 110,521 | 0.00285 | 0.00894 | 3.135 |
| 305 - Nondependent abuse of drugs | ||||||
| 2 | 295 - Schizophrenic disorders | 20,198 | 74,082 | 0.00216 | 0.00599 | 2.768 |
| 250 - Diabetes mellitus | ||||||
| 3 | 401 - Essential hypertension | 31,180 | 113,647 | 0.00334 | 0.00919 | 2.750 |
| 295 - Schizophrenic disorders | ||||||
| 4 | 070 - Viral hepatitis | 30,753 | 108,271 | 0.0033 | 0.00875 | 2.657 |
| 305 - Nondependent abuse of drugs | ||||||
| 5 | 403 - Hypertensive chronic kidney disease | 23,494 | 81,366 | 0.00252 | 0.00658 | 2.613 |
| 305 - Nondependent abuse of drugs | ||||||
| 6 | 304 - Drug dependence | 9,669 | 33,232 | 0.00104 | 0.00269 | 2.593 |
| 493 - Asthma | ||||||
| 7 | 345 - Epilepsy and recurrent seizures | 11,249 | 37,667 | 0.00121 | 0.00305 | 2.527 |
| 305 - Nondependent abuse of drugs | ||||||
| 8 | 585 - Chronic kidney disease (CKD) | 22,892 | 75,822 | 0.00245 | 0.00613 | 2.499 |
| 305 - Nondependent abuse of drugs | ||||||
| 9 | 278 - Overweight, obesity and other hyperalimentation | 9,576 | 31,602 | 0.00103 | 0.00256 | 2.490 |
| 295 - Schizophrenic disorders | ||||||
| 10 | 648 - Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium | 17,608 | 57,798 | 0.00189 | 0.00467 | 2.477 |
| 305 - Nondependent abuse of drugs | ||||||
Table 2. Ranked list of edges where High Income (HI) population is over-represented in comparison to Low Income (LI) population.
| Rank | Edge Pair | Count |
Normalized |
Fold-change | ||
|---|---|---|---|---|---|---|
| HI | LI | HI | LI | |||
| 1 | 244 - Acquired hypothyroidism | 36,054 | 15,020 | 0.00386 | 0.00121 | 3.181 |
| 648 - Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium | ||||||
| 2 | 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | 139,723 | 63,894 | 0.01497 | 0.00517 | 2.898 |
| 664 - Trauma to perineum and vulva during delivery | ||||||
| 3 | 654 - Abnormality of organs and soft tissues of pelvis | 86,596 | 47,674 | 0.00928 | 0.00385 | 2.407 |
| 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | ||||||
| 4 | 652 - Malposition and malpresentation of fetus | 39,193 | 21,995 | 0.0042 | 0.00178 | 2.361 |
| 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | ||||||
| 5 | 663 - Umbilical cord complications | 113,957 | 66,694 | 0.01221 | 0.00539 | 2.264 |
| 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | ||||||
| 6 | 663 - Umbilical cord complications | 134,474 | 80,865 | 0.01441 | 0.00654 | 2.204 |
| 664 - Trauma to perineum and vulva during delivery | ||||||
| 7 | 660 - Obstructed labor | 27,094 | 16,627 | 0.0029 | 0.00134 | 2.160 |
| 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | ||||||
| 8 | 645 - Late pregnancy | 57,453 | 37,220 | 0.00616 | 0.00301 | 2.046 |
| 659 - Other indications for care or intervention related to labor and delivery, not elsewhere classified | ||||||
| 9 | 656 - Other known or suspected fetal and placental problems affecting management of mother | 40,455 | 26,209 | 0.00433 | 0.00212 | 2.046 |
| 664 - Trauma to perineum and vulva during delivery | ||||||
| 10 | 661 - Abnormality of forces of labor | 27,986 | 18,203 | 0.003 | 0.00147 | 2.038 |
| 664 - Trauma to perineum and vulva during delivery | ||||||
Diagnosis Analysis
Next we extend the comorbidity results to investigate the specific diagnosis nodes which comprise the over-represented edges of each subgroup.
Focusing on the low income population’s top 10 over-represented edge pairs (Table 1) we find multiple occurrences of nodes that constitute drug abuse or dependence. Analyzing the top 10 over-represented edge pairs for the high income population (Table 2) reveals multiple occurrences of edges containing the specific ICD9-CM code 664: Trauma to perineum and vulva during delivery. Trauma code 664 contained edges to a number of conditions which included known or suspected fetal and placental problems, abnormality of forces of labor, and umbilical cord complications.
Network Metric Analyses
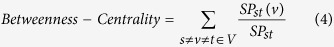
Thus far, the analyses presented in this work have demonstrated the utility of the proposed fold-change metric. These analyses have highlighted how fold-change rankings can be utilized to identify significantly over-represented diagnoses, which can be beneficial in differentiating the health concerns of various population subgroups. However, with our final analysis we take the fold-change metric one step further, demonstrating that combined with a standard network analysis (betweenness-centrality), it can be used to discern core-differences between the population groups. These differences are not immediately evident on the network not weighted by fold-change metric. Betweenness-centrality is a network metric which provides a normalized measure of the global importance of a node in communicating between pairs of nodes in the network, considering the shortest paths33.
Utilizing the methodology detailed in the Network Construction section prior, two networks were constructed representing the high and low income populations. These networks were created utilizing a naive partitioning, in which the over-represented comorbidity pairs of patients in the high income population were added as edges to one network, while the over-represented comorbidity pairs of the low income population were added as edges to the other. The standard metric of betweenness-centrality was calculated on each network independently, and the top 10 diagnosis nodes ranked in decreasing order by betweenness-centrality are presented within Table 3. As can be seen from the results, there are a number of high-ranking diagnoses which coincide with the over-represented diagnoses identified by the fold-change rankings. For the high income population these included pregnancy related conditions such as Other current conditions in the mother classified elsewhere, while Nondependent abuse of drugs and a number of chronic conditions receive high centrality scores within the low income population.
Table 3. Betweenness-Centrality Rankings on unmodified High and Low income population networks.
| Rank | Low Income Population |
High Income Population |
||||
|---|---|---|---|---|---|---|
| ICD Code | Betweenness Centrality | Diagnosis Name | ICD Code | Betweenness Centrality | Diagnosis Name | |
| 1 | 250 | 0.300 | Diabetes mellitus | 401 | 0.295 | Essential hypertension |
| 2 | 401 | 0.210 | Essential hypertension | 427 | 0.162 | Cardiac dysrhythmias |
| 3 | 305 | 0.102 | Nondependent abuse of drugs | 272 | 0.128 | Disorders of lipoid metabolism |
| 4 | 276 | 0.070 | Disorders of fluid, electrolyte, and acid-base | 285 | 0.121 | Other and unspecified anemias |
| 5 | 496 | 0.047 | Chronic airway obstruction not elsewhere classified | 244 | 0.094 | Acquired hypothyroidism |
| 6 | 285 | 0.041 | Other and unspecified anemias | 648 | 0.081 | Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium |
| 7 | 428 | 0.038 | Heart failure | 276 | 0.080 | Disorders of fluid electrolyte, and acid-base balance |
| 8 | 278 | 0.028 | Overweight, obesity and other hyperalimentatio | 311 | 0.057 | Depressive disorder not elsewhere classified |
| 9 | 414 | 0.026 | Other forms of chronic ischemic heart disease | 424 | 0.028 | Other diseases of endocardium |
| 10 | 599 | 0.020 | Other disorders of urethra and urinary tract | 733 | 0.026 | Other disorders of bone and cartilage |
Looking to Tables 4 and 5, we again provide rankings of betweenness-centrality calculated on both the low and high income population networks. However, in this case, each network underwent a range of pruning thresholds, at which all edges with a fold-change below the specified threshold value were removed. A complete overview of the process can be found in the Methods section. As a note, the high income population (Table 5) threshold at 2.0 has only two non-zero centrality scores after pruning, the remaining three spots are intentionally blank. It is overtly evident that the threshold value has a profound impact on the network structure, as the betweenness-centrality rankings undergo significant reordering across the range of thresholds. This can be seen in the high income population where diagnosis such as diabetes mellitus drops from Rank 1 to 5, while schizophrenic disorders, which was previously ranked outside the top-5, rises to rank 2. This phenomena is mirrored in the low income population where diagnoses such as hypertension and cardiac dysrhythmias were initially ranked 1 and 2, quickly fall outside the top 5, and are replaced by pregnancy related conditions such as trauma to perineum and vulva during delivery at higher threshold values. A deeper discussion as to the implications of these changes can be found in the Discussion section.
Table 4. Thresholded Betweenness-Centrality Rankings - Low Income Population.
| Rank | ICD Code | Betweenness Centrality | Diagnosis Name | ICD Code | Betweenness Centrality | Diagnosis Name |
|---|---|---|---|---|---|---|
| Threshold - 1.25 | Threshold - 1.50 | |||||
| 1 | 305 | 0.218 | Nondependent abuse of drugs | 305 | 0.200 | Nondependent abuse of drugs |
| 2 | 250 | 0.179 | Diabetes mellitus | 250 | 0.045 | Diabetes mellitus |
| 3 | 401 | 0.036 | Essential hypertension | 491 | 0.012 | Chronic bronchitis |
| 4 | 496 | 0.034 | Chronic airway obstruction | 401 | 0.012 | Essential hypertension |
| 5 | 571 | 0.025 | Chronic liver disease and cirrhosis | 295 | 0.012 | Schizophrenic disorders |
| Threshold - 1.75 | Threshold - 2.0 | |||||
| 1 | 305 | 0.070 | Nondependent abuse of drugs | 305 | 0.020 | Nondependent abuse of drugs |
| 2 | 250 | 0.012 | Diabetes mellitus | 295 | 0.007 | Schizophrenic disorders |
| 3 | 70 | 0.010 | Viral hepatitis | 491 | 0.005 | Chronic bronchitis |
| 4 | 491 | 0.008 | Chronic bronchitis | 70 | 0.004 | Viral hepatitis |
| 5 | 295 | 0.006 | Schizophrenic disorders | 250 | 0.001 | Diabetes mellitus |
Table 5. Thresholded Betweenness-Centrality Rankings - High Income Population.
| Rank | ICD Code | Betweenness Centrality | Diagnosis Name | ICD Code | Betweenness Centrality | Diagnosis Name |
|---|---|---|---|---|---|---|
| Threshold - 1.25 | Threshold - 1.50 | |||||
| 1 | 427 | 0.068 | Cardiac dysrhythmias | 244 | 0.027 | Acquired hypothyroidism |
| 2 | 244 | 0.065 | Acquired hypothyroidism | 648 | 0.022 | Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium |
| 3 | 424 | 0.060 | Other diseases of endocardium | 424 | 0.019 | Other diseases of endocardium |
| 4 | 272 | 0.055 | Disorders of lipoid metabolism | 427 | 0.017 | Cardiac dysrhythmias |
| Threshold - 1.75 | Threshold - 2.0 | |||||
| 5 | 648 | 0.047 | Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium | 272 | 0.014 | Disorders of lipoid metabolism |
| 1 | 664 | 0.001 | Trauma to perineum and vulva during delivery | 659 | 0.001 | Other indications for care or intervention related to labor and delivery not elsewhere classified |
| 2 | 659 | 0.001 | Other indications for care or intervention related to labor and delivery not elsewhere classified | 664 | 0.0006 | Trauma to perineum and vulva during delivery |
| 3 | 648 | 0.0005 | Other current conditions in the mother classifiable elsewhere but complicating pregnancy, childbirth, or the puerperium | |||
| 4 | 663 | 0.0001 | Umbilical cord complications | |||
| 5 | 645 | 0.00001 | Late pregnancy | |||
Finally, in an effort to compare the observations from our fold-change ranking, with those detected using network structure alone, we performed community detection on the complete high and low income population networks. The results of these analyses can be found in the supplementary material.
Discussion
A review of the relevant literature reveals strong support for the observations derived from the income-stratified networks above. Beginning with the low income population, prior work has linked individuals’ with lower socioeconomic status to a higher prevalence of chronic disease such as diabetes and obesity34,35,36. A study by Bassuk et al., which focused on the “Prevalence of Mental Health and Substance Use Disorders Among Homeless and Low-Income Housed Mothers”, found a significant increase in the rate of both mental health and substance use disorders amongst the low-income population when compared the general population. Additionally, the study highlighted an increased prevalence of the mental disorder schizophrenia amongst homeless solitary women37.
Likewise we find support in the literature for the over-represented diagnoses of the high income population. As noted prior, pregnancy related conditions constituted almost the entirely of the high income populations over-represented conditions. We conjecture the preponderance of pregnancy related conditions may be attributed to increased access to prenatal care, as many of the identified conditions were likely diagnosed during an expectant mothers prenatal visits over the course her pregnancy. It is well established that due to the cost of these visits, and limited access to resources, lower socioeconomic populations often times fail to receive prenatal care at the appropriate times, if at all38.
In a similar fashion we find that a survey of diagnosis nodes corresponding to these over-represented edges can be supported by medical literature. The low income population’s prevalence of drug abuse or dependence nodes are connected to well documented comorbid conditions such as hepatitis and recurrent seizures39,40,41. Additionally a closer investigation of the diagnosis pairs yields another less apparent condition, kidney disease. Recent work has begun linking the long established toxic effects of drug use and abuse to the development of chronic kidney disease, fostering additional support for the power of our network-based technique to identify clinically useful comorbidities within a population subgroup42,43,44. For the high income population we evaluated conditions that occurred comorbidly with the diagnosis Trauma to perineum and vulva during delivery (ICD9-CM code 664), which appeared multiple times in the set of over-represented edges. Investigation revealed that women who experience the pregnancy complications comorbid to code 664 have a significantly higher probability of their child being delivered with the aid of forceps45. This is particularly noteworthy as prior work has associated delivery with forceps with a 10-fold increased risk of perineal injury46. These findings again highlight the power of our network technique to identify high-risk diagnoses for a population subgroup, in this case representing high income pregnant women.
Moving to the network-focused analyses, as the overarching goal of this work was to provide a technique through which differentiating and representative diagnoses between two population sub-groups could be identified, the measure of betweenness-centrality is an excellent evaluation lens. In the context of co-morbidity network structures betweenness-centrality can be viewed as a measure of a diagnosis’s connectivity, i.e. the number of edge pairs which contain the diagnosis. Looking back over the betweenness-centrality results, one of the principle observations can be found in the stark difference between the centrality rankings on the unmodified and pruned networks for each population subgroup.
This differentiation is critically important as it demonstrates the utility of the fold-change metric in uncovering the core differences between population subgroups. By punning the network using the fold-change metric, we are able to remove peripheral edges for comorbidity pairs that have only a slight over-representation in either population. Recalculating the betweenness-centrality on these pruned networks offers us the opportunity to identify key nodes of a network representing highly polarizing comorbidities between the population subgroups.
Breaking down the results we can find explicit examples of where the identification of specific diagnoses would not have been apparent though analysis of the networks alone, but required the introduction of the fold-change metic into the analysis pipeline. For the high income population we see a ranking of 1, 2 and 3 for diabetes mellitus, essential hypertension and nondependent abuse of drugs respectively on the unmodified network. As noted prior these are certainly conditions which are to expected to be over-represented in a lower income population. However, these are also extremely prevalent diagnoses, particularly hypertension which can occur comorbidly with a multitude of diagnoses. Increasing the threshold value to 2, provides a number of interesting changes. First, prevalent diagnoses such as diabetes mellitus and essential hypertension fall in the rankings, indicating that the majority of their connections were only weakly over-represented between the two subgroups. While diagnoses such as nondependent abuse of drugs and schizophrenic disorders claim the top 2 spots. While less prevalent these diagnosis have a much stronger over-representation between the population subgroups, potentially helping to highlight avenues of care or resource distribution.
We find similar patterns upon analysis of the high income population’s results. While the unpruned network presents various cardiac conditions such as essential hypertension, dysrhythmias and unspecified anemias. Increasing the threshold highlights previously discussed pregnancy related conditions. At 1.5 we find current conditions in the mother classified elsewhere, and 2.0 presents trauma to perineum and vulva during delivery.
For completeness we ran two standard community detection algorithms WalkTrap and label-propagation. These analyses can aid in an understanding of how the underlying network structure may effect network metrics such as centrality measures, as it will help provide insights into the connectivity between various comorbidity patterns. As can be seen from the results (found in the supplementary material), community detection on the partitioned subgroup networks offers little insight into the populations diagnoses distribution. The majority of diagnoses are grouped into a single community, with only a select few placed into meaningful communities. Although this subset of communities may appear to highlight some similar occurrence patterns to the fold-change rankings, such as pregnancy related conditions, these occurrences are in fact an artifact of the highly interconnected subgraph of co-occurring diagnoses during pregnancy. It is clear that standard community detection alone fails to provide the ability to identify specific differentiations between population sub-groups, again highlighting the utility of the incorporating the fold-change metric into the analysis pipeline.
Through this work we have demonstrated and validated that the proposed network technique provides a clear differentiation in frequent diagnosis between population subgroups, in particular individuals in the upper and lower quartiles of income within the United States adult population. While this case study was focused on the identification of specific population health conditions based on varying socioeconomic levels, the network approach used for this identification can be easily extended to a multitude of population subgroups and external factors. As an example a similar analysis is provided in the supplementary material with patients further stratified by various insurance providers. It is important to note the scale of the data and observations discussed. Both the data used for this analysis as well as many of the cited works were collected at the national level. This was done intentionally in an effort to validate the observations and results of our technique against established medical literature acting as a ground truth. While national data is imperative for effective analysis of the general population, we believe this technique can be applied at the community level to start making differences, for example, to Accountable Care Organizations grappling for answers around resource allocation and budgeting. Our methodology may aid in identifying potentially unique comorbidities within a specific subgroup or population, allowing physicians and nurses to provide more accurate and targeted care for individuals they see on a daily basis as well as direct potential resources and information.
Finally, it is clear that this work is only a stepping stone to greater population heath management. For this type of analytics to truly take hold we will need the collaboration of data scientists, medical professionals and policy makers alike to produce, analyze and act on the insights gained through tools such as this. Looking forward as personalized treatment options have been key to improving the quality of patient care, a deeper understanding of the population health conditions will be critical for improving treatment options and resource management for a population.
Study Data and Methods
Data
For the analyses performed in this work we utilized the Nationwide Inpatient Sample (NIS) provided by the Healthcare Cost and Utilization Project (HCUP)47. At the time of this publication the NIS is the largest publicly available all-payer inpatient health care database in the United States. The NIS contains hospital discharge records for a stratified sample of patients from approximately 20% of United States hospitals, representing 44 different states (at the time of this publication) and has been cited in over two thousand different peer-reviewed journal articles.
Each record contains both the personal characteristics of the patient, including their age, gender, and race, and administrative information including their length of stay, and discharge status. Additionally, the NIS provides diagnostic information, including up to 15 (2003–2008 datasets) or 25 (2009) diagnoses, surgical and nonsurgical procedures. Diagnoses were coded using The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)48. The ICD-9-CM coding methodology uses a taxonomy of five-digit codes, where the first three digits represent the general diagnosis and the remaining two digits can be used as modifiers describing factors such as location or severity. For this work we “collapsed” the codes, using only the first three digit general diagnosis. This allows us to both prevent similar diagnoses from being represented as multiple edges within the network, as well improve the overall interpretability of the results.
To construct the diagnosis networks used in our analyses we utilized a total of 21,662,600 patient hospitalization records representing the set of 9,306,956 high income and 12,355,644 low income records; the details of this partitioning from the HCUP data can be found in the Methods section below. These networks represent the co-occurrences of 934 unique ICD9-CM diagnosis codes between patients in the low and high income populations. Additionally it should be noted that for this analysis we considered records from only those patients with an age over 20 to exclude child related diagnoses and focus on the adult population.
Methods
Before detailing the methodology used in the network construction and analysis it is important to detail the population being evaluated. As stated earlier this case study focuses on the comparison of low and high income individuals. The NIS income data is based on the median household income for a patient’s specific zip code. Under this definition an income level of 1 represents a reported income in the lowest quartile, while a 4 represents the highest median quartile at the individual’s respective location. The low income population subgroup was determined as the set of all patient records in the lowest median income quartile (1), while the high income population subgroup represents those in highest median income quartile (4).
To build the diagnosis networks, first we extracted the unique set of ICD9-CM comorbid diagnosis codes between patients in the low and high income populations. To account for the difference in population size the network edge weights were normalized using Equation 1. Here N represents the total number of records in a population (low or high income), while Cij represents the number of co-occurrences of diagnosis i and j within the patients of each population respectively.
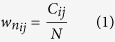 |
Next the ratios between  and
and  were computed to identify those diagnoses which occur in greater proportion amongst each of the populations. We define the ratio of diagnoses i and j between the two population subgroups as the fold-change (Equation 2). For clarity, the edge analysis performed in this work focuses on differences in diagnoses occurrence between each population, rather than the population on the whole. This is done in an effort to demonstrate the potential benefit of utilizing population level health records for specific community analysis. It should be noted that all normalized edge weights below the threshold 0.0001 were set to 0 to prevent high fold-change ratios from an extremely rare diagnosis.
were computed to identify those diagnoses which occur in greater proportion amongst each of the populations. We define the ratio of diagnoses i and j between the two population subgroups as the fold-change (Equation 2). For clarity, the edge analysis performed in this work focuses on differences in diagnoses occurrence between each population, rather than the population on the whole. This is done in an effort to demonstrate the potential benefit of utilizing population level health records for specific community analysis. It should be noted that all normalized edge weights below the threshold 0.0001 were set to 0 to prevent high fold-change ratios from an extremely rare diagnosis.
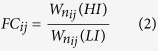 |
To aid in interpretation of the differences in the observed networks, the edge weights were normalized further to fall within the interval [−1, 1] using the transformation found in Equation 3. WHL represents the edge weight calculated as a quotient of the high income population’s edge weight by the low income population’s respective edge weight and WLH represents the opposite quotient. Finally, due to the density of the network to avoid over-saturation of nodes and edges and allow for an optimal visualization we introduce a visualization threshold Vt. The threshold displays only those edges where Vt < abs(WDiff). It should be noted that while the threshold Vt was set experimentally to reduce the number of edges and related nodes with low weights for the visualizations provided, the analyses in this work were performed on the complete network.
 |
In order to determine statistical significance of the fold change results we performed permutation tests using the Fisher-Yeats shuffle algorithm49. For each diagnosis code pair we performed a 10,000 iteration shuffle. At each iteration we randomly shuffled the high and low income level labels at each occurrence and calculated the resulting fold-change. The resulting 10,000 fold-changes are averaged and compared to the true fold-change to obtain a Z-score evaluated at 95% significance level.
For our final set of analysis we perform a set of network analyses, including betweenness-centrality and community detection. Betweenness-centrality is a network metric, which on per node basis provides the proportion of shortest-paths through the network which pass through each node50. The mathematical definition is provided in Equation 4, where SPst is the total number of shortest paths from node s to node t and SPst(v) is the number of those paths that pass through v.
 |
We began the betweenness-centrality analysis by computing node rankings on the complete network for both populations independently. The networks are undirected, but have edge weights corresponding to the fold-change metric detailed prior. For the pruning analysis the complete network was created for each population, and all edges below the specified fold-change threshold were removed. The betweenness-centrality was calculated at every step from 1–2 at intervals of 0.25.
It should be noted that all fold-change values are above 1. As noted fold-change is a normalized metric, indicating the level of over-representation of specific diagnosis co-occurance pattern between the population subgroups. As such, under represented comorbidities in one network (fold-change values less than 1) are presented in the second network where the reciprocal fold-change is utilized.
For our community detection we chose two widely utilized algorithms in Walktrap and label-propagation, both run with default parameters51,52. These algorithms represent two distinctly different approaches to discovering communities from the underlying network structure in an unsupervised manner, and thus can offer a fairly comprehensive overview of the types of diagnosis communities within each population subgroup. While Walktrap attempts to find densely connected subgraphs, via random walks, label propagation utilizes a majority voting technique where at each iteration a diagnosis node adopts the label that most of its neighbors currently have.
Additional Information
How to cite this article: Feldman, K. et al. Insights into Population Health Management Through Disease Diagnoses Networks. Sci. Rep. 6, 30465; doi: 10.1038/srep30465 (2016).
Supplementary Material
Acknowledgments
We thank Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality provided data used in this study. This study was partially supported by the Swiss National Science Foundation through a SCOPES 2013 Joint Research Projects grant SNSF IZ73Z0-152415, NSF IIS 144795, by DARPA Grants FA9550-12-1-0405 and FA9550-12-1-0406 negotiated by AFOSR.
Footnotes
Author Contributions N.V.C., G.S., K.F., M.K. and Z.O. designed the study. G.S. and Z.O. provided the data. K.F., G.S., D.G. and N.V.C. performed analysis. N.V.C., K.F., G.S., D.G., M.K. and Z.O. wrote and reviewed the manuscript. All authors approve the manuscript for publication.
References
- Yoo I. et al. Data mining in healthcare and biomedicine: a survey of the literature. Journal of medical systems 36, 2431–2448 (2012). [DOI] [PubMed] [Google Scholar]
- Jensen P. B., Jensen L. J. & Brunak S. Mining electronic health records: towards better research applications and clinical care. Nature Reviews Genetics 13, 395–405 (2012). [DOI] [PubMed] [Google Scholar]
- Davis D. A., Chawla N. V., Christakis N. A. & Barabási A.-L. Time to care: a collaborative engine for practical disease prediction. Data Mining and Knowledge Discovery 20, 388–415 (2010). [Google Scholar]
- McCormick T. H., Rudin C., Madigan D. et al. Bayesian hierarchical rule modeling for predicting medical conditions. The Annals of Applied Statistics 6, 652–668 (2012). [Google Scholar]
- Bryan C. & Boren S. A. The use and effectiveness of electronic clinical decision support tools in the ambulatory/primary care setting: a systematic review of the literature. Informatics in primary care 16, 79–91 (2008). [DOI] [PubMed] [Google Scholar]
- Lee J. W. R., Brancati F. L. & Yeh H.-C. Trends in the prevalence of type 2 diabetes in asians versus whites results from the united states national health interview survey, 1997–2008. Diabetes Care 34, 353–357 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M., Austin P. C., Manuel D. G. & Tu J. V. Comparison of cardiovascular risk profiles among ethnic groups using population health surveys between 1996 and 2007. Canadian Medical Association Journal 182, E301–E310 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaesmer H., Riedel-Heller S., Braehler E., Spangenberg L. & Luppa M. Age-and gender-specific prevalence and risk factors for depressive symptoms in the elderly: a population-based study. International Psychogeriatrics 23, 1294–1300 (2011). [DOI] [PubMed] [Google Scholar]
- Dahlgren G. & Whitehead M. Policies and strategies to promote social 9. Equity in Health. Stockholm: Institute for Future Studies (1991). [Google Scholar]
- Adler N. E. & Ostrove J. M. Socioeconomic status and health: what we know and what we don’t. Annals of the New York academy of Sciences 896, 3–15 (1999). [DOI] [PubMed] [Google Scholar]
- Marmot M. G., Kogevinas M. & Elston M. A. Social/economic status and disease. Annual review of public health 8, 111–135 (1987). [DOI] [PubMed] [Google Scholar]
- Lynch J. W., Smith G. D., Kaplan G. A. & House J. S. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. Bmj 320, 1200–1204 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy B. P., Kawachi I., Glass R. & Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the united states: multilevel analysis. Bmj 317, 917–921 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson R. G. & Pickett K. E. Income inequality and population health: a review and explanation of the evidence. Social science & medicine 62, 1768–1784 (2006). [DOI] [PubMed] [Google Scholar]
- Tarlov A. R. Public policy frameworks for improving population health. Annals of the New York Academy of Sciences 896, 281–293 (1999). [DOI] [PubMed] [Google Scholar]
- Birch S. & Chambers S. To each according to need: a community-based approach to allocating health care resources. CMAJ: Canadian Medical Association Journal 149, 607 (1993). [PMC free article] [PubMed] [Google Scholar]
- Hidalgo C. A., Blumm N., Barabási A.-L. & Christakis N. A. A dynamic network approach for the study of human phenotypes. PLoS computational biology 5, e1000353 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhaeuser K. & Chawla N. V. A network-based approach to understanding and predicting diseases. In Social computing and behavioral modeling Chap. 26, 1–8 (Springer, 2009). [Google Scholar]
- Lusis A. J. & Weiss J. N. Cardiovascular networks systems-based approaches to cardiovascular disease. Circulation 121, 157–170 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folino F. & Pizzuti C. Link prediction approaches for disease networks. In Information Technology in Bio-and Medical Informatics Chap. 3, 99–108 (Springer, 2012). [Google Scholar]
- Cramer A. O., Waldorp L. J., van der Maas H. L. & Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences 33, 137–150 (2010). [DOI] [PubMed] [Google Scholar]
- Chen Y. & Xu R. Mining cancer-specific disease comorbidities from a large observational health database. Cancer informatics 37 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scala A. et al. Using networks to understand medical data: the case of class iii malocclusions. PloS one 7, e44521 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auconi P., Caldarelli G., Scala A., Ierardo G. & Polimeni A. A network approach to orthodontic diagnosis. Orthodontics & Craniofacial Research 14, 189–197 (2011). [DOI] [PubMed] [Google Scholar]
- Scala A. et al. Complex networks for data-driven medicine: the case of class iii dentoskeletal disharmony. New Journal of Physics 16, 115017 (2014). [Google Scholar]
- Barabási A.-L., Gulbahce N. & Loscalzo J. Network medicine: a network-based approach to human disease. Nature Reviews Genetics 12, 56–68 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho D.-Y., Kim Y.-A. & Przytycka T. M. Network biology approach to complex diseases. PLoS Comput Biol 8, e1002820 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis D. A. & Chawla N. V. Exploring and exploiting disease interactions from multi-relational gene and phenotype networks. PloS one 6, e22670 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akutekwe A. & Seker H. A hybrid dynamic bayesian network approach for modelling temporal associations of gene expressions for hypertension diagnosis. In Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Annual Conference, 804–807 (IEEE, 2014). [DOI] [PubMed] [Google Scholar]
- Bartsch R. P., Liu K. K., Bashan A. & Ivanov P. C. Network physiology: How organ systems dynamically interact. PloS one 10, e0142143 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov P. C. & Bartsch R. P. Network physiology: mapping interactions between networks of physiologic networks. In Networks of Networks: the last Frontier of Complexity Chap. 10, 203–222 (Springer, 2014). [Google Scholar]
- Bashan A., Bartsch R. P., Kantelhardt J. W., Havlin S. & Ivanov P. C. Network physiology reveals relations between network topology and physiological function. Nature communications 3, 702 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furlong L. I. Human diseases through the lens of network biology. Trends in Genetics 29, 150–159 (2013). [DOI] [PubMed] [Google Scholar]
- Connolly V., Unwin N., Sherriff P., Bilous R. & Kelly W. Diabetes prevalence and socioeconomic status: a population based study showing increased prevalence of type 2 diabetes mellitus in deprived areas. Journal of Epidemiology and Community Health 54, 173–177 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins J. M., Vaccarino V., Zhang H. & Kasl S. V. Socioeconomic status and diagnosed diabetes incidence. Diabetes research and clinical practice 68, 230–236 (2005). [DOI] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiologic reviews 29, 29–48 (2007). [DOI] [PubMed] [Google Scholar]
- Bassuk E. L., Buckner J. C., Perloff J. N. & Bassuk S. S. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. American Journal of Psychiatry 155, 1561–1564 (1998). [DOI] [PubMed] [Google Scholar]
- Sword W. A socio-ecological approach to understanding barriers to prenatal care for women of low income. Journal of Advanced Nursing 29, 1170–1177 (1999). [DOI] [PubMed] [Google Scholar]
- Bell J. et al. Hepatitis c virus in intravenous drug users. The Medical Journal of Australia 153, 274–276 (1990). [DOI] [PubMed] [Google Scholar]
- Thomas D. L. et al. Correlates of hepatitis c virus infections among injection drug users. Medicine 74, 212–220 (1995). [DOI] [PubMed] [Google Scholar]
- Alldredge B. K., Lowenstein D. H. & Simon R. P. Seizures associated with recreational drug abuse. Neurology 39, 1037–1037 (1989). [DOI] [PubMed] [Google Scholar]
- Miller P. Principles of Addiction: Comprehensive Addictive Behaviors and Disorders. v. 1. (2013).
- Pendergraft W. F., Herlitz L. C., Thornley-Brown D., Rosner M. & Niles J. L. Nephrotoxic effects of common and emerging drugs of abuse. Clinical Journal of the American Society of Nephrology CJN–00360114 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe A., Howse M., Bell G. & Henry J. Substance abuse and the kidney. Qjm 93, 147–152 (2000). [DOI] [PubMed] [Google Scholar]
- Patel R. R. & Murphy D. J. Forceps delivery in modern obstetric practice. BMJ 328, 1302–1305 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christianson L., Bovbjerg V., McDavitt E. & Hullfish K. Risk factors for perineal injury during delivery. American journal of obstetrics and gynecology 189, 255–260 (2003). [DOI] [PubMed] [Google Scholar]
- HCUP National Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). Agency for healthcare research and quality. Rockville, MD. www.hcup-us.ahrq.gov/nisoverview.jsp Accessed: 2016-03-17 (2007. –2009).
- Slee V. N. The international classification of diseases: ninth revision (icd-9). Annals of internal medicine 88, 424–426 (1978). [DOI] [PubMed] [Google Scholar]
- Fisher R. A., Yates F. et al. Statistical tables for biological, agricultural and medical research. Statistical tables for biological, agricultural and medical research (1949). [Google Scholar]
- Freeman L. C. A set of measures of centrality based on betweenness. Sociometry 35–41 (1977). [Google Scholar]
- Pons P. & Latapy M. Computing communities in large networks using random walks. In Computer and Information Sciences-ISCIS 2005, 284–293 (Springer, 2005). [Google Scholar]
- Raghavan U. N., Albert R. & Kumara S. Near linear time algorithm to detect community structures in large-scale networks. Physical Review E 76, 036106 (2007). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.