Abstract
Burkholderia mallei is the causative agent of glanders, an incapacitating disease with high mortality rates in respiratory cases. Its endemicity and ineffective treatment options emphasize its public health threat and highlight the need for a vaccine. Live attenuated vaccines are considered the most viable vaccine strategy for Burkholderia, but single-gene-deletion mutants have not provided complete protection. In this study, we constructed the select-agent-excluded B. mallei ΔtonB Δhcp1 (CLH001) vaccine strain and investigated its ability to protect against acute respiratory glanders. Here we show that CLH001 is attenuated, safe, and effective at protecting against lethal B. mallei challenge. Intranasal administration of CLH001 to BALB/c and NOD SCID gamma (NSG) mice resulted in complete survival without detectable colonization or abnormal organ histopathology. Additionally, BALB/c mice intranasally immunized with CLH001 in a prime/boost regimen were fully protected against lethal challenge with the B. mallei lux (CSM001) wild-type strain.
INTRODUCTION
Burkholderia mallei, the causative agent of glanders, is a Gram-negative, obligate mammalian pathogen. Glanders is primarily a disease of solipeds, with rare cases occurring among humans (1, 2). Naturally acquired human cases occur in areas of endemicity, particularly among those exposed to infected solipeds (2–4). Additionally, cases have been reported among laboratory workers (5, 6). The World Organization for Animal Health coordinates ongoing efforts toward worldwide eradication; however, regional endemicity still exists in Africa, Asia, the Middle East, and South America (2). Recent equid outbreaks in the Middle East and Asia (7–9) set the stage for possible glanders reintroduction into disease-free regions; as a result, glanders has been classified as a reemerging disease.
Glanders is a debilitating and often fatal disease transmitted via cutaneous and respiratory routes. Disease course and severity are route dependent, with respiratory cases being the most severe (3). Respiratory infection is characterized by rapid onset of symptoms, including fever, lymphadenopathy, pulmonary abscesses, pneumonia, disseminated organ infection, and, ultimately, septicemia (3, 5, 10). Because of the high incidence of septicemia following respiratory infection, fatality rates in human respiratory cases have been estimated at 90% without treatment and 40% with aggressive antibiotic therapy (11).
The use of B. mallei as a biothreat agent has been documented in different world military conflicts (10, 12, 13). Its amenability to aerosolization, low infectious dose, high case fatality rate, and high-level antibiotic resistance make B. mallei a top candidate for malevolent use (1, 10). Because of its perceived public health threat, the Department of Health and Human Services has categorized B. mallei as a tier 1 select agent. The lack of effective treatments against these bacteria highlights the need for an effective vaccine. Numerous vaccine strategies have been tested; however, to date there are no approved vaccines and the search for a candidate that can provide sterilizing immunity has proven difficult.
Live attenuated vaccines, the use of which is regarded as the most viable strategy against B. mallei, have been tested with some success (14–17). Recently, our laboratory evaluated an iron acquisition-deficient B. mallei ΔtonB (TMM001) strain for use as a live attenuated vaccine in acute inhalational glanders and melioidosis (B. pseudomallei) murine models. BALB/c mice intranasally (i.n.) vaccinated with TMM001 at 1.5 × 105 and 1.5 × 104 CFU doses and i.n. challenged with 1.5 × 104 CFU of B. mallei strain lux (CSM001) had survival rates of 100% and 75%, respectively. Necropsy and organ CFU enumeration showed that all mice had splenomegaly and splenic abscesses due to TMM001 colonization (16). This study was significant because it revealed the first attenuated strain to provide 100% and 75% survival against B. mallei and B. pseudomallei challenge, respectively. However, the persistence of TMM001 poses a significant safety concern. In an effort to achieve increased safety while still maintaining protection, we utilized the TMM001 strain as a platform for additional gene deletion.
Type six secretion systems (T6SSs) are highly conserved among Gram-negative bacteria (18, 19), and the essential role of T6SS cluster 1 (T6SS-1) genes in the virulence of B. mallei was demonstrated using rodent models of infection (20). Further, the hemolysin coregulated protein (Hcp1) of T6SS-1 serves as both a structural component and a secreted protein which plays an important role in T6SS-1 function and B. mallei pathogenesis (18, 20, 21). Deletion of the T6SS apparatus components (including the hcp1 gene) resulted in B. mallei and B. pseudomallei mutants that exhibited significant impairment in intracellular growth, intracellular spread, and multinucleated giant cell (MNGC) formation (21, 22). MNGC formation is characteristic of B. mallei and B. pseudomallei infections and has been detected in eukaryotic cell culture as well as in animal models of infection (21, 23, 24). MNGCs are believed to be involved in the ability of these organisms to establish persistent infections by allowing intracellular spread and immune evasion (1, 22, 25). We predicted that deletion of both the hcp1 and tonB genes of B. mallei would produce a strain more susceptible to host clearance, resulting in a safer and yet fully protective vaccine.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
The bacterial strains used in this study are listed in Table 1. Escherichia coli cells were grown in Luria-Bertani (LB) media at 37°C. All manipulations of B. mallei strains were conducted in CDC-approved and -registered biosafety level 3 (BSL3) or CDC/USDA-approved and -registered animal biosafety level 3 (ABSL3) facilities at the University of Texas Medical Branch, and experiments were performed in accordance with standard select agent operating practices. B. mallei strains were taken from freezer stocks, plated on LB agar containing 4% glycerol (LBG) and 200 μM FeSO4, and incubated 37°C for 3 days. For liquid cultures, 2 to 3 colonies were inoculated into 20 ml of LBG broth. Liquid cultures were then incubated overnight (18 h) at 37°C with agitation (200 rpm). Challenge and vaccination doses were prepared from overnight LBG cultures and diluted in phosphate-buffered saline (PBS) in a total volume of 50 μl (25 μl/naris).
TABLE 1.
Bacterial strains used in this study
| Strain | Relevant featuresa | Reference or source |
|---|---|---|
| B. mallei ATCC 23344 | Human clinical isolate; Kms Pbr | 26 |
| B. mallei CSM001 | B. mallei ATCC 23344 with mini-Tn5::luxKm2; Kmr Pbr | 27 |
| B. mallei TMM001 | B. mallei ATCC 23344 with an unmarked intragenic deletion in bmaa1801 (ΔtonB) | 16 |
| B. mallei CLH001 | B. mallei TMM001 with unmarked intragenic deletion in bmaa0742 (Δhcp1) | This study |
| B. mallei CLH002 | B. mallei ATCC 23344 with an unmarked intragenic deletion of bmaa0742 (Δhcp1) | This study |
| E. coli S17-1 (pMo130-ΔBPSS1498) | Donor strain containing pMo130–Δbpss1498 plasmid; Smr Tpr Pbs Kmr | 22 |
Km, kanamycin; Pb, polymyxin B; Sm, streptomycin; Tp, trimethoprim.
Construction of B. mallei Δhcp1 and ΔtonB Δhcp1 mutants.
The B. mallei ΔtonB Δhcp1 (CLH001) and Δhcp1 (CLH002) mutants were developed using a donor strain and a plasmid strain donated by Mary Burtnick (University of South Alabama). The donor strain was a chemically competent E. coli S17-1 λ pir strain containing a pMo130ΔNX plasmid designed to introduce a 162-bp intragenic in-frame deletion in the hcp1 gene (22). The CLH002 mutant was created by introducing the plasmid from the donor strain into B. mallei 23344 via biparental mating. Deletion mutants were isolated by selection on kanamycin (Km) agar plates, followed by counterselection on 5% sucrose–yeast extract–tryptone (YT) agar supplemented with 200 μM FeSO4. The CLH001 mutant was created by introducing the plasmid into B. mallei TMM001 via conjugal transfer and repeating the screening and confirmation process described above. The Δhcp1 mutation was then confirmed via PCR amplification, followed by sequencing, of the hcp1 gene using the following primers: forward primer, ATG CTG GCC GGA ATA TAT CTC; reverse primer, GCC ATT CGT CCA GTT TGC GG.
Animal studies.
All animal experiments were performed using female 6- to 8-week-old BALB/c mice or NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NOD SCID gamma [NSG]) mice obtained from Charles River (Wilmington, MA, USA). BALB/c mice are a common model for the study of acute B. mallei and B. pseudomallei infections, as BALB/c mice are highly susceptible and succumb to infection at doses which are comparable to those observed in humans. The NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ or NSG mouse is a mutant mouse which combines the severe combined immune deficiency (SCID) mutation and an interleukin-1 (IL-2) receptor gamma chain deficiency which disables cytokine signaling. This is considered the most highly immunocompromised mouse model, as it lacks mature B cells, T cells, and functional NK cells and is deficient in cytokine signaling. As such, this mouse model was used to assess the safety of CLH001 vaccination. Mice were housed in microisolator cages under pathogen-free conditions, provided with rodent feed and water ad libitum, and maintained on a 12-h light cycle. To allow adequate acclimation, mice were housed within the animal facility for 1 week prior to experimentation. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Animal Care and Use Committee of the University of Texas Medical Branch (protocol no. 0503014B).
Survival study.
Anesthetized BALB/c mice (n = 11) were challenged i.n. with 1.5 × 104 CFU of a B. mallei luminescent reporter strain (CSM001) or isogenic mutants TMM001, CLH002, or CLH001. The challenge dose for each strain, 1.5 × 104 CFU, was equivalent to 22 50% lethal doses (LD50) of CSM001. At day 2 postinfection, mice (n = 3) were euthanized and their lungs, livers, and spleens were aseptically harvested for CFU enumeration. The remaining BALB/c mice (n = 8) were monitored for survival for 21 days. Survival curves were generated and analyzed using the Kaplan-Meier method, and significant differences in survival curves were ascertained via a log rank test. At the 21-day experimental endpoint, the surviving animals (n = 8 for the TMM001, CLH001, and CLH002 groups) were euthanized and the lungs, livers, and spleens were aseptically harvested. The lungs, livers, and spleens were plated for CFU enumeration (n = 5) or histopathological evaluation (n = 3).
Immunocompromised mouse survival study.
Anesthetized NSG mice (n = 10) were i.n. challenged with 1.5 × 104 CFU of either CSM001 (n = 4) or CLH001 (n = 6). The challenge dose for each strain, 1.5 × 104 CFU, was equivalent to 22 LD50 of CSM001. The mice were monitored for survival for 21 days. Survival curves were generated and analyzed using the Kaplan-Meier method. Significant differences in survival curves were ascertained via a log rank test. At the 21-day experimental endpoint, the surviving animals (n = 6 for CLH001) were euthanized and the lungs, livers, and spleens were aseptically harvested. Organs were plated for CFU enumeration (n = 4) or histopathological evaluation (n = 2).
Prime and boost vaccination study.
Anesthetized BALB/c mice (n = 11) were administered a series of three i.n. vaccinations consisting of 50 μl PBS or 1.5 × 104 CFU or 1.5 × 105 CFU of CLH001 at 2-week intervals (days −49, −35, and −21 prechallenge). At days −35, −21, and −1 prechallenge, mice (n = 3) were anesthetized and retro-orbital blood was collected for antibody (Ab) analysis. On day 0 prior to challenge, mice (n = 3) were euthanized and lungs, livers, and spleens were aseptically removed. Organs from the PBS-vaccinated mice were submitted for histopathological analysis, and the organs from the CLH001-vaccinated groups were plated for CFU enumeration. The remaining BALB/c mice (n = 8) were i.n. challenged with 1.5 × 104 CFU (22 LD50) of CSM001. BALB/c mice were monitored for survival for 35 days. Survival curves were generated and analyzed using the Kaplan-Meier method. Significant differences (P ≤ 0.05) were ascertained via a log rank test. To determine significant differences in individual treatment results compared to those seen with the PBS-treatment control, an additional log rank test was employed using an adjusted definition of significance (P ≤ 0.05 of pairwise comparisons). At the 35-day experimental endpoint, the surviving animals (n = 5 for CLH001 [1.5 × 104 CFU] and n = 8 for CLH001 [1.5 × 105 CFU]) were euthanized and the organs were aseptically harvested. Lungs, livers, and spleens were plated for CFU enumeration (n = 3 for CLH001 [1.5 × 104 CFU] and n = 5 for CLH001 [1.5 × 105 CFU]) and submitted for histopathological evaluation (n = 2 for CLH001 [1.5 × 104 CFU] and n = 3 for CLH001 [1.5 × 105 CFU]).
High-dose B. mallei ATCC 23344 challenge prime and boost vaccination study.
Anesthetized BALB/c mice (n = 8 for control group and n = 11 for vaccine group) were administered a series of three i.n. vaccinations consisting of 50 μl PBS or 1.5 × 105 CFU of CLH001 at 2-week intervals (days −49, −35, and −21 prechallenge). At days −35, −21, and −1 prechallenge, mice (n = 3) were anesthetized and retro-orbital blood was collected for antibody analysis. On day 0 prior to challenge, mice (n = 3 from the CLH001-vaccinated group and n = 3 from the PBS-vaccinated group) were euthanized and their lungs, livers, and spleens were aseptically removed. Organs from the PBS-vaccinated mice were placed in formalin for histopathological analysis, while organs from the CLH001-vaccinated groups were plated for CFU enumeration. The remaining BALB/c mice (n = 8) were i.n. challenged with 3.5 × 105 CFU (140 LD50) of B. mallei ATCC 23344. BALB/c mice were monitored for survival for 35 days. Survival curves were generated and analyzed using the Kaplan-Meier method. Significant differences (P ≤ 0.05) were ascertained via a log rank test. Additionally, at 35 days (experimental endpoint), the surviving animals (n = 7 from CLH001-vaccinated group) were euthanized and the lungs, livers, and spleens were aseptically harvested and plated for CFU enumeration (n = 4). The remaining sets of organs (n = 3) were placed in formalin for histopathological evaluation.
Organ CFU enumeration.
The lungs, livers, and spleens were homogenized in 1 ml of PBS using a tissue grinder (Covidien, Mansfield, MA). Ten-fold serial dilutions of the homogenate were made in PBS, and 100 μl of each dilution was plated on 100-mm-diameter LBG plates supplemented with 200 μM FeSO4 (LBG with FeSO4). For each organ, 500 μl of the remaining organ homogenate was plated on a 150-mm-diameter LBG plate with FeSO4 to increase culture sensitivity. Since CLH001 contains a ΔtonB mutation that results in poor growth in the absence of free iron supplementation, LBG medium with FeSO4 was used to maximize recovery, if any, of the CLH001 vaccine strain. The resulting plates were incubated for 96 h at 37°C, and their contents were enumerated by a standard plate count method and are reported as CFU per organ. The sensitivity of the plating method for bacterial detection was approximately ≤10 CFU per organ.
Histopathological evaluation.
At the indicated time points, anesthetized BALB/c mice were euthanized and lungs, livers, and spleens were collected. Organs were placed in 10% formalin, paraffin embedded, and processed for histopathology. Hematoxylin-and-eosin-stained slides were examined for the presence or absence of perivascular and peribronchial infiltrates, necrosis, and microabscesses in lungs, granulomas and necrosis in livers, and inflammation and necrosis in spleens and were scored in a blind manner by a pathologist on the basis of disease severity using the following scale: 0, unremarkable; 1, minimal; 2, mild; 3, moderate; 4, severe. Student's t test was performed to ascertain significant differences in histopathological scores between individual treatments compared to the results determined for the PBS treatment control or naive mice for each organ.
B. mallei-specific IgG total, IgG1, and IgG2a antibody analysis.
Whole blood was collected via retro-orbital bleeding of anesthetized BALB/c mice. The blood was stored in Microvette tubes without anti-coagulant and incubated at room temperature for 20 min to permit clotting. Following centrifugation, serum was collected and stored at −80°C. Samples were inactivated by gamma irradiation using a JL Shepherd model 109-68 Cobalt-60 research irradiator (JL Shepherd & Associates, San Fernando, CA). Samples were irradiated on dry ice until 5 megarads (MRAD) of exposure was reached, and sterility was verified by plating 10% of the serum volume on LBG with FeSO4. Irradiated serum from PBS or vaccinated BALB/c mice was evaluated for B. mallei-specific total IgG, IgG1, and IgG2a using an enzyme-linked immunosorbent assay (ELISA) performed in 96-well Costar high-binding microplates (Corning, Inc., Corning, NY). Briefly, irradiated B. mallei was diluted to a concentration of 10 μg/ml in 1× PBS and wells were coated with 100 μl/well of diluted suspension and incubated overnight at 4°C. Wells were washed twice with wash buffer (1× PBS containing 0.05% Tween 20) and incubated with 250 μl of blocking solution (1× PBS, 1% bovine serum albumin, 0.05% Tween 20) for 2 h at room temperature (RT). After blocking, plates were washed twice with wash buffer. Two-fold dilutions of mouse sera were made with sample diluent (1× PBS, 0.5% bovine serum albumin, and 0.05% Tween 20) in triplicate. A 100-μl volume of diluted sera was added to sample wells along with 100 μl of 1:10,000 anti-Ig class or subclass horseradish peroxidase conjugate (Southern Biotechnology Associates, Inc., Birmingham, AL), and plates were incubated at RT for 2 h. The plates were washed four times with wash buffer prior to addition of 100 μl of tetramethylbenzidine (TMB) substrate solution (eBioscience, Inc., San Diego, CA). After 15 min, 100 μl of stop solution (2 N H2SO4) was added and the wells were read at 450 nm using an Epoch microplate spectrophotometer (BioTek Instruments, Inc., Winooski, VT). The results were reported as the reciprocal of the highest titer giving an optical density (OD) reading of at least 0.1, which was at least twice the background ± 1 standard deviation (SD). All assays were performed in triplicate, and results were reported as the mean reciprocal endpoint titer ± SD.
Serum bactericidal assay.
An overnight culture of B. mallei ATCC 23344 was diluted 1:100 in fresh LBG and grown to log phase (OD at 600 nm [OD600] of 0.6). The bacterial concentration was adjusted to 1 × 105 CFU/well in a 96-well plate and incubated with 30% heat-inactivated (56°C for 1 h), pooled strain CLH001 prime and boost vaccine serum (n = 3) or 5 μg/ml anti-B. mallei lipopolysaccharide (LPS) monoclonal antibody (MAb) 3d11 (AbD Serotec, Raleigh, NC) in LBG broth containing 22 μl guinea pig complement (Sigma-Aldrich, St. Louis, MO). Bacteria incubated in LBG broth containing 30% heat-inactivated pooled naive serum (n = 3) and 22 μl guinea pig complement were used as a negative control. After 6 h of incubation (37°C and 135 rpm), 10-fold serial dilutions were plated on 100 mM LBG agar and incubated for 72 h at 37°C. The bacterial counts were reported as CFU counts per milliliter. Each experimental group was assayed in triplicate. Significant differences in bacterial survival between groups were determined using one-way analysis of variance (ANOVA).
RESULTS
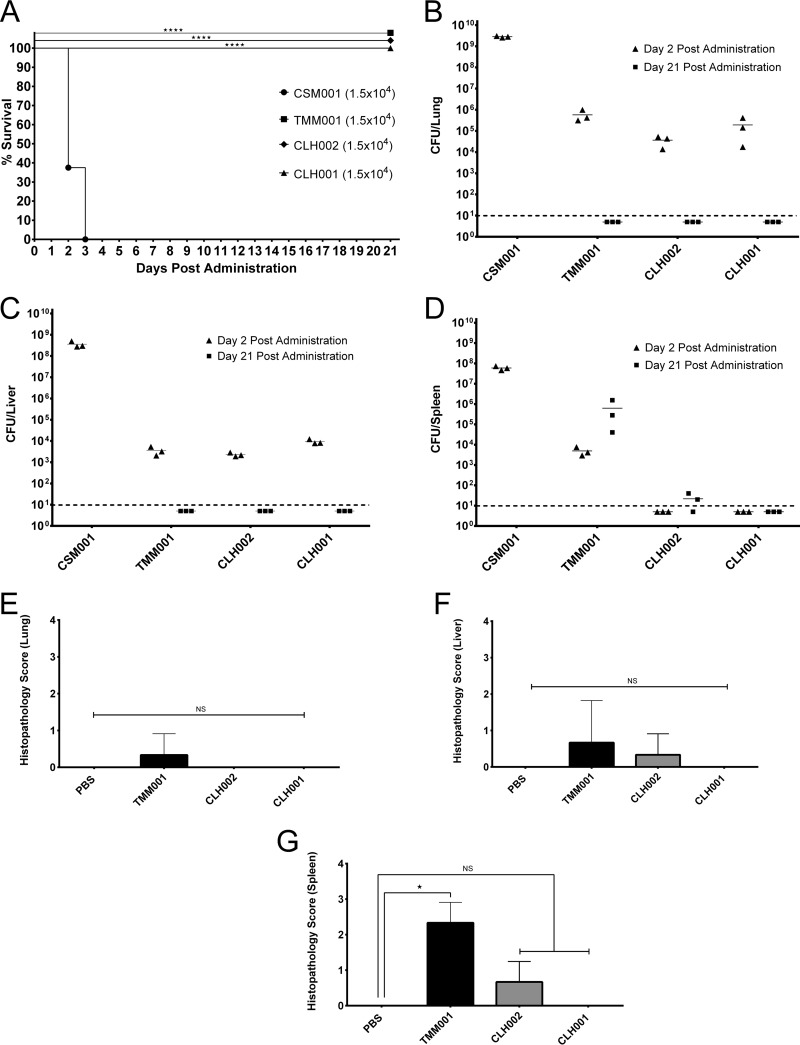
To assess the in vivo attenuation of mutant strains, BALB/c mice were challenged with 1.5 × 104 CFU of B. mallei ΔtonB (TMM001), B. mallei Δhcp1 (CLH002), B. mallei ΔtonB Δhcp1 (CLH001), or highly virulent B. mallei lux (CSM001). The challenge dose for each strain, 1.5 × 104 CFU, was equivalent to 22 LD50 of CSM001. All the animals infected with the CSM001 succumbed to infection by day 3 postchallenge. In contrast, all mice receiving TMM001, CLH002, or CLH001 survived to the end of the study (⭑⋆⭑⋆, P < 0.0001) (Fig. 1A). At days 2 and 21 postchallenge, the lungs, spleens, and livers were removed, homogenized, and plated for CFU enumeration. At day 2 postchallenge, the CFU counts in organs from TMM001-, CLH002-, and CLH001-infected mice were greatly reduced compared to the counts in those from CSM001-infected mice (Fig. 1B to D). At day 21 postchallenge, bacteria were not recovered from the lungs and livers of TMM001-, CLH002-, and CLH001-infected mice (Fig. 1B and C). As previously observed (16), high CFU numbers were recovered from the spleens of TMM001-infected mice (Fig. 1D). In contrast, lower numbers of bacteria were recovered from the spleens of CLH002-infected mice and no bacteria were recovered from the spleens of mice receiving CLH001.
FIG 1.
CLH001 is highly attenuated in BALB/c mice compared to strain CSM001 and exhibits increased safety in comparison to strains TMM001 and CLH002 at day 21 postinfection. (A) Percent survival of BALB/c mice (n = 8) following i.n. challenge with 1.5 × 104 CFU of CSM001 (●), TMM001 (■), CLH002 (◆), or CLH001 (▲) at 21 days postinfection. (B to D) Colonization of mouse lungs (B), livers (C), and spleens (D) (n = 3) at day 2 (▲) and day 21 (■) postinfection with 1.5 × 104 CFU of TMM001, CLH002, or CLH001. The limit of detection was 10 CFU/organ (horizontal dotted line). (E to G) Results of comparisons of histopathological scores for lungs (E), livers (F), and spleens (G) of PBS-treated mice versus mice infected with TMM001, CLH002, or CLH001 (n = 3) at 21 days postinfection. NS, not significant.
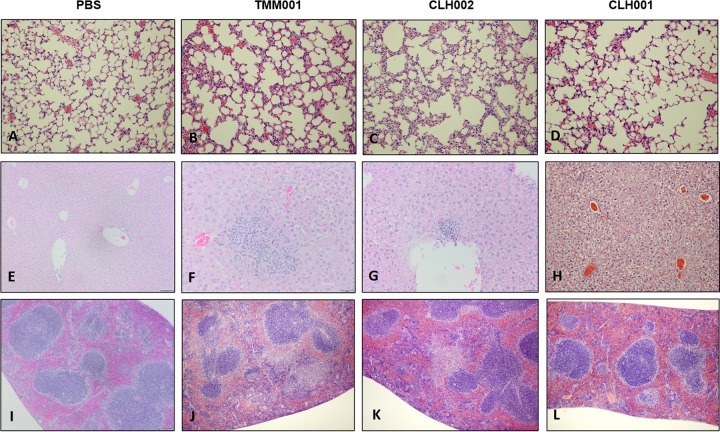
Results of histopathological analysis of the tissues (lungs, livers, and spleens) of mice challenged with the different strains were compared to the results from PBS-treated BALB/c mice (Fig. 2). The organs of TMM001-infected mice presented with mild to moderate pathological changes, including mild perivascular and peribronchial inflammatory infiltrates in the lung sections (Fig. 2B), foci of mild hepatocellular necrosis (Fig. 2F), and mild to moderate necrosis of follicles visible in the spleen (Fig. 2J). While the TMM001 organs generally exhibited increased abnormal findings relative to similar organs from the other treatment groups, only the spleens exhibited significant changes in histopathology compared to spleens from PBS-treated mice (⭑, P = 0.02) (Fig. 1G), and minimal pathological changes were noted in lungs and livers (Fig. 1E and F). Overall, reduced pathological changes were noted in CLH002-challenged mice compared to TMM001-infected mice. The results seen with lungs of CLH002-challenged BALB/c mice were considered mostly unremarkable (Fig. 2C), but the livers and spleens exhibited small foci of necrosis (Fig. 2G and K). In contrast, the results seen with organs of mice vaccinated with CLH001 mutant were unremarkable, and the organs resembled organs from PBS-treated mice (Fig. 2D, H, and L).
FIG 2.
Representative images of organ pathology in challenged mice. Hematoxylin-and-eosin-stained tissues displayed the types of pathology seen in lungs (A to D), livers (E to H), and spleens (I to L) of mice challenged with PBS or 1.5 × 104 CFU of TMM001, CLH002, or CLH001 at 21 days postchallenge.
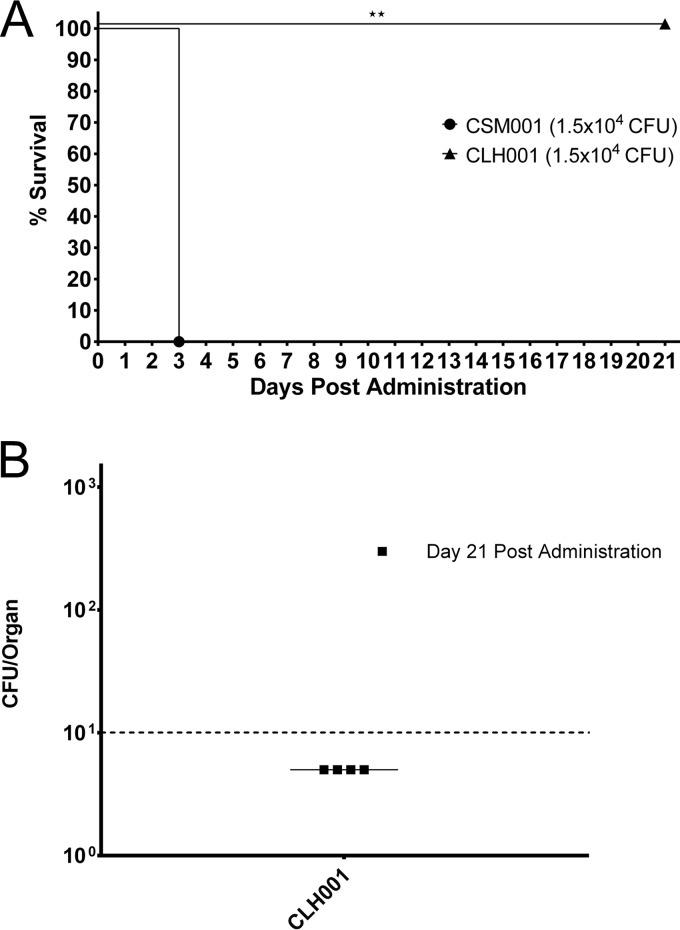
We further evaluated the safety of our CLH001 vaccine in NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NOD SCID gamma [NSG]) mice. The NSG mice are considered the most highly immunodeficient mouse available, and such immunodeficiency provides a practical model to test vaccine-associated morbidity and mortality. NSG mice challenged i.n. with 1.5 × 104 CFU of CSM001 or CLH001 were used to evaluate persistence and/or dissemination to target organs. The challenge dose was equivalent to 22 LD50 of CSM001. All mice challenged with CSM001 (n = 4) succumbed to infection by day 3 postchallenge. In contrast, mice receiving CLH001 (n = 6) survived to the end of the study (⋆⭑, P = 0.0027) (Fig. 3A). At 21 days postchallenge, the organs of surviving mice were evaluated for CFU and no bacteria were detected in the lungs, livers, or spleens (Fig. 3B) of any of the mice. Gross pathology and histology analysis of these organs indicated that the architecture was unremarkable compared to that of organs from an uninfected NSG mouse (data not shown).
FIG 3.
NSG mice infected with CLH001 showed 100% survival and complete bacterial clearance. (A) Percent survival of NSG mice following i.n challenge with 1.5 × 104 CFU of CSM001 (n = 4, ●) or CLH001 (n = 6, ▲) at 21 days postinfection. (B) Colonization of mouse lungs, livers, and spleens (n = 4) at day 21 postinfection with 1.5 × 104 CFU of CLH001 (■). The limit of detection was 10 CFU/organ (horizontal dotted line).
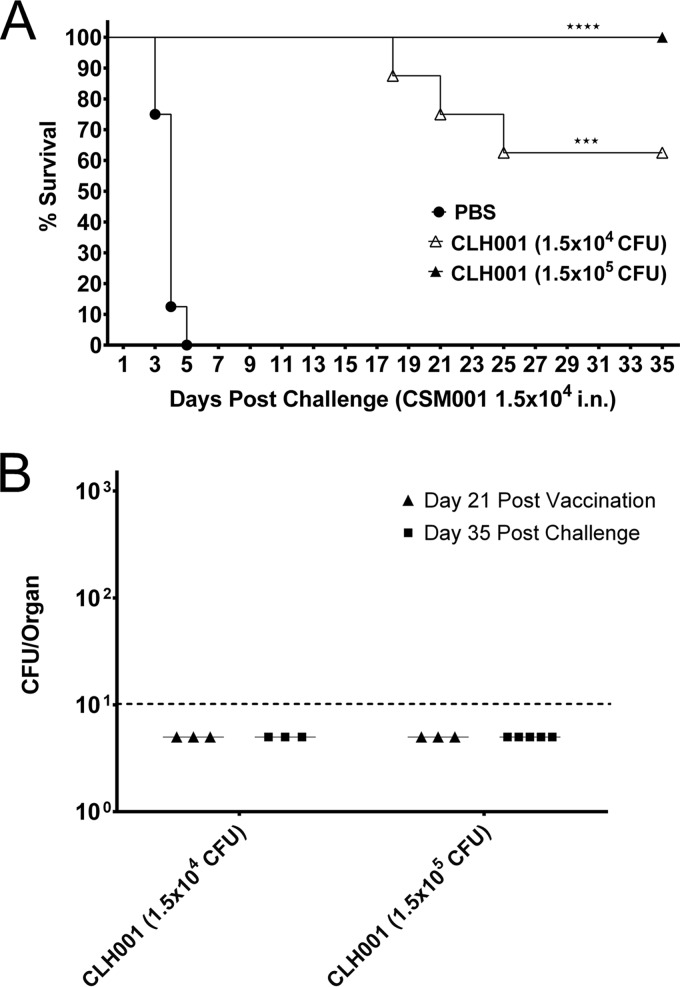
Next, we evaluated whether CLH001 vaccination was protective against a lethal dose of CSM001 in BALB/c mice. Mice received a prime vaccination and two boost vaccinations (14 days apart) with 1.5 × 104 or 1.5 × 105 CFU of CLH001. Serum was collected from mice (n = 3) at 2-week intervals following each prime and boost dose and compared to serum from TMM001-vaccinated mice. B. mallei-specific IgG, IgG2a, and IgG1 reciprocal endpoint titers were determined via indirect ELISA. A retrospective analysis of serum from TMM001-vaccinated mice found that the vaccine generated a strong B. mallei-specific IgG response (mean reciprocal endpoint titer = 51,200 ± 0) with a Th1 bias (IgG2a/IgG1 ratio, 4.4) (Table 2). As predicted, CLH001-vaccinated mice developed an anamnestic response to all antibodies tested following each subsequent CLH001 vaccination at both doses. The sera previously subjected to the CLH001 (1.5 × 105 CFU) prime and two boosts had the highest B. mallei-specific IgG total value for this vaccine and gave values similar to those seen in TMM001-vaccinated mice. Further, the observed ≥4.0 ratio of IgG2a/IgG1 has also been described as being favorable for protection (Table 2) (14, 15, 28, 29). The BALB/c mice vaccinated with the prime and two boosts (PBS at the equivalent of 1.5 × 104 CFU or CLH001 at 1.5 × 105 CFU) were challenged with 1.5 ×104 CFU of CSM001. All PBS-treated mice succumbed to infection by day 5 postchallenge; however, animals vaccinated with the two CLH001 doses exhibited survival rates of 62.5% (⋆⭑⋆, P < 0.0002) and 100% (⭑⋆⭑⋆, P < 0.0001), respectively, at the 35-day experimental endpoint (Fig. 4A).
TABLE 2.
Serum antibody response of BALB/c mice i.n. vaccinated with B. mallei live attenuated strains
| Vaccine/dosage (P, B, or 2B)a | Serum titerb |
IgG2a/IgG1 serum ratio | ||
|---|---|---|---|---|
| IgG | IgG2a | IgG1 | ||
| PBS | ND | ND | ND | |
| TMM001/1.5 × 104 CFU (P) | 51,200 ± 0 | 136,533 ± 48,272 | 31,289 ± 14,504 | 4.4 |
| CLH001/1.5 × 104 CFU (P) | 400 ± 0 | ND | ND | |
| CLH001/1.5 × 105 CFU (P) | 3,733 ± 2,325 | 944 ± 163 | ND | |
| CLH001/1.5 × 104 CFU (B) | 4,267 ± 2,133 | 5,511 ± 473 | 1,422 ± 154 | 3.9 |
| CLH001/1.5 × 105 CFU (B) | 19,200 ± 7,692 | 31,259 ± 7,853 | 8,533 ± 1,742 | 3.7 |
| CLH001/1.5 × 104 CFU (2B) | 19,911 ± 5,321 | 18,489 ± 6,517 | 8,533 ± 3,695 | 2.2 |
| CLH001/1.5 × 105 CFU (2B) | 42,667 ± 6,967 | 96,711 ± 8,533 | 24,178 ± 2,011 | 4 |
Antibody titers were determined at 2 weeks after primary vaccination (P), 2 weeks after first boost (B), and 3 weeks after second boost (2B). PBS control animals were vaccinated with 50 μl of PBS. Data from TMM001-vaccinated animals (prime vaccination only) are included for comparison.
To determine serum antibody titers, sera from 3 mice/group were tested by indirect ELISA with irradiated B. mallei ATCC 23344 whole cells used as the antigen. Titer determinations were performed in triplicate, and data are reported as the mean reciprocal endpoint titers ± standard deviations (SD). ND, not detected, because titers less than or equal to 100 were considered to represent negative results.
FIG 4.
Prime and boost vaccination with CLH001 (1.5 × 105 CFU) provided 100% protection with no discernible organ colonization following CSM001 challenge. (A) Mice were i.n. immunized with a prime and two boosts of PBS (n = 8, ●) or of CLH001 at 1.5 × 104 CFU (n = 11, Δ) or 1.5 × 105 CFU (n = 11, ▲). Three weeks after receiving their second boost, mice were i.n. challenged with 1.5 × 104 CFU (22 LD50) of CSM001. (B) Colonization of mouse lungs, livers, and spleens (n = 3/CLH001 vaccination group) at day 21 after the second vaccination boost (▲) and day 35 postchallenge with CSM001 (n = 3 for the group administered CLH001 at 1.5 × 104 CFU [CLH001 1.5 × 104 group] and n = 4 for CLH0001 1.5 × 105 group, ■). The limit of detection was 10 CFU/organ (horizontal dotted line).
Organs were collected 21 days postvaccination and 35 days postchallenge for CFU enumeration. Bacteria were not detected in the lungs, livers, or spleens (Fig. 4B) of any of the mice tested. Additionally, gross pathology and histology analysis of these organs collected at 35 days postchallenge indicated that the architecture was mostly unremarkable compared to that of organs from PBS-treated uninfected mice (data not shown).
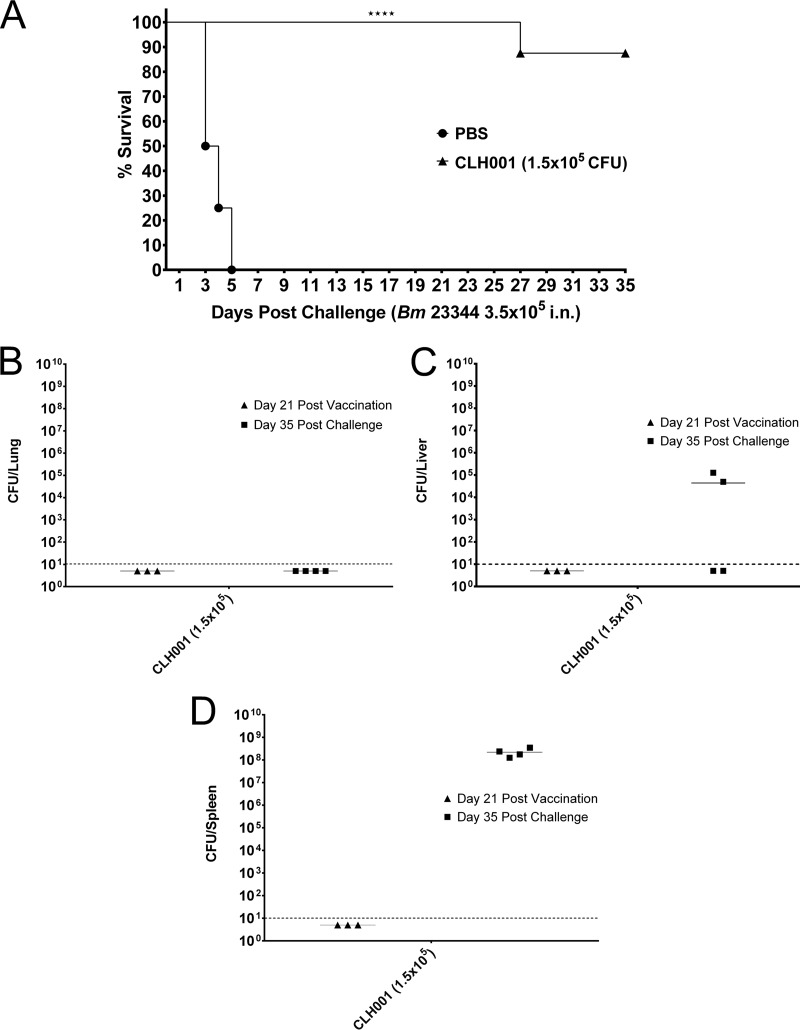
Next, we evaluated whether CLH001 was protective against high-dose challenge with B. mallei wild-type strain ATCC 23344. BALB/c mice were administered a prime and two boosts (14 days apart) with PBS or 1.5 × 105 CFU of CLH001 and were challenged with 3.5 × 105 CFU (140 LD50) of B. mallei 23344 at 21 days after the last vaccine boost. B. mallei-specific IgG, IgG2a, and IgG1 reciprocal endpoint titers from sera collected 2 weeks following each vaccination closely mimicked those seen in the previous vaccination experiment that had used the prime and two boosts (data not shown). All PBS-treated mice succumbed to infection, and survival was maintained at 87.5% (⭑⋆⭑⋆, P < 0.0001) in CLH001-vaccinated mice until the experimental endpoint (Fig. 5A). Although bacteria were not detected in the lungs, livers, or spleens (Fig. 5B) of any of the mice at day 21 postvaccination or in the lungs (Fig. 5B) at day 35 postchallenge, significant bacterial counts were recovered from two of the livers (4.97 × 104 and 1.28 × 105 CFU/organ) (Fig. 5C) and all of the spleens (mean, 3.5 × 108 CFU/organ) (Fig. 5D).
FIG 5.
Vaccination with CLH001 (1.5 × 105 CFU) provided significant protection following a B. mallei (Bm) 23344 high-dose challenge, but bacterial organ colonization was observed. (A) Mice were i.n. immunized with a regimen consisting of a prime and two boosts of PBS (●) (n = 8) or 1.5 × 105 CFU CLH001 (▲) (n = 11). Three weeks after the last boost, mice were i.n. challenged with 3.5 × 105 CFU (140 LD50) of B. mallei 23344. (B to D) Colonization of lungs (B), livers (C), and spleens (D) of CLH001-vaccinated mice at day 21 postvaccination (▲) (n = 3) and day 35 postchallenge (■) (n = 4). The limit of detection was 10 CFU/organ (horizontal dotted line).
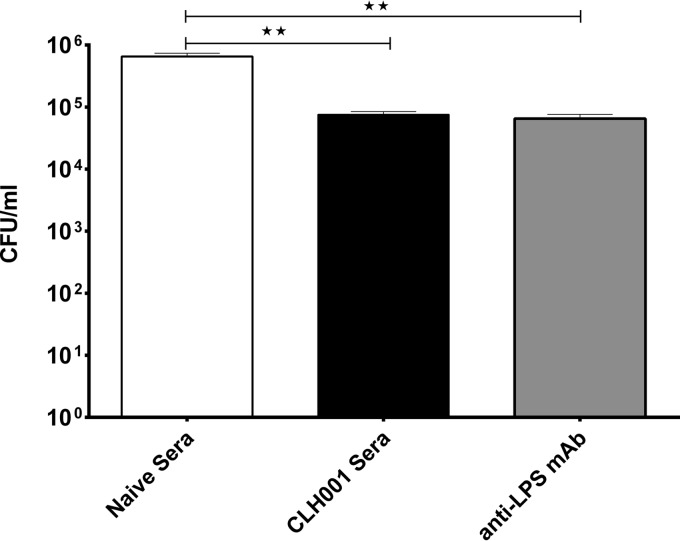
The correlation between higher levels of B. mallei-specific antibodies in animals vaccinated with CLH001 at 1.5 × 105 CFU and increased survival rates led us to hypothesize that antibodies likely play an important role in protection. As such, we performed a serum bactericidal assay to evaluate whether antibodies from CLH001-vaccinated mice were able to reduce bacterial burden. B. mallei ATCC 23344 was incubated in LBG media containing guinea pig complement and one of the following: heat-inactivated naive sera, heat-inactivated CLH001 sera, or anti-B. mallei LPS monoclonal antibody (anti-LPS MAb). The number of bacteria grown in the presence of naive serum indicated nearly a 6-fold increase over the initial bacterial concentration; meanwhile, the number of bacteria grown in the presence of CLH001 sera or anti-LPS MAb decreased below the initial bacterial concentration and represented significantly fewer bacteria than the level in the naive serum culture (⭑⋆, P = 0.0062 and P = 0.0063 for these groups, respectively) (Fig. 6).
FIG 6.
CLH001 serum promotes killing of B. mallei 23344 in vitro. Serum bactericidal assays were performed by incubating 1.0 ×105 CFU of B. mallei 23344 and guinea pig complement plus heat-inactivated naive sera, heat-inactivated CLH001 sera, or anti-B. mallei LPS monoclonal antibody. After 6 h, samples were serially diluted and plated to determine CFU counts per milliliter. Experiments were performed in triplicate.
DISCUSSION
This study evaluated a B. mallei double deletion mutant as a live attenuated vaccine candidate. Overall, our data indicate that the addition of the Δhcp1 deletion to the TMM001 strain was successful in addressing the persistence issue associated with the TMM001 backbone strain (16). In all survival and vaccination studies performed (including the NSG mouse study), the vaccine strain was cleared from all target organs by 21 days postadministration. Additionally, histopathology analysis of target organs from animals receiving this vaccine strain showed unremarkable tissue sections. In this study, we have demonstrated that CLH001 is attenuated in vivo. The additional gene deletion in the CLH001 strain provides increased safety and added protection against wild-type reversion; as a result, this has become the first B. mallei strain to be excluded from the U.S. Federal Select Agent Program. This exclusion provides an obvious advantage by allowing further vaccine characterization and optimization work to be performed more cost effectively and expeditiously in biosafety level 2 laboratories.
Another advantage of this double mutant is that, unlike the TMM001 backbone strain, its attenuation is not solely dependent on the organism's inability to take up bound iron sources. Virulence of the TMM001 strain has been shown to be partially restored when free iron is supplied (16). Approximately 1% of the Caucasian population suffers from hemochromatosis, an inherited genetic defect resulting in excess free iron. Administration of an iron-deficient strain such as TMM001 to this population could potentially result in adverse effects; however, the additional gene deletion in CLH001 eliminates this safety concern. Although not tested for protection against B. mallei challenge, mice given 1.5 × 104 CFU of the CLH002 strain (Δhcp1 mutant) showed 100% survival, complete clearance of the lungs and liver, minimal splenic colonization, and minimal liver and spleen histopathology. Taken together, our results indicate that CLH001 may be sufficiently attenuated to be tolerated if inadvertently administered to this population subset.
A number of vaccine studies have examined the correlation between a vaccine's ability to generate high B. mallei-specific IgG titers and a Th1-driven immune response (IgG2a/IgG1 ratio of ≥1) and its ability to provide protection against B. mallei infection (14, 15, 28, 29). Our report supports the results of those studies, with the greatest protection observed in vaccinated mice (1.5 × 105 CFU of CLH001) with the highest IgG total titers and IgG2a/IgG1 ratios. This correlation, along with the fact that CLH001-vaccinated serum was able to reduce viable bacterial counts when cocultured with B. mallei, provides evidence that this live attenuated vaccine stimulates a strong humoral response that is at least partially responsible for protection. However, it is widely accepted that the generation of a robust but appropriate cellular response is also important for protection (30–33). Therefore, the select agent exclusion status of CLH001 will accelerate experiments to characterize the cellular responses to the vaccine, such as adoptive transfer, T cell recall, and T cell proliferation.
CLH001 represents the first Burkholderia vaccine that approaches sterile immunity against high doses of the B. mallei CSM001 strain. As such, its inability to provide complete protection and prevent colonization with B. mallei ATCC 23344 was unexpected. It is likely that the high challenge dose used was able to overwhelm the immune response generated by CLH001 using our current vaccination regimen. The challenge dose given in this experiment represents a 20-fold increase over the dose of CSM001 bacteria used to challenge in the initial experiment. Although it is evident that further vaccine optimization is required, CLH001 exhibits safety and protection superior to that seen with other previously tested vaccines (30–33). Future optimization will focus on reducing the number of boosts and determining the ideal vaccine dose that will protect against higher dosages of B. mallei 23344 and other B. mallei strains. This vaccine also has the potential to provide cross-protection against other Burkholderia strains, since a pilot study demonstrated that CLH001 was partially protective against a lethal dose of B. pseudomallei K96243 (data not shown). The high antibody titers and significant protection achieved in this study provide a rationale for vaccine optimization, including increasing the CLH001 vaccine dosage, testing alternative vaccination routes, and/or adding an adjuvant to maximize immune responses. Silva et al. demonstrated that administration of a live attenuated vaccine via the subcutaneous route using the closely related organism B. pseudomallei resulted in vigorous recruitment of professional antigen-presenting cells (APCs) and stimulated a robust humoral response capable of providing partial protection against lethal i.n. dose challenge with B. pseudomallei (34). Although it is not clear whether it is superior to i.n. vaccination in terms of protection, this route of vaccination represents a more conventional and acceptable vaccination method that warrants exploration with strain CLH001. Adjuvants are commonly incorporated into vaccine formulations to increase and/or tailor innate, adaptive, and humoral responses. Although our vaccine was not fully protective in the second trial, it is possible that the cellular response elicited by CLH001 was insufficient. Inclusion of the appropriate adjuvant in our vaccination formulation may increase the magnitude of the cellular response generated by CLH001 vaccination alone. One such adjuvant that has shown promise in B. mallei and B. pseudomallei vaccine formulations and prophylactic therapy is CpG oligodeoxynucleotide (CpG ODN) (35, 36). The CpG ODN is a Toll-like receptor 9 (TLR9) agonist that has been shown to activate B and NK cells, stimulate antibody production, and drive Th1 cell development (37). Incorporating an adjuvant such as CpG into our vaccine formulation has the potential to increase protection and reduce the number of required vaccine dosages by stimulating a more robust Th1-biased humoral and cellular response(s). We are confident that continued optimization of this CHL001 strain will result in a live attenuated strain that can be advanced into preclinical studies.
ACKNOWLEDGMENTS
We thank Mary Burtnick at the University of South Alabama for providing us with E. coli S17-1(pMo130-ΔBPSS1498).
C.L.H. was supported by the United States Army's Long Term Health Education and Training (LTHET) Program established under Army regulation 623-1. This study was partially supported by NIH/NIAID grant U54 AI057156 and UTMB seed funds.
The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAID or NIH.
REFERENCES
- 1.Galyov EE, Brett PJ, DeShazer D. 2010. Molecular insights into Burkholderia pseudomallei and Burkholderia mallei pathogenesis. Annu Rev Microbiol 64:495–517. doi: 10.1146/annurev.micro.112408.134030. [DOI] [PubMed] [Google Scholar]
- 2.Khan I, Wieler LH, Melzer F, Elschner MC, Muhammad G, Ali S, Sprague LD, Neubauer H, Saqib M. 2013. Glanders in animals: a review on epidemiology, clinical presentation, diagnosis and countermeasures. Transbound Emerg Dis 60:204–221. doi: 10.1111/j.1865-1682.2012.01342.x. [DOI] [PubMed] [Google Scholar]
- 3.Van Zandt KE, Greer MT, Gelhaus HC. 2013. Glanders: an overview of infection in humans. Orphanet J Rare Dis 8:131. doi: 10.1186/1750-1172-8-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verma AK, Saminathan M, Tiwari R, Dahama K, Singh V. 2014. Glanders—a re-emerging zoonotic disease: a review. J Biol Sci 14:38–51. doi: 10.3923/jbs.2014.38.51. [DOI] [Google Scholar]
- 5.Howe C, Miller WR. 1947. Human glanders; report of six cases. Ann Intern Med 26:93–115. doi: 10.7326/0003-4819-26-1-93. [DOI] [PubMed] [Google Scholar]
- 6.Srinivasan A, Kraus CN, DeShazer D, Becker PM, Dick JD, Spacek L, Bartlett JG, Byrne WR, Thomas DL. 2001. Glanders in a military research microbiologist. N Engl J Med 345:256–258. doi: 10.1056/NEJM200107263450404. [DOI] [PubMed] [Google Scholar]
- 7.Malik P, Singha H, Khurana SK, Kumar R, Kumar S, Raut AA, Riyesh T, Vaid RK, Virmani N, Singh BK, Pathak SV, Parkale DD, Singh B, Pandey SB, Sharma TR, Chauhan BC, Awasthi V, Jain S, Singh RK. 2012. Emergence and re-emergence of glanders in India: a description of outbreaks from 2006 to 2011. Vet Ital 48:167–178. [PubMed] [Google Scholar]
- 8.Hornstra H, Pearson T, Georgia S, Liguori A, Dale J, Price E, O'Neill M, Deshazer D, Muhammad G, Saqib M, Naureen A, Keim P. 2009. Molecular epidemiology of glanders, Pakistan. Emerg Infect Dis 15:2036–2039. doi: 10.3201/eid1512.090738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scholz HC, Pearson T, Hornstra H, Projahn M, Terzioglu R, Wernery R, Georgi E, Riehm JM, Wagner DM, Keim PS, Joseph M, Johnson B, Kinne J, Jose S, Hepp CM, Witte A, Wernery U. 2014. Genotyping of Burkholderia mallei from an outbreak of glanders in Bahrain suggests multiple introduction events. PLoS Negl Trop Dis 8:e3195. doi: 10.1371/journal.pntd.0003195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gregory CG, Waag DM. 2007. Glanders, chapter 6, p 121–146. In Dembek ZF. (ed), Medical aspects of biological warfare. Borden Institute, Walter Reed Army Medical Center, Washington, DC. [Google Scholar]
- 11.Currie BJ. 2010. Burkholderia pseudomallei and Burkholderia mallei: melioidosis and glanders, p 2869–2879. In Mandell GL, Bennett JE, Dolin R (ed), Principles and practice of infectious diseases, 7th ed Churchill Livingston Elsevier, Philadelphia, PA. [Google Scholar]
- 12.Wheelis M. 1998. First shots fired in biological warfare. Nature 395:213. [DOI] [PubMed] [Google Scholar]
- 13.Alibek K, Handelman S. 1999. Biohazard: the chilling true story of the largest covert biological weapons program in the world. Random House, New York, NY. [Google Scholar]
- 14.Ulrich RL, Amemiya K, Waag DM, Roy CJ, DeShazer D. 2005. Aerogenic vaccination with a Burkholderia mallei auxotroph protects against aerosol-initiated glanders in mice. Vaccine 23:1986–1992. doi: 10.1016/j.vaccine.2004.10.017. [DOI] [PubMed] [Google Scholar]
- 15.Bandara AB, DeShazer D, Inzana TJ, Sriranganathan N, Schurig GG, Boyle SM. 2008. A disruption of ctpA encoding carboxy-terminal protease attenuates Burkholderia mallei and induces partial protection in CD1 mice. Microb Pathog 45:207–216. doi: 10.1016/j.micpath.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 16.Mott TM, Vijayakumar S, Sbrana E, Endsley JJ, Torres AG. 2015. Characterization of the Burkholderia mallei tonB mutant and its potential as a backbone strain for vaccine development. PLoS Negl Trop Dis 9:e0003863. doi: 10.1371/journal.pntd.0003863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bozue JA, Chaudhury S, Amemiya K, Chua J, Cote CK, Toothman RG, Dankmeyer JL, Klimko CP, Wilhelmsen CL, Raymond JW, Zavaljevski N, Reifman J, Wallqvist A. 2016. Phenotypic characterization of a novel virulence-factor deletion strain of Burkholderia mallei that provides partial protection against inhalational glanders in mice. Front Cell Infect Microbiol 6:21. doi: 10.3389/fcimb.2016.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mougous JD, Cuff ME, Raunser S, Shen A, Zhou M, Gifford CA, Goodman AL, Joachimiak G, Ordonez CL, Lory S, Walz T, Joachimiak A, Mekalanos JJ. 2006. A virulence locus of Pseudomonas aeruginosa encodes a protein secretion apparatus. Science 312:1526–1530. doi: 10.1126/science.1128393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pukatzki S, Ma AT, Sturtevant D, Krastins B, Sarracino D, Nelson WC, Heidelberg JF, Mekalanos JJ. 2006. Identification of a conserved bacterial protein secretion system in Vibrio cholerae using the Dictyostelium host model system. Proc Natl Acad Sci U S A 103:1528–1533. doi: 10.1073/pnas.0510322103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schell MA, Ulrich RL, Ribot WJ, Brueggemann EE, Hines HB, Chen D, Lipscomb L, Kim HS, Mrazek J, Nierman WC, Deshazer D. 2007. Type VI secretion is a major virulence determinant in Burkholderia mallei. Mol Microbiol 64:1466–1485. doi: 10.1111/j.1365-2958.2007.05734.x. [DOI] [PubMed] [Google Scholar]
- 21.Burtnick MN, DeShazer D, Nair V, Gherardini FC, Brett PJ. 2010. Burkholderia mallei cluster 1 type VI secretion mutants exhibit growth and actin polymerization defects in RAW 264.7 murine macrophages. Infect Immun 78:88–99. doi: 10.1128/IAI.00985-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burtnick MN, Brett PJ, Harding SV, Ngugi SA, Ribot WJ, Chantratita N, Scorpio A, Milne TS, Dean RE, Fritz DL, Peacock SJ, Prior JL, Atkins TP, Deshazer D. 2011. The cluster 1 type VI secretion system is a major virulence determinant in Burkholderia pseudomallei. Infect Immun 79:1512–1525. doi: 10.1128/IAI.01218-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duval CW, White PG. 1907. The Histological lesions of experimental glanders. J Exp Med 9:352–380. doi: 10.1084/jem.9.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harley VS, Dance DA, Drasar BS, Tovey G. 1998. Effects of Burkholderia pseudomallei and other Burkholderia species on eukaryotic cells in tissue culture. Microbios 96:71–93. [PubMed] [Google Scholar]
- 25.Kespichayawattana W, Rattanachetkul S, Wanun T, Utaisincharoen P, Sirisinha S. 2000. Burkholderia pseudomallei induces cell fusion and actin-associated membrane protrusion: a possible mechanism for cell-to-cell spreading. Infect Immun 68:5377–5384. doi: 10.1128/IAI.68.9.5377-5384.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yabuuchi E, Kosako Y, Oyaizu H, Yano I, Hotta H, Hashimoto Y, Ezaki T, Arakawa M. 1992. Proposal of Burkholderia gen. nov. and transfer of seven species of the genus Pseudomonas homology group II to the new genus, with the type species Burkholderia cepacia (Palleroni and Holmes 1981) comb. nov. Microbiol Immunol 36:1251–1275. doi: 10.1111/j.1348-0421.1992.tb02129.x. [DOI] [PubMed] [Google Scholar]
- 27.Massey S, Johnston K, Mott TM, Judy BM, Kvitko BH, Schweizer HP, Estes DM, Torres AG. 2011. In vivo bioluminescence imaging of Burkholderia mallei respiratory infection and treatment in the mouse model. Front Microbiol 2:174. doi: 10.3389/fmicb.2011.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amemiya K, Bush GV, DeShazer D, Waag DM. 2002. Nonviable Burkholderia mallei induces a mixed Th1- and Th2-like cytokine response in BALB/c mice. Infect Immun 70:2319–2325. doi: 10.1128/IAI.70.5.2319-2325.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amemiya K, Meyers JL, Trevino SR, Chanh TC, Norris SL, Waag DM. 2006. Interleukin-12 induces a Th1-like response to Burkholderia mallei and limited protection in BALB/c mice. Vaccine 24:1413–1420. doi: 10.1016/j.vaccine.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 30.Silva EB, Dow SW. 2013. Development of Burkholderia mallei and pseudomallei vaccines. Front Cell Infect Microbiol 3:10. doi: 10.3389/fcimb.2013.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mott TM, Estes DM, Torres AG. 2011. Recent progress in the development of vaccines for glanders and melioidosis, chapter 4, p 93–110. In Feodorova VA, Motin VL (ed), Vaccines against bacterial biothreat pathogens. Research Signpost, Kerala, India. [Google Scholar]
- 32.Bondi SK, Goldberg JB. 2008. Strategies toward vaccines against Burkholderia mallei and Burkholderia pseudomallei. Expert Rev Vaccines 7:1357–1365. doi: 10.1586/14760584.7.9.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choh LC, Ong GH, Vellasamy KM, Kalaiselvam K, Kang WT, Al-Maleki AR, Mariappan V, Vadivelu J. 2013. Burkholderia vaccines: are we moving forward? Front Cell Infect Microbiol 3:5. doi: 10.3389/fcimb.2013.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Silva EB, Goodyear A, Sutherland MD, Podnecky NL, Gonzalez-Juarrero M, Schweizer HP, Dow SW. 2013. Correlates of immune protection following cutaneous immunization with an attenuated Burkholderia pseudomallei vaccine. Infect Immun 81:4626–4634. doi: 10.1128/IAI.00915-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitlock GC, Deeraksa A, Qazi O, Judy BM, Taylor K, Propst KL, Duffy AJ, Johnson K, Kitto GB, Brown KA, Dow SW, Torres AG, Estes DM. 2010. Protective response to subunit vaccination against intranasal Burkholderia mallei and B. pseudomallei challenge. Procedia Vaccinol 2:73–77. doi: 10.1016/j.provac.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Judy BM, Taylor K, Deeraksa A, Johnston RK, Endsley JJ, Vijayakumar S, Aronson JF, Estes DM, Torres AG. 2012. Prophylactic application of CpG oligonucleotides augments the early host response and confers protection in acute melioidosis. PLoS One 7:e34176. doi: 10.1371/journal.pone.0034176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vollmer J, Weeratna R, Payette P, Jurk M, Schetter C, Laucht M, Wader T, Tluk S, Liu M, Davis HL, Krieg AM. 2004. Characterization of three CpG oligodeoxynucleotide classes with distinct immunostimulatory activities. Eur J Immunol 34:251–262. doi: 10.1002/eji.200324032. [DOI] [PubMed] [Google Scholar]