Abstract
Background
A low physical activity (PA) level in pregnancy is associated with several adverse health outcomes. Early identification of pregnant women at risk of physical inactivity could inform strategies to promote PA, but no studies so far have presented attempts to develop prognostic models for low PA in pregnancy. Based on moderate-to-vigorous intensity PA (MVPA) objectively recorded in mid/late pregnancy, our objectives were to describe MVPA levels and compliance with the PA guideline (≥150 MVPA minutes/week), and to develop a prognostic model for non-compliance with the PA guideline.
Methods
From a multi-ethnic population-based cohort, we analysed data from 555 women with MVPA recorded in gestational week (GW) 28 with the monitor SenseWear™ Pro3 Armband. Predictor variables were collected in early pregnancy (GW 15). We organized the predictors within the domains health, culture, socioeconomic position, pregnancy, lifestyle, psychosocial factors, perceived preventive effect of PA and physical neighbourhood. The development of the prognostic model followed several steps, including univariate and multiple logistic regression analyses.
Results
Overall, 25 % complied with the PA guideline, but the proportion was lower in South Asians (14 %) and Middle Easterners (16 %) compared with Westerners (35 %). Among South Asians and Middle Easterners, 35 and 28 %, respectively, did not accumulate any MVPA minutes/week compared with 18 % among Westerners. The predictors retained in the prognostic model for PA guideline non-compliance were ethnic minority background, multiparity, high body fat percentage, and perception of few physically active friends. The prognostic model provided fair discrimination between women who did vs. did not comply with the PA guideline.
Conclusion
Overall, the proportion who complied with the PA guideline in GW 28 was low, and women with ethnic minority background, multiparity, high body fat percentage and few physically active friends had increased probability of non-compliance. The prognostic model showed fair performance in discriminating between women who did comply and those who did not comply with the PA guideline.
Electronic supplementary material
The online version of this article (doi:10.1186/s12884-016-0985-x) contains supplementary material, which is available to authorized users.
Keywords: Physical activity, Pregnancy, Multi-ethnic, Prediction
Background
Meeting the recommended levels of physical activity (PA) has particular public health importance during pregnancy as both mother and offspring may benefit. Intervention studies have shown that PA reduces the risk of gestational diabetes (GDM) and neonates being large for gestational age [1–4]. Furthermore, GDM predisposes the mother and her offspring for developing type 2 diabetes and obesity in the future [5–7]. While there is a considerable uncertainty around the cost-effectiveness of interventions including PA promotion during pregnancy [8], the potential for health care workers to reach women across social groups is evident. By capitalizing on this window of opportunity, PA promotion during pregnancy may have long-lasting impact on health outcomes and social health inequalities.
For the general population, there is evidence of substantial health benefit from performing 150 min/week of moderate-to-vigorous intensity PA (MVPA) [9–11], and the same activity target is recommended for healthy pregnant women [12,13]. Despite the health-enhancing effects, the proportion of pregnant women who meet the recommended PA levels ranges from 4 to 60 % [14–17]. In addition to true population differences, this partly reflects different guidelines and methods of PA measurement.
Estimates of PA levels in most studies are based on self-reports [18]. Besides the cohort of this study, we are aware of only one other population-based study of PA correlates that includes objectively recorded PA [16]. We have previously reported on objectively recorded MVPA in early pregnancy from the STORK Groruddalen cohort from which we report in the present study [19]. The scarcity of studies based on objective methods means that estimates of PA levels and PA correlates are prone to reporting bias and inaccuracy [20]. Studies based on objective methods are required to contribute new knowledge about groups and individuals at risk of insufficient MVPA at different stages of pregnancy.
Successful promotion of PA in pregnancy depends on interventions that positively modifies PA behaviour and methods to identify individuals and groups at increased risk of not meeting the recommended levels of PA. Prognostic models are tools that combine multiple predictors to obtain an estimate of probability of a future outcome [21]. Prognostic models are distinctively different from etiological models underpinned by causal theory [22], and they may even be non-causal [23]. While prognostic models are more commonly applied to predict disease outcomes, they may also predict lifestyle outcomes [21]. However, there are few examples of prognostic models developed to predict PA [24], and to our knowledge, no previous studies have presented a prognostic model for insufficient MVPA in pregnancy. To make prognostic models relevant for the clinical setting, it is recommended that predictors should originate from low-cost data collection methods that are not burdensome for the patients [25]. At the same time, potential predictors must reflect current evidence on PA correlates. A consistent association has been shown between low PA levels and non-Western ethnicity, low educational level, past pregnancies and low levels of pre-pregnancy PA [16, 19, 26]. Findings are equivocal with respect to the association with maternal age, occupational group, marital status, and smoking [26].
To inform strategies to promote PA among pregnant women in multi-ethnic populations, there is a need for research based on objective measures to obtain valid estimates of PA levels and their distribution in populations. Objectively recorded PA can also enhance prognostic studies to determine insufficient PA, as accurate predictions rely on unbiased PA data. Based on objectively recorded MVPA, our objectives were to describe MVPA levels and compliance with the PA guideline (i.e. ≥150 MVPA minutes/week) in gestational week (GW) 28, and to develop and validate a prognostic model of guideline non-compliance based on clinical data collected in early pregnancy (GW 15).
Methods
Population, setting and data collection
Data originated from the population-based STORK Groruddalen cohort study (STORK-G), in which participants were pregnant women from multi-ethnic districts in Oslo [27]. Recruitment took place between May 2008 and May 2010 at three public Child Health Clinics where women received antenatal care. Inclusion criteria were planned birth at either of two study hospitals, ≤20 weeks’ gestation, ability to communicate in Norwegian (or Arabic, English, Sorani, Somali, Tamil, Turkish, Urdu, Vietnamese), and ability to give written consent. Exclusion criteria were pre-gestational diabetes or other conditions necessitating intensive hospital follow-up during pregnancy. In total, 823 women were included at the baseline visit (mean GW 15.1, SD 3.7), while 772 attended the follow-up visit (mean GW 28.3, SD1.3) [27]. Anthropometric measurements were recorded and questionnaire data collected during face-to-face interviews at the baseline visit. If required, the interviewing midwives used translated versions of the questionnaires (in one of the eight languages listed under the inclusion criteria), and professional interpreters assisted during interviews if needed. MVPA was objectively recorded for 4 to 7 days immediately after the follow-up visit. Participants gave informed written consent before participation. The Regional Committee for Medical and Health Research Ethics for South Eastern Norway and The Norwegian Data Inspectorate approved the study protocol. The study methods are described in detail elsewhere [27].
Primary outcomes
The two primary outcomes were MVPA minutes/week and PA guideline compliance (150 MVPA minutes/week: yes/no). We calculated MVPA minutes/week by multiplying mean MVPA minutes/day by seven (days). MVPA was objectively recorded with the multi-sensor SenseWear™ Pro3 Armband (SWA) (BodyMedia Inc., Pittsburgh, Pennsylvania, USA). The device collects data on acceleration, skin temperature, heat flux and galvanic skin response, while machine learning algorithms produce estimates of energy expenditure based on the incoming data [28]. The SWA provides valid estimates of energy expenditure during pregnancy [29, 30]. The SWA was affixed across the right triceps brachii of the participant at the follow-up visit (GW 28), and she was asked to wear it continuously for the next 4 to 7 days, except during shower/water activities. We downloaded data with the software from the manufacturer (SenseWear™ Professional Research Software Version 6.1, BodyMedia Inc). The summed value of 1-min epochs was used to estimate metabolic equivalents (METs) (1 MET = 3.5 ml O2 · kg−1 · min−1). MVPA was restricted to bouts ≥10 subsequent minute epochs ≥3METs, and these minutes were extracted with SQL Server Management Studio (Microsoft®) and SQL Server Express version 11.0.5058.0 (Microsoft®). A day of recording was valid if the participant wore the SWA for at least 19.2 h, i.e. 80 % of a 24-h sampling period [31]. In the analysis, we included only data from women with ≥2 valid days of SWA wear time.
Predictors
We selected candidate predictors for PA guideline non-compliance from data collected by trained midwives at the baseline visit. Ethnicity referred to the participant’s country of birth or the country of birth of the mother of the participant if the mother was born outside Europe or North America. Ethnic categories analysed were Western, South Asian, Middle Eastern and other ethnicity. Occupation was recorded according to the International Standard Classification of Occupations [32]. Occupational groups analysed were managers/° occupations, clerical/care occupations, and elementary occupations/homemakers. Parity was categorised as nullipara, unipara and multipara (≥2 births). Pre-pregnancy PA was self-reported and referred to duration and frequency of pre-defined endurance activities three months pre-pregnancy (running/jogging, bicycling, aerobic classes, dancing, ball sports, swimming and brisk walking/skiing) [33]. We calculated total minutes/week by multiplying minutes/sessions by sessions/week (never, 0.5x/week, 1x/week, 2x/week, 4.5x/week and daily), and the total was dichotomised (150 min/week yes/no). Perception of physically active friends was a measure of the underlying construct descriptive norm, i.e. the participants’ perceptions about the physical activity behaviour in other relevant groups [34]. Friends, and in particular same-aged and female friends, were considered to be significant context-specific groups for physical activity among pregnant women [34]. Hence, building upon the combined friends and family scale developed by Okun and colleagues [35], we modified the scale to include three-items pertaining to perceptions of how many friends, same-aged friends and same-aged female friends who were physically active ≥3x/week. Each item was scored on a 5-point Likert Scale (0 = none, 5 = all). The item loadings derived by exploratory factor analysis ranged from 0.88 to 0.93 while the Cronbach Alpha score was 0.89, indicating a one-factor structure with a high level of internal consistency. The sum score of the three items was median-dichotomized into many versus few physically active friends. Perceived preventive effect of PA was expressed as the sum of scores of nine items (cardiovascular, musculoskeletal, type 2 diabetes, cancer, hypertension, mental illness, overweight/obesity, abdominal/intestinal disease, and, asthma/allergies) scored on 3-point scales (0 = no effect, 1 = little effect, 2 = large effect). Body fat percentage was measured with bioelectric impedance analysis using Tanita-Weight BC-418 MA (Tanita Corp., Tokyo, Japan) [27, 36]. Descriptions of candidate predictors not included in the full model are available as supplementary material [Additional file 1].
Reasons for missing data
Of the 823 subjects included at baseline, 51 did not attend the follow-up visit in GW 28 due to abortions/preterm birth (n = 18) or unknown reasons (n = 33). Among the remaining 772 who attended the follow-up visit, reasons for missing MVPA data were: no available SWA due to logistical problems (n = 47), the participant declined or was unable to wear the SWA (n = 48), or the participant wore the SWA but had insufficient wear time (n = 122).
Statistical analyses
Descriptive characteristics are presented as mean, median, standard deviation (SD), interquartile range and proportions. Group differences are analysed by t-tests and Chi-square tests, as appropriate.
Development of prognostic model
Development and validation of the prognostic model are reported in accordance with the TRIPOD-statement [21]. To develop the prognostic model, we initially identified potential predictors based on a review of the literature. The predictors were organized into eight domains (health, culture, socioeconomic position, pregnancy, lifestyle, psychosocial factors, perceived preventive effect of PA and physical neighbourhood). Following removal of predictors with p > 0.2 in univariate regression [37], candidate predictors in seven of the domains remained (no predictors remained in the domain physical neighbourhood). To enhance the prediction, we included the strongest predictor from each of the seven domains in the full model [24]. Starting with the full model, we performed multiple logistic regression analysis with backward elimination to determine the final prognostic model. Further details are presented as supplementary material [Additional file 2].
Calibration of the final model was assessed by the Hosmer-Lemeshow test. A calibration plot presents the test result graphically by showing agreement between observed and predicted values by sample deciles, where perfect predictions align along the 45° line [25]. We assessed the ability of the model to discriminate between women who complied vs. did not comply with the PA guideline by the Area Under the Receiver Operating Characteristic (AU-ROC) curve [25].
Internal validation of prognostic model
We performed a bootstrap resampling procedure using 1,000 iterations to correct for overfitting [38, 39]. The shrunk model consisted of corrected coefficients calculated as the average of the coefficients from the 1,000 bootstrap samples. As internal validation of the discrimination, we calculated the bias-corrected AU-ROC (i.e. the average of all 1,000 AU-ROCs) with bootstrap generated 95 % CI.
P-values ≤0.05 were considered statistically significant. All analyses were performed in Stata 13 [40].
Sensitivity analysis
We analysed sensitivity to number of SWA days by repeating the multiple logistic regression with backward elimination, starting with the full mode, using observations with ≥4 valid SWA days and comparing the resultant odds ratios with the odds ratios from the original model based on observations with ≥2 valid SWA days.
Starting with the full model, we performed multiple logistic regression analysis with backward elimination.
Results
Sample characteristics
The sample consisted of 555 participants with valid SWA data. At the baseline visit, mean (min-max/SD) age was 30.1 years (19.3–45.1/4.9) and pre-pregnancy body mass index (BMI) was 24.4 kg/m2 (14.9–49.2/4.8), while body fat percentage was 33.1 % (10.9–53.5/7.4) (Table 1). SWA wear time mean (SD) was 3.6 (1.0) days. Compared with women not eligible for the analyses, the sample was marginally older, had marginally lower body mass index, and had a higher proportion of Western women (Table 1).
Table 1.
Characteristics of cohort at stratified by eligibility for analysis
| Valid SWA data (eligible) | Without valid SWA data (not eligible) | ||||
|---|---|---|---|---|---|
| (n = 555) | (n = 268) | ||||
| n | % | n | % | P-value a | |
| Ethnicity | <0.01 | ||||
| South Asian | 125 | (22.5) | 75 | (28.0) | |
| Middle Eastern | 75 | (13.5) | 51 | (19.0) | |
| Other ethnicity | 100 | (18.0) | 61 | (22.8) | |
| Western | 255 | (46.0) | 81 | (30.2) | |
| Occupation | 0.20 | ||||
| Elementary occupations and homemakers | 150 | (27.4) | 86 | (33.5) | |
| Clerical/care occupations | 196 | (35.8) | 86 | (33.5) | |
| Manager/° occupations | 202 | (36.8) | 85 | (33.0) | |
| Missing | 7 | 11 | |||
| Education | 0.39 | ||||
| <10 years | 85 | (15.4) | 48 | (18.2) | |
| 10–12 years | 216 | (39.0) | 108 | (40.9) | |
| University or college | 252 | (45.6) | 108 | (40.9) | |
| Missing | 2 | 4 | |||
| Parity | 0.11 | ||||
| None (nulliparous) | 253 | (45.6) | 128 | (47.8) | |
| 1 (uniparous) | 201 | (36.2) | 79 | (29.5) | |
| ≥2 (multiparous) | 101 | (18.2) | 61 | (22.7) | |
| Smoking 3 months pre-pregnancy | 0.96 | ||||
| Non-smoker | 455 | (82.4) | 218 | (82.6) | |
| Irregular or daily smoker | 97 | (17.6) | 46 | (17.4) | |
| Missing | 3 | 4 | |||
| Self-reported pre-pregnancy PA | 0.16 | ||||
| ≥150 min/wk | 220 | (40.6) | 91 | (35.4) | |
| <150 min/wk | 322 | (59.4) | 166 | (64.6) | |
| Missing | 13 | 11 | |||
| Health pre-pregnancy | 0.78 | ||||
| Poor/not too good | 58 | (10.6) | 30 | (11.5) | |
| Good | 279 | (50.7) | 137 | (52.3) | |
| Very good | 213 | (38.7) | 95 | (36.2) | |
| Missing | 5 | 6 | |||
| Pelvic girdle-/lumbopelvic pain | 0.87 | ||||
| Yes | 228 | (41.8) | 107 | (41.2) | |
| No | 318 | (58.2) | 153 | (58.8) | |
| Missing | 9 | 8 | |||
| Mean | SD | Mean | SD | P-value b | |
| Age (years) | 30.1 | (4.9) | 29.3 | (4.8) | 0.02 |
| BMI pre-pregnancy | 24.4 | (4.8) | 25.0 | (4.9) | <0.01 |
| Body fat percentage | 33.1 | (7.4) | 34.5 | (7.3) | 0.15 |
SD standard deviation, SWA Sensewear Armband, BMI body mass index
a Chi-Square test
b t-test
PA guideline compliance (unadjusted analyses)
Overall, 25 % complied with the PA guideline in GW 28. By ethnic groups, 35 % of Westerners complied with the guideline, 14 % of South Asians and 16 % of Middle Easterners. (Table 2). Having university/college education, manager/° occupations, being nullipara, and having a low body fat percentage were all associated with compliance (Table 2).
Table 2.
Moderate-to-vigorous intensity physical activity and compliance with the physical activity guideline at follow-up visit (n = 555)
| MVPA min/wk a | PA guideline compliance a | ||||
|---|---|---|---|---|---|
| Median | IQR | n | % | P-value b | |
| Overall | 64.4 | (12.8–152.3) | 141 | (25.4) | |
| Ethnicity | <0.01 | ||||
| South Asian | 23.8 | (0–119.0) | 18 | (14.4) | |
| Middle Eastern | 35.0 | (0–95.7) | 12 | (16.0) | |
| Other ethnicity | 59.3 | (0–137.1) | 22 | (22.0) | |
| Western | 84.0 | (26.8–183.4) | 89 | (34.9) | |
| Occupation | <0.01 | ||||
| Elementary occupations & homemakers | 26.8 | (0–99.8) | 23 | (15.3) | |
| Clerical/care occupations | 55.4 | (0–125.1) | 41 | (20.9) | |
| Manager/° occupations | 103.3 | (35.0–184.3) | 76 | (37.6) | |
| Education | <0.01 | ||||
| <10 years education | 47.8 | (0–117.2) | 15 | (17.7) | |
| 10–12 years education | 38.5 | (0–107.6) | 42 | (19.4) | |
| University/college | 84.0 | (23.3–177.0) | 84 | (33.3) | |
| Parity | <0.01 | ||||
| None (nulliparous) | 78.4 | (12.8–169.8) | 80 | (31.6) | |
| 1 (uniparous) | 66.5 | (21.0–161.0) | 54 | (26.9) | |
| ≥2 (multiparous) | 30.3 | (0–85.8) | 7 | (6.9) | |
| Planned pregnancy | 0.04 | ||||
| Yes | 75.6 | (19.3–159.3) | 114 | (27.6) | |
| No | 38.5 | (0–108.5) | 26 | (19.0) | |
| Smoking 3 months pre-pregnancy | 0.50 | ||||
| Non-smoker | 65.3 | (0–155.8) | 118 | (25.9) | |
| Irregular or daily smoker | 57.8 | (19.3–141.4) | 22 | (22.7) | |
| Self-reported pre-pregnancy PA | 0.02 | ||||
| ≥150 min/week | 84.0 | (9.6–178.5) | 68 | (30.9) | |
| <150 min/week | 49.0 | (12.8–133.0) | 70 | (21.7) | |
| Physically active friends | <0.01 | ||||
| Many | 77.0 | (19.3–179.7) | 81 | (31.3) | |
| Few | 51.3 | (0–119.0) | 60 | (20.3) | |
| Health pre-pregnancy | <0.01 | ||||
| Poor/not too good | 40.3 | (0–105.0) | 8 | (13.8) | |
| Good | 51.3 | (0–127.8) | 60 | (21.5) | |
| Very good | 84.0 | (23.3–175.0) | 72 | (33.8) | |
| Pelvic girdle-/lumbopelvic pain | 0.07 | ||||
| Yes | 51.9 | (6.4–120.8) | 48 | (21.1) | |
| No | 72.6 | (17.5–164.5) | 89 | (28.0) | |
| Mean | SD | P-value c | |||
| Age, years | 29.8 | (4.6) | 0.39 | ||
| Body fat percentage | 29.7 | (7.3) | <0.01 | ||
IQR interquartile range, PA physical activity, MVPA moderate-to-vigorous physical activity
a Recorded by Sensewear Armband Pro3
b Chi-square test of difference between categories in PA guideline compliance
c Unpaired t-test
MVPA minutes/week (unadjusted analyses)
Overall, 25 % of the sample recorded no MVPA minutes/week in bouts ≥10 min. The proportion was 18 % for Westerners, 35 % for South Asians and 18 % for Middle Easterners. Differences in MVPA minutes/week were observed across ethnic groups, educational categories, parity categories and pre-pregnancy PA (Table 2).
Prognostic model
After elimination of predictors from the original list of candidate predictors [Additional file 2], remaining predictors included in the full model were ethnicity (P < 0.01), occupation (P < 0.01), parity (P < 0.01), pre-pregnancy PA (P = 0.02), physically active friends (P < 0.01), perceived preventive effect of PA (P = 0.14) and body fat percentage (P < 0.01). After multiple logistic regression with backward elimination, the four predictors retained in the final prognostic model were ethnicity, parity, physically active friends and body fat percentage (Nagelkerke R2 = 0.14) (Table 3). The sensitivity analysis based on data from participants with ≥4 valid SWA days supported the results in the original prognostic model.
Table 3.
Odds ratios for not meeting the physical activity guideline by multiple logistic regression analyses (n = 535)
| Predictors | Final model | Bootstrap validation | ||||
|---|---|---|---|---|---|---|
| OR | (95 % CI) | P-value | OR | (95 % CI) | P-value | |
| Ethnicity (ref: Western) | ||||||
| South Asian | 2.7 | (1.5, 4.8) | <0.01 | 2.7 | (1.4, 5.0) | <0.01 |
| Middle Eastern | 2.2 | (1.1, 4.5) | 0.03 | 2.2 | (1.1, 4.5) | 0.04 |
| Other | 1.8 | (1.0, 3.3) | 0.05 | 1.8 | (1.0, 3.4) | 0.05 |
| Parity (ref: nulliparous) | ||||||
| 1 (uniparous) | 1.2 | (0.8, 1.8) | 0.48 | 1.2 | (0.7, 1.9) | 0.50 |
| ≥2 (multiparous) | 5.3 | (2.1, 12.9) | <0.01 | 5.3 | (1.9, 1.6) | <0.01 |
| Physically active friends (ref: many) a | ||||||
| Few | 1.7 | (1.1, 2.6) | 0.01 | 1.7 | (1.1, 2.7) | 0.02 |
| Body fat percentage | 1.1 | (1.06, 1.13) | <0.01 | 1.1 | (1.06, 1.13) | <0.01 |
| Constant | 0.07 | (0.02 0.21) | <0.01 | 0.07 | (0.02, 0.22) | <0.01 |
OR odds ratio, CI confidence interval, PA physical activity
aMissing values on 20 women
The final prognostic model demonstrated fair discrimination between women who complied and did not comply with the PA guideline (AU-ROC = 0.749) (Fig. 1) [41]. The calibration plot (Fig. 2) and the Hosmer-Lemeshow test (P = 0.85) based on the final model demonstrated a good match between the predicted and observed outcomes across deciles of the data.
Fig. 1.
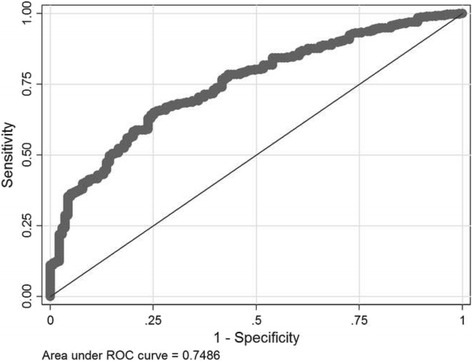
Receiver Operating Characteristics (ROC) curve. The discriminatory power of the prognostic model, expressed as the area under the Receiver Operating Characteristics (ROC) curve
Fig. 2.
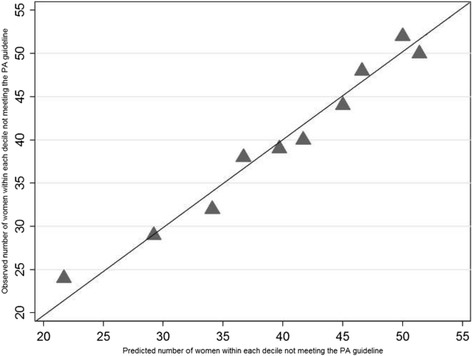
Calibration plot. Triangles (▲) express the agreement between observed and predicted non-compliance with the physical activity guideline for each sample decile. The 45° line represents perfect predictions
Model validation
The adjusted coefficients derived by the bootstrap resampling corresponded with the coefficients in the final prognostic model, indicating the model was not overfitted. The bias corrected AU-ROC (95 % CI) was 0.757 (0.638, 0.784), which indicates bias was marginal (−0.008).
An example of risk estimation for sub-groups using the prognostic model shows that the predicted probability of PA guideline non-compliance is 98 % for multiparous South Asian women with few physically active friends and 38 % body fat.
Discussion
To our knowledge, the STORK-G is the only population-based pregnancy cohort in Europe that includes objectively recorded MVPA. Special efforts were made to recruit ethnic minority women who constitute a growing proportion of pregnant women in Europe. Furthermore, the present study is the first to develop and validate a prognostic model for non-compliance with a PA guideline for pregnant women.
Only 25 % of pregnant women complied with the PA guideline in GW 28. Even more alarming, only 14 % of South Asians and 16 % of Middle Easterners complied, while the prevalence was 35 % among Western women. The prevalence of PA guideline compliance was 33 % among women with university/college education and 19 % among those with <12 years education. One in four never recorded MVPA of at least 10 min duration. The prognostic model showed that ethnic minority background, multiparity, high body fat percentage and few physically active friends predicted non-compliance with the PA guideline. The predicted outcome was correct for three out of four women, which is considered as a fair discriminatory performance (bias corrected AU-ROC 0.757).
Guideline compliance and MVPA
Previous studies show a large variation in PA guideline compliance, which partly reflect different guideline recommendations. Studies have shown the proportion of women who achieved 150 MVPA minutes/week based on total MVPA minutes dropped by approximately 50 % after extracting exclusively MVPA in bouts ≥10 min [42, 43]. Conceptually, the restriction of MVPA to bouts of activity corresponds better with studies based on self-reported PA, since questionnaire items typically refer to PA restricted to bouts [44]. Our findings are in accordance with studies of guideline compliance (≥150 MVPA minutes/week) based on self-reported PA which have shown that 11–32 % of pregnant women meet the target [15, 45, 46]. There are no population-based cohort studies that use objectively recorded MVPA restricted to bouts, but results from smaller studies of predominantly White healthy women suggest that 28–45 % of pregnant women comply with the PA guideline [42, 43]. The allowance of 2-min-interruptions within bouts and the homogeneous population are possible explanations why compliance was higher in those studies [42, 43]. We observed ethnic differences in prevalence of non-compliance and proportions with no recorded MVPA. Given that MVPA in bouts reflects recreational and transport activities better than MVPA without restriction, the ethnic difference may indicate that ethnic minority women perform such activities less frequently, or at intensities <3 METs. Previous population-based studies in Scandinavia have not addressed ethnic differences in PA in pregnancy [14, 47], but we found similar ethnic differences in MVPA, not restricted to bouts, from the current cohort in early pregnancy [19]. In agreement with our findings, a population based study from US using objectively recorded PA from pregnant women showed that non-Hispanic Black women recorded less MVPA than White women [16]. As the ethnic composition of our sample is different, our study contributes new and important evidence highlighting that ethnic differences in physical activity in mid-/late pregnancy is a public health concern in Northern Europe. Future research should explore mechanisms underlying these differences.
Prediction of non-compliance with the PA guideline
The prognostic analysis presented is best described as a combined development and validation study [21], and as far as we are aware, it is the first report of a prognostic model development for PA guideline non-compliance in pregnancy. It was our motivation to extend the utility of predictors, from providing odds ratios (reflecting groups’ probabilities of non-compliance), to a model that could discriminate those who comply from those who do not comply with the PA guideline. The prognostic model of non-compliance with the PA guideline consisted of ethnicity, parity, physically active friends and body fat percentage.
The strong association observed between multiparity and non-compliance has been reported consistently [14, 47]. We found no significantly increased risk for uniparas (OR 1.2), probably due to few uniparas in the sample. While causal associations cannot be determined in the present study, our results concur with studies indicating special approaches are needed to promote PA among pregnant women with children.
To our knowledge, the observed positive association between many physically active friends and PA guideline compliance has not been reported previously in studies of pregnant women. A positive association between maternal PA and PA level of the spouse partly lends support to our finding [48]. In another Norwegian pregnancy cohort, no association was observed between exercise and the perceived exercise habits of friends [49]. The conflicting finding may partly reflect that exercise was self-reported and assessed at a later stage of pregnancy in a highly educated population [49]. Our finding suggests that a perception of having few physically active friends is a relevant predictor of PA guideline non-compliance in socially heterogeneous populations.
Our study showed that the probability of non-compliance with the PA guideline in GW 28 was strongly associated with body fat percentage in GW 15, and this finding concurs with previous reports of an inverse association between BMI and PA [14]. While BMI measures are more accessible in a primary health care setting, we decided to use bio-impedance derived body fat percentage based on reports of ethnic differences in the ratio between body fat and BMI [50]. Surprisingly, pre-pregnancy PA was not associated with PA guideline non-compliance in the final model. It seems plausible that the association between body fat percentage and non-compliance partly mediates the association between pre-pregnancy PA and PA level in pregnancy. Pre-pregnancy PA was self-reported and the lack of association may be explained by poor agreement between self-reported and objectively recorded PA [44, 51]. To our knowledge, an associations between pre-pregnancy PA and PA in pregnancy manifest only in studies based on self-reported PA at both time points [52, 53]. Hence, health care workers should be cautious in making inferences based upon self-reported PA as a measure of the true PA level.
The four predictors in the final prognostic model were strongly associated with PA guideline non-compliance, but this does not guarantee correct discrimination between women who did comply versus women who did not comply [54], and we observed only a fair discriminatory performance. Since measures of discriminatory performance may supplement odds ratios with information about the probability of non-compliance of an individual [55], we encourage integration of such measures in future studies to, hopefully, develop prognostic model with a better discriminatory performance.
Strengths and weaknesses
The present study has several strengths such as the objectively recorded PA, the prospective design, the population-based sample, inclusion of a high proportion of ethnic minority women often excluded in research, a wide range of theoretically informed variables including psychosocial variables related to PA, and a high attendance rate [27]. Compared with other frequently used methods for objective PA recording (such as accelerometry), the SWA is considered more user-friendly and accurate [56]. Furthermore, we used bouts of MVPA ≥10 min, which is more strongly associated with health outcomes in the general populations, but is less studied in pregnancy. The ethnic composition of the cohort was representative for the largest ethnic groups of pregnant women in the participating city districts [27], probably making the study relevant to the pregnant populations in other European countries. While external validation of a prognostic model is optimal, it is often not feasible. Hence, we used the bootstrap procedure to correct for over-fitting, which is considered the optimal internal validation method [25].
However, this study also has weaknesses. In total, 33 % of the original cohort had incomplete or missing SWA data. A higher drop-out among ethnic minorities may have biased the estimates of MVPA minutes/week and PA guideline compliance. However, associations and the odds ratios are less prone to bias [57]. While energy expenditure recorded with other SWA models have been validated among pregnant women [29, 30], the model used in the present study has not been formally validated. However, estimates of energy expenditure does not differ significantly between the models [58]. Including SWA data from individuals with a minimum of 2 valid days in analyses deviates from the recommended minimum of 3–5 valid days [31]. However, by requiring wear time ≥19.2 h/day, an even lower number of valid days has been deemed sufficient [59]. Sensitivity analysis based on ≥4 valid days yielded similar odds ratios. Finally, wearing the SWA may have motivated participants to extend periods of MVPA.
Conclusion
The low prevalence of PA guideline compliance (25 %) in GW 28 and the relatively large proportion (25 %) of women who never recorded MVPA in bouts ≥ 10 min are causes for concern from a public health perspective. Despite the higher prevalence of PA guideline non-compliance in certain risk groups, the overall non-compliance highlights the need for interventions reaching all pregnant women. The development of a prognostic model showed that the most important predictors of guideline non-compliance were ethnic minority background, multiparity, few physically active friends and high body fat percentage. While the odds ratios were highly significant, the model performed fairly well in discriminating between women who did comply and did not comply with the PA guideline. No previous studies of PA in pregnancy have included assessments of the discriminatory performance of predictors. To inform the risk assessments made by antenatal health care staff as part of their lifestyle counselling, future research should integrate measures of discriminatory performance in prospective studies of PA during pregnancy.
Abbreviations
AU-ROC, area under the receiver operating characteristic; BMI, body mass index; GDM, gestational diabetes mellitus; GW, gestational week; MET, metabolic equivalents; MVPA, moderate-to-vigorous intensity physical activity; OR, odds ratio; PA, physical activity; SD, standard deviation; STORK-G, stork-groruddalen cohort study; SWA, Sensewear Armband
Acknowledgements
The authors are grateful for the contribution of the women who participated in this study, and the staff at the child health clinics in Stovner, Grorud and Bjerke districts in Oslo. We are also grateful for the contributions by Britt Stuge, PhD. (Department of Orthopaedics, Oslo University Hospital, Norway) and Katrine M. Owe, PhD. (Norwegian Resource Centre for Women’s Health and National Institute of Public Health, Norway) who commented on the operationalization of pelvic girdle pain.
Funding
The Stork Groruddalen Research Programme was funded by The Norwegian Research Council, The South-Eastern Norway Regional Health Authority, The Norwegian Directorate of Health, and, collaborative partners in district administrations for Stovner, Grorud and Bjerke within the City of Oslo. KRR is funded by a full-time PhD-scholarship from the Norwegian National Advisory Unit on Women’s Health (Oslo University Hospital). The funding bodies were not involved in decisions concerning the study design, or collection, analysis and interpretation of date or in writing the manuscript.
Availability of data and materials
Due to ethical restrictions and patient confidentiality, not all data can be made publicly available. Data are available upon request from the Medical Faculty at the University of Oslo for researchers who meet the criteria for access to confidential data. Access can be arranged by direct request to co-author Anne Karen Jenum (a.k.jenum@medisin.uio.no).
Authors’ contributions
RSF, AKJ, SB and KRR contributed substantially to the conception and design of the study. AKJ, KM, YO and SB planned the acquisition of data. RSF, AKJ, KM, EWM, YO, SB and KRR made substantial contributions to the analysis and interpretation of data, and, in drafting the manuscript. All authors revised the draft manuscript critically and have read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Participants gave informed written consent before participation. The Regional Committee for Medical and Health Research Ethics for South Eastern Norway approved the study protocol.
Additional files
Operationalization of variables. Detailed presentation of the operationalization of candidate predictors considered for analysis not included in the full model. (PDF 220 kb)
Predictor selection procedure. Presentation of the step-by-step procedure used for identifying candidate predictors and selecing the final predictors included in the prognostic model. (PDF 152 kb)
Contributor Information
Kåre Rønn Richardsen, Email: kareri@hioa.no.
Ragnhild Sørum Falk, Email: rs@ous-hf.no.
Anne Karen Jenum, Email: a.k.jenum@medisin.uio.no.
Kjersti Mørkrid, Email: kjersti.morkrid@fhi.no.
Egil Wilhelm Martinsen, Email: e.w.martinsen@medisin.uio.no.
Yngvar Ommundsen, Email: yngvar.ommundsen@nih.no.
Sveinung Berntsen, Email: sveinung.berntsen@uia.no.
References
- 1.Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynecol. 2012;24(6):387–394. doi: 10.1097/GCO.0b013e328359f131. [DOI] [PubMed] [Google Scholar]
- 2.Wiebe HW, Boule NG, Chari R, Davenport MH. The effect of supervised prenatal exercise on fetal growth: a meta-analysis. Obstet Gynecol. 2015;125(5):1185–1194. doi: 10.1097/AOG.0000000000000801. [DOI] [PubMed] [Google Scholar]
- 3.Sanabria-Martinez G, Garcia-Hermoso A, Poyatos-Leon R, Alvarez-Bueno C, Sanchez-Lopez M, Martinez-Vizcaino V. Effectiveness of physical activity interventions on preventing gestational diabetes mellitus and excessive maternal weight gain: a meta-analysis. BJOG. 2015;122(9):1167–1174. doi: 10.1111/1471-0528.13429. [DOI] [PubMed] [Google Scholar]
- 4.Russo LM, Nobles C, Ertel KA, Chasan-Taber L, Whitcomb BW. Physical activity interventions in pregnancy and risk of gestational diabetes mellitus: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(3):576–582. doi: 10.1097/AOG.0000000000000691. [DOI] [PubMed] [Google Scholar]
- 5.Guo J, Chen JL, Whittemore R, Whitaker E. Postpartum Lifestyle Interventions to Prevent Type 2 Diabetes Among Women with History of Gestational Diabetes: A Systematic Review of Randomized Clinical Trials. J Womens Health (Larchmt) 2016;25(1):38–49. doi: 10.1089/jwh.2015.5262. [DOI] [PubMed] [Google Scholar]
- 6.Heida KY, Franx A, van Rijn BB, Eijkemans MJ, Boer JM, Verschuren MW, Oudijk MA, Bots ML, van der Schouw YT. Earlier Age of Onset of Chronic Hypertension and Type 2 Diabetes Mellitus After a Hypertensive Disorder of Pregnancy or Gestational Diabetes Mellitus. Hypertension. 2015;66(6):1116–1122. doi: 10.1161/HYPERTENSIONAHA.115.06005. [DOI] [PubMed] [Google Scholar]
- 7.Veeraswamy S, Vijayam B, Gupta VK, Kapur A. Gestational diabetes: the public health relevance and approach. Diabetes Res Clin Pract. 2012;97(3):350–358. doi: 10.1016/j.diabres.2012.04.024. [DOI] [PubMed] [Google Scholar]
- 8.NICE (National Institute for Health and Clinical Excellence). NICE Public Health Guidance, No 27. Weight Management before, during and after Pregnancy. NICE: London. 2010. https://www.nice.org.uk/guidance/ph27/resources/weight-management-before-during-and-after-pregnancy-1996242046405. Accessed 20 May 2016.
- 9.WHO . Global recommendations on physical activity for health. Geneva, Switzerland: WHO Press; 2010. [PubMed] [Google Scholar]
- 10.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 11.Powell KE, Paluch AE, Blair SN. Physical activity for health: What kind? How much? How intense? On top of what? Annu Rev Public Health. 2011;32:349–365. doi: 10.1146/annurev-publhealth-031210-101151. [DOI] [PubMed] [Google Scholar]
- 12.Canadien Society for Exercise Physiology. Canadian Physical Activity Guidelines - Scientific Statement. http://www.csep.ca/CMFiles/Guidelines/CanadianPhysicalActivityGuidelinesStatements_E%203.pdf. Accessed 5 Jan 2016.
- 13.ACSM . ACSM’s guidelines for exercise testing and prescription. Philadelphia, Pa: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 14.Juhl M, Madsen M, Andersen AM, Andersen PK, Olsen J. Distribution and predictors of exercise habits among pregnant women in the Danish National Birth Cohort. Scand J Med Sci Sports. 2012;22(1):128–138. doi: 10.1111/j.1600-0838.2010.01125.x. [DOI] [PubMed] [Google Scholar]
- 15.Evenson KR, Savitz DA, Huston SL. Leisure-time physical activity among pregnant women in the US. Paediatr Perinat Epidemiol. 2004;18(6):400–407. doi: 10.1111/j.1365-3016.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 16.Evenson KR, Wen F. Prevalence and correlates of objectively measured physical activity and sedentary behavior among US pregnant women. Prev Med. 2011;53(1–2):39–43. doi: 10.1016/j.ypmed.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Santos PC, Abreu S, Moreira C, Lopes D, Santos R, Alves O, Silva P, Montenegro N, Mota J. Impact of compliance with different guidelines on physical activity during pregnancy and perceived barriers to leisure physical activity. J Sports Sci. 2014 doi: 10.1080/02640414.2014.893369. [DOI] [PubMed] [Google Scholar]
- 18.Pereira MA, Rifas-Shiman SL, Kleinman KP, Rich-Edwards JW, Peterson KE, Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007;32(4):312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berntsen S, Richardsen KR, Morkrid K, Sletner L, Birkeland KI, Jenum AK. Objectively recorded physical activity in early pregnancy: a multiethnic population-based study. Scand J Med Sci Sports. 2014;24(3):594–601. doi: 10.1111/sms.12034. [DOI] [PubMed] [Google Scholar]
- 20.Ainsworth B, Cahalin L, Buman M, Ross R. The current state of physical activity assessment tools. Prog Cardiovasc Dis. 2015;57(4):387–395. doi: 10.1016/j.pcad.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13:1. doi: 10.1186/s12916-014-0241-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shmueli G. To Explain or to Predict? Stat Sci. 2010;25(3):289–310. doi: 10.1214/10-STS330. [DOI] [Google Scholar]
- 23.Moons KG, Royston P, Vergouwe Y, Grobbee DE, Altman DG. Prognosis and prognostic research: what, why, and how? BMJ. 2009;338:b375. doi: 10.1136/bmj.b375. [DOI] [PubMed] [Google Scholar]
- 24.King AC, Kiernan M, Oman RF, Kraemer HC, Hull M, Ahn D. Can we identify who will adhere to long-term physical activity? Signal detection methodology as a potential aid to clinical decision making. Health Psychol. 1997;16(4):380. doi: 10.1037/0278-6133.16.4.380. [DOI] [PubMed] [Google Scholar]
- 25.Steyerberg EW. Clinical prediction models: a practical approach to development, validation, and updating. New York: Springer; 2009. [Google Scholar]
- 26.Gaston A, Cramp A. Exercise during pregnancy: a review of patterns and determinants. J Sci Med Sport. 2011;14(4):299–305. doi: 10.1016/j.jsams.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 27.Jenum AK, Sletner L, Voldner N, Vangen S, Morkrid K, Andersen LF, Nakstad B, Skrivarhaug T, Rognerud-Jensen OH, Roald B, et al. The STORK Groruddalen research programme: A population-based cohort study of gestational diabetes, physical activity, and obesity in pregnancy in a multiethnic population. Rationale, methods, study population, and participation rates. Scand J Public Health. 2010;38(Suppl 5):60–70. doi: 10.1177/1403494810378921. [DOI] [PubMed] [Google Scholar]
- 28.Mechanick JI, Kushner RF. Lifestyle Medicine : A Manual for Clinical Practice. Cham: Springer International Publishing; 2016. [Google Scholar]
- 29.Berntsen S, Stafne SN, Morkved S. Physical activity monitor for recording energy expenditure in pregnancy. Acta Obstet Gynecol Scand. 2011;90(8):903–907. doi: 10.1111/j.1600-0412.2011.01172.x. [DOI] [PubMed] [Google Scholar]
- 30.Smith KM, Lanningham-Foster LM, Welk GJ, Campbell CG. Validity of the SenseWear(R) Armband to predict energy expenditure in pregnant women. Med Sci Sports Exerc. 2012;44(10):2001–2008. doi: 10.1249/MSS.0b013e31825ce76f. [DOI] [PubMed] [Google Scholar]
- 31.Matthews CE, Hagstromer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population-based research. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S68–S76. doi: 10.1249/MSS.0b013e3182399e5b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ILO . International standard classification of occupations: ISCO-88. Geneva: International Labour Office; 1990. [Google Scholar]
- 33.Brantsaeter AL, Owe KM, Haugen M, Alexander J, Meltzer HM, Longnecker MP. Validation of self-reported recreational exercise in pregnant women in the Norwegian Mother and Child Cohort Study. Scand J Med Sci Sports. 2010;20(1):e48–e55. doi: 10.1111/j.1600-0838.2009.00896.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Priebe CS, Spink KS. When in Rome: Descriptive norms and physical activity. Psychol Sport Exercise. 2011;12(2):93–98. doi: 10.1016/j.psychsport.2010.09.001. [DOI] [Google Scholar]
- 35.Okun MA, Karoly P, Lutz R. Clarifying the contribution of subjective norm to predicting leisure-time exercise. Am J Health Behav. 2002;26(4):296–305. doi: 10.5993/AJHB.26.4.6. [DOI] [PubMed] [Google Scholar]
- 36.Ueda Y, Maruo M, Nakano H, Honda Y, Miyama T, Nishizawa M, Heymsfield S. Estimation of body fat mass in pregnant women by a new method using bioelectrical impedance analysis with compensation for intrauterine component weight. Int J Body Compos Res. 2006;4(4):145. [Google Scholar]
- 37.Hosmer JDW, Lemeshow S, Sturdivant RX. Model-Building Strategies and Methods for Logistic Regression. In: Hosmer J, DW, Lemeshow S, Sturdivant R, editors. Applied Logistic Regression. 3rd ed. Hoboken, New Jersey, US: John Wiley & Sons, Inc.; 2013. p. 89–151.
- 38.Labarere J, Bertrand R, Fine MJ. How to derive and validate clinical prediction models for use in intensive care medicine. Intensive Care Med. 2014;40(4):513–527. doi: 10.1007/s00134-014-3227-6. [DOI] [PubMed] [Google Scholar]
- 39.Steyerberg EW, Harrell FE, Jr, Borsboom GJ, Eijkemans M, Vergouwe Y, Habbema JDF. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54(8):774–781. doi: 10.1016/S0895-4356(01)00341-9. [DOI] [PubMed] [Google Scholar]
- 40.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013.
- 41.Kleinbaum DG, Klein M. Assessing Discriminatory Performance of a Binary Logistic Model: ROC Curves. In: Kleinbaum DG, Klein M, editors. Logistic Regression: A Self-Learning Text. New York, NY: Springer New York; 2010. pp. 345–387. [Google Scholar]
- 42.Smith KM, Campbell CG. Physical activity during pregnancy: impact of applying different physical activity guidelines. J Pregnancy. 2013 doi: 10.1155/2013/165617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Fabio DR, Blomme CK, Smith KM, Welk GJ, Campbell CG. Adherence to physical activity guidelines in mid-pregnancy does not reduce sedentary time: an observational study. Int J Behav Nutr Phys Act. 2015;12(1):191. doi: 10.1186/s12966-015-0191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Evenson KR, Chasan-Taber L, Symons Downs D, Pearce EE. Review of self-reported physical activity assessments for pregnancy: summary of the evidence for validity and reliability. Paediatr Perinat Epidemiol. 2012;26(5):479–494. doi: 10.1111/j.1365-3016.2012.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borodulin KM, Evenson KR, Wen F, Herring AH, Benson AM. Physical activity patterns during pregnancy. Med Sci Sports Exerc. 2008;40(11):1901–1908. doi: 10.1249/MSS.0b013e31817f1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kraschnewski JL, Chuang CH, Downs DS, Weisman CS, McCamant EL, Baptiste-Roberts K, Zhu J, Kjerulff KH. Association of Prenatal Physical Activity and Gestational Weight Gain: Results from the First Baby Study. Women’s Health Issues. 2013;23(4):e233–e238. doi: 10.1016/j.whi.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Owe KM, Nystad W, Bo K. Correlates of regular exercise during pregnancy: the Norwegian Mother and Child Cohort Study. Scand J Med Sci Sports. 2009;19(5):637–645. doi: 10.1111/j.1600-0838.2008.00840.x. [DOI] [PubMed] [Google Scholar]
- 48.Leppanen M, Aittasalo M, Raitanen J, Kinnunen TI, Kujala UM, Luoto R. Physical activity during pregnancy: predictors of change, perceived support and barriers among women at increased risk of gestational diabetes. Matern Child Health J. 2014;18(9):2158–2166. doi: 10.1007/s10995-014-1464-5. [DOI] [PubMed] [Google Scholar]
- 49.Haakstad LA, Voldner N, Henriksen T, Bo K. Why do pregnant women stop exercising in the third trimester? Acta Obstet Gynecol Scand. 2009;88(11):1267–1275. doi: 10.3109/00016340903284901. [DOI] [PubMed] [Google Scholar]
- 50.Deurenberg P, Deurenberg M, Deurenberg Yap S. Guricci: Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3(3):141–146. doi: 10.1046/j.1467-789X.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 51.Brett KE, Wilson S, Ferraro ZM, Adamo KB. Self-report Pregnancy Physical Activity Questionnaire overestimates physical activity. Can J Public Health. 2015;106(5):e297–e302. doi: 10.17269/cjph.106.4938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chasan-Taber L, Schmidt MD, Pekow P, Sternfeld B, Manson J, Markenson G. Correlates of physical activity in pregnancy among Latina women. Matern Child Health J. 2007;11(4):353–363. doi: 10.1007/s10995-007-0201-8. [DOI] [PubMed] [Google Scholar]
- 53.Ning Y, Williams MA, Dempsey JC, Sorensen TK, Frederick IO, Luthy DA. Correlates of recreational physical activity in early pregnancy. J Matern Fetal Neonatal Med. 2003;13(6):385–393. doi: 10.1080/jmf.13.6.385.393. [DOI] [PubMed] [Google Scholar]
- 54.Pepe MS, Janes H, Longton G, Leisenring W, Newcomb P. Limitations of the odds ratio in gauging the performance of a diagnostic, prognostic, or screening marker. Am J Epidemiol. 2004;159(9):882–890. doi: 10.1093/aje/kwh101. [DOI] [PubMed] [Google Scholar]
- 55.Krasnik A. Categorizations of migrants and ethnic minorities-are they useful for decisions on public health interventions? Eur J Public Health. 2015 doi: 10.1093/eurpub/ckv177. [DOI] [PubMed] [Google Scholar]
- 56.Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc. 2010;42(11):2134–2140. doi: 10.1249/MSS.0b013e3181e0b3ff. [DOI] [PubMed] [Google Scholar]
- 57.Nilsen RM, Vollset SE, Gjessing HK, Skjaerven R, Melve KK, Schreuder P, Alsaker ER, Haug K, Daltveit AK, Magnus P. Self-selection and bias in a large prospective pregnancy cohort in Norway. Paediatr Perinat Epidemiol. 2009;23(6):597–608. doi: 10.1111/j.1365-3016.2009.01062.x. [DOI] [PubMed] [Google Scholar]
- 58.Vernillo G, Savoldelli A, Pellegrini B, Schena F. Validity of the SenseWear Armband to assess energy expenditure in graded walking. J Phys Act Health. 2015;12(2):178–183. doi: 10.1123/jpah.2013-0437. [DOI] [PubMed] [Google Scholar]
- 59.Herrmann SD, Barreira TV, Kang M, Ainsworth BE. Impact of accelerometer wear time on physical activity data: a NHANES semisimulation data approach. Br J Sports Med. 2014;48(3):278–282. doi: 10.1136/bjsports-2012-091410. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions and patient confidentiality, not all data can be made publicly available. Data are available upon request from the Medical Faculty at the University of Oslo for researchers who meet the criteria for access to confidential data. Access can be arranged by direct request to co-author Anne Karen Jenum (a.k.jenum@medisin.uio.no).


