Abstract
Multiple sclerosis (MS) is an autoimmune mediated neurodegenerative disease characterized by demyelination and oligodendrocyte (OL) loss in the central nervous system and accompanied by local inflammation and infiltration of peripheral immune cells. Although many risk factors and symptoms have been identified in MS, the pathology is complicated and the cause remains unknown. It is also unclear whether OL apoptosis precedes the inflammation or whether the local inflammation is the cause of OL death and demyelination. This review briefly discusses several models that have been developed to specifically ablate oligodendrocytes in an effort to separate the effects of demyelination from inflammation.
Keywords: multiple sclerosis, oligodendrocyte, apoptosis, demyelination, optic neuritis
Multiple sclerosis (MS) is an autoimmune mediated neurodegenerative disease characterized by demyelination and oligodendrocyte (OL) loss in multiple focal sites throughout the central nervous system (CNS). The loss of myelin and OLs is accompanied by local inflammation and infiltration of peripheral immune cells. Together, this pathology results in the interruption of axonal communication and functional deficits (Miller and Fyffe-Maricich, 2010). Although genetics, environment, geography, gender, and infection have been considered risk factors for MS, the initial cause remains unknown. Clinical symptoms include numbness and tingling, pain in arms and legs, bladder and bowel problems, difficulties with attention and memory, fatigue, mood changes, and visual disturbances. One of the first and most common clinical manifestations in MS patients is optic neuritis (Aranda et al., 2015), which is characterized by inflammation and demyelination of the optic nerve, initiating as an acute episode of blurred vision or visual loss in one eye with recovery occurring after 2–3 weeks in nearly 80% of patients (Arnold, 2005).
The pathology of MS and optic neuritis is complicated. It is unclear whether OL death precedes inflammation or whether local inflammation drives OL loss. Likewise, it is not well defined whether the loss of axonal communication is a consequence of demyelination or inflammation. The most common model to study optic neuritis is experimental autoimmune encephalomyelitis (EAE), which is induced by injection of myelin peptides into mice, rats, guinea pigs, or rabbits. However, studying cellular responses in optic neuritis in the EAE model is complicated by the inflammation and demyelination that occurs in other regions of the brain and spinal cord. For this reason, efforts have been made to locally demyelinate the optic nerve. For instance, Aranda et al. (2015) induced demyelination via microinjection of bacterial lipopolysaccharide (LPS) directly into rats’ optic nerves. Although significant demyelination of optic nerve was observed 21 days after LPS injection, microglia activation was present as early as 1 day after injection, suggesting that even local injection to the optic nerve initiates a neuroinflammatory response.
Various models have been developed in an effort to separate the effects of inflammation from demyelination in MS models and to provide insights into the effects of oligodendrocyte loss. For example, studies have used PLP/CreERT; ROSA26-eGFP-DTA mice to transcriptionally express diphtheria toxin A subunit (DT-A) upon tamoxifen injection specifically in OLs to induce apoptosis and demyelination in the CNS. These mice develop severe neurological symptoms such as ataxia and tremor, which peaks 5 weeks after injection. While by 10 weeks after injection the mice recover from most impairment, a secondary wave of symptoms including seizures and impaired motor skills manifest beginning at 40 weeks after injection (Traka et al., 2010, 2016). The loss of oligodendrocytes in this model is widespread and not limited to the optic nerve. Furthermore, the secondary functional deficits that occur may be a reflection of an inflammatory response. The development of a new model that targets demyelination to the optic nerve and does not have a primary inflammatory component would likely contribute new understanding regarding the pathology of optic neuritis. Here we provide a brief discussion of a new approach to induce local demyelination in the CNS and outline some initial observations suggesting its applicability to the study of optic neuritis.
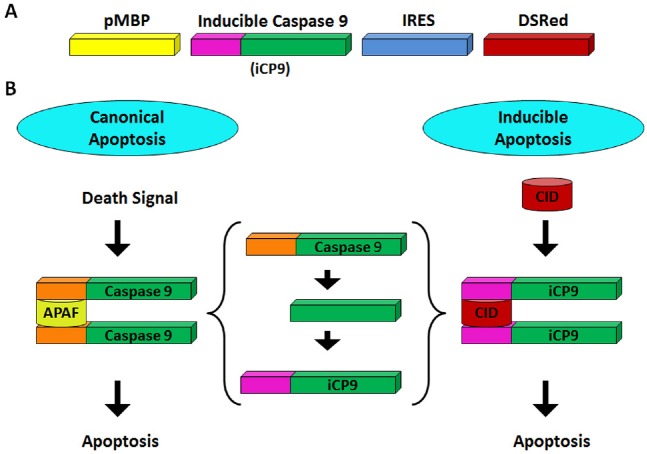
To specifically induce apoptosis in oligodendrocytes in initial studies, we constructed a lentiviral vector with a fragment of the rat myelin basic protein promoter (pMBP) targeting an inducible caspase (iCP9) sequence and reporter sequence to cells of the OL lineage. Dimerization of the iCP9 by delivery of a small molecule, chemical inducer of dimerization (CID), induced apoptosis in OLs in the absence of damage to any other cell type. In primary rat cortical cultures, while all cell types were infected with the virus, only oligodendrocytes were driven to apoptosis upon CID addition. Similarly, in vivo injection of the viral construct resulted in infection of neurons, astrocytes, and oligodendrocytes in the corpus callosum of rats. Subsequent delivery of CID, however, resulted in apoptosis specifically in mature OLs and rapid local demyelination (Caprariello et al., 2012). Whether the rapid demyelination seen in this model reflected priming of the tissue by the trauma of the needle injection or expression of viral coat proteins on the apoptotic cell is unclear. To avoid the complication of viral delivery, a series of transgenic animals were generated in which iCP9 construct and a DsRed reporter were driven off the same fragment of the MBP promoter to specifically target OL apoptosis (Figure 1A).
Figure 1.
Model of induced apoptosis in transgenic caspase 9 animals.
(A) Schematic of the transgene in MBP-inducible caspase 9 (MBP-iCP9) transgenic mice, in which iCP9 is transcriptionally regulated by myelin basic protein specific promoter sequence (pMBP). The presence of internal ribosome entry site (IRES) allows for the co-translation of DsRed fluorescent protein. (B) Schematic of the differences between canonical and the inducible model. Apoptosis is initiated in the canonical model by dimerization of caspase 9 via apoptotic protease activating factor 1 (APAF-1). Whereas, in the inducible model the APAF-1 binding site (orange) is replaced with a chemically induced dimerization (CID) binding domain (purple). Upon CID introduction, the MBP expressing oligodendrocytes undergo apoptosis.
In these transgenic animals, dimerization of the iCP9 by CID that is tissue permeable, and locally penetrates the CNS, results in selective induction of apoptosis in the OLs population without directly damaging or activating other cell types (Figure 1B). Systemic delivery of CID for 3 days during the first postnatal week resulted in a reduction of approximately 60% of the CC1+ oligodendrocytes in all regions of the CNS examined. This suggests that oligodendrocytes throughout the CNS are susceptible to CID induced apoptosis. Of the multiple transgenic lines generated, differences in expression levels of DsRed were seen depending on the specific line and age of the animals. Maximal reporter expression was seen during the second postnatal week and approximately 70% of the CC1+ cells were DsRed+. Little or no expression of DsRed was observed in the peripheral nervous system with no effect on myelination after CID exposure. One major advantage of the iCP9 system is that it allows for tight spatial targeting of oligodendrocyte loss through local delivery of the CID. Similar to other systems, the efficiency and specificity of the promoter used to target iCP9 is a limitation in this approach. In the MBP-iCP9 animals, the fragment of the MBP promoter is highly specific for oligodendrocytes, but its activity is reduced in older animals making this model suitable for developmental studies.
Using the MBP-iCP9 transgenic mice, mature OLs were ablated in a region of the spinal cord between postnatal days 4–7. This resulted in an inhibition of myelination during the first postnatal week demonstrating that mature OLs are essential for CNS myelination. The inhibition of myelination was transient. Myelination recovered to apparently normal levels 2 weeks after stopping CID treatment indicating that disruption of the timing of developmental myelination does not dramatically impair myelin formation. Remarkably, while recovery appeared normal, when CID treated regions were challenged with a second insult in adult animals, there was a significant impairment of remyelination from a lysolecithin lesion suggesting that an insult to the OL population early in life may compromise the response to subsequent demyelinating lesions (Caprariello et al., 2015). This data implies a residual change in CNS tissue as a result of early oligodendrocyte loss. It may be that the oligodendrocyte lineage is itself compromised through early exhaustion of progenitors. Alternatively, local changes in the cellular environment associated with astrocytes or microglial cells may compromise secondary repair. Distinguishing between these possibilities requires further studies.
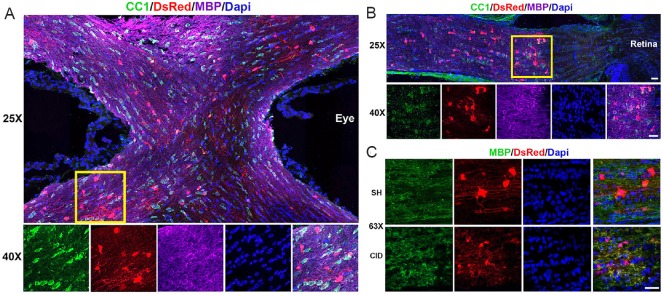
Since the optic nerve presents the most intensely studied white matter track with respect to glial biology, current studies are expanding to investigate the effects of demyelination of the optic nerve in MBP-iCP9 transgenic mice. Preliminary results indicate that DSRed+ OLs are present in the optic chiasm (Figure 2A) and the optic nerve (Figure 2B) of the transgenic mice as a subpopulation of CC1+ cells. Furthermore, intravitreal CID injection at P12 for 2 consecutive days induces OL apoptosis in the optic nerve at P15 as indicated in Figure 2C. These results allow for demyelination of the optic nerve by specifically ablating the OLs without affecting other cell types. Since at any single time point not all CC1+ cells are DSRed+, OLs ablation and demyelination in response to a single period of CID administration is expected to be partial, and whether extended exposure to CID results in increased myelin loss is currently being assessed.
Figure 2.
DsRed+ oligodendrocytes, present in optic nerve, undergo apoptosis after CID exposure.
(A) and (B) MBP-inducible caspase 9 (MBP-iCP9) transgenic mice were sacrificed at 25 days and cryostat sections from optic chiasm (A) and optic nerve (B) were stained with anti-APC antibody (CC1) (green), DsRed (red), and myelin basic protein (MBP) (magenta); 4′,6-diamidino-2-phenylindole (DAPI) (blue) was used as a nuclear counterstain. Images were taken using a 25× and 40× objective on a spinning confocal microscope. DsRed cells are observed both in the optic chiasm and the optic nerve as a subpopulation of the CC1+ cells. (C) MBP-iCP9 transgenic mice were injected 2 consecutive days with 5 mM chemically induced dimerization (CID) intravitreally and sacrificed on day 3. Longitudinal sections were stained with antibodies against MBP (green) and DsRed (red); DAPI (blue) was used as a nuclear counterstain. Images were taken using a 63× objective of a confocal microscope. CID injection induces apoptosis in the optic nerve and results in beading in the MBP (Scale bars: 10 μm).
Although our understanding of the biology of the OL lineage in myelination and demyelination is reasonably well developed, our knowledge of the effects of demyelination on neuronal populations is limited. Apoptosis of retinal ganglion cells (RGCs) has been observed in animal models of MS and optic neuritis and is correlated with the optic nerve inflammation. For instance, chronic models of EAE in rats demonstrated that RGC loss manifests prior to the onset of clinical symptoms of optic neuritis (Hobom et al., 2004), suggesting that RGC apoptosis may be independent from inflammation or the target of inflammatory attack. However, a relapsing/remitting EAE mouse model has revealed that RGC loss begins 5 days after the signs of optic neuritis were established (Shindler et al., 2006), indicating that RGC apoptosis may be secondary to inflammatory response. Regardless of inflammation being a cause or an effect, the presence of inflammatory factor significantly complicates interpretation of the underlying mechanisms.
A recent study (Hovhannisyan et al., 2015) investigated the effects of lack of myelin on neuronal function utilizing Jimpy mutant mice, in which a point mutation in the proteolipid protein gene (plp1) results in OL death and prevents normal myelination in the CNS. Although myelination of axons was absent from the optic nerve of Jimpy mice, optikinetic reflex measurements showed a functional visual system, suggesting that the lack of myelination in RGC axons had little effect on retinal function. Whether a similar retention in function is observed after demyelination is unknown, but it can now be addressed by OLs depletion in the optic nerve of the MBP-iCP9 transgenic mice. It may be that demyelination will result in RGCs apoptosis and axonal degeneration or that axonal degeneration seen in optic neuritis reflects inflammatory factors and not OL apoptosis and direct demyelination. Whatever the outcomes, the development of new models to selectively ablate myelinating cells in the vertebrate CNS will yield critical insights into the biology of myelination and the pathology of demyelination.
Footnotes
Funding: This work has been supported in part by Genentech.
References
- Aranda ML, Dorfman D, Sande PH, Rosenstein RE. Experimental optic neuritis induced by the microinjection of lipopolysaccharide into the optic nerve. Exp Neurol. 2015;266:30–41. doi: 10.1016/j.expneurol.2015.01.010. [DOI] [PubMed] [Google Scholar]
- Arnold AC. Evolving management of optic neuritis and multiple sclerosis. Am J Ophthalmol. 2005;139:1101–1108. doi: 10.1016/j.ajo.2005.01.031. [DOI] [PubMed] [Google Scholar]
- Caprariello AV, Mangla S, Miller RH, Selkirk SM. Apoptosis of oligodendrocytes in the central nervous system results in rapid focal demyelination. Ann Neurol. 2012;72:395–405. doi: 10.1002/ana.23606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caprariello AV, Batt CE, Zippe I, Romito-DiGiacomo RR, Karl M, Miller RH. Apoptosis of oligodendrocytes during early development delays myelination and impairs subsequent responses to demyelination. J Neurosci. 2015;35:14031–14041. doi: 10.1523/JNEUROSCI.1706-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobom M, Storch MK, Weissert R, Maier K, Radhakrishnan A, Kramer B, Bahr M, Diem R. Mechanisms and time course of neuronal degeneration in experimental autoimmune encephalomyelitis. Brain Pathol. 2004;14:148–157. doi: 10.1111/j.1750-3639.2004.tb00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovhannisyan A, Benkner B, Biesemeier A, Schraermeyer U, Kukley M, Munch TA. Effects of the jimpy mutation on mouse retinal structure and function. J Comp Neurol. 2015;523:2788–2806. doi: 10.1002/cne.23818. [DOI] [PubMed] [Google Scholar]
- Miller RH, Fyffe-Maricich SL. Restoring the balance between disease and repair in multiple sclerosis: insights from mouse models. Dis Model Mech. 2010;3:535–539. doi: 10.1242/dmm.001958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shindler KS, Guan Y, Ventura E, Bennett J, Rostami A. Retinal ganglion cell loss induced by acute optic neuritis in a relapsing model of multiple sclerosis. Mult Scler. 2006;12:526–532. doi: 10.1177/1352458506070629. [DOI] [PubMed] [Google Scholar]
- Traka M, Podojil JR, McCarthy DP, Miller SD, Popko B. Oligodendrocyte death results in immune-mediated CNS demyelination. Nat Neurosci. 2016;19:65–74. doi: 10.1038/nn.4193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traka M, Arasi K, Avila RL, Podojil JR, Christakos A, Miller SD, Soliven B, Popko B. A genetic mouse model of adult-onset, pervasive central nervous system demyelination with robust remyelination. Brain. 2010;133:3017–3029. doi: 10.1093/brain/awq247. [DOI] [PMC free article] [PubMed] [Google Scholar]