Abstract
Recent advances in hip arthroscopy offer an approach for treating an uncommon but highly disabling injury from intra-articular missile injury to the hip. Hip arthroscopy affords the patient the benefit of minimally invasive surgery while allowing for the diagnosis and treatment of concomitant pathology, which may be either acute, from the trauma of the missile, or chronic. We present a technique for the removal of projectiles from the central and peripheral compartments of the hip joint. Through a surgical series of a variety of gunshot wounds, we detail the unique aspects of retrieval for the various missile endpoints. We describe this technique for bullets or pieces of bullets lodged within the hip joint space, bone of the acetabulum, or femoral head. Furthermore, we provide an example in which hip arthroscopy is not a suitable option for treatment because of the resulting fracture pattern, which necessitates open reduction along with internal fixation.
Arthroscopic extraction of a bullet and bullet fragments in patients who have sustained a gunshot wound and retained the missile within the hip joint was first introduced in 1998.1 Seven cases that underwent arthroscopic removal of retained intra-articular missile fragments in the hip have been published since the index article.1, 2, 3, 4, 5 Of these 7 patients, 4 were treated exclusively by arthroscopy whereas the other 3 were treated with a combination of arthroscopic and open procedures.1, 2, 3, 4, 5 We present an arthroscopic-only surgical technique that has been safe and reproducible in 4 patients.
Preoperative planning with plain films and computed tomography is used to identify the location of bullet fragments and additional pathology (Fig 1). The trajectory and final location of the missile influence the ballistic pathology. The missile may be located free-floating within the joint, located peri-articularly, or lodged within the bone of the acetabulum or femoral head.
Fig 1.
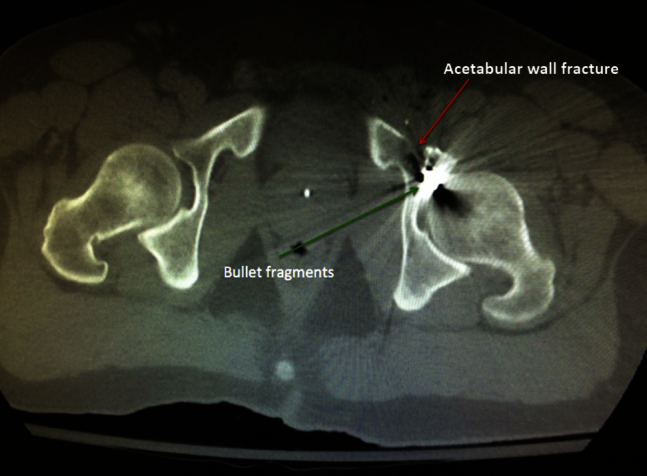
Preoperative axial computed tomography scan showing an anteroinferior acetabular wall fracture (red arrow) and missile fragments (green arrow) extending from the peripheral compartment to the central compartment across the fracture line.
© 2016 Allston J. Stubbs
Fracture stability should be considered before application of traction to the hip joint because traction may displace some fracture patterns. Arthroscopy affords the surgeon the ability to assess fracture stability directly in a traction-based environment within the central compartment and a traction-less environment within the peripheral compartment. In our first case example, the bullet was partially lodged within the femoral head with an associated nondisplaced femoral head fracture.6 Because of exposure to the synovial fluid and the risk of plumbism,7 the bullet was removed without further displacement of the femoral head fracture. Missiles that are enveloped by the bone of the femoral head without exposure to the hip joint may be left alone. In our third case, the missile traversed perpendicularly to the femoral head and neck junction, and traction-less hip arthroscopy of the peripheral compartment was performed to assess the femoral neck bone stability before lower extremity traction was applied for central-compartment evaluation.6
Surgical Technique
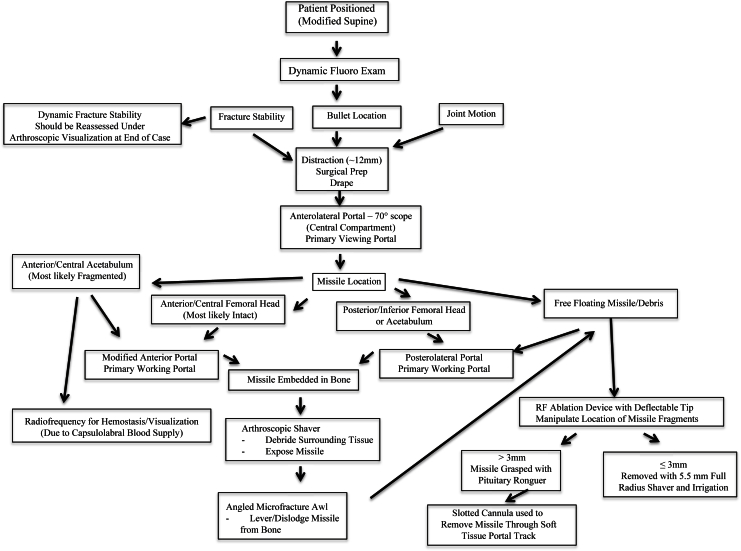
The patient is placed in the modified supine position on a fracture table (OrthoVision; Steris, Mentor, OH). A dynamic fluoroscopic examination is performed to assess bullet fragment location, joint motion, and fracture stability (Fig 2). Next, under fluoroscopic guidance, the operative hip is carefully distracted approximately 12 mm and prepared and draped according to a standard protocol.8 The anterolateral portal is established and used as the primary viewing portal with a 70° arthroscope (Smith & Nephew, Andover, MA). The fluid pressure is maintained between 40 and 60 mm Hg with 1:10,000 dilute epinephrine in lactated Ringer irrigation solution at a flow rate of less than 1 L/min. Unless there is potential for an unstable fracture pattern, the central compartment of the hip is first assessed under traction. The peripheral compartment is evaluated after the removal of traction. We recommend a standardized and consistently reproducible method of performing diagnostic arthroscopy to inspect all central- and peripheral-compartment anatomy. During the diagnostic portion of the case, the missile location and subsequent pathology determine the best position for the primary instrumentation portal. Missiles lodged in the anterior or central aspects of the femoral head or acetabulum are best addressed with a modified anterior working portal and an anterolateral camera portal. In contrast, a posterolateral working portal and anterolateral camera portal permit the best access to posterior/inferior femoral head pathology as well as free-floating missiles and associated debris that settles along the posterior acetabular articular surface—a common position for settling of foreign debris in a traumatized, bed-bound patient.
Fig 2.
Flow diagram for surgical technique based on missile location. (Fluoro, fluoroscopic; Prep, preparation; RF, radiofrequency.)
© 2016 Allston J. Stubbs and Elizabeth A. Howse
Femoral Head and Neck Bullets
Femoral head bullets that have violated the hip joint through the acetabulum leave a debris field along the acetabulum but maintain primary integrity. With the 70° arthroscope, the exposed bullet is viewed from the anterolateral portal. An arthroscopic shaver is used to help expose the embedded missile and debride surrounding tissue (Fig 3). The bullet is dislodged by use of an angled microfracture awl (Arthrex, Naples, FL) around the perimeter of the missile fragment to lever the fragment out of the acetabulum (Fig 4, Video 1). To prevent fragmentation of the soft missile's malleable metal, the bullet should be levered out of the cartilage or bone rather than directly grasped. A one-quarter–inch curved osteotome may be used instead of a microfracture awl to dislodge the missile fragment if the surgeon can achieve an appropriate angle from the working portal; however, most osteotomes are too large for effective maneuverability in hip arthroscopy. Once the fragment is dislodged from the femoral head, it is removed from the joint with a pituitary rongeur (Surgipro, Shawnee, KS), which is used through a slotted cannula (Smith & Nephew). Most missile fragments are frequently larger than the diameters of the standard arthroscopy cannulas; thus, we recommend a slotted cannula (Smith & Nephew) to provide a soft-tissue channel or track to guide removal of the bullet and arthroscopic instrument from the joint through the soft tissue to the skin for retrieval. A hip arthroscopy radiofrequency ablation device with a deflectable tip (Smith & Nephew) may also be used to manipulate fragments within the joint to facilitate arthroscopic capture in the narrow hip joint space (Fig 5).
Fig 3.
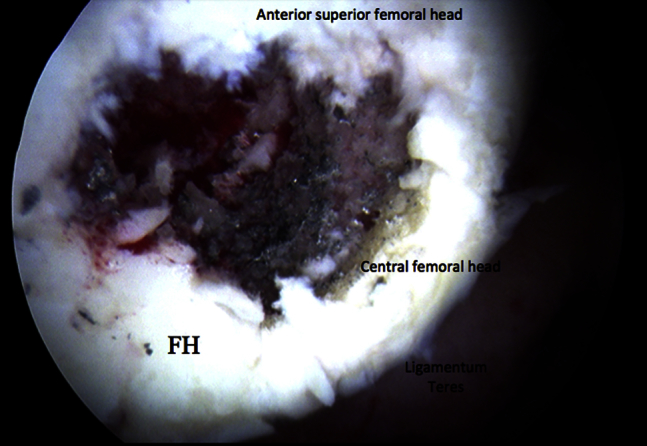
Residual metallic debris and residue in the femoral head (FH) along the path of the bullet, best debrided with a shaver, visualized through the anterolateral portal.
© 2016 Allston J. Stubbs
Fig 4.
Peripheral-compartment view showing a microfracture pick being used as a hook and elevator.
© 2016 Allston J. Stubbs
Fig 5.
Flexible radiofrequency device used for hemostasis and mobilizing fragments in the peripheral compartment.
© 2016 Allston J. Stubbs
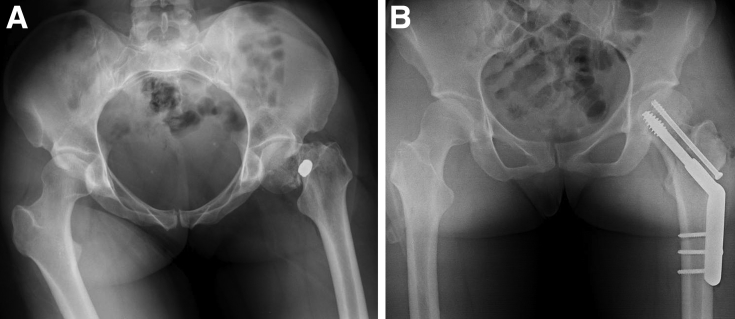
Bullet violation of the femoral neck in younger patients has potentially catastrophic consequences, which may necessitate emergent open reduction–internal fixation rather than an arthroscopic approach (Fig 6). In situations in which less than 30% of the neck has been affected by bullet trauma,9 as in case 3 in our study, we used tractionless arthroscopy to assess the femoral neck for stability as well as the medial femoral circumflex terminal vessels for integrity. With the hip flexed to 40°, peripheral-compartment access is initiated with the 70° arthroscope in the modified anterior portal and instrumentation from the anterolateral portal. Debris removal is achieved with a 5.5-mm full-radius arthroscopic shaver (Smith & Nephew), with greater flow achieved through a 5.5-mm inflow cannula (Smith & Nephew) around the arthroscope. Similar to the central compartment, the flexible-tip radiofrequency ablation probe can facilitate fragment retrieval. Finally, dynamic assessment under direct arthroscopic visualization confirms femoral neck stability with the patient under anesthesia. In cases of femoral neck instability or suspected instability, the surgeon can proceed with femoral neck operative fixation with the patient in the supine position.
Fig 6.
(A) Preoperative anteroposterior pelvis view showing a left femoral neck fracture due to a gunshot wound. (B) Postoperative anteroposterior pelvis view showing open removal of the missile and treatment of the fracture with a dynamic hip screw. Arthroscopy was not indicated in this missile trauma case.
© 2016 Allston J. Stubbs
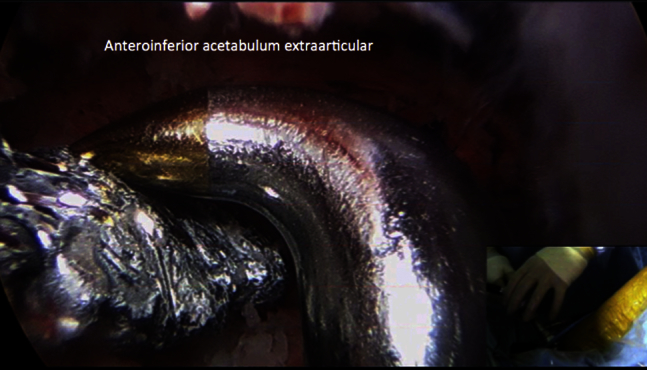
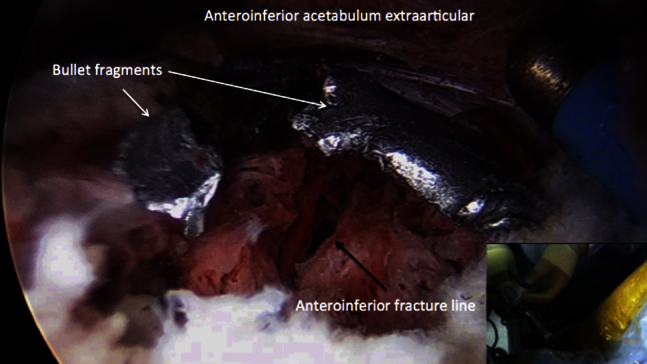
Acetabular Bullets
In contrast to bullets lodged in the femoral head, acetabulum-based bullets break more easily into 2 or more larger bullet fragments with associated bone, cartilage, and metallic debris. Bullet removal may involve central- and peripheral-compartment foreign-body extraction. We recommend an initial evaluation from the central compartment under traction to address central-compartment pathology. As seen in our fourth case, we used our knowledge of the central-compartment ballistic pathology along the anterior acetabular wall to localize and retrieve bullet fragments from the peripheral compartment. Similar to the situation in the central compartment, the angled microfracture awls are an efficient tool for levering bullet fragments lodged in bone without disturbing surrounding bone architecture. The pituitary rongeur (Surgipro) and slotted cannula (Smith & Nephew) are used to remove bullet fragments from the peripheral compartment and surrounding soft tissues that do not fit through standard arthroscopic cannulas and shavers. Because the acetabular labrum receives most of its blood supply from the capsulolabral interface, a flexible radiofrequency device is an essential tool to provide hemostasis and visualization during local debridement and fragment extraction.
Free-Floating Bullets
With the patient in the supine position, free-floating missile and osteochondral fragments will settle along the posterior acetabular wall. These free-floating fragments can be accessed by use of a posterolateral working portal. The size of these fragments determines the approach for removal. Fragments measuring less than 3 mm are removed with a 4.5- or 5.5-mm full-radius arthroscopic shaver. Fragments measuring greater than 3 mm are removed with a pituitary rongeur assisted by a slotted cannula through the large soft-tissue envelope about the hip.
Post-Extraction Procedures
Regardless of initial missile position and method for extraction of the missile fragments, all fragments are saved for complete accounting of an exploded missile and forensic examination. After missile extraction, any additional interventions are performed as needed. After arthroscopic removal of the missile fragments and treatment of concurrent pathology, the surgeon will likely have irrigated and debrided the joint with over 4 L of saline solution and, thereby, decreased the risk of infection (Table 1).
Table 1.
Pearls and Pitfalls of Surgical Technique
| Pearls |
| Minimally invasive technique for bullet extraction without open surgical dislocation |
| Treatment of concomitant pathology (labral tears, chondromalacia) to reduce risk of future pain and advancing pathology |
| Irrigation of contaminated joint space |
| Balloting of femoral head with a probe to assess for avascular necrosis or chondral injury/softening |
| Evaluation of medial femoral circumflex artery terminal branches |
| Pitfalls |
| Lack of Foley catheter contributing to suboptimal fluid management |
| Lack of routine abdominal examinations to assess for fluid extravasation |
| Lack of preoperative assessment of neurovascular function in affected extremity |
| Failure to identify and remove all missile fragments |
| Displacement of nondisplaced fractures of proximal femur or acetabulum |
© 2016 Allston J. Stubbs
The portal sites are closed with No. 3-0 Monocryl sutures (Ethicon, Somerville, NJ) in an inverted fashion of the subcutaneous tissue. A soft dressing is placed about the hip. Postoperative weight bearing is determined by the concomitant presence of acetabular fractures, osteochondral defects undergoing microfracture, labral repairs, and additional chondral defects. A standard postoperative protocol is used with a 20-lb touch-down weight-bearing restriction and use of an anti-rotation bolster pillow for 2 to 8 weeks depending on the extent of operative interventions and, if applicable, fracture pattern.
Discussion
The need for missile extraction from a joint is well-established. A retained missile or missile fragments can cause short- and long-term arthropathy and additional sequelae such as plumbism.7 However, hip arthroscopy for the extraction of bullets and bullet fragments is a relatively new surgical technique.1 Compared with open arthrotomy, hip arthroscopy allows for an expedited recovery because of its minimally invasive nature and minimized iatrogenic trauma to a hip that has already sustained the insult of a gunshot wound.1, 2, 3, 4, 5
Our all-arthroscopic surgical technique has been reproducible and efficacious in 4 patients who each had a different bullet trajectory and unique associated pathology. Arthroscopic extraction of bullets in and about the hip joint has several benefits: (1) it is minimally invasive, which decreases additional trauma and tissue disruption; (2) it ensures substantial irrigation of the hip joint, thus reducing the risk of joint sepsis; and (3) it allows for treatment of concurrent pathology.1, 2, 3, 4, 5
A known complication of hip arthroscopy is the potential for extravasation of fluid into the abdomen.10, 11 Fluid extravasation may cause abdominal pain and may potentially cause abdominal compartment syndrome, resulting in cardiac arrest, as well as extravasation of fluid beyond the abdomen and into the thoracic cavity.10, 11 Kocher et al.11 performed a cohort study of 15 expert hip arthroscopists (who had performed a total of 25,648 hip arthroscopies) to determine the potential risk of fluid extravasation. They reported 40 cases of fluid extravasation (0.1% of cases) and determined that iliopsoas tenotomy and capsulotomy were risk factors for the development of fluid extravasation. They also showed that the sequence of surgical procedures played a role in the likelihood of fluid extravasation and that increased pump pressure was also likely a contributing factor. Al-Asiri and Wong,5 in their case of arthroscopic missile removal from the acetabulum, maintained a pump pressure of 20 mm Hg to minimize the potential risk of fluid extravasation through the fracture line.12 In our technique, we maintained a pump pressure of 40 to 60 mm Hg, without complications of fluid extravasation. All surgeons performing hip arthroscopy should be aware of the risk of fluid extravasation and should be aware that this risk is likely higher because of communication along bullet tracts connecting the abdomen, pelvis, and hip joint. As an example of this potential issue, 3 of our 4 patients underwent an exploratory laparotomy before arthroscopy related to associated bullet injury to the abdomen.
Hip arthroscopy provides a minimally invasive and efficient method for treating retained intra-articular missile fragments. Our technique highlights the use of several instruments for missile removal and provides pearls for reducing iatrogenic insult during hip surgery.
Footnotes
The authors report the following potential conflict of interest or source of funding: S.M. receives support from Wake Forest Innovations Spark Award for development of rotator cuff repair device (Co-PI: S.M., Christopher J. Tuohy; co-investigator: Michael T. Freehill); Orthopaedic Research and Education Foundation (OREF) Resident Clinician Scientist Award (PI: S.M.). S.M. has submitted Utility Patent Application No. 8,926,626 B2 for “Tissue tensioning devices and related methods.” A.J.S. receives support from Smith & Nephew Endoscopy, Wake Forest Baptist Health, Bauerfeind, and Johnson & Johnson.
Supplementary Data
Arthroscopic removal of missiles from two patients' left hips. For each procedure, the patient was placed in the modified supine position. In the first patient, the missile was extracted from the central compartment. The microfracture pick was used to dislodge the missile embedded in the patient's femoral head. In the second example, the missile was removed from the peripheral compartment through the modified anterior portal.
© 2016 Allston J. Stubbs and Elizabeth A. Howse
References
- 1.Cory J.W., Ruch D.S. Arthroscopic removal of a .44 caliber bullet from the hip. Arthroscopy. 1998;14:624–626. doi: 10.1016/s0749-8063(98)70061-1. [DOI] [PubMed] [Google Scholar]
- 2.Teloken M.A., Schmietd I., Tomlinson D.P. Hip arthroscopy: A unique inferomedial approach to bullet removal. Arthroscopy. 2002;18:E21. doi: 10.1053/jars.2002.32232. [DOI] [PubMed] [Google Scholar]
- 3.Mineo R.C., Gittins M.E. Arthroscopic removal of a bullet embedded in the acetabulum. Arthroscopy. 2003;19:E121–E124. doi: 10.1016/j.arthro.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 4.Singleton S.B., Joshi A., Schwartz M.A., Collinge C.A. Arthroscopic bullet removal from the acetabulum. Arthroscopy. 2005;21:360–364. doi: 10.1016/j.arthro.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 5.Al-Asiri J., Wong I. Arthroscopic bullet removal from the acetabulum (hip joint) J Surg Tech Case Rep. 2012;4:121–125. doi: 10.4103/2006-8808.110260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dienst M., Gödde S., Seil R., Hammer D., Kohn D. Hip arthroscopy without traction: In vivo anatomy of the peripheral hip joint cavity. Arthroscopy. 2001;17:924–931. doi: 10.1053/jars.2001.25342. [DOI] [PubMed] [Google Scholar]
- 7.Miller A.N., Carroll E.A., Pilson H.T. Transabdominal gunshot wounds of the hip and pelvis. J Am Acad Orthop Surg. 2013;21:286–292. doi: 10.5435/JAAOS-21-05-286. [DOI] [PubMed] [Google Scholar]
- 8.Mannava S., Howse E.A., Stone A.V. Basic hip arthroscopy: Supine patient positioning and dynamic fluoroscopic evaluation. Arthrosc Tech. 2015;4:e391–e396. doi: 10.1016/j.eats.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mardones R., Gonzalez C., Cabanela M.E., Trousdale R.T., Berry D.J. Extended femoral osteotomy for revision of hip arthroplasty: Results and complications. J Arthroplasty. 2005;20:79–83. doi: 10.1016/j.arth.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Verma M., Sekiya J.K. Intrathoracic fluid extravasation after hip arthroscopy. Arthroscopy. 2010;26(suppl):S90–S94. doi: 10.1016/j.arthro.2010.02.019. [DOI] [PubMed] [Google Scholar]
- 11.Kocher M.S., Frank J.S., Nasreddine A.Y. Intra-abdominal fluid extravasation during hip arthroscopy: A survey of the MAHORN group. Arthroscopy. 2012;28:1654–1660.e2. doi: 10.1016/j.arthro.2012.04.151. [DOI] [PubMed] [Google Scholar]
- 12.Bartlett C.S., DiFelice G.S., Buly R.L., Quinn T.J., Green D.S., Helfet D.L. Cardiac arrest as a result of intraabdominal extravasation of fluid during arthroscopic removal of a loose body from the hip joint of a patient with an acetabular fracture. J Orthop Trauma. 1998;12:294–299. doi: 10.1097/00005131-199805000-00014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic removal of missiles from two patients' left hips. For each procedure, the patient was placed in the modified supine position. In the first patient, the missile was extracted from the central compartment. The microfracture pick was used to dislodge the missile embedded in the patient's femoral head. In the second example, the missile was removed from the peripheral compartment through the modified anterior portal.
© 2016 Allston J. Stubbs and Elizabeth A. Howse