Abstract
Objective
A growing number of asthma patients are using Complementary and Alternative Medicine (CAM). Prior studies have not examined CAM use among the older adult population.
Methods
Data from the 2011 Behavioral Risk Factor Surveillance Survey (BRFSS), a national telephone survey, and the Asthma Call-Back survey (ACBS), a survey conducted among BRFSS individuals reporting asthma, was used for the analyses. The study population consisted of 7685 individuals aged 55 years or older with current asthma. The relationship of CAM use with demographic and asthma outcomes was analyzed using logistic regression.
Results
CAM use was reported by 39% (3030). Breathing techniques were the most commonly reported CAM therapy. Demographic factors associated with CAM use include female gender (OR 1.36, p<0.002), having at least a college education (OR 1.76, p<0.001), cost barrier to healthcare (OR 1.43, p<0.001), and living in the West (OR 1.31, p<0.01). An inverse relationship was noted between income and CAM use. Those who had received an asthma action plan (OR 1.29, p<0.005), current smokers (OR 1.35, p<0.02), or impaired asthma control (as defined by symptoms affecting sleep, symptoms limiting activities, and rescue medication use) were more likely to use CAM (OR 1.37, p<0.001; OR 1.38, p<0.001; and OR 1.2, p<0.046, respectively).
Conclusions
A large proportion of asthmatic older adults use CAM. In addition, older adults with asthma who use CAM have decreased asthma control, and further studies are needed to determine a causal role.
Keywords: Alternative Medicine, Geriatric
Introduction
In the United States, asthma affects an estimated 3.1 million individuals aged 65 and over with an increasing prevalence in recent years.(1) As compared to all adults with asthma, older adults (≥ 65 years) have the highest asthma-related hospitalization and mortality rates. From 2007-2009, the death rate for adult asthmatics aged 65 and older was the highest of all age groups, reaching 5.8 per 10 000 persons with asthma.(1, 2) Older adults with asthma are more likely to have impaired quality of life and a reduction in functional status compared to other adults their age.(3) The elderly population is also at risk for underdiagnosis given multiple comorbidities. A lack of asthma recognition in this age group may contribute to suboptimal treatment and poor outcomes.(3)
Complementary and alternative medicine (CAM) use is defined as “a group of diverse medical and healthcare systems, practices, and products that are not generally considered to be part of conventional medicine” by the NIH National Center for Complementary and Alternative Medicine.(4) A growing number of patients are using CAM with, or instead of, prescribed medications for a variety of chronic diseases. According to the 2007 National Health Interview Survey (NHIS), roughly 4 in 10 adults in the U.S. use some form of CAM.(5) The most commonly reported forms of CAM include acupuncture, aromatherapy, breathing techniques, herbal products, homeopathy, and yoga.(6)
In a review of 12 prior studies assessing CAM use in the adult asthmatic population, the prevalence ranged broadly from 4% to 79%. However, when Slader et al. assessed the quality of the studies more rigorously, the prevalence of adult asthmatics using CAM was estimated between 20% and 30%.(6) The perceived improvement in asthma symptoms with CAM use is generally positive, with many patients reporting superiority of CAM use over conventional medication.(7) Nevertheless, studies have also revealed an association between CAM use and poorer health-related quality of life among adult asthmatics.(8)
The association between age and CAM use among asthmatics is inconsistent. Differing studies have revealed no relationship to age, increased use among middle aged adults, or increased use among younger individuals.(7-13) To our knowledge, there are no studies that have focused exclusively on CAM use in the older adult population with asthma. The aim of this study was to identify the demographic characteristics associated with CAM use, and to assess any associations between CAM use and asthma outcomes in the older adult asthmatic population.
Methods
Data from the 2011 Behavioral Risk Factor Surveillance Survey (BRFSS) and Asthma Call-back survey (ACBS) was used for the analyses. The Behavioral Risk Factor Surveillance Survey (BRFSS) is a cross-sectional random digit dialing telephone survey performed in all 50 states, the District of Columbia, Guam, Puerto Rico, and U.S. Virgin Islands.(14) The 2011 Asthma Call-back survey (ACBS) is an in-depth asthma survey conducted with BRFSS respondents who report a current or prior asthma diagnosis. The ACBS is administered 2 weeks following the BRFSS. The 2011 ACBS included 16 693 subjects from 40 states, the District of Columbia, and Puerto Rico. The survey asks questions to assess the individual's history of asthma, health care utilization, medications, cost of asthma care, comorbid conditions, and CAM use.
This study was restricted to those aged 55 years or older, with current asthma, in an effort to include a greater proportion of the baby boom generation, who were expected to be between 46 and 64 years old in 2010.(15) Current asthma was defined as responding “yes” to the following two questions on the ACBS: “Did a physician ever tell you that you had asthma?” and “Do you still have asthma?” Those with missing data on CAM use were excluded (n=27). This resulted in 7685 respondents for this study.
Outcome Measures
The primary outcome was self-reported CAM use to control asthma over the past 12 months. CAM users were defined as responding “yes” to the use of at least one of the following: herbs, vitamins, acupuncture, acupressure, aromatherapy, homeopathy, reflexology, yoga, breathing techniques, naturopathy, or other alternative care. The frequency and additional specific details of each CAM modality were not included in the ACBS survey. Those who responded “no” to all CAM methods were considered CAM non-users.
The predictor variables were chosen a priori based on previous research.(7, 8, 10-12, 16) These variables included sex, age, BMI, race, education, annual household income, geographic region, impaired access to health care due to cost, lack of or gap in health insurance, ER visit in the past 12 months due to asthma, asthma control, asthma severity, completion of an asthma management plan, asthma duration, smoking history, flu shot status in the past 12 months, and history of physician-diagnosed depression. Comorbid disease, other than depression, was not included as Morgan et al. previously published a study using the BRFSS and ACBS that revealed no relationship of CAM use with comorbid cardiovascular disease, diabetes, and stroke.(12)
Impaired access to health care due to cost was defined as responding “yes” to any of the following questions: “Was there a time in the past 12 months when you needed to see your PCP for your asthma but could not because of cost?,” “Was there a time in the last 12 months when you were referred to a specialist for asthma care but could not go because of cost?,” or “Was there a time in the past 12 months when you needed to buy medication for asthma but could not because of cost?” Lack of health insurance was defined as responding “no” to “Do you have any kind of health care coverage, including health insurance prepaid plans such as HMOs, or government plans such as Medicare or Medicaid?” or “yes” to “During the past 12 months was there any time that you did not have any health insurance or coverage?”
The responses to asthma impairment measures, including frequency of symptoms, nighttime awakenings, interference with activity, and rescue medication use (Table 1), were used to classify asthma as controlled or uncontrolled based on an adaptation of the National Institutes of Health Expert Panel Report-3 (NIH EPR-3) guidelines. The type and number of medications reported to control asthma were correlated with level of severity, using the NIH EPR-3 as a guideline, as the ACBS did not include information regarding the dose and strength of medications.(17) Those using only a rescue medication (short-acting beta-agonist or anti-cholinergic) were classified as intermittent. Those using an inhaled corticosteroid (ICS) or other controller medication were classified as mild. Those using 2 controller medications were classified as moderate. Those using more than 2 controller medications were classified as severe. A combination drug consisting of an ICS and a long-acting beta-agonist was considered to be 2 controller medications.
Table 1.
Classification of asthma control adopted from the National Asthma Education and Prevention Program Expert Panel Report 3 Guidelines
| Controlled | Uncontrolled | |
|---|---|---|
| Asthma symptomsa | ≤8 days | >8 days |
| Nighttime awakeningsb | ≤2 days | >2 days |
| Interference with activityc | Not at all or a little | Moderate amount or a lot |
| Rescue medicationd | ≤2 times per week | >2 times per week |
Symptoms were determined based on the response to the question “During the past 30 days, on how many days did you have any symptoms of asthma?”
Nighttime awakenings were determined based on the response to the question “During the past 30 days, on how many days did symptoms of asthma make it difficult for you to stay asleep?”
Interference with activity was determined based on the response to the question “During the past 12 months, would you say you limited your usual activities due to asthma not at all, a little, a moderate amount, or a lot?
Frequency of rescue medication was determined based on the response to the question “How many times per day or per week do you use a [short-acting β2-agonist or anti-cholinergic]?”
Statistical Analysis
Weighted proportions were used to adjust for loss of: sample between the BRFSS interview and the ACBS interview; variation in respondents’ probability of selection; disproportionate selection of population subgroups relative to the state's population distribution; or nonresponse.(18) Univariable analysis between the independent variables and CAM use was assessed using Pearson's Chi-square. To control for confounding variables, those variables that were statistically significant (p<0.05) in the univariable analysis were further analyzed using a multivariable logistic regression. Backward Wald stepwise regression was used to obtain odds ratios (OR) and 95% confidence intervals (95% CIs). Missing responses were not analyzed in the regression. SPSS® statistics version 22 (IBM Corp., Armonk, NY, USA) was used for all analyses.
Results
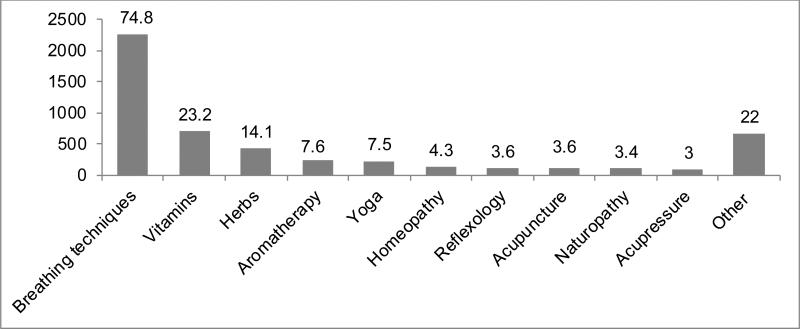
After limiting the study population to those ≥ 55 years old with current asthma, 7685 were included for analysis. Overall, 39% (3030) used at least one type of CAM. The most commonly reported CAM was breathing techniques (75%), followed by vitamins (23%), herbs (14%), and aromatherapy (8%) Those who specified “other alternative care” most commonly reported use of Primatene mist, relaxation techniques (chiropractor, massage, tai chi), meditation/prayer, hot liquids (tea, coffee), steam, saline nasal spray, diet, and exercise (Figure 1).
Figure 1.
Type of CAM use. Numbers above columns denote percentage (%) among CAM users.
Table 2 details the baseline demographic characteristics. The mean age was 67.2 years (range, 55-99 years) with 68% female and 83% Caucasian. Slightly more than half attained a college education (54%). More than two-thirds reported an annual household income of less than $50 000 (70%). The subjects were well distributed across the United States.
Table 2.
The relationship of CAM use with demographic characteristics.
| Characteristics | No. with current asthma (%)a | No. with current asthma that use CAM (%)a,b | P-value |
|---|---|---|---|
| Sex | |||
| Female | 5694 (67.7) | 2329 (41.6) | P<0.001 |
| Male | 1991 (32.3) | 701 (35.2) | |
| Age | |||
| 55-59 | 1662 (24.3) | 756 (43.8) | P<0.001 |
| 60-64 | 1759 (25.8) | 728 (42.6) | |
| 65-69 | 1541 (19.1) | 584 (37.8) | |
| 70-74 | 1172 (13.4) | 429 (34.9) | |
| BMI | |||
| 12 to <18.5 | 112 (1.1) | 50 (43.1) | P=0.385 |
| 18.5 to <25 | 1746 (21.9) | 712 (38.9) | |
| 25 to <30 | 2409 (34.4) | 936 (39.2) | |
| 30+ | 3134 (42.6) | 1226 (39.8) | |
| Race/ethnicity | |||
| White | 6541 (82.8) | 2560 (40.4) | P=0.051 |
| Black of African American | 632 (11.5) | 238 (32.3) | |
| Other race | 461 (5.8) | 205 (37.0) | |
| Education | |||
| Did not graduate high school | 857 (19.0) | 328 (40.8) | P<0.001 |
| Graduated high school | 2195 (26.5) | 777 (33.2) | |
| Attended college or technical school | 2214 (31.2) | 930 (44.2) | |
| Graduated from college or technical school | 2406 (23.2) | 989 (39.1) | |
| Annual household income | |||
| <$10,000 | 672 (9.5) | 318 (41.4) | P<0.001 |
| $10,000 to <$25,000 | 2211 (32.5) | 952 (43.9) | |
| $25,000 to <$50,000 | 1883 (27.5) | 701 (37.3) | |
| $50,000 to <$75,000 | 932 (12.5) | 349 (38.1) | |
| ≥ $75,000 | 1107 (17.9) | 378 (35.6) | |
| Geographic regionc | |||
| Midwest | 2226 (23.7) | 843 (38.3) | P=0.009 |
| South | 2114 (32.1) | 807 (40.2) | |
| West | 1947 (23.1) | 828 (39.2) | |
| Northeast | 1398 (21.1) | 552 (40.0) | |
| Impaired access to healthcare due to cost | |||
| No | 6385 (82.1) | 2337 (37.0) | P<0.001 |
| Yes | 1299 (17.9) | 692 (50.8) | |
| Lack of or gap in health insurance | |||
| No | 7013 (90.1) | 2703 (38.8) | P<0.001 |
| Yes | 657 (9.9) | 319 (44.3) |
Frequencies are unweighted and proportions are weighted. Missing responses are excluded.
Proportions are based on the total within each subset variable
Based on the U.S. Census Bureau-designated regions.
The relationship of CAM use and demographic characteristics is summarized in Table 2. Female gender was positively correlated with increased CAM use (42% vs 35%, p<0.001). As age increased, the overall proportion of those using CAM decreased (p<0.001). Level of educational attainment was associated with CAM use (p<0.001), with the highest proportion among those attending college (44%). Annual household income was also significantly associated with CAM use (p<0.001), with the highest proportion among those with an income between $10 000 to $25 000 (44%) versus those with an income greater than $75 000 (36%). CAM use was reported slightly more in the South and Northeast (40% in each region) as compared to the Midwest and West (38% and 39%, respectively, p<0.009). Those with impaired access to health care due to cost had a significantly higher proportion of CAM use than those who did not (51% versus 37%, p<0.001). Similarly, those with a lack of, or a gap in health insurance had a significantly higher proportion of CAM use than those who did not (44% versus 39%, p<0.001). No statistically significant associations were seen with BMI and race.
The relationship of CAM use and asthma outcomes is summarized in Table 3. Those with at least one ER visit in the past year due to asthma had a higher proportion of CAM use than those who did not (50% versus 38%, p<0.001). CAM use was significantly associated with asthma severity (p<0.001) with those classified as intermittent based on SABA use alone having the highest proportion of CAM use (43%) versus those classified as mild, moderate, or severe (40%, 38%, and 39%, respectively). Those with impaired asthma control in all domains had significantly higher proportion of CAM use (p<0.001). Other variables associated with a higher proportion of CAM use included those who had received an asthma action plan (45% vs 37%, p<0.001), asthma diagnosed ≥5 years ago (41% vs 32%, p<0.002), smoking history (p<0.001), lack of flu vaccine (42% vs 38%, p<0.001), and a history of depression (48% vs 34%, p<0.001).
Table 3.
The relationship of CAM use with asthma outcomes.
| Characteristics | No. with current asthma (%)a | No. with current asthma that use CAM (%)a,b | P-value |
|---|---|---|---|
| ER visit in past 12 months due to asthma | |||
| No | 6748 (87.5) | 2560 (37.8) | P<0.001 |
| Yes | 907 (12.5) | 452 (49.5) | |
| Asthma severity based on number of medications | |||
| Intermittent (SABA alone) | 1406 (26.6) | 590 (42.9) | P<0.001 |
| Mild (ICS or other single agent) | 1225 (21.0) | 471 (39.8) | |
| Moderate (2 controllers) | 1973 (38.4) | 708 (38.3) | |
| Severe (more than 2 controllers) | 809 (14.0) | 352 (38.6) | |
| Asthma action plan received | |||
| No | 5578 (72.8) | 2061 (37.2) | P<0.001 |
| Yes | 1937 (27.2) | 899 (45.4) | |
| Time since asthma diagnosis | |||
| <12 months | 197 (2.3) | 60 (31.6) | P<0.002 |
| 12 months to 5 years | 790 (10.4) | 285 (31.0) | |
| ≥ 5 years ago | 6661 (87.2) | 2681 (41.0) | |
| Smoking history | |||
| Never smoked | 3514 (43.9) | 1337 (37.9) | P<0.001 |
| Current smoker | 969 (16.5) | 447 (43.7) | |
| Former smoker | 3182 (39.6) | 1240 (39.5) | |
| Flu shot within past 12 months | |||
| No | 2758 (37.1) | 1181 (41.6) | P<0.001 |
| Yes | 4815 (62.9) | 1844 (38.2) | |
| History of physician-diagnosed depression | |||
| No | 4804 (60.3) | 1679 (33.6) | P<0.001 |
| Yes | 2848 (39.7) | 1330 (48.3) | |
| Asthma symptoms during the past 30 days | |||
| ≤8 days | 3219 (47.7) | 1258 (39.5) | P<0.001 |
| >8 days | 3411 (52.3) | 1496 (43.4) | |
| Difficulty sleeping due to asthma symptoms during the past 30 days | |||
| ≤2 days | 5469 (72.3) | 1938 (36.8) | P<0.001 |
| >2 days | 1905 (27.7) | 957 (46.7) | |
| Activity limitation due to asthma | |||
| Not at all or a little | 5088 (65.0) | 1763 (35.0) | P<0.001 |
| A moderate amount or a lot | 2536 (35.0) | 1242 (48.2) | |
| Rescue medication use | |||
| ≤2 times per week | 1313 (38.9) | 504 (38.4) | P<0.001 |
| >2 times per week | 1911 (61.1) | 866 (44.9) |
Abbrev: SABA – short acting beta agonist; ICS – inhaled corticosteroid
Frequencies are unweighted and proportions are weighted. Missing responses are excluded.
Proportions are based on the total within each subset variable
After regression analysis (Table 4), females had a 1.36-fold higher odds of using CAM than males (p<0.002). As compared to those who did not graduate high school, there was an increased odds of using CAM among those who attended college (OR 1.51, p<0.01) or graduated from college (OR 1.76, p<0.001). Geographic region was significant for those living in the West, as they were significantly more likely to use CAM as compared to other regions (OR 1.31, p<0.014). There was an inverse relationship between income and CAM use, as those in the highest income bracket were 40% less likely to use CAM than those in the lowest income bracket (p<0.006). Those with a cost barrier to health care had a 1.43-fold higher odds of using CAM compared to those without impaired access due to cost (p<0.001). There was an increased odds of using CAM among those with impaired asthma control, as defined by symptoms affecting sleep (OR 1.37, p<0.001), activity limitation (OR 1.38, p<0.001), and rescue medication use (OR 1.2, p<0.046). Those who had received an asthma action plan had a 1.29-fold higher odds of using CAM (p<0.005). Current smokers were significantly more likely to use CAM than those who never smoked (OR 1.35, p<0.02). There was no significant relationship between CAM use and lack of health insurance, ER visit due to asthma, asthma severity, asthma duration, flu vaccination status, and physician-diagnosed depression after controlling for confounding factors through regression analysis.
Table 4.
Multivariable subtype logistic regression of factors associated with CAM.
| aOR | 95% CI | p-value | |
|---|---|---|---|
| Sex | |||
| Male | 1.0 | REF | REF |
| Female | 1.36 | 1.12-1.65 | 0.002 |
| Education | |||
| Did not graduate high school | 1.0 | REF | REF |
| Graduated high school | 1.01 | 0.73-1.4 | 0.96 |
| Attended college or technical school | 1.51 | 1.09-2.1 | 0.01 |
| Graduated from college or technical school | 1.76 | 1.24-2.44 | 0.001 |
| Annual household income | |||
| <$10,000 | 1.0 | REF | REF |
| $10,000 to <$25,000 | 0.77 | 0.57-1.04 | 0.09 |
| $25,000 to <$50,000 | 0.67 | 0.49-0.92 | 0.014 |
| $50,000 to <$75,000 | 0.64 | 0.44-0.92 | 0.017 |
| ≥ $75,000 | 0.6 | 0.41-0.86 | 0.006 |
| Geographic regiona | |||
| Midwest | 1.0 | REF | REF |
| South | 0.98 | 0.79-1.22 | 0.85 |
| West | 1.31 | 1.06-1.64 | 0.014 |
| Northeast | 1.07 | 0.83-1.37 | 0.6 |
| Impaired access to health care due to cost | |||
| No | 1.0 | REF | REF |
| Yes | 1.43 | 1.16-1.78 | 0.001 |
| Asthma action plan received | |||
| No | 1.0 | REF | REF |
| Yes | 1.29 | 1.08-1.53 | 0.005 |
| Smoking history | |||
| Never smoked | 1.0 | REF | REF |
| Current smoker | 1.35 | 1.05-1.74 | 0.02 |
| Former smoker | 1.10 | 0.92-1.31 | 0.32 |
| Symptoms affecting sleep during past 30 days | |||
| ≤2 | 1.0 | REF | REF |
| >2 | 1.37 | 1.14-1.65 | 0.001 |
| Limitation of activities during past 12 months | |||
| Not at all or a little | 1.0 | REF | REF |
| Moderate amount or a lot | 1.38 | 1.15-1.66 | 0.001 |
| Rescue medication use | |||
| ≤2 times per week | 1.0 | REF | REF |
| >2 times per week | 1.2 | 1.0-1.43 | .046 |
Based on the U.S. Census Bureau-designated regions.
Discussion
The aim of this study was to determine the characteristics associated with CAM use among older adults with asthma as prior studies have found disparate results regarding the relationship of age and CAM use.(6, 9-12, 19) To our knowledge, this is the largest study assessing CAM use in the older adult asthmatic population. We found that the proportion of older adults with asthma who use CAM was 38%, which is similar to or greater than prior prevalence rates from studies of all adult asthmatics (including a previous study also utilizing the ACBS, which reported an overall adult asthmatic CAM usage rate of 39.6%).(6, 10-12, 16) CAM use may appeal to an older adult population, as they have more difficulty with inhaler technique, an increased risk of side effects from conventional medications, and the potential for drug interactions with multiple medications that are used to treat comorbidities.(20, 21)
The use of breathing techniques was by far the most commonly reported type of CAM. Breathing exercises are often considered a well-tolerated and safe adjunct therapy along with conventional asthma treatment.(22) Randomized studies assessing the benefit of breathing exercises are scarce, although in a recent Cochrane review, there were significant differences in quality of life and asthma symptoms favoring improvement.(23) The next most commonly reported CAM remedies were vitamins and herbs. Although these may be beneficial, they are not without risks in the older adult population. Vitamins in excess of the recommended daily allowance (RDA) may have significant side effects, and herbs may interact with other drugs.(24) It is important to ask about CAM therapies, as patients often do not willingly convey information about CAM use to their physicians. A systematic review found that disclosure rates varied greatly from 23%-72%.(25) In our previous study of 46 older adults with asthma, CAM use was frequently reported in focus groups, although the participants had not disclosed the CAM use to their physician.(26)
Our findings reveal that the relationship between CAM use and demographic characteristics in the older adult asthma population had notable similarities and differences to prior studies of adult asthma subjects. After adjusting for confounding factors, CAM use was associated with female gender, lower income, and impaired access to health care due to cost. The poverty rate for those aged 65 and older has increased in recent years, with a rate of almost 10% reported from the U.S. Census bureau.(27) The cost of conventional treatment for asthma may explain why those with cost barriers use more CAM. Those with higher education and recipients of asthma action plans were also more likely to use CAM. Previous studies have noted an inconsistent correlation with education and CAM use. Some studies found CAM use to be associated with more education,(7, 8, 12) whereas others found no association.(10, 11, 16) It is possible that those educated about their illness may seek out a variety of treatments available and question the recommendation of conventional practitioners.(7) There was a trend toward decreased CAM use as age increases, although this did not remain significant on regression analysis.
We found that poor asthma control, as defined by 3 of the 4 impairment measures (symptoms affecting sleep, limitation of activities, and use of rescue medication), remained significant for CAM use after adjusting for multiple variables. This is consistent with previous studies that have revealed a relationship between poor asthma control and CAM use.(10, 11, 19) It has been suggested that those with uncontrolled asthma may be dissatisfied with conventional therapy and more motivated to use CAM therapies.(11) Asthma severity based on the number of controller medications, however, was unrelated to CAM use after regression analysis. Consistent with our results, studies assessing asthma severity have been variable, although the definitions of asthma severity have also differed.(8, 9, 12, 16, 28) Our study suggests that an individual's perception of asthma control, rather than physician-classified asthma severity, may be a more important predictor of CAM use. Whether the lack of asthma control motivates older adults to utilize CAM or whether CAM use causes loss of asthma control cannot be answered by this study but clearly deserves further investigation.
This study has several limitations. The survey relies on a self-reported physician diagnosis of asthma, and older adults may confuse asthma with other common diseases that have similar symptoms, such as chronic obstructive pulmonary disease (COPD), congestive heart failure, recurrent aspiration, and gastroesophageal reflux. (29) It cannot be distinguished whether those with Asthma-COPD overlap syndrome (ACOS) are more or less likely to use CAM, as the ACBS did not exclude those with COPD. George et al. found that self-reported use of CAM among COPD patients was 41%, which is similar to the overall prevalence of 38% we found among older adults with asthma.(30) In our study, current smokers were more likely to use CAM, although details regarding the number of pack years are not known.
This study is also at risk for self-selection bias as no information could be obtained from non-respondents. There was no assessment of mental or functional status, which may underestimate the effect of those who rely on others for activities of daily living, such as answering telephone calls. The sample size was large, although there was a female and Caucasian predominance, which may affect generalizability. Factors other than cost, such as a transportation barrier, may impair access to health care for some older adults with asthma. There are also limitations classifying asthma severity based on self-reported medication use. For example, symptomatic asthmatics reporting SABA use only may be misclassified if they are hesitant to use medications. Lastly, the cross-sectional nature of this study limits the ability to infer causation.
In conclusion, CAM use in the older adult asthmatic population is frequent, with nearly 40% using some type of CAM. Characteristics associated with CAM use include lower socioeconomic status, cost barrier to healthcare, higher education, and living in the West. Asthma specific outcomes associated with CAM use include current smokers, poor asthma control, and recipients of asthma action plans. It is important for physicians to ask about CAM use in the older adult asthmatic population, as the use of such therapies is frequent, underreported, and may be a marker of poor asthma control.
Contributor Information
Claire E. Ward, Division of Allergy and Clinical Immunology, Department of Internal Medicine, University of Michigan Health System, Ann Arbor, MI
Alan P. Baptist, Division of Allergy and Clinical Immunology, Department of Internal Medicine, University of Michigan Health System, Ann Arbor, MI, abaptist@med.umich.edu
References
- 1.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. Vital & health statistics Series 3, Analytical and epidemiological studies. 35. US Dept of Health and Human Services, Public Health Service, National Center for Health Statistics; 2012. National surveillance of asthma: United States, 2001-2010. pp. 1–67. [PubMed] [Google Scholar]
- 2.Moorman JE, Mannino DM. Increasing U.S. asthma mortality rates: who is really dying? The Journal of asthma : official journal of the Association for the Care of Asthma. 2001;38(1):65–71. doi: 10.1081/jas-100000023. [DOI] [PubMed] [Google Scholar]
- 3.Enright PL, McClelland RL, Newman AB, Gottlieb DJ, Lebowitz MD. Underdiagnosis and undertreatment of asthma in the elderly. Cardiovascular Health Study Research Group. Chest. 1999;116(3):603–13. doi: 10.1378/chest.116.3.603. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Complementary and Alternative Medicine [2014 January 3]; Available from: http://nccam.nih.gov/health/whatiscam.
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. National health statistics reports. 2008;(12):1–23. [PubMed] [Google Scholar]
- 6.Slader CA, Reddel HK, Jenkins CR, Armour CL, Bosnic-Anticevich SZ. Complementary and alternative medicine use in asthma: who is using what? Respirology. 2006;11(4):373–87. doi: 10.1111/j.1440-1843.2006.00861.x. [DOI] [PubMed] [Google Scholar]
- 7.Astin JA. Why patients use alternative medicine: results of a national study. Jama. 1998;279(19):1548–53. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 8.Huo N, Ray GE, Mehta S, LoBello SG. Complementary and alternative medicine use among people with asthma and health-related quality of life. The Journal of asthma : official journal of the Association for the Care of Asthma. 2015;52(3):308–13. doi: 10.3109/02770903.2014.963867. [DOI] [PubMed] [Google Scholar]
- 9.Ernst E. Complementary therapies for asthma: what patients use. The Journal of asthma : official journal of the Association for the Care of Asthma. 1998;35(8):667–71. doi: 10.3109/02770909809048969. [DOI] [PubMed] [Google Scholar]
- 10.Marino LA, Shen J. Characteristics of complementary and alternative medicine use among adults with current asthma, 2006. The Journal of asthma : official journal of the Association for the Care of Asthma. 2010;47(5):521–5. doi: 10.3109/02770900903576320. [DOI] [PubMed] [Google Scholar]
- 11.Chen W, Fitzgerald JM, Rousseau R, Lynd LD, Tan WC, Sadatsafavi M. Complementary and alternative asthma treatments and their association with asthma control: a population-based study. BMJ open. 2013;3(9):e003360. doi: 10.1136/bmjopen-2013-003360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan W, Center H, Arms-Chavez C, LoBello SG. Complementary and alternative medicine use and asthma: relation to asthma severity and comorbid chronic disease. The Journal of asthma : official journal of the Association for the Care of Asthma. 2014;51(3):333–8. doi: 10.3109/02770903.2013.871559. [DOI] [PubMed] [Google Scholar]
- 13.Shaw A, Noble A, Salisbury C, Sharp D, Thompson E, Peters TJ. Predictors of complementary therapy use among asthma patients: results of a primary care survey. Health & social care in the community. 2008;16(2):155–64. doi: 10.1111/j.1365-2524.2007.00738.x. [DOI] [PubMed] [Google Scholar]
- 14.Center for Disease Control and Prevention [2014 January 3];Behavioral risk factor surveillance system [Data file and codebook] 2011 Available from: http://www.cdc.gov/brfss/annual_data/annual_2011.html.
- 15.Vincent GK, Velkoff VA. The older population in the United States: 2010 to 2050. United States Census Bureau. 2010 May;:1–14. [Google Scholar]
- 16.Blanc PD, Trupin L, Earnest G, Katz PP, Yelin EH, Eisner MD. Alternative therapies among adults with a reported diagnosis of asthma or rhinosinusitis : data from a population-based survey. Chest. 2001;120(5):1461–7. doi: 10.1378/chest.120.5.1461. [DOI] [PubMed] [Google Scholar]
- 17.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. The Journal of allergy and clinical immunology. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Behavioral risk factor surveillance system asthma call-back survey history and analysis guidance [cited 2014 January 3] 2011 Available from: http://www.cdc.gov/brfss/acbs/2011/documentations/ACBS_2011.pdf.
- 19.Knoeller GE, Mazurek JM, Moorman JE. Complementary and alternative medicine use among adults with work-related and non-work-related asthma. The Journal of asthma : official journal of the Association for the Care of Asthma. 2012;49(1):107–13. doi: 10.3109/02770903.2011.637597. [DOI] [PubMed] [Google Scholar]
- 20.Baptist AP, Hamad A, Patel MR. Special challenges in treatment and self-management of older women with asthma. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2014;113(2):125–30. doi: 10.1016/j.anai.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braman SS, Hanania NA. Asthma in older adults. Clinics in chest medicine. 2007;28(4):685–702, v. doi: 10.1016/j.ccm.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Arden-Close E, Teasdale E, Tonkin-Crine S, Pitre N, Stafford-Watson M, Gibson D, et al. Patients' perceptions of the potential of breathing training for asthma: a qualitative study. Primary care respiratory journal : journal of the General Practice Airways Group. 2013;22(4):449–53. doi: 10.4104/pcrj.2013.00092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freitas DA, Holloway EA, Bruno SS, Chaves GS, Fregonezi GA, Mendonca KP. Breathing exercises for adults with asthma. The Cochrane database of systematic reviews. 2013;10:CD001277. doi: 10.1002/14651858.CD001277.pub3. [DOI] [PubMed] [Google Scholar]
- 24.Eliopoulos C. Using complementary and alternative therapies wisely. Geriatric nursing. 1999;20(3):139–42. quiz 43. [PubMed] [Google Scholar]
- 25.Robinson A, McGrail MR. Disclosure of CAM use to medical practitioners: a review of qualitative and quantitative studies. Complementary therapies in medicine. 2004;12(2-3):90–8. doi: 10.1016/j.ctim.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Baptist AP, Deol BB, Reddy RC, Nelson B, Clark NM. Age-specific factors influencing asthma management by older adults. Qualitative health research. 2010;20(1):117–24. doi: 10.1177/1049732309355288. [DOI] [PubMed] [Google Scholar]
- 27.DeNavas-Walt C, Proctor BD. Income, Poverty, and Health Insurance Coverage in the United States. US Census Bureau; Washington, DC: 2013. pp. 60–249. [Google Scholar]
- 28.Ng TP, Wong ML, Hong CY, Koh KT, Goh LG. The use of complementary and alternative medicine by asthma patients. QJM : monthly journal of the Association of Physicians. 2003;96(10):747–54. doi: 10.1093/qjmed/hcg121. [DOI] [PubMed] [Google Scholar]
- 29.Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, et al. Asthma in the elderly: Current understanding and future research needs--a report of a National Institute on Aging (NIA) workshop. The Journal of allergy and clinical immunology. 2011;128(3 Suppl):S4–24. doi: 10.1016/j.jaci.2011.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.George J, Loannides-Demos LL, Santamaria NM, Kong DCM, Stewart K. Use of complementary and alternative medicines by patients with chronic obstructive pulmonary disease. Medical Journal of Australia. 2004;181(5):248–51. doi: 10.5694/j.1326-5377.2004.tb06262.x. [DOI] [PubMed] [Google Scholar]