Abstract
Background
During deployment and upon returning home, Veterans experience emotional challenges that test their social and psychological adaptation and place them at risk for suicidal thinking. Individual variability in skill-based capacity to adaptively perceive, understand, correctly use and manage emotions (called emotional competence) may play a role in the development of psychological suffering and suicidal thinking. Based on research in healthy and clinical samples, poor emotional competence was predicted to be associated with suicidal thinking among returning Veterans.
Methods
Participants were selected from the W.F. Caveness Vietnam Head Injury Study (VHIS) registry that in the late 1960’s began prospectively assessing 1221 Veterans (Raymont, V., Salazar, A. M., Krueger, F., & Grafman, J., 2011). The study sample was comprised of Veterans examined between 2003–2006 and included 185 participants who at the time of assessment with the Beck Depression Inventory (BDI) did (N=46) or did not endorse (N=139) suicidal thinking then or during the previous two weeks and received performance based measures of emotional competence (MSCEIT, version 2.0) and theory of mind. MSCEIT subtests and theory of mind tasks were condensed via principal component analysis: Component 1 (Emotion Processing) included Using, Understanding and Managing emotions tasks, and Component 2 (Emotion Perception) included Perceiving emotions.
Results
Veterans endorsing suicidal thoughts showed poorer Emotion Processing whereas Emotion Perception and theory of mind tasks did not show significant group effects. In addition, Veterans who endorsed thoughts of suicide were deployed at a younger age, had lower education, and tended to report more negative experiences in social interactions upon return to the US.
Conclusions
The capacity to understand, use and manage emotionally charged stimuli and situations may represent risk factors for suicidal thinking among Veterans.
Keywords: Emotional intelligence, MSCEIT, suicide, Veterans, psychopathology
A clear relationship between psychological pain and suicidal thoughts has been established through phenomenology and life history research (Shneidman, 1996). Theoretical models of suicide (Shneidman, 1992) suggest that appraisal of life events as negative is a critical factor. More recently, other experts (Joiner, 2005) have pointed out that individuals may develop suicidal thoughts or behavior when feeling overwhelmed by the complexity of social and emotional events in their lives. Thus, actual negative emotional events, judgment of these events, and the ability to manage emotional consequences may each play a role in the development of suicidal thinking. Specifically, coping with negative emotional events may require accurate appraisal of the events and the ability to manage the associated emotions.
Some of these skills fall under the rubric of emotional intelligence, which has often been measured with the Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) (Mayer, Salovey, & Caruso, 2012). The MSCEIT reliably measures the capacity to adaptively perceive, experience, understand and manage emotional material (Mayer, Salovey & Caruso, 2004). To reduce response bias, in the MSCEIT emotional intelligence is measured as a set of skills, not as self-reported personality characteristics (Landy, 2005; Mayer, Salovey & Caruso, 2008). Because this measure is skills-based, it will be called emotional competence from this point forward to distinguish it from measures of personality (Landy, 2005; Mayer et al., 2008). Performance on the MSCEIT is positively associated with real world social abilities (Mayer, Roberts, & Barsade, 2008) and psychological well-being (Lanciano, & Curci, 2015). On the other hand, it is negatively associated with maladaptive behaviors, including illegal drug use (Brackett, Mayer, & Warner, 2004).
Given that emotional competence is among the best predictors of adaptive coping strategies to stress (Extremera & Fernández-Berrocal, 2002; Limonero, Tomás-Sábado, Fernández-Castro, & Gómez-Benito, 2004; Limonero, Tomás-Sábado, & Fernández-Castro, 2006a; Limonero, Tomás-Sábado, & Fernández-Castro, 2006b; Limonero, Tomás-Sábado, Fernández-Castro, Gómez-Romero, & Aradilla-Herrero, 2012; Cabello, Navarro Bravo, Latorre, & Fernández-Berrocal, 2014), it is surprising that only few studies have examined its relationship with suicidal tendencies. In one study, Szanto and colleagues (2012) reported that one of the ostensible components of emotional intelligence (i.e., perception of social emotions) was poorer among elderly suicide attempters relative to elderly with no psychiatric history. Euthymic patients with a history of a serious suicide attempt made more errors in perception of disgust in human faces (Richard-Devantoy, Guillaume, Olie, Courtet, & Jollant, 2013) than participants with history of depression and never depressed participants. This indicates that components of emotional intelligence may constitute a set of cognitive abilities that is associated with a lower tendency for suicidal ideation in individuals with depression (Abdollahi, & Talib, 2015).
Veterans may experience unusual emotional challenges upon returning home. Recent data shows that Veterans who left active-duty commit suicide at a rate 40 to 60% higher than their civilian peers (Kang et al., 2015). Veterans with traumatic brain injury and history of suicidal behavior or ideation reported that they perceived themselves to be a burden to their families and to society as a whole (Brenner, Homaifar, Adler, Wolfman, & Kemp, 2009.) Furthermore, they reported inability to handle shifting moods and social isolation (Brenner et al., 2009). Perception of themselves as a burden was a predictor for suicidal ideation in Veterans who were treated for mental health issues (Monteith, Pease, Forster, Homaifar, & Bahraini, 2015). Whereas Veterans’ personal life events and experiences in the war zone undoubtedly play a role in their depression and suicidal tendencies, the ability to cope with these emotional challenges is also likely to play an important part (Kuipers & Lancaster, 2000). Veterans’ capacity to cope with emotional challenges has not been fully characterized in the literature. Determining emotional competence among returning Veterans with thoughts of suicide serves as a first step towards assessing whether emotional competence levels may be a factor for suicidal risk. Due to the combination of life changes and elevated suicidal thinking and behavior, Veterans represent an important population to investigate the relationship between emotional competence and suicidal thinking.
In the present study, we used archival data from the W. F. Caveness Vietnam Study registry (Raymont et al., 2011). Emotional competence was measured using the MSCEIT (Mayer & Salovey, 1997). Data from the W. F. Caveness registry (Raymont et al., 2011) have contributed to establishing the validity of the emotional competence construct and to understanding its neuroscientific bases (Krueger et al., 2009; Barbey, Colom & Grafman, 2014). We predicted that returning Veteran participants endorsing suicidal thinking would show poorer emotional competence relative to returning Veterans who did not endorse suicidal thinking.
Method
Participants
Participants were selected from the W. F. Caveness Vietnam Head Injury Study (VHIS) registry. The VHIS registry included 1221 American Soldiers who survived penetrating brain wounds and closed head injuries (8% of the cohort) suffered in Vietnam between 1967 and 1970 (Caveness et al., 1979; Raymont et al., 2011). Field neurosurgeons were asked to provide post-injury clinical information to establish a registry of individuals anticipated to survive. There were about 2000 registry forms, but addresses were found for 1221 Veterans. Exclusionary criteria included spinal cord injury or insufficient medical records. Between August 1981 and August 1984, 520 Veterans from the registry (and 85 neurologically healthy comparison participants recruited from VA files of non-head-injured soldiers who had served in Vietnam during the same years as the injured Veterans) agreed to participate in a clinical assessment study at Walter Reed Army Medical Center. There were 90 (35.3%) Veterans assigned to an Army Infantry Unit, 54 (21.2%) were Marines, 31 (12.2%) were in cavalry units and 8 (3.1%) were in Special Forces. The remainder of participants was in support services or in units that did not see direct ground combat. There were 119 (50.4%) who reported constant combat exposure and 62 (6.3%) who reported intermittent combat exposure during their tour of duty.
Between April 2003 and November 2006, 254 Veterans (199 brain injured and 55 without brain injury) were re-examined. Participants with complete measurement of emotional competence using the Mayer-Salovey-Caruso emotional intelligence test (Mayer, Salovey, & Caruso, 2002) (131 Veterans with CT scan ascertained brain injury, and 54 non-brain-injured Veterans) were included. The effects of brain injury on suicide tendencies will be described in a separate manuscript in preparation. All participants were men. Mean age was 58.69 (SD=3.49) (M=58.46, SD=3.41 for the parent sample of 254 participants). A majority of the sample was of Caucasian descent (92.4%) (89.4% in the parent sample) and primarily right handed (77.3%) (75.6% in the parent sample). Mean education was 15 years (SD=2.43) (M=14.8, SD=2.52 for the parent sample). Participants’ characteristics before time of enrollment were available from military and VA records. Participants underwent a personal interview (VR) aimed at recording type of military unit they belonged to in Vietnam, and assessing type and (subjective) degree of combat exposure. Participants were also asked to rate the feedback (negative or otherwise) they received upon returning to the US. All participants gave informed written consent before completing the study.
Suicide Assessment
Thoughts of suicide were assessed using the Beck Depression Inventory (Beck, Steer & Brown, 1996) at the same visit during which emotional competence was measured. In the Beck Depression Inventory, participants are asked if they are currently experiencing suicidal tendencies or have experience them over the previous two weeks. Participants could respond: a) “I do not have any thoughts of killing myself”, b) “I have thoughts of killing myself but I would not carry them out”, c) “I would like to kill myself”, and d) “I would kill myself if I had a chance”. There were 45 individuals (97.8%) who endorsed item b) and only one participant endorsing item c). These constituted the “endorsement of suicide thought” group. None of the participants endorsed item d). The comparison sample was composed of the 139 participants who endorsed item a).
Experimental Tasks: Emotional competence
The Mayer-Salovey-Caruso emotional intelligence test (MSCEIT version 2.0) (Mayer et al., 2002) was used to measure emotional competence (Krueger et al., 2009). Emotional competence is defined in the present study as a set of mental capacities (i.e., an ability-based construct not including personality traits, preferences, or inclinations) allowing an individual to adaptively perceive, experience, understand and manage emotions in the self and the other. The term emotional competence is preferred in the present report over emotional intelligence (EI) (Mayer & Salovey, 1997) because the latter has recently been expanded to include personality features (Landy, 2005; Mayer et al., 2008).
The MSCEIT 2.0 is a 141-item scale includes basic emotion perception (Faces and Pictures Tasks) and more complex tasks measuring how emotions are used for facilitating thought (Sensations and Facilitation tasks), and how emotions are understood (Blends and Changes tasks), and managed (Emotion Management and Emotional Relationships tasks). Correct answers are determined based on expert or general consensus scores (Mayer, Salovey, Caruso, Sitarenios, & 2003). The MSCEIT has high reliability (e.g., r=.93 for general consensus scoring) and there is evidence for the validity of the task based on research on the construct of emotional intelligence (Mayer, Salovey, & Caruso, 2004).
There are 8 MSCEIT tasks each of which may include parcels or individual items. See Figure 1 for example items from the task. A parcel occurs, for instance, when a participant is shown a face (in the Faces task) and asked about different emotions in the same face in five subsequent items. Individual items ask for a single response per stimulus. Some tasks use a 5-point rating scale, whereas some other tasks use a multiple-choice response format to ensure that results generalize across response methods and to reduce correlated measurement error. A brief explanation of the individual tasks follows. The Faces task includes 4 parcels and 5 responses per parcel, and requires participants to view a series of faces and indicate on a five-point scale the degree to which a specific emotion is present. The Pictures task includes 6 parcels and 5 responses - each parcel is, in principle, the same as the faces task, but in the picture task landscapes and abstract designs constitute the target stimuli and the response scale consists of cartoon faces (not words) of specific emotions. The Sensations task includes 5 parcels with 3 responses for each parcel. Participants are asked to generate an emotion and match sensations to them. For instance, they may generate a feeling of envy and decide the temperature associated with it. The Facilitation task includes 5 parcels with 3 responses each in which participants judge the moods that best accompany or assist specific cognitive tasks and behaviors. For instance, the extent to which happiness may help in planning a party. In the Blends task (comprised of 12 free-standing items), participants are requested to identify emotions that may be combined to form another emotion. They may conclude, for example, that malice is a combination of envy and aggression.
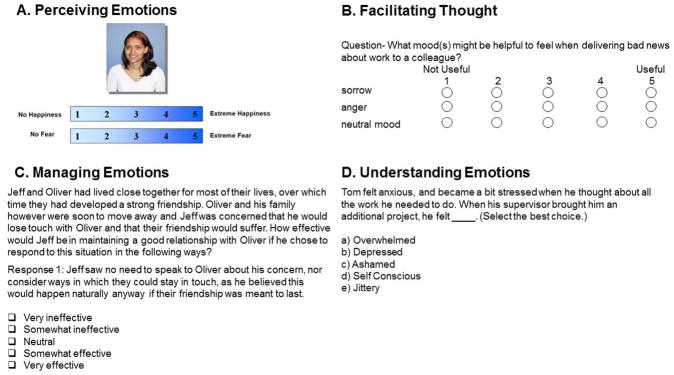
Figure 1.
Example stimuli from the MSCEIT battery of tasks. Part A represents an example stimulus from the Perceiving Emotions Task. Part B depicts an example from the Facilitating Thoughts task. Part C includes an example from the Managing Emotions task and Part D depicts an example from the Understanding Emotions task.
In the Changes task (20 items), participants are asked to select an emotion resulting from the intensification of another feeling. For example, they may identify panic as the most likely consequence of intensified fear. Respondents in the Emotion Management task (5 parcels; 4 responses each) are asked to judge the most effective actions in obtaining the specified emotional outcome for an individual in a story. They are asked to decide, for example, what a character may do to reduce her anger, or prolong her joy. Finally, in the Emotional Relationships task (3 parcels; 3 responses each), respondents judge the most effective actions for one person to use in the management of another person’s feelings. For more information see (Caruso, Mayer & Salovey, 2002).
These brief examples portray the extent to which the MSCEIT tasks measure purpose and complexity of emotion processing. For instance, a correct response in the “character need to reduce anger” question is indicative of the fact that the responder knows what it takes to reduce anger in general (emotion management). Furthermore, the example provided in Fig. 1C is meant to assess the responder’s capacity to predict what behavior will be beneficial to maintain a strong friendship (use of emotion). There is growing evidence that emotion competence skills translate into real life behavior (Mayer, et al., 2008; Lanciano & Curci, 2015).
Theory of Mind Tasks
To determine the specificity of any emotional competence findings, Veterans were tested on two theory of mind tasks: the faux pas detection (Leopold et al., 2012) and the Happé tasks (Happé, 1994). It was expected that scores on these tasks would not predict suicidal thinking unlike the MSCEIT scores (because these tasks do not directly reference emotional situations). For the Happé tasks, participants were presented with 16 stories with little emotional content (8 theory of mind stories and 8 physical response stories) selected from those developed by Happé (Happé, 1994). Theory of mind items required appreciation of the intentions of the persons described in the stories, whereas physical story questions involved an understanding of the physical implications of the story. Participants received two points for each correct answer, one point for a partial answer, and zero points for incorrect answers or no response. A theory of mind and a physical story score were calculated.
Ten faux pas recognition short stories were administered describing a main character unintentionally hurting or insulting another character in the story by saying something inappropriate with story-specific questions asked to participants. The experimenter read the story to participants who had their own copy to read. After each story, participants were asked a series of questions. The stories remained available to participants while questions were asked (to avoid memory effects). To control for verbal comprehension, participants were also asked two control questions irrespective of correctly answering the question. First, participants received a Faux Pas detection question: “was something awkward said in the story”? For positive answers (and the story was a Faux Pas story) participants were asked 5 additional Faux Pas follow up questions. Maximum total score was 60. If participants answered ‘no’ to any Faux Pas detection questions, they received 0 points for that particular story, but could still receive one point for each correctly answered control question (including questions on comprehension of the faux pas story). The raw scores for each question/answer combination (faux pas story/faux pas question; faux pas story/comprehension question; comprehension story/comprehension question; comprehension story/faux pas question) were used in the analyses.
Psychiatric and Cognitive Assessment
A psychiatrist (VR) administered the Structured Clinical Interview for DSM-IV-TR Axis I disorders, Non-Patient edition (SCID-N/P) (First, Spitzer, Gibbon & Williams, 2002). To measure severity of current depression and anxiety participants were assessed using the Beck Depression Inventory, Second Edition (BDI-II) (Beck et al., 1996) and the Hamilton Anxiety scale (HAS). The BDI-II (Beck et al., 1996) is a 21-item self-report instrument for measuring severity of depression. Participants rate each symptom/item on a scale of 0 to 3 (higher numbers indicate greater severity). An overall BDI score (0–63) is attained by summing the severity ratings for each item. The Hamilton Anxiety scale (HAS) (Hamilton, 1959) is a widely used interview scale measuring the severity of anxiety, based on 14 parameters (e.g., anxious mood, tension, fears, insomnia, somatic complaints and behavior at the interview) rated on a scale of 0 to 4, with 0 being "there is no problem" and 4 being "the situation is disabling."
Participants’ current intelligence was measured using the WAIS-III (Wechsler, 1997). Assessment of general intelligence at time of enlistment was carried out using the Armed Forces Qualification Test (AFQT-7A) (Anonymous, 1960) an extensively standardized test within the U.S. military measuring vocabulary knowledge, arithmetic word problem solving, object – function matching and mental imagery ability with multiple choice questions.
Statistical Analysis
Descriptive statistics (means and standard deviations and t-tests, and Chi-square for categorical data) were used to characterize participants based on their endorsement of suicidal thoughts. All analyses assumed variance between the groups was not equivalent based on the Levene’s test for equality of variance. Logistic regressions were used to examine the study hypotheses.
Before fitting the MSCEIT tasks scores into a logistic regression model, a principal component analysis was computed using the extraction method with varimax rotation and Kaiser normalization. Summary scores for each MSCEIT task were included in the model for each subject: (Perceiving Emotions: Faces, Pictures; Using Emotion: Sensation, Facilitation; Understanding Emotions: Blends, Changes; Managing Emotions: Emotion Management, Social Management). Tasks were not weighted. The number of factors was determined using a general law of parsimony that combined the percent of cumulative variance method and number of nontrivial factors (defined as factors with at least three variables loading above 0.30) method. Once the number of factors were determined, we examined which tasks had the highest loading for each factor. The same procedure was applied to all theory of mind (faux pas and Happé) tasks before fitting the variables’ scores to a logistic regression model.
Results
Sample Description
The group of participants that reported suicidal thoughts were compared to the group who did not report suicidal thoughts based on demographics, cognitive function, and psychiatric assessment (see Table 1). There were significant differences between the two groups on age and age at the time they served in Vietnam; those individuals who did not report suicidal thinking were older than the group who did report suicidal thinking [age: t(136.30)=2.99, p=.003, d=0.5; age in Vietnam: t(135.19)= 2.95, p=.004, d=0.5]. The two groups significantly differed in years of education, with the group who did not report suicidal thoughts having slightly higher educational levels [t(102.73)=2.63, p=.01, d=0.5.] The two groups did not significantly differ on general intelligence as measured by the WAIS-III [t(80.11)=.45, p=.66, d=0.1]or AFQT scores (estimate of premorbid intelligence) [t(68.47)=0.41, p=.65, d=0.1].
Table 1.
Demographic, cognitive, and clinical variables
| No Suicide Thoughts (N=139) | Suicide Thoughts (N=46) | |||
|---|---|---|---|---|
|
| ||||
| M | SD or % | M | SD or % | |
| Age** | 59.02 | 3.77 | 57.67 | 2.16 |
| Age in Vietnam** | 20.89 | 3.28 | 19.71 | 1.68 |
| Total years of education* | 15.20 | 2.55 | 14.27 | 1.90 |
| Race (N, % Caucasians) | 129 | 92.80% | 42 | 91.3% |
| Handedness (N, % right handed) | R: 105, L: 20 | 75.5% | R: 38, L: 6 | 82.6% |
| AFQT (percentile) | 62.8 | 24.3 | 64.8 | 23.2 |
| WAIS-III FS IQ | 106.11 | 14.60 | 105.02 | 14.14 |
| BDI*** | 5.02 | 5.29 | 21.17 | 10.25 |
| HAS*** | 2.05 | 2.62 | 6.21 | 4.59 |
Notes. M=Mean, SD=standard deviation. AFQT=Armed Forces Qualification Test. WAIS = Wechsler Adult Intelligence Scale-III for cognitive abilities, FSIQ = full scale IQ, VIQ= verbal IQ, PIQ = performance IQ BDI = Beck Depression Inventory HAS = Hamilton Anxiety Scale. Groups were compared on these variables using t-tests and chi-square tests, equal variance not assumed.
Significance level: two-tailed tests; p<.05*, p<.01**, p<.001***.
The group with reported thoughts of suicide had significantly greater severity of depression and anxiety; these levels are in the mild to moderate range [depression: t(50.95)=5.66, p<.001, d=1.6; anxiety: t(53.15)=10.25, p<.0001, d=2.8]. The groups did not significantly differ on race or handedness [race: Χ(3)=3.36, p=.34, r=0.13; handedness: Χ (4)=3.30, p=.51, r=0.13].
In terms of service assignment, among Veterans endorsing suicide thoughts 11.6% were in combat service support (i.e., expected to be exposed to occasional mortar attack), 18.6 % were in combat support (i.e., expected intermittent enemy contact), 14.0% were in combat unit with expected intermittent enemy contact and 55.8% were in combat unit with expected constant enemy contact (0% were in support units that exposed them to no action). Among Veterans not endorsing suicide thinking, the rates of service assignment were respectively 10.1% in combat service support, 13.2% in combat support, 29.5% in combat unit with intermittent contact and 43.4% in combat unit with constant contact (3.9% were in support units that exposed them to no action) [Χ (4)=6.5, p=.16, r=0.22].
Among Veterans reporting suicide thoughts, 2.4% were not exposed to combat, whereas 38.1% had mild exposure, 26.2% had moderate, and 33.3% had severe combat exposure. Among Veterans not reporting suicide thinking, 0% had no combat exposure and 51.3% had mild, 27.0% moderate or 20.9% severe combat exposure [Χ (4)=6.2, p=0.17, r=0.37].
Seventy (38.9%) Veterans reported experiencing negative reactions upon their return from Vietnam and were significantly more likely to experience suicidal thoughts [Χ (2)=6.6, p=0.04, r=0.19]. Among participants endorsing suicidal ideation, 28.9 % (relative to 25.2% not endorsing suicidal ideation) admitted to having a history of minor and 4.4% (relative to 1.5% not endorsing suicidal ideation) major trouble with the law (but 6.7 among suicidal ideation vs. 0.7% without suicidal ideation responded do not know) [Χ (3)=7.6, p=0.06, r=0.41].
Whereas mood and anxiety disorders occurred more frequently among veterans endorsing suicidal ideation, rates of concurrent psychiatric diagnoses (with the exception of Post-traumatic Stress Disorder, PTSD) were low (see Table 2). The groups significantly differed on major depression [Χ (1)= 9.2, p<.005, r=0.22], dysthymic disorder [Χ (1)= 6.9, p<.01, r=.19], panic disorder [Χ (1)=24, p<.001, r=0.36], PTSD [Χ (1)=23, p<.001, r=.35] and psychotic symptoms [Χ (1)= 8.4, p<.005, r=.21], but not alcohol abuse [Χ (1)= 0.5, p>.8, r=.05]. See Table 2 for additional details.
Table 2.
Psychiatric disorders at the time of emotion competence measurement
| No Suicide Thoughts (N=139) | Suicide Thoughts (N=46) | |||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Major depression ** | 0 | 0% | 3 | 6.5% |
| Dysthymic disorder ** | 4 | 2.9% | 6 | 13.0% |
| Panic disorder *** | 1 | 0.7% | 9 | 19.6 |
| PTSD *** | 14 | 10.1% | 19 | 41.3% |
| Alcohol abuse | 5 | 3.6% | 2 | 4.3% |
| Psychotic symptoms ** | 2 | 1.4% | 5 | 10.9% |
Notes. Diagnoses are based on SCID assessment. Chi-square analyses were used to compare the groups. PTSD= Post-traumatic Stress Disorder.
Significance level: two-tailed tests; p<.05*, p<.01**, p<.001***.
Notably, only 3 (6.5%) participants endorsing suicidal thinking met criteria for current major depression episode. There were no Veterans with Bipolar disorder (I or II), among participants reporting suicidal thoughts and one in each category among Veterans not reporting suicidal thinking. There were minimal reports of concurrent use of sedative hypnotics, cannabis, stimulants, opioid, cocaine, hallucinogens/phencyclidine.
Lifetime prevalence for major depression, dysthymia, panic disorder, post-traumatic stress disorder, and alcohol abuse was higher among Veterans endorsing suicidal thoughts (see Table 3). Psychotic symptoms were 4 times more frequent among Veterans endorsing suicidal thoughts (Table 3). Generalized anxiety disorder (GAD) rates were also higher among Veterans reporting suicidal thoughts [11% vs 1.4% met criteria for GAD, Χ (2)= 8.4, p<.02, r=.21]. No Veterans with suicidal thoughts had a history of bipolar disorder I or II (one with BPAD I and one with BPAD II among Veterans without suicidal thoughts). Among Veterans endorsing suicidal thoughts, none met lifetime criteria for a mood disorder due to a general medical condition (1 among Veterans not endorsing suicidal thoughts), whereas 2 Veterans endorsing suicidal thoughts (4.2%, versus 1 or .7% not endorsing suicide thoughts) had a history of substance-induced mood disorder [Χ (2)=3.2, p>.2, r=.13]. There were no significant group effects (and low rates, 5% or less) of sedative hypnotics or anxiolytics, stimulants, opioids, cocaine, hallucinogens (including PCP) or multi substance abuse. Six (or 13.7%) Veterans with suicide thoughts admitted to lifetime use of marijuana compared with 9 (or 6.5%) among Veterans without suicide thoughts [Χ (2)=2.3, p>.3, r=.11]. Among participants endorsing suicidal ideation, only 5 (11.5%) had a family history for any psychiatric disorder, compared to 22 (18.5%) among participants not endorsing suicidal ideation [Χ (1)=1.3, p>.2, r=.08]. Family diagnosis of dementia or substance misuse also did not discriminate between participants with and without suicidal thoughts.
Table 3.
Lifetime psychiatric disorders
| No Suicide Thoughts (N=139) | Suicide Thoughts (N=46) | |||
|---|---|---|---|---|
|
| ||||
| N | % | N | % | |
| Major depression* | ||||
| Absent | 100 | 80.3% | 28 | 60.9% |
| Uncertain | 4 | 2.9% | 5 | 10.9% |
| Present | 23 | 16.5% | 13 | 28.3% |
| Dysthymic Disorder* | ||||
| Absent | 135 | 97.1% | 40 | 87% |
| Uncertain | 0 | 0% | 1 | 2.2% |
| Present | 4 | 2.9% | 5 | 10.9% |
| Psychotic symptoms* | ||||
| Absent | 134 | 96.4% | 39 | 84.8% |
| Uncertain | 1 | .7% | 1 | 2.2% |
| Present | 4 | 2.9 | 6 | 13.0% |
| Panic disorder ** | ||||
| Absent | 124 | 89.2% | 32 | 69.6% |
| Uncertain | 8 | 5.8% | 4 | 8.7% |
| Present | 6 | 4.3% | 10 | 21.7% |
| PTSD*** | ||||
| Absent | 78 | 56.1% | 13 | 28.3% |
| Uncertain | 27 | 19.4% | 6 | 13.0% |
| Present | 33 | 23.7% | 27 | 58.7% |
| Alcohol abuse* | ||||
| Absent | 74 | 53.2% | 15 | 32.6% |
| Uncertain | 36 | 27.3% | 21 | 45.7% |
| Present | 24 | 17.3% | 9 | 19.6% |
Note. Chi-square analyses were used to compare the groups.
Significance level: p<.05*, p<.01**, p<.001***.
Twenty-one (47.7%) participants endorsing suicidal thoughts were taking psychotropic medications (i.e., antidepressants or anxiolytics) compared to 19.5% participants who did not endorse suicidal thinking. Ten (22.7%) were taking 1 psychotropic (vs. 16 or 12.3% of participants not endorsing suicidal ideation), and 11 (25%) were taking 2 or more psychotropic medications (vs. 8 or 6.2% among participants not endorsing suicidal ideation) [Χ (2)=16.9, p<.001, r=.3]. Eleven (25%) participants endorsing suicidal thinking took one anticonvulsant/ mood stabilizer medication and 5 (11.4%) took 2 or more, whereas 18 (13.8%) among participants not endorsing suicidal thinking took 1 and 6 (4.6%) took 2 or more [Χ (2)=6.2, p<.05, r=.18]. Among participants endorsing suicidal thinking 7 (15.9%) used either one opioid drug or another type of medication favoring sleep and 5 (11.4%) took at least two. This compared to 12 (9.2%) and 6 (4.6%) among participants not endorsing suicidal ideation [Χ (2)=4.4, p>.1, r=.15]. There were no participants who reported taking stimulant medications. In summary, these findings suggest that a substantial number of participants endorsing suicidal thoughts were detected and treated using medications. Data on the number of participants that were undergoing psychological therapy was unavailable.
Suicidal Ideation and Emotional Competence
Principal component analysis on all MSCEIT tasks yielded a 2-factor solution explaining cumulatively 55.3% of the variance (Table 4). The model converged after three iterations. Factor 1 (Emotion Processing) explained 37.2% of the variance. There were high loadings for this factor for the tasks Understanding Emotions: Blends and Changes and for the task Managing Emotions: social management (0.73–0.82). Factor 2 (Emotion Perception) explained 18.1% of the variance. For the Emotion Perception Factor 2, the highest loadings were found for the Perceiving Emotions: Faces and Pictures Tasks (0.73–0.87).
Table 4.
Principal component analysis of MSCEIT tasks
| Component
| ||
|---|---|---|
| Task Type | 1: Emotion Processing | 2: Emotion Perception |
| Perceiving Emotions | ||
| Faces | −.06 | .87 |
| Pictures | .34 | .73 |
| Using Emotions | ||
| Sensations | .64 | .29 |
| Facilitation | .51 | .11 |
| Understanding Emotions | ||
| Blends | .76 | .05 |
| Changes | .82 | −.11 |
| Managing Emotions | ||
| Emotion Management | .64 | .15 |
| Social Management | .73 | .16 |
Notes. Extraction Method: Principal Component Analysis. Rotation Method: Varimax with Kaiser Normalization. Rotation converged in 3 iterations.
A logistic regression model was computed with suicidal thoughts as the dependent variable and MSCEIT Factors 1 and 2 as the independent variables. In this model, Factor 1 (Emotion Processing) was significantly associated with suicidal thoughts [Χ=−0.47, SE=0.21, Wald Chi-square (1)=4.9, p=.03]. Factor 2 (Emotion Perception) was not associated with suicidal thoughts [Χ=0.16, SE=0.19, Wald Chi-square (1) =0.7, p=.4)], see Table 5.
Table 5.
Logistic regression model predicting suicidal thinking using MSCEIT factors
| Predictors | B | S.E. | Wald | df | p-value | Exp (B) |
|---|---|---|---|---|---|---|
| Emotion Processing | −.47 | .21 | 4.97 | 1 | .03 | .62 |
| Emotion Perception | .16 | .19 | .69 | 1 | .41 | 1.17 |
Education was significantly correlated with MSCEIT Factor 1 (Emotion Processing) (r=.36, p<.001) but not with Factor 2 (r=−.05, p>.4). Age was significantly correlated with MSCEIT Factor 1 (r=.25, p=.001) but not with Factor 2 (r=−.07, p>.3).
To address the specificity of these results, factors derived from the principal component analysis based on the theory of mind tasks were fitted into a model predicting suicidal thinking. A principal component analysis was conducted on the faux pas task including Comprehension story/ comprehension question, comprehension story/faux pas question, faux pas story/comprehension question, and faux pas story/faux pas question scores) and Happé tasks (based on Physical response story and Theory of Mind scores). This analysis yielded a 2-factor solution explaining 61.8% of the variance. Factor 1 explained 46.2 % of the variance and was composed of all tasks except for the Comprehension story and Faux Pas question task. Factor 2 explained 19.1 % of the variance and included the Comprehension story and Faux Pas question. A logistic regression model was computed with suicidal thinking as the dependent variable and theory of mind Factors 1 and 2 as the independent variables. Factor 1 [Χ= 0.95 (SE=0.19), Wald Chi-square (1) =0.25, p=.6] and 2 [Χ=−0.28 (SE=0.16), Wald Chi-square (1) = 2.9, p=.09] were not significantly associated with suicidal thoughts. Education was significantly correlated with theory of mind Factor 1 (r=.35, p<.001) but not Factor 2 (r=.09, p>.2). Age was not significantly correlated with theory of mind Factor 1 (r=.03, p>.6) and Factor 2 (r=.06, p>.4). In summary, whereas competence in understanding, using and managing emotional tasks (Emotion Processing) predicted suicidal thinking, emotion perception and theory of mind tasks did not. Correlations showed that competence with emotion processing tasks was partially influenced by age and education.
Discussion
In this study, we hypothesized that Veterans who endorsed suicidal thinking over the previous two weeks would have poorer emotional competence than Veterans who did not endorse suicidal thinking. Consistent with this hypothesis, participants endorsing suicidal thoughts showed poorer performance on emotional competence tasks measuring emotion understanding, emotion facilitation, and management. There were no significant group differences in the ability to detect basic emotions, or to predict others’ mental states. Veterans endorsing suicidal thinking were deployed at younger age, had relatively lower education, and tended to report more negative experiences in social interactions upon return to the US. They did not experience significantly more combat exposure or front line location in the battlefield.
Concurrent and lifetime psychiatric diagnoses (including major depression, PTSD and alcoholism) were significantly associated with reported suicide thinking, but the effects were small to moderate. This result is consistent with a recent comprehensive review (Black, Gallaway, Bell, & Ritchie, 2011) suggesting that the majority of army soldiers who committed suicide did not have a documented psychiatric illness, contrary to findings among civilians (Maris, Berman, & Silverman, 2000). However, dimensional severity of depression and anxiety was greater among Veterans endorsing suicide thoughts and these effects were large (Table 1). This finding is consistent with the importance of aggressively treating PTSD and major depression among users of the Veterans Health Administration System to establish the most effective suicide prevention efforts (Conner et al., 2014).
Some limitations should be acknowledged. First, suicide thoughts were endorsed as occurring up to 2 weeks before or at the time of emotional competence assessment (Beck et al., 1996). Contrary to many naturalistic settings, participants were frequently in contact with VHIS staff. This may have reduced the rates of suicidal thoughts. In addition, Veterans who endorsed suicidal thinking with intention were likely to be helped in the mental health clinic and therefore did not get to complete the MSCEIT. Because many Veterans had substantial combat exposure and a brain injury, these results cannot be generalized to all Veterans. The study design was not suited to address directionality of findings, thus cognitive alterations associated with depression might have caused weaker emotional competence. Absence of group differences in FSIQ, theory of mind and basic emotional competence tasks suggest that the suicide thoughts endorsing group was not generally cognitively weaker relative to the non-suicide thoughts endorsing group.
According to E.S. Shneidman, mental anguish sharply separates the minds of individuals who do and do not contemplate suicide (Shneidman, 1996). An individual’s resolve to turn thoughts into action (suicidal intention) depends on level of hope, disinhibition, cultural and religious believes and perceived stigma to name a few. Suicidal thoughts convey anguish and desperation generating an “idea of death (nothingness, cessation) as the solution (Shneidman, 1996, page 8): a clear difficulty finding alternative avenues to manage highly emotional situations. The personal emotional situations of returning Veterans are challenging, but prior to the present study there was no evidence that Veterans endorsing suicidal thoughts may have poor ability to process, use and manipulate non-personal emotional material.
The relationship between emotional competence and suicidal thinking comes from two lines of research. One shows that socioemotional perception may be altered in individuals with a history of suicide attempts (Szanto et al., 2012), suggesting that emotional skills may help preventing suicidal thinking during depression (Abdollahi & Talib, 2015). The second line of research suggests that suicidal thoughts may stem from Veterans’ perception to be a burden to family and society (Monteith et al., 2015). Poor management of emotional situations may occur when returning to a civilian status (Brenner et al., 2009).These views are consistent with recent research showing that negative affects are experimentally less easily induced among people with higher emotional intelligence, which also facilitates returning to a positive emotional baseline (Limonero et al., 2015).
One of the strengths of this study is the empirical demonstration that weaker emotional competence is associated with endorsement of thoughts of suicide. Individuals who endorsed thoughts of ending their life demonstrated poor understanding, usage and management of complex (e.g., appreciating what mood would be appropriate while delivering bad news to a colleague, Figure 1B) emotional stimuli and situations. Critically, the present research is important because it shows that performance-based skills in handling emotional material (vs. personality characteristics or attitudes, prone to subjective report bias) are associated with reported suicidal thinking. In addition, this finding was quite specific because basic emotion perception (perception of the emotion portrayed in a human face, Figure 1A) and non-emotional theory of mind tasks were not significantly associated with endorsed suicidal thoughts.
Elderly suicide attempters with poorer emotion perception have shown signs of poor social functioning including, “struggle against others, hostility in relationships, and perceived lack of social support” (Szanto et al., 2012 – page 262). Similarly, Vietnam Veterans admitting to suicidal thinking reported experiencing more negative social reactions upon returning from deployment. The latter association was all the more striking because the negative social reactions Veterans reported experiencing occurred some thirty years before. The literature suggests that pre-enlistment psychological disturbance may play a significant role in suicide attempts (Nock et al., 2014). Was poorer emotional competence present prior to deployment among Veterans who endorsed suicidal thoughts? Correlations with demographic variables suggest a cautious “yes”. Because of the moderate significant association between emotional competence and years of education, and because Veterans endorsing suicide thinking were on average less educated, some degree of emotional competence deficit might have preceded deployment. In addition, the positive association between age and emotional competence together with the result that Veterans admitting to having suicide thoughts were younger at deployment suggests that as a group Veterans endorsing suicide thinking had relatively weaker emotional competence skills at the outset. Thus, it is purported that poor emotional competence constitutes part of the foundation that may lead to suicidal thinking (and not vice versa), such that poor ability to manage or regulate negatively charged circumstances might lead to suicidal tendencies.
There is evidence that emotional intelligence (Bar-On, 2004) can be taught with effects lasting beyond the teaching period (Dugan, Weatherly, Girod, Barber, & Tsue, 2014; Zijlmans, Embregts, Gerits, Bosman, & Derksen, 2015). Improving emotional skills improves emotional coping, but also benefits individuals who meet people who learned emotional intelligence skills, as shown by the improvement in satisfaction among patients who encountered emotionally trained clinicians (Dugan et al., 2014).
Improved emotional intelligence has positive effects on psychiatric conditions. Four weeks and twelve training sessions helped patients with borderline personality disorder to enhance emotional competence and to a significant decrease in depression (Jahangard et al. 2012). Programs for teaching emotional competence in school age children exist (Stone & Dillehunt, 1978; Shure & Spivack, 1982; Greenberg, Kusche, Cook, & Quamma, 1995), but skills-based emotional competence can be taught in adulthood. Learning of skills-based emotional competence has lasting effects on adult psychosocial adaptation and personal health (Nelis et al., 2011; Kotsou, Nelis, Grégoire, & Mikolajczak, 2011).
Future research may investigate if teaching emotional competence may also improve Veterans’ sense of agency (i.e., a sense of efficacy and being in control of one’s life) which has been directly associated with military personnel’s lower emotional distress and severity of suicidal ideation (Bryan et al., 2014). Active-duty military service members with a past history of suicide intention or attempts benefitted from as little as twelve outpatient individual cognitive behavioral psychotherapy sessions with about a 60% reduction of suicide attempts in the two years following therapy (Rudd et al., 2015). These findings are encouraging for the design and development of research to evaluate prospectively effects of enhanced emotional competence on suicide thinking and behavior.
Conclusions
In summary, the present study found that Vietnam Veterans who reported suicidal thoughts showed difficulty comprehending, using, and managing complex emotional material. Weaker emotional competence may have limited their ability to manage psychosocial challenges and negatively affected their social interactions upon returning from deployment. Failure to cope with emotionally challenging events may have induced thoughts of suicide as a means of reducing emotional pain.
Acknowledgments
Supported by the US National Institute of Neurological Disorders and Stroke intramural research program and a project grant from the US Army Medical Research and Material Command administered by the Henry M. Jackson Foundation (Vietnam Head Injury Study Phase III: a 30-year postinjury follow-up study - DAMD17-01-1-0675).
Contributor Information
Sergio Paradiso, Una Mano per la Vita, Association of Families and their Doctors, Catania, Italy; Nucleo UDP – Fundacion Ineco para las Neurosciencias (NUFIN), Univesidad Diego Portales, Santiago, Chile.
Janelle Beadle, Department of Gerontology, University of Nebraska at Omaha.
Vanessa Raymont, Centre for Mental Health, Department of Medicine, Imperial College London, UK.
Jordan Grafman, Brain Injury Research Cognitive Neuroscience Laboratory Rehabilitation Institute of Chicago; Department of Physical Medicine & Rehabilitation, Neurology, Cognitive Neurology and Alzheimer’s Center, Department of Psychiatry, Feinberg School of Medicine & Department of Psychology, Weinberg College of Arts and Sciences Northwestern University, Chicago, Illinois.
References
- Anonymous. Armed Forces Qualification Test. 1960. (AFQT-7A). Department of Defense Form 1293. [Google Scholar]
- Abdollahi A, Talib MA. Emotional intelligence as a mediator between rumination and suicidal ideation among depressed inpatients: The moderating role of suicidal history. Psychiatry Research. 2015;30:591–597. doi: 10.1016/j.psychres.2015.05.046. http://dx.doi.org/10.1016/j.psychres.2015.05.046. [DOI] [PubMed] [Google Scholar]
- Barbey AK, Colom R, Grafman J. Distributed neural system for emotional intelligence revealed by lesion mapping. Social Cognitive Affective Neuroscience. 2014;9:265–72. doi: 10.1093/scan/nss124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-On R. The Bar-On Emotional Quotient Inventory (EQ-i): Rationale, description and psychometric properties. In: Geher G, editor. Measuring emotional intelligence: Common ground and controversy. Hauppauge, NY: Nova Science; 2004. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-Second Edition (BDI-II) The Psychological Corporation; San Antonio: TX: 1996. [Google Scholar]
- Black SA, Gallaway MS, Bell MR, Ritchie EC. Prevalence and risk factors associated with suicides of army soldiers 2001–2009. Military Psychology. 2011;23:433–451. doi: 10.1080/08995605.2011.590409. [DOI] [Google Scholar]
- Brackett MA, Mayer JD, Warner RM. Emotional intelligence and its relation to everyday behavior. Personality and Individual Differences. 2004;36(6):1387–1402. doi: 10.1016/S0191-8869(03)00236-8. [DOI] [Google Scholar]
- Brenner LA, Homaifar BY, Adler LE, Wolfman JH, Kemp J. Suicidality and veterans with a history of traumatic brain injury: precipitants events, protective factors, and prevention strategies. Rehabilitation Psychology. 2009;54:390–397. doi: 10.1037/a0017802. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E, Etienne N, Ray-Sannerud BN, Morrow CE, … Young-McCaughon S. Improving the detection and prediction of suicidal behavior among military personnel by measuring suicidal beliefs: An evaluation of the Suicide Cognitions Scale. Journal of Affective Disorders. 2014;159:15–22. doi: 10.1016/j.jad.2014.02.021. Epub 2014 Feb 19. [DOI] [PubMed] [Google Scholar]
- Caruso DR, Mayer JD, Salovey P. Relation of an ability measure of emotional intelligence to personality. Journal of Personality Assessment. 2002;79:306–320. doi: 10.1207/S15327752JPA7902_12. [DOI] [PubMed] [Google Scholar]
- Cabello R, Navarro Bravo B, Latorre JM, Fernández-Berrocal P. Ability of university level education to prevent age-related decline in emotional intelligence. Frontiers in Aging Neuroscience. 2014;6(37):1–7. doi: 10.3389/fnagi.2014.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caveness WF, Meirowsky AM, Rish BL, Mohr JP, Kistler JP, Dillon D, Weiss GH. The nature of posttraumatic epilepsy. Journal of Neurosurgery. 1979;50:545–553. doi: 10.3171/jns.1979.50.5.0545. [DOI] [PubMed] [Google Scholar]
- Conner KR, Bossarte RM, He H, Arora J, Lu N, Tu XM, … Katz IR. Posttraumatic stress disorder and suicide in 5.9 million individuals receiving care in the veterans health administration system. Journal of Affective Disorders. 2014;166:1–5. doi: 10.1016/j.jad.2014.04.067. [DOI] [PubMed] [Google Scholar]
- Dugan JW, Weatherly RA, Girod DA, Barber CE, Tsue TT. A longitudinal study of emotional intelligence training for otolaryngology residents and faculty. JAMA Otolaryngol Head Neck Surg. 2014;140:720–6. doi: 10.1001/jamaoto.2014.1169. [DOI] [PubMed] [Google Scholar]
- Extremera N, Fernández-Berrocal P. Relation of perceived emotional intelligence and health-related quality of life of middle-aged women. Psychological Reports. 2002;91:47–59. doi: 10.2466/pr0.2002.91.1.47. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorder, Non-Patient Edition. American Psychiatric Association; Washington, DC: 2002. [Google Scholar]
- Greenberg MT, Kusche CA, Cook ET, Quamma JP. Promoting emotional competence in school-aged children: The effects of the PATHS curriculum. Development and Psychopathology. 1995;7:117–136. doi: 10.1017/S0954579400006374. [DOI] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Happé FG. An advanced test of theory of mind: Understanding of story characters' thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. Journal of Autism and Developmental Disorders. 1994;24:129–154. doi: 10.1007/BF02172093. O162-32.S7/94/MOO-0129SO7.O0/0. [DOI] [PubMed] [Google Scholar]
- Isometsä E, Henriksson M, Marttunen M, Heikkinen M, Aro H, Kuoppasalmi K, … Lönnqvist J. Mental disorders in young and middle aged men who commit suicide. British Medical Journal. 1995;310:1366–1367. doi: 10.1136/bmj.310.6991.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangard L, Haghighi M, Bajoghli H, Ahmadpanah M, Ghaleiha A, Zarrabian MK, … Brand S. Training emotional intelligence improves both emotional intelligence and depressive symptoms in inpatients with borderline personality disorder and depression. International Journal Psychiatry Clinical Practice. 2012;16:197–204. doi: 10.3109/13651501.2012.687454. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- Kang HK, Bullman TA, Smolenski DJ, Skopp NA, Gahm GA, Reger MA. Suicide risk among 1.3 million veterans who were on active duty during the Iraq and Afghanistan wars. Annals of Epidemiology. 2015;25:96–100. doi: 10.1016/j.annepidem.2014.11.020. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Warner CH, Ivany C, Petukhova MV, Rose S, Bromet EJ … Army STARRS Collaborators. Predicting suicides after psychiatric hospitalization in US Army soldiers: the Army study to assess risk and resilience in service members (Army STARRS) Journal of the American Medical Association Psychiatry. 2015;72:49–57. doi: 10.1001/jamapsychiatry.2014.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotsou I, Nelis D, Grégoire J, Mikolajczak M. Emotional plasticity: Conditions and effects of improving emotional competence in adulthood. Journal of Applied Psychology. 2011;96:827–39. doi: 10.1037/a0023047. [DOI] [PubMed] [Google Scholar]
- Krueger F, Barbey AK, McCabe K, Strenziok M, Zamboni G, Solomon J, … Grafman J. The neural bases of key competencies of emotional intelligence. Proceedings of National Academy of Science. 2009;106:22486–91. doi: 10.1073/pnas.0912568106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuipers P, Lancaster A. Developing a suicide prevention strategy based on the perspectives of people with brain injuries. Journal of Head Trauma Rehabilitation. 2000;15:1275–1284. doi: 10.1097/00001199-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Lanciano T, Curci A. Does Emotions Communication Ability Affect Psychological Well-Being? A Study with the Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) v2.0. Health Community. 2015;30:1112–21. doi: 10.1080/10410236.2014.921753. [DOI] [PubMed] [Google Scholar]
- Landy F. Some historical and scientific issues related to research on emotional intelligence. Journal of Organizational Behavior. 2005;26:411–424. doi: 10.1002/job.317. [DOI] [Google Scholar]
- Leopold A, Krueger F, dal Monte O, Pardini M, Pulaski SJ, Solomon J, … Grafman J. Damage to the left ventromedial prefrontal cortex impacts affective theory of mind. Social Cognitive Affective Neuroscience. 2012;7:871–80. doi: 10.1093/scan/nsr071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limonero JT, Tomás-Sábado J, Fernández-Castro J, Gómez-Benito J. Influencia de la inteligencia emocional percibida en el estrés laboral de enfermería. Ansiedad Estrés. 2004;10:29–41. [Google Scholar]
- Limonero JT, Tomás-Sábado J, Fernández-Castro J. Relación entre inteligencia emocional percibida y ansiedad ante la muerte en estudiantes universitarios. Ansiedad Estrés. 2006a;12:267–278. [Google Scholar]
- Limonero JT, Tomás-Sábado J, Fernández-Castro J. Perceived emotional intelligence and its relation to tobacco and cannabis use among university students. Psicothema. 2006b;18(Suppl):95–100. [PubMed] [Google Scholar]
- Limonero JT, Tomás-Sábado J, Fernández-Castro J, Gómez-Romero MJ, Aradilla-Herrero A. Estrategias de afrontamiento resilientes y regulación emocional: Predictores de satisfacción con la vida. Psicologia Conductual. 2012;20:183–196. [Google Scholar]
- Maris RW, Berman AL, Silverman MM. Comprehensive Textbook of Suicidality. Guilford Press; New York: NY: 2000. [Google Scholar]
- Mayer JD, Salovey P. What is emotional intelligence? In: Salovey P, Sluyter D, editors. Emotional development and emotional intelligence: Implications for educators. New York: Basic Books; 1997. pp. 3–31. [Google Scholar]
- Mayer JD, Salovey P, Caruso DR. Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) user's manual. MHS Publishers; Toronto, Ontario, Canada: 2002. [Google Scholar]
- Mayer JD, Salovey P, Caruso DR, Sitarenios G. Measuring Emotional Intelligence With the MSCEIT V2.0. Emotion. 2003;3:97–105. doi: 10.1037/1528-3542.3.1.97. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P, Caruso DR. Emotional intelligence: Theory, findings, and implications. Psychological Inquiry. 2004;15:197–215. [Google Scholar]
- Mayer JD, Salovey P, Caruso DR. Emotional intelligence: new ability or eclectic traits? The American Psychologist. 2008;63:503–517. doi: 10.1037/0003-055x.63.6.503. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Roberts RD, Barsade SG. Human abilities: Emotional intelligence. Annual Review of Psychology. 2008;59:507–536. doi: 10.1146/annurev.psych.59.103006.093646. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P, Caruso DR. The validity of the MSCEIT: Additional analyses and evidence. Emotion Review. 2012;4:403–408. doi: 10.1177/1754073912445815. [DOI] [Google Scholar]
- McNamara D. Preventing Army suicides: A call for help. Clinical Psychiatry News. 2010 Jun;38(6) doi: 10.1016/S0270-6644(10)70246-0. [DOI] [Google Scholar]
- Monteith LL, Pease JL, Forster JE, Homaifar BY, Bahraini NH. Values as moderators of the association between interpersonal-psychological constructs and suicidal ideation among Veterans. Archives of Suicide Research. 2015;19:422–34. doi: 10.1080/13811118.2015.1004486. [DOI] [PubMed] [Google Scholar]
- Nelis D, Kotsou I, Quoidbach J, Hansenne M, Weytens F, Dupuis P, … Mikolajczak M. Increasing emotional competence improves psychological and physical well-being, social relationships, and employability. Emotion. 2011;11:354–66. doi: 10.1037/a0021554. [DOI] [PubMed] [Google Scholar]
- Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS … Army STARRS Collaborators. Prevalence and correlates of suicidal behavior among soldiers: Results from the Army study to assess risk and resilience in service members (Army STARRS) Journal of American Medical Association Psychiatry. 2014;71:514–22. doi: 10.1001/jamapsychiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymont V, Salazar AM, Krueger F, Grafman J. "Studying injured minds" - the Vietnam head injury study and 40 years of brain injury research. Frontiers in Neurology. 2011;2:1–13. doi: 10.3389/fneur.2011.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie EC. Suicide and the United States Army: Perspectives from the Former Psychiatry Consultant to the Army Surgeon General. Cerebrum. 2012 Jan; [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Guillaume S, Olie E, Courtet P, Jollant F. Altered explicit recognition of facial disgust associated with predisposition to suicidal behavior but not depression. Journal of Affective Disorders. 2013;150:590–593. doi: 10.1016/j.jad.2013.01.049. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Bryan CJ, Wertenberger EG, Peterson AL, Young-McCaughan S, Mintz J, … Bruce TO. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: Results of a randomized clinical trial with 2-year follow-up. American Journal of Psychiatry. 2015;172:441–449. doi: 10.1176/appi.ajp.2014.14070843. [DOI] [PubMed] [Google Scholar]
- Schmitz WM, Jr, Allen MH, Feldman BN, Gutin NJ, Jahn DR, Kleespies PM, … Simpson S. Preventing suicide through improved training in suicide risk assessment and care: An American Association of Suicidology task force report addressing serious gaps in U.S. mental health training. Suicide & life-threatening behavior. 2012;3:292–304. doi: 10.1111/j.1943-278X.2012.00090.x. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. What do suicides have in common? In: Bongar B, editor. Suicide – Guidelines for Assessment, management, and treatment. Oxford University Press; New York, Oxford: 1992. [Google Scholar]
- Shneidman ES. The Suicidal Mind. Oxford University Press; New York, Oxford: 1996. [Google Scholar]
- Stone KF, Dillehunt HQ. Self Science: The Subject Is Me. Santa Monica, CA: Goodyear Publishing Company; 1978. [Google Scholar]
- Shure MB, Spivack G. Interpersonal problem-solving in young children: a cognitive approach to prevention. American Journal of Community Psychology. 1982;10:341–56. doi: 10.1007/BF00896500. [DOI] [PubMed] [Google Scholar]
- Szanto K, Dombrovski AY, Sahakian BJ, Mulsant BH, Houck PR, Reynolds CF, … Clark L. Social emotion recognition, social functioning, and attempted suicide in late-life depression. American Journal of Geriatric Psychiatry. 2012;20:257–65. doi: 10.1097/JGP.0b013e31820eea0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Intelligence Scale. 3. The Psychological Corporation; San Antonio, TX: 1997. [Google Scholar]
- Vergare MJ, Binder RL, Cook IA, Galanter M, Lu FG. Practice Guideline for the Psychiatric Evaluation of Adults. 2 2006. [Google Scholar]
- Zijlmans LJ, Embregts PJ, Gerits L, Bosman AM, Derksen JJ. The effectiveness of staff training focused on increasing emotional intelligence and improving interaction between support staff and clients. Journal of Intellectual Disabilities Research. 2015;59:599–612. doi: 10.1111/jir.12164. [DOI] [PubMed] [Google Scholar]