Abstract
The current study examined the relation between parental expressed emotion (EE) and treatment outcome among adolescents participating in a treatment study for adolescent anorexia nervosa, as well as its impact on family functioning. One hundred and twenty-one families were assigned to family-based treatment or adolescent-focused therapy. Paternal criticism predicted lesser improvement in eating disorder psychopathology at end of treatment. There was also a significant interaction between maternal hostility and treatment, indicating that adolescents whose mothers displayed hostility had greater increases in percent of expected body weight in adolescent-focused therapy than family-based treatment. In addition, maternal hostility predicted less improvement in general family functioning and family communication at the end of treatment. Findings suggest that maternal and paternal EE may differentially impact treatment outcome and should be directly attended to in clinical settings. Future research is needed to further explore ways in which parental EE can be effectively modified in treatment.
Keywords: anorexia nervosa, expressed emotion, family functioning, adolescents
Anorexia nervosa (AN) is associated with elevated mortality rates (Arcelus, Mitchell, Wales, & Nielsen, 2011) and serious medical complications (Katzman, 2005). Unfortunately, only about half of adolescents who receive treatment for AN achieve full remission (Lock et al., 2010), and few factors have been found to predict outcome (Le Grange et al., 2012). Furthermore, many predictors of outcome that have been identified (i.e. prior hospitalization, age, and duration of illness) are not modifiable and therefore do not provide possible treatment targets (Le Grange et al., 2012).
The role of the family in the treatment of eating disorders has been a matter of clinical interest for some time, and some of these factors may be modifiable. Indeed, older theories about the aetiology and treatment of AN viewed the illness as a maladaptive attempt by the patient to separate from an overinvolved family (Minuchin, Rosman, & Baker, 1978) and sometimes advocated for the exclusion of parents from treatment to increase adolescent autonomy (Harper, 1983). In contrast, current theories view impairments in family functioning as a consequence of AN, rather than a cause, and parents are appreciated as an important resource in treatment for adolescents (Eisler, 2005). Unfortunately, however, little is known about how particular family characteristics might moderate the impact of family involvement on adolescent outcome. Therefore, understanding the emotional health and functioning of families is important.
Expressed emotion (EE) is one useful way to assess the emotional health of families who are coping with illness. Specifically, EE measures a relative’s attitudes and behaviours towards an ill family member in five areas (i.e. critical comments, hostility, emotional overinvolvement, positive remarks, and warmth; Brown, Birley, & Wing, 1972). By definition, families with high EE make more critical comments, express more hostility, and/or engage in overprotection or self-sacrifice (i.e. emotional overinvolvement) towards the ill patient. Families who score above certain cut-offs on these three components are considered high on EE, whereas those who do not are classified as low on EE (Leff & Vaughn, 1985). Because of this, research on EE has historically focused primarily on the ‘negative’ aspects of EE, although recent research has examined the five components separately to also focus on the ‘positive’ aspects of EE (Le Grange, Hoste, Lock, & Bryson, 2011).
Expressed emotion has been shown to impact treatment outcome for patients with a variety of psychiatric and physical illnesses. In families of patients with schizophrenia and depression, level of EE has been found to be a robust predictor of relapse (Butzlaff & Hooley, 1998). In families of patients with AN, high parental EE has been associated with treatment dropout and poor treatment outcome (Le Grange, Eisler, Dare, & Hodes, 1992; Szmukler, Eisler, Russell, & Dare, 1985), with some studies finding a particularly important role for maternal criticism (Eisler, Simic, Russell, & Dare, 2007; van Furth et al., 1996), whereas parental warmth has been found to predict good treatment outcome (Le Grange et al., 2011). In adult women with eating disorders, parental criticism is stressful and associated with worse eating disorder symptomatology (Medina-Pradas, Navarro, Lopez, Grau, & Obiols, 2011). In spite of the fact that families of patients with eating disorders have lower rates of high EE than those with schizophrenia (Vaughn & Leff, 1976a), EE nevertheless seems to play an important role in eating disorder treatment.
Therefore, EE may be one potentially modifiable treatment target. High parental EE is associated with parental anxiety and depression among patients with eating disorders (Duclos et al., 2014; Kyriacou, Treasure, & Schmidt, 2008; Zabala, Macdonald, & Treasure, 2009), but very little is known about how EE relates with general familial factors, particularly in adolescents with eating disorders. In families of adults with bulimia nervosa, those who were high on EE had more family conflict and less organization (Hedlund, Fichter, Quadflieg, & Brandl, 2003). In families of patients with other psychiatric disorders, those high on EE rated themselves as less cohesive and less adaptive; high EE was also associated with higher levels of family conflict and achievement orientation for mothers but not for fathers (Hibbs, Hamburger, Kruesi, & Lenane, 1993; Sullivan & Miklowitz, 2010). To our knowledge, however, familial factors associated with parental EE have not been examined among adolescents with AN. Given its significant role in both adult and adolescent psychopathology, a better understanding of factors associated with EE and its impact on treatment would be useful. Should EE be associated with treatment outcome in adolescents with AN, leveraging this potentially modifiable characteristic may help to improve outcome.
Although EE has been recognized as an influential factor in mental illness for many years, the mechanisms through which EE impacts relapse and course of treatment are not well understood, leading some to refer to EE as a ‘black box’ (Jenkins & Karno, 1992, p. 10). EE is not a measure of general family functioning, but rather the emotional and behavioural response of a relative to a family member’s illness. EE has been primarily studied among families of adults with schizophrenia, but there is evidence that relatives with high EE tend to have higher expectations of patients and may become more frustrated and controlling when patients do not live up to their expectations (Hooley, 2007), whereas those with low EE tend to believe that undesirable symptoms result from a genuine disorder that is not under the patient’s control (Barrowclough & Hooley, 2003; Leff & Vaughn, 1985). More recently, it has been proposed that high EE is a form of ‘toxic family stress’ (Peris & Miklowitz, 2015), which adds to the existing stress of a psychiatric illness. Negative parental reactions to the illness can create a cycle of negative parent–child interactions that may interfere with successful treatment. Improving negative family interactions associated with EE may improve the prognosis of children struggling with a mental illness, although little is known about the possible problematic family interactions associated with EE in eating disorders.
One purpose of the current study is to add to the very limited knowledge of family interactions associated with EE among adolescents with AN. Patients were drawn from a larger treatment study comparing two forms of treatment for adolescent AN: family-based therapy (FBT) and individual adolescent-focused therapy (AFT; Lock et al., 2010). Ciao, Accurso, Fitzsimmons-Craft, Lock, and Le Grange (2015) examined changes in family functioning in this study and found that FBT, when compared with AFT, was associated with some improvement in communication and behaviour control from baseline to end of treatment. Although high EE was not found to predict or moderate the effect of treatment on full remission from AN (Le Grange et al., 2012), it is unknown how the subcomponents of EE might differentially impact the two main facets of treatment outcome (i.e. weight gain and improvement in eating disorder psychopathology). Previous studies have found that perceived parental EE is related to psychological change but not changes in body mass index (Moulds et al., 2000), suggesting that it is worthwhile to examine these two facets of treatment outcome separately. In addition, the current study examined mothers and fathers separately, as previous studies have found differences in maternal and paternal EE in regard to their relation to treatment outcome (e.g. van Furth et al., 1996). Finally, in addition to summary EE scores, the current study also examined the five EE components separately, rather than only categorizing families as high EE versus low EE, in order to determine whether the separate EE components differentially impact treatment outcome.
The primary aim of the current study was to determine whether parental EE at baseline predicted weight gain or eating disorder psychopathology severity at end of treatment. It was hypothesized that high parental EE at baseline would predict lesser weight gain and lesser psychological improvement for families receiving FBT but not AFT, given parents’ significant role in the recovery process in FBT. A secondary aim of the current study was to examine the relation between EE and adolescent-reported family functioning, in order to identify possible problematic parental behaviours associated with poorer family functioning at end of treatment. We hypothesized that maternal criticism and hostility would be associated with worse family functioning at end of treatment, regardless of treatment type.
Method
Participants
Participants were 121 adolescents and their families taking part in a multisite treatment study for AN at The University of Chicago and Stanford University (Lock et al., 2010). Eligible participants were between the ages of 12 and 18, lived with a parent or legal guardian, and met DSM-IV (APA, 1994) criteria for AN, not including the amenorrhea criterion. Independent assessors not involved in treatment delivery conducted all assessments, including a diagnostic assessment to ensure that participants met diagnostic criteria. Patients were randomly assigned to 24 hours of either FBT (Lock, Le Grange, Agras, & Dare, 2001) or AFT (Fitzpatrick, Moye, Hoste, Lock, & Le Grange, 2010; Robin et al., 1999) over 12 months.
Treatments
Family-based therapy empowers parents to take charge of the recovery process and disrupt eating disordered behaviours (Lock & Le Grange, 2013). In the first of three phases, parents are given responsibility for choosing and monitoring their child’s meals and snacks in an effort to promote rapid weight restoration. As the patient’s weight increases and resistance to eating improves, responsibility over eating is gradually handed back to the adolescent in phase 2. During the final phase, problem solving of general adolescent developmental issues is reviewed.
In contrast to FBT, AFT puts the adolescent in charge of recovery (Fitzpatrick et al., 2010). AFT focuses on increasing patients’ ego strength and coping skills and aiding them in developing increased autonomy. In addition to weight gain, the first phase focuses on developing an understanding of the ways in which AN helps the adolescent manage developmental challenges. The second phase encourages exploration of adolescent issues and aids the adolescent in identifying and tolerating emotions, and the third phase focuses on generalization of skills learned during treatment and issues of termination.
Procedure
Assessments were conducted at four time points: baseline, end of treatment, and 6- and 12-month follow-ups. Assessors were not involved in treatment delivery. Diagnostic interviews were conducted to assess eating disorder and comorbid psychopathology. Families completed the Standardized Clinical Family Interview (SCFI; Kinston & Loader, 1984), from which EE ratings were made, only at baseline. Families completed the Family Assessment Device (FAD; Epstein, Baldwin, & Bishop, 1983), a self-report measure of family functioning, at baseline and end of treatment. Full remission was defined in the primary outcome paper as reaching at least 95% of expected body weight for sex, age, and height, and global scores on the Eating Disorders Examination within one standard deviation (SD) of published norms (Lock et al., 2010). The study was approved by the Institutional Review Boards of The University of Chicago and Stanford University.
Measures
Standardized Clinical Family Interview (Kinston & Loader, 1984)
The SCFI, which was administered at baseline by trained assessors, is a structured interview in which all family members are interviewed together. It includes general questions about family life, including similarities and differences between family members, time spent together, roles and responsibilities in the household, discipline, conflict, decision making, and the family’s involvement with extended family and their community. EE ratings were made from the videotaped SCFI interviews by trained raters (R. R. and D. L. G.). Interrater reliability was established at 0.80. Although the Camberwell Family Interview (CFI; Vaughn & Leff, 1976b) has historically been used to assess EE in families of patients with schizophrenia and eating disorders (e.g. van Furth et al., 1996), the SCFI was chosen because it is more efficient in administration and scoring, and it correlates well with the CFI (Hodes, Dare, Dodge, & Eisler, 1999).
The SCFI yields five EE dimensions, which are rated as follows: critical comments and positive remarks are frequency counts. Hostility is a global scale, meaning that the entirety of the individual’s responses in the interview is considered prior to making a rating. Hostility is rated from 0 to 3 and is defined as generalization of criticism about the patient, rejection of the patient, or both. Emotional overinvolvement is a global scale rated from 0 to 5 (higher scores indicate more emotional overinvolvement and includes overprotective or self-sacrificing behaviours by the parent or extreme emotional responses towards the patient or in the interview). Warmth is a global scale rated from 0 to 5 (higher scores indicate more warmth) and is based on a parent’s tone of voice when talking about or interacting with the patient, as well as sympathy for and interest in the patient.
Eating Disorder Examination (Cooper & Fairburn, 1987)
The Eating Disorder Examination (EDE) is a semi-structured interview designed to assess the behavioural and cognitive psycho-pathology associated with eating disorders. EDE global score was used in this study as a measure of overall eating disorder pathology. This interview was conducted at both baseline and end of treatment. Higher scores indicate more severe pathology.
Family Assessment Device (Epstein, Baldwin, & Bishop, 1983; Kabacoff, Miller, Bishop, Epstein, & Keitner, 1990)
The FAD is a self-report measure of family functioning made up of seven subscales: problem solving (e.g. ‘We try to think of different ways to solve problems’), communication (e.g. ‘When someone is upset the others know why’), roles (e.g. ‘We make sure members meet their family responsibilities’), affective responsiveness (e.g. ‘We are reluctant to show our affection for each other’), affective involvement (e.g. ‘If someone is in trouble, the others become too involved’), behaviour control (e.g. ‘You can easily get away with breaking the rules’), and general functioning (e.g. ‘Individuals are accepted for what they are’). Adolescent report of family functioning was used in this study. Given that we were examining the impact of EE on the patient, the adolescents’ perspective on family functioning seemed to be most relevant, and previous research suggests that this perspective is most strongly predictive of treatment outcome (Ciao et al., 2015). Items are scored from 1 (strongly agree) to 4 (strongly disagree), and higher scores on this measure indicate greater impairment in functioning. Internal consistencies for all subscale scores in the current sample were acceptable (α coefficients ranging from .67 for Roles to .90 for General Functioning). Adolescents completed the FAD at baseline and end of treatment.
Data analysis
High EE was defined as the presence of any critical comments or hostility, or an emotional overinvolvement score of 3 or higher for at least one parent (Le Grange et al., 2011; Leff & Vaughn, 1985). Because EE subscale distributions were positively skewed, data were recoded to indicate presence (0) or absence (=0) of each of the ratings for the purposes of this study. The presence/absence of critical comments, hostility, emotional overinvolvement, positive remarks, and warmth (EE subscales) were examined as predictors of adolescent outcome, separately by parent (mother or father). Separate linear regression models were used to examine the effect of each EE subscale (mother or father) on two outcomes: percent of expected body weight and level of eating disorder psychopathology (i.e. global EDE score), controlling for the baseline value of the outcome. Models also included the main effect for treatment and the interaction between treatment and EE. EE subscales and treatment were centred as −0.5 and 0.5. All available data were used for analysis.
Additionally, multiple stepwise regressions were used to examine the relationship between EE and self-reported family functioning (Aim 1), with each of five EE subscales (i.e. critical comments, hostility, emotional overinvolvement, positive remarks, and warmth) for both mothers and fathers as dichotomous (present vs. absent) predictors and each aspect of family functioning (FAD subscales) at end of treatment as individual outcomes, controlling for baseline family functioning, baseline eating disorder psychopathology, and treatment. EE subscale scores with significance values p <.05 were retained in each of the final multivariable models. To correct for the use of multiple comparisons, p <.01 was used as the significance threshold across all analyses, given that the Bonferroni correction has been criticized for being too conservative (e.g. Perneger, 1998).
Results
Patients were primarily female (91.8%) with a mean age of 14.4 (SD = 1.6), a duration of illness of 12.2 months (SD = 12.0), and a percent of expected body weight at baseline of 80.4 (SD = 3.6). The majority were characterized by restricting type (82.6%, n = 100) rather than binge/purge type (17.4%, n = 21). The majority (79.1%) came from intact families and were White (75.4%). Twelve families (10.9%) were Asian, eight (7.3%) were Hispanic, one (0.9%) was Black, and six (5.5%) identified as ‘other’. Of the 121 families, 110 had at least one parent who completed the SCFI at baseline, including 106 (87.6%) mothers and 91 (75.2%) fathers. One hundred four (86.0%) and 103 (85.1%) adolescents had outcome data at the end of treatment for expected body weight and eating disorder psychopathology, respectively, but only 97 of those had a baseline EE rating. There were no differences in maternal or paternal EE ratings between patients with end of treatment data (ns = 94 and 81) and those with missing data at end of treatment owing to lack of study assessment completion (ns = 12 and 10; ps >.05).
Families with mothers who made critical comments were more likely to drop out of treatment (45.0% vs. 16.3%; χ2 = 7.878, p = .005) than those with no maternal criticism. There were no other differences in maternal EE ratings between patients who dropped out of treatment (n = 23) and those who did not (n = 83; ps >.01). There were no differences in paternal EE ratings between patients who dropped out of treatment (n = 17) and those who did not (n = 74; ps >.01). Drop-out rates did not differ by treatment (14.8% in FBT vs. 5.0% in AFT; χ2 = 3.221, p = .073). Finally, t-tests demonstrated no differences between families with any EE versus no EE with respect to baseline percent of expected body weight (ps >.01) or global EDE score (ps >.01). All results are presented in Table 1.
Table 1.
Parental expressed emotion and treatment outcome
| Dropout
|
Percent of expected body weight
|
EDE global
|
|||||
|---|---|---|---|---|---|---|---|
| χ2 | p | t | p | t | p | ||
| Critical comments | Mother | 7.878 | .005 | 0.171 | .864 | −2.230 | .028 |
| Father | 0.021 | .886 | 0.213 | .831 | −1.320 | .190 | |
| Hostility | Mother | 0.856 | .355 | −0.268 | .790 | −0.673 | .502 |
| Father | 1.32 | .251 | −0.131 | .896 | −2.227 | .028 | |
| Emotional overinvolvement | Mother | 0.449 | .503 | 1.605 | .111 | −2.470 | .015 |
| Father | 0.007 | .932 | 0.840 | .398 | −0.180 | .859 | |
| Positive remarks | Mother | 2.587 | .108 | −0.405 | .686 | 0.263 | .793 |
| Father | 0.014 | .906 | −1.048 | .297 | −1.859 | .066 | |
| Warmth | Mother | 0.720 | .396 | −1.445 | .152 | −1.022 | .309 |
| Father | 1.272 | .259 | −1.528 | .130 | 1.085 | .281 | |
Note: EDE = Eating Disorder Examination.
Parental expressed emotion and treatment outcome
Rates of high EE were relatively low, with less than a third (n = 32, 29.1%) of families having at least one parent with high EE. Table 2 shows EE scores for each parent by subscale. The presence of hostility in mothers and fathers was least common, followed by critical comments and emotional overinvolvement. The presence of positive remarks and expressions of warmth in mothers and fathers was relatively common.
Table 2.
Expressed emotion subscales for fathers (n = 91) and mothers (n = 106) at baseline
| Subscale | Parent | Present vs. absent (n, %) | Mean | SD | Median | Range |
|---|---|---|---|---|---|---|
| CC | Father | 15 (16.5%) | 0.26 | 0.77 | 0 | 0–5 |
| Mother | 20 (18.9%) | 0.50 | 1.7 | 0 | 0–14 | |
| EOI | Father | 26 (28.6%) | 0.35 | 0.62 | 0 | 0–3 |
| Mother | 48 (45.3%) | 0.68 | 0.89 | 0 | 0–4 | |
| H | Father | 2 (2.2%) | 0.03 | 0.23 | 0 | 0–2 |
| Mother | 3 (2.8%) | 0.03 | 0.17 | 0 | 0–1 | |
| PR | Father | 44 (48.4%) | 0.84 | 1.17 | 0 | 0–6 |
| Mother | 73 (68.9%) | 1.61 | 1.81 | 1 | 0–11 | |
| W | Father | 71 (78.0%) | 1.66 | 1.3 | 2 | 0–5 |
| Mother | 91 (85.8%) | 2.05 | 1.36 | 2 | 0–5 |
Note: CC = critical comments; EOI = emotional overinvolvement; H = hostility; PR = positive remarks; W = warmth.
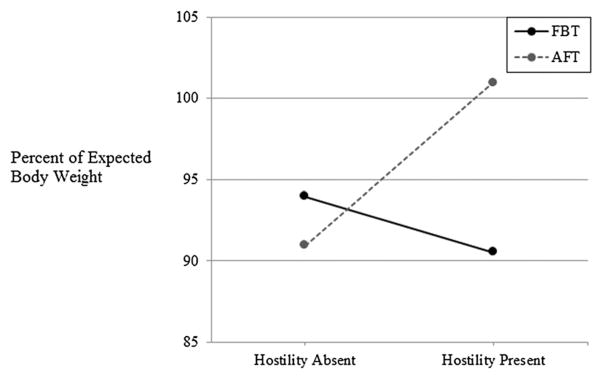
At the end of treatment, adolescents (n = 104) had a mean expected body weight of 91.76 (SD = 9.86, range: [69.30, 121.59]). After controlling for percent of expected body weight at baseline, there was a significant treatment × maternal hostility interaction (B = −44.134, SE = 11.382, p = .0002). For adolescents whose mothers displayed hostility, those in AFT had greater increases in percent of expected body weight than those in FBT, whereas treatment did not moderate the effect of maternal hostility on body weight outcome at the end of treatment (Figure 1). None of the remaining maternal EE sub-scales predicted improved percent of expected body weight at the end of treatment (ps >.01). None of the paternal EE sub-scales significantly predicted improved percent of expected body weight at the end of treatment (ps >.01). Table 3 presents each of the linear regression models examining maternal and paternal EE as predictors of outcome.
Figure 1.
The impact of maternal hostility on weight restoration by treatment
Table 3.
Linear regression models examining the impact of expressed emotion on adolescents’ outcomes at the end of treatment
| Critical comments
|
Hostility
|
Emotional overinvolvement
|
Positive remarks
|
Warmth
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | |
| Percent of expected body weight | |||||||||||||||
| %EBW at baseline | 0.850 | 0.273 | .002 | 0.899 | 0.253 | .001 | 0.954 | 0.275 | .001 | 0.891 | 0.274 | .002 | 0.854 | 0.268 | .002 |
| Treatment | 0.407 | 2.494 | .871 | −18.324 | 5.708 | .002 | 2.308 | 1.948 | .239 | 1.920 | 2.129 | .370 | −0.476 | 2.725 | .862 |
| EE subscale (mother) | −1.881 | 2.488 | .452 | −1.719 | 5.694 | .763 | 2.764 | 1.944 | .158 | 1.928 | 2.095 | .360 | 6.655 | 2.686 | .015 |
| Treatment × EE subscale (mother) | −6.610 | 4.997 | .189 | −44.134 | 11.382 | .0002 | −2.604 | 3.840 | .499 | 2.488 | 4.202 | .555 | 8.308 | 5.378 | .126 |
| %EBW at baseline | 0.893 | 0.290 | .003 | 0.886 | 0.295 | .004 | 1.006 | 0.287 | .001 | 0.832 | 0.291 | .006 | 0.853 | 0.300 | .006 |
| Treatment | −0.993 | 2.780 | .722 | 2.416 | 2.133 | .261 | 0.085 | 2.261 | .970 | 2.200 | 2.079 | .293 | 2.314 | 2.574 | .372 |
| EE subscale (father) | 1.288 | 2.754 | .641 | 3.155 | 7.167 | .661 | 3.977 | 2.225 | .078 | 3.624 | 2.062 | .083 | 1.777 | 2.592 | .495 |
| Treatment × EE subscale (father) | −10.621 | 5.508 | .058 | Not estimated | −9.949 | 4.454 | .028 | −3.830 | 4.104 | .354 | 0.475 | 5.134 | .927 | ||
| Eating disorder psychopathology | |||||||||||||||
| EDE at baseline | 0.334 | 0.073 | .001 | 0.369 | 0.073 | .001 | 0.371 | 0.075 | .001 | 0.362 | 0.074 | .001 | 0.374 | 0.074 | .001 |
| Treatment | −0.643 | 0.268 | .018 | −0.018 | 0.665 | .979 | −0.428 | 0.212 | .046 | −0.361 | 0.227 | .116 | −0.262 | 0.304 | .390 |
| EE subscale (mother) | 0.402 | 0.267 | .135 | 0.723 | 0.658 | .275 | 0.052 | 0.214 | .810 | 0.056 | 0.225 | .805 | −0.052 | 0.299 | .861 |
| Treatment × EE subscale (mother) | −0.772 | 0.527 | .146 | 0.803 | 1.321 | .545 | −0.401 | 0.417 | .339 | −0.302 | 0.456 | .509 | −0.400 | 0.597 | .505 |
| EDE at baseline | 0.332 | 0.073 | .001 | 0.403 | 0.080 | .001 | 0.360 | 0.079 | .001 | 0.359 | 0.081 | .001 | 0.340 | 0.084 | .001 |
| Treatment | −0.635 | 0.281 | .027 | −0.335 | 0.229 | .148 | −0.513 | 0.253 | .046 | −0.428 | 0.231 | .068 | −0.575 | 0.292 | .052 |
| EE subscale (father) | 0.999 | 0.280 | .0006 | −1.233 | 0.786 | .121 | 0.292 | 0.246 | .239 | 0.120 | 0.231 | .604 | −0.053 | 0.274 | .846 |
| Treatment × EE subscale (father) | −0.663 | 0.555 | .236 | Not estimated | −0.388 | 0.495 | .435 | −0.077 | 0.452 | .865 | 0.548 | 0.580 | .348 | ||
Note: Effects for the treatment × paternal hostility interaction could not be estimated owing to problems with multicollinearity.
EBW = expected body weight; EE = expressed emotion; EDE = Eating Disorder Examination.
At the end of treatment, adolescents (n = 103) had a mean EDE global score of 0.93 (SD = 1.16, range: [0.00, 4.89]). None of the maternal EE subscales significantly predicted improved eating disorder psychopathology at the end of treatment (ps >.01). For paternal EE, the presence of critical comments significantly predicted less improvement in eating disorder psychopathology at end of treatment (B = 0.999, SE = 0.280, p = .0006), after controlling for eating disorder psychopathology at baseline. This effect indicated that the presence of paternal criticism at baseline predicted less improvement in eating disorder psychopathology. None of the remaining paternal EE subscales predicted improved eating disorder psychopathology at end of treatment (ps >.01).
Parental expressed emotion and family functioning
Maternal hostility significantly predicted level of general family functioning and family communication at the end of treatment, after controlling for baseline family functioning, baseline eating disorder psychopathology, and treatment. However, no other facet of maternal or paternal EE significantly predicted other aspects of family functioning at the end of treatment, including affective response, affective involvement, roles, behaviour control, or problem solving (ps >.01; Table 4).
Table 4.
Linear regression models examining the impact of expressed emotion on family functioning at the end of treatment
| Global functioning
|
Communication
|
Affective response
|
Affective involvement
|
Roles
|
Behaviour control
|
Problem solving
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | B | SE | p | |
| FAD subscale at baseline | 0.639 | 0.095 | .001 | 0.739 | 0.118 | .001 | 0.786 | 0.119 | .001 | 0.600 | 0.094 | .3001 | 0.874 | 0.117 | .001 | 0.587 | 0.102 | .001 | 0.481 | 0.125 | .001 |
| EDE at baseline | −0.012 | 0.038 | .759 | −0.028 | 0.031 | .371 | −0.033 | 0.041 | .421 | −0.011 | 0.034 | .752 | 0.017 | 0.026 | .506 | 0.007 | 0.029 | .807 | 0.014 | 0.039 | .730 |
| Treatment | −0.206 | 0.108 | .059 | −0.178 | 0.086 | .042 | −0.078 | 0.120 | .515 | −0.079 | 0.098 | .422 | −0.180 | 0.074 | .017 | −0.145 | 0.082 | .080 | −0.046 | 0.115 | .688 |
| Maternal hostility | 0.995 | 0.317 | .003 | 0.831 | 0.262 | .002 | 0.897 | 0.352 | .013 | – | – | – | – | – | – | – | – | – | – | – | – |
| Maternal warmth | – | – | – | 0.296 | 0.124 | .020 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
Note: FAD = Family Assessment Device; EDE = Eating Disorder Examination.
General family functioning
The overall model for general family functioning was significant and accounted for almost one half of the variance in this outcome, F(4, 69) = 16.248, p <.0001, R2 = .485. Maternal hostility significantly predicted worse family functioning at the end of treatment (B = 0.995, SE = 0.317, p = .003).
Family communication
The overall model for family communication was significant and accounted for approximately two fifths of the variance in this outcome, F(5, 73) = 10.109, p <.0001, R2 = .426. Maternal hostility (B = 0.831, SE = 0.262 p = .002) predicted significantly more impaired family communication at the end of treatment.
Discussion
The purpose of the current study was to examine whether parental EE at baseline predicted adolescent treatment outcome among families participating in a treatment study for adolescent AN, as well as to explore the relation between EE and adolescent-reported family functioning. In contrast to previous studies finding that high EE predicted poor treatment outcome (Eisler et al., 2007; Le Grange et al., 1992; van Furth et al., 1996), there were no main effects of maternal or paternal hostility, emotional overinvolvement, positive remarks, or warmth on either improvement in percent of expected body weight or eating disorder psychopathology. However, paternal (but not maternal) criticism did predict significantly less improvement in eating disorder psychopathology at the end of treatment, suggesting that fathers who express criticism may hinder adolescent improvement in eating disorder cognitions and behaviours.
Finding that lower paternal criticism was related to psychological improvement but not weight restoration is in keeping with a previous study of hospitalized patients with AN, which found that perceived family EE was not related to change in body mass index but was related to psychological functioning (Moulds et al., 2000). The reason that cognitive change may be more likely to occur for children of fathers with low levels of criticism is an area in need of further exploration; however, there is a large body of research indicating that the quality of parent–child relationships and attachment is related to cognitive and behavioural development in children (Moretti & Peled, 2004). It is possible that families with low EE provide an environment that facilitates healthy cognitive change, whereas this change is more difficult in families with high EE. Nevertheless, families appear to be able to provide structural support around specific behaviours (e.g. efforts towards weight gain) regardless of level of EE. Previous studies have found that maternal criticism can impact treatment outcome (van Furth et al., 1996); thus, it is surprising that maternal criticism did not also predict outcome in the current study, although it was related to treatment dropout. Taken together, however, these findings suggest the importance of addressing the presence of any criticism in either parent across treatments.
An interaction of maternal hostility with treatment was found, which indicated that for adolescents whose mothers expressed any hostility, AFT was associated with greater gains in percent of expected body weight compared with FBT. This finding was significant in spite of the extremely low prevalence (~3%) of hostility in mothers, suggesting that it is a potent predictor of outcome, although it will not often be present. Weight restoration is a primary goal in both AFT and FBT, although in FBT, parents are the main agents of change, whereas in AFT, the main responsibility for weight gain falls to the patient. Although FBT seeks to reduce parental criticism and hostility in order to improve treatment outcome, these results suggest that individual treatment might be advantageous with respect to weight when maternal hostility is present. These findings should be replicated but may have important treatment implications in regard to choosing appropriate treatments for families. Adolescents with mothers displaying hostility may be better off in individual therapy; alternatively, it is possible that these families could still do well in FBT with additional interventions designed to reduce maternal hostility. Importantly, however, there were no differences in improvements in eating disorder psychopathology by maternal hostility, and remission rates were not impacted by high EE. This is consistent with a previous analysis finding that EE emerged as neither a predictor nor a moderator of treatment outcome (i.e. remission) in FBT or AFT (Le Grange et al., 2012).
In addition, maternal hostility emerged as a unique predictor of change in family functioning across treatments. Both general family functioning and family communication were better at the end of treatment for families whose mothers expressed no hostility. The importance of maternal hostility has been found in previous studies (van Furth et al., 1996). Unlike the effect of maternal hostility on weight restoration, however, the effect of maternal hostility on family functioning emerged across treatments. Contrary to hypotheses, maternal hostility was not related to the majority of family functioning subscales, and maternal criticism did not emerge as a significant predictor. It is somewhat surprising that other aspects of family functioning, such as roles or problem solving, were not related to parental EE, as these topics are specifically addressed in the family interview and can easily lend themselves to expressions of anger or criticism. Findings should be replicated, but these data suggest that some aspects of family interactions are not negatively impacted by high EE, and that families with mothers high on hostility may benefit from additional interventions specifically targeted at improving family communication.
Differences between this study and previous studies finding that EE is related to treatment outcome (Le Grange, Eisler, Dare, & Hodes, 1992; Szmukler, Eisler, Russell, & Dare, 1985; van Furth et al., 1996) may be due to a higher threshold for recovery set in this study (Lock et al., 2010), or may be due in part to limited variability due to floor effects; the rates of all five EE dimensions were very low in this group. The low levels of high EE in this study are consistent with other studies of families of adolescents with AN (Le Grange et al., 2011) and remain well below rates found in studies of patients with schizophrenia (Vaughn & Leff, 1976a).
The study had several limitations. Not all parents completed the EE interview, and it is possible that those who did not complete it were higher on EE than those who did. Future studies should also examine multiple reporters of family functioning. Adolescents’ self-report, although found to be predictive of treatment outcome (Ciao et al., 2015), likely assesses a combination of subjective perception and objective family functioning. There was also not a measure of adolescents’ perception of their parents’ level of EE; it is possible that this is just as important as actual parental EE.
Parents who are low on EE differ from those high on EE in the extent to which they view a disorder as legitimate, and the degree to which they express empathy for the person suffering from the illness (Leff & Vaughn, 1985). This may be particularly relevant for parents of patients with AN, who may not immediately understand the disorder or realize that the patient is not simply being wilful or stubborn in his or her reluctance to eat. FBT has been shown to be superior to individual therapy and has been recommended as the first line of treatment for adolescents with AN who are medically stable for outpatient treatment (Couturier, Kimber, & Szatmari, 2013), although the current findings suggest that this may not be true for adolescents with mothers high on hostility. A fundamental tenet of FBT is externalization of the illness, where the family is educated about the nature of eating disorders, and it is explained that patients cannot simply ‘just eat’. Instead, they are in the grip of a powerful disorder that is influencing their behaviours, thoughts, and emotions. The illness is often given a name by the family in an effort to separate the healthy part of the patient from the eating disorder. Parents are reminded that their healthy child is still there, suffering from the disorder, and they should remain compassionate towards their child even in the face of significant resistance from the eating disorder. Thus, the low EE characteristics of viewing the disorder as a legitimate illness and remaining empathic may make parents particularly effective in the context of FBT. It is possible that parents who express hostility have more difficulty separating the illness and the patient, and their children may therefore do better in individual treatment.
Parents are also encouraged to take a noncritical stance towards the patient, which can be facilitated by successfully conceptually separating the patient from the illness. Providing psychoeducation around the treatment implications of parental criticism in treatment can be useful in helping parents to moderate critical feelings they may be experiencing. The current findings can also be shared with parents to emphasize that even low levels of criticism may be harmful to the recovery of a patient with AN.
Although parental EE was not found to be related to achieving full remission or 95% of expected body weight, the current findings suggest that even at low levels, parental EE may influence eating-related cognitions for adolescents with AN and impact family functioning. Therapists should continue to attend to parental EE in treatment and emphasize the importance of creating an environment that may facilitate cognitive improvement.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Barrowclough C, Hooley JM. Attributions and expressed emotion: A review. Clinical Psychology Review. 2003;23:849–880. doi: 10.1016/s0272-7358(03)00075-8. [DOI] [PubMed] [Google Scholar]
- Brown GW, Birley JL, Wing JK. Influence of family life on the course of schizophrenic disorders: A replication. British Journal of Psychiatry. 1972;121:241–258. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse: A meta-analysis. Archives of General Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Ciao AC, Accurso EC, Fitzsimmons-Craft EE, Lock J, Le Grange D. Family functioning in two treatments for adolescent anorexia nervosa. International Journal of Eating Disorders. 2015;48:81–90. doi: 10.1002/eat.22314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Z, Fairburn CG. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6:1–8. [Google Scholar]
- Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders. 2013;46:3–11. doi: 10.1002/eat.22042. [DOI] [PubMed] [Google Scholar]
- Duclos J, Dorard G, Berthoz S, Curt F, Faucher S, Falissard B, Godart N. Expressed emotion in anorexia nervosa: What is inside the “black box”? Comprehensive Psychiatry. 2014;55:71–79. doi: 10.1016/j.comppsych.2013.10.002. [DOI] [PubMed] [Google Scholar]
- Eisler I. The empirical and theoretical base of family therapy and multiple family day therapy for adolescent anorexia nervosa. Journal of Family Therapy. 2005;27:104–131. [Google Scholar]
- Eisler I, Simic M, Russell G, Dare C. A randomized controlled trial of two forms of family therapy in adolescent anorexia nervosa: A five-year follow-up. Journal of Child Psychology and Psychiatry. 2007;48:552–560. doi: 10.1111/j.1469-7610.2007.01726.x. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Fitzpatrick KK, Moye A, Hoste R, Lock J, Le Grange D. Adolescent focused psychotherapy for adolescents with anorexia nervosa. Journal of Contemporary Psychotherapy. 2010;40:31–39. [Google Scholar]
- Harper G. Varieties of parenting failure in anorexia nervosa: Protection and parentectomy. Journal of the American Academy of Child and Adolescent Psychiatry. 1983;22:134–139. doi: 10.1016/s0002-7138(09)62326-8. [DOI] [PubMed] [Google Scholar]
- Hedlund S, Fichter MM, Quadflieg N, Brandl C. Expressed emotion, family environment, and parental bonding in bulimia nervosa: A 6-year investigation. Eating and Weight Disorders. 2003;8:26–35. doi: 10.1007/BF03324986. [DOI] [PubMed] [Google Scholar]
- Hibbs ED, Hamburger SD, Kruesi MJP, Lenane M. Factors affecting expressed emotion in parents of ill and normal children. American Journal of Orthopsychiatry. 1993;63:103–112. doi: 10.1037/h0079395. [DOI] [PubMed] [Google Scholar]
- Hodes M, Dare C, Dodge E, Eisler I. The assessment of expressed emotion in a standardized family interview. Journal of Child Psychology and Psychiatry. 1999;40:617–625. [PubMed] [Google Scholar]
- Hooley JM. Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology. 2007;3:329–352. doi: 10.1146/annurev.clinpsy.2.022305.095236. [DOI] [PubMed] [Google Scholar]
- Jenkins JH, Karno M. The meaning of expressed emotion: Theoretical issues raised by cross-cultural research. American Journal of Psychiatry. 1992;149:9–21. doi: 10.1176/ajp.149.1.9. [DOI] [PubMed] [Google Scholar]
- Kabacoff RI, Miller IW, Bishop DS, Epstein NB, Keitner GI. A psychometric study of the McMaster Family Assessment Device in psychiatric, medical, and nonclinical samples. Journal of Family Psychology. 1990;3:431–439. [Google Scholar]
- Katzman DK. Medical complications in adolescents with anorexia nervosa: A review of the literature. International Journal of Eating Disorders. 2005;37:S52–S59. doi: 10.1002/eat.20118. [DOI] [PubMed] [Google Scholar]
- Kinston W, Loader P. Eliciting whole-family interaction with a standardized clinical interview. Journal of Family Therapy. 1984;6:347–363. [Google Scholar]
- Kyriacou O, Treasure J, Schmidt U. Expressed emotion in eating disorders assessed via self-report: An examination of factors associated with expressed emotion in carers of people with anorexia nervosa in comparison to control families. International Journal of Eating Disorders. 2008;41:37–46. doi: 10.1002/eat.20469. [DOI] [PubMed] [Google Scholar]
- Le Grange D, Eisler I, Dare C, Hodes M. Family criticism and self-starvation: A study of expressed emotion. Journal of Family Therapy. 1992;14:177–192. [Google Scholar]
- Le Grange D, Hoste RR, Lock J, Bryson SW. Parental expressed emotion of adolescents with anorexia nervosa: Outcome in family-based treatment. International Journal of Eating Disorders. 2011;44:731–734. doi: 10.1002/eat.20877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Agras WS, Moye An, Bryson SW, Jo B, Kraemer HC. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behaviour Research and Therapy. 2012;50:85–92. doi: 10.1016/j.brat.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff J, Vaughn C. Expressed emotion in families. London: Guilford Press; 1985. [Google Scholar]
- Lock J, Le Grange D. Treatment manual for anorexia nervosa: A family-based approach. 2. New York: Guilford Press; 2013. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Dare C. Treatment manual for anorexia nervosa: A family-based approach. New York: Guilford Press; 2001. [Google Scholar]
- Lock J, Le Grange D, Agras WS, Moye A, Bryson SW, Jo B. Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry. 2010;67:1025–1032. doi: 10.1001/archgenpsychiatry.2010.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Pradas C, Navarro JB, Lopez SR, Grau A, Obiols JE. Dyadic view of expressed emotion, stress, and eating disorder psychopathology. Appetite. 2011;57:743–748. doi: 10.1016/j.appet.2011.08.016. [DOI] [PubMed] [Google Scholar]
- Minuchin S, Rosman BL, Baker L. Psychosomatic families. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- Moretti MM, Peled M. Adolescent-parent attachment: Bonds that support healthy development. Paediatrics & Child Health. 2004;9:551–555. doi: 10.1093/pch/9.8.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulds ML, Touyz SW, Schotte D, Beumont PJV, Griffiths R, Russell J, Charles M. Perceived expressed emotion in the siblings and parents of hospitalized patients with anorexia nervosa. International Journal of Eating Disorders. 2000;27:288–296. doi: 10.1002/(sici)1098-108x(200004)27:3<288::aid-eat5>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Peris TS, Miklowitz DJ. Parental expressed emotion and youth psychopathology: New directions for an old construct. Child Psychiatry and Human Development. 2015 doi: 10.1007/s10578-014-0526-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perneger TV. What’s wrong with Bonferroni adjustments. British Medical Journal. 1998;316:1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1482–1489. doi: 10.1097/00004583-199912000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan AE, Miklowitz DJ. Family functioning among adolescents with bipolar disorder. Journal of Family Therapy. 2010;24:60–67. doi: 10.1037/a0018183. [DOI] [PubMed] [Google Scholar]
- Szmukler GI, Eisler I, Russell GF, Dare C. Anorexia nervosa, parental “expressed emotion” and dropping out of treatment. British Journal of Psychiatry. 1985;147:265–271. doi: 10.1192/bjp.147.3.265. [DOI] [PubMed] [Google Scholar]
- van Furth EF, van Strien DC, Martina LML, van Son MJM, Hendrickx JJP, van Engeland H. Expressed emotion and the prediction of outcome in adolescent eating disorders. International Journal of Eating Disorders. 1996;20:19–31. doi: 10.1002/(SICI)1098-108X(199607)20:1<19::AID-EAT3>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff J. The influence of family and social factors on the course of psychiatric illness: A comparison of schizophrenic and depressed neurotic patients. British Journal of Psychiatry. 1976a;129:125–137. doi: 10.1192/bjp.129.2.125. [DOI] [PubMed] [Google Scholar]
- Vaughn CE, Leff J. The measurement of expressed emotion in the families of psychiatric patients. British Journal of Social and Clinical Psychology. 1976b;15:157–165. doi: 10.1111/j.2044-8260.1976.tb00021.x. [DOI] [PubMed] [Google Scholar]
- Zabala MJ, Macdonald P, Treasure J. Appraisal of caregiving burden, expressed emotion and psychological distress in families of people with eating disorders: A systematic review. European Eating Disorders Review. 2009;17:338–349. doi: 10.1002/erv.925. [DOI] [PubMed] [Google Scholar]