Abstract
Introduction
Falls among older adults (aged ≥65 years) are the leading cause of both injury deaths and emergency department (ED) visits for trauma. We examine the characteristics and prevalence of older adult ED fallers as well as the recurrent ED visit and mortality rate.
Methods
This was a retrospective analysis of a cohort of elderly fall patients who presented to the ED between 2005 and 2011 at two urban, level-1 trauma, teaching hospitals with approximately 80,000-95,000 annual visits. We examined the frequency of ED revisits and death at 3 days, 7 days, 30 days, and 1 year controlling for certain covariates.
Results
Our cohort included 21,340 patients. The average age was 78.6. An increasing proportion of patients revisited the ED over the course of a year, ranging from 2% of patients at 3 days to 25% at 1 year. Death rates increased from 1.2% at 3 days to 15% at 1 year. 10,728 (50.2%) patients returned to the ED at some point during our 7-year study period and 36% of patients had an ED revisit or death within 1 year. In multivariate logistic regression, male sex and comorbidities were associated with ED revisits and death.
Conclusion
Over a third of older adult ED fall patients had an ED revisit or died within one year. Falls are one of the geriatric syndromes that contribute to frequent ED revisits and death rates. Future research should determine whether falls increase the risk of such outcomes and how to prevent future fall and death.
Keywords: geriatrics, emergency care, trauma
1. Introduction
Falls among older adults (aged ≥65 years) are the leading cause of both injury deaths and emergency department (ED) visits for trauma.1 Falls can have devastating and long-term consequences for older adults including reduced mobility, loss of independence, and premature death.2 Each year, falls are responsible for more than 20,000 deaths and 2.3 million ED visits nationwide and incur more than $30 billion (in 2010 US dollars) in direct medical costs.3 The decline in health, social isolation and loss of confidence has been well documented after an initial fall.4-6,10–12 Moreover, it is well known that falling is a risk factor for future falls7,8 contributing to the patient's overall morbidity.
Previous studies have followed ED patients between 6 months to 1 year after an initial ED visit but did not focus on ED revisits and mortality.5,7 In the community, older adults with recurrent falls are more likely to have a significantly higher mortality over a 1 to 3 year period with a marked increase of admissions to long-term care facilities.9 With rates of ED visits increasing,10 it is important to quantify these statistics in the ED population to understand the related morbidity. To date there are limited data demonstrating the long-term relationship between older adult ED fall patients and recurrent ED visits and mortality.
This study will longitudinally examine administrative data of ED patients over a 7 year period. We report the characteristics and prevalence of fallers as well as the recurrent ED visit and mortality rate.
2. Methods
2.1 Study design and Study Setting
We conducted an analysis of a cohort of patients who presented to the ED at two urban, level 1 trauma, teaching hospitals with approximately 80,000-95,000 annual visits. Patients were eligible if aged ≥ 65 years, and presented to the ED between February 1, 2005 and December 31, 2011 with a fall-related ED diagnosis. We had follow up data for the cohort until December 31, 2012. Fall-related ED visits were defined as visits with International Classification of Diseases-9th edition (ICD-9) codes of E880.X-E888.X. Data were obtained from hospital and ED databases. Our hospital institutional review board approved of this study.
2.2 Study Protocol
We examined the frequency of accumulated ED revisits and death at 3 days, 7 days, 30 days, and 1 year. We defined an event as having at least one ED revisit before the specific time (3, 7, 30 day and 1 year). We included characteristics of patients likely to impact our outcomes such as age, sex, self-reported race/ethnicity, self-reported primary language, primary insurance, having a primary care physician (PCP), median income, Charlson comorbidity and injury severity score (ISS). Median income was estimated based on home zip code.11 Charlson comorbidities were based on index date diagnosis codes and ISS was estimated using the Center for Disease Control and Prevention's Barrell Matrix (Clark/Ahmed article).12
2.3 Data Analysis
We calculated differences in demographics using Wilcoxon, t, or chi-square test where appropriate. We estimated adjusted odds ratios for ED visit and death controlling for age, sex, self-reported race/ethnicity, self-reported primary language, primary insurance, median income (based on zip code), having a primary care physician, Charlson comorbidity and ISS using multivariable logistic regression models. However, we could not determine if patients visited other EDs. Because these patients were not called for follow up, we could not confirm they were lost to follow up and therefore we did not censor them. We also generated cause-specific Kaplan-Meier curves for ED visit, death, and a composite of ED visit and death. We included variables likely to predict outcomes.13-16 Statistical analysis was performed using SAS Version 9.4 (SAS Institute, Cary, North Carolina).
3. Results
Our cohort included 21,340 older adult patients who presented to the ED with a fall related diagnosis. The average age was 78.6; most were white females who spoke English, had Medicare insurance, an average Charlson comorbidity of 2.7 and Injury Severity score of 5.8 and medium income of $70,152. Most (57%) patients were discharged after their index visit, 37% were admitted to the hospital and 6% were admitted to the observation unit (See Table 1).
Table 1.
Characteristics of older adult patients who visited the ED for a fall, February 1, 2005-December 31, 2011
| Incident visit | |
|---|---|
| N=21,340 | |
| Age, mean (SD) | 79 (8) |
| Sex, Male (%) | 7,419 (35) |
| Race/Ethnicity | |
| White (%) | 17,549 (82) |
| Black (%) | 1,251 (6) |
| Hispanic (%) | 888 (4) |
| Asian (%) | 433 (2) |
| Other (%) | 242 (1) |
| Unknown (%) | 977 (5) |
| Primary Language | |
| English (%) | 18,865 (88) |
| Median Income for zip code, mean (SD) | 70,152 (25,778) |
| Insurance Medicare (%) | 15,808 (74) |
| Private (%) | 3,024 (14) |
| Medicaid/Commonwealth (%) | 577 (3) |
| Self pay (%) | 358 (2) |
| Other/missing (%) | 1,573 (7) |
| Primary care physician listed (%) | 21, 263 (100) |
| Charlson Comorbidity, mean (SD) | 2.7 (3) |
| Injury Severity Score, mean (SD) | 5.8 (6) |
| Disposition | |
| Admitted on index visit(%) | 9191 (43) |
| Hospital (%) | 7977 (37) |
| Observation unit (%) | 1214 (6) |
| Discharged | 12149 (57) |
An increasing proportion of patients revisited the ED over the course of a year, ranging from 2% of patients at 3 days to 25% at 1 year. Male sex, race/ethnicity, median income, comorbidities, and ISS were consistently associated with more ED revisits at 3, 7, 30 days and 1 year (See Table 2). 10,728 patients returned to the ED at some point during our study period 2005-2011 (50.2%). Of those, 2,397 (22.3) had a fall related diagnosis and 3,602 (33.6) were admitted on their first ED revisit. 7,609 patients (36%) had an ED revisit or death within 1 year. Patients who returned to the ED with a fall diagnosis constituted the highest proportion at 3 days (38.1%), while those who returned to the ED and were hospitalized with a fall diagnosis consistently represented nearly 10% of those who returned to the ED.
Table 2.
Characteristics of older adult fall patients with accumulated rates of ED revisits at various time intervals after their incident ED visit, N=21,340, February 1, 2005-December 31, 2011
| Incident Visit |
Accumulated rate of ED revisit at 3 days |
Accumulated rate of ED revisit at 7 days |
Accumulated rate of ED revisit at 30 days |
Accumulated rate of ED revisit at 1 year |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | P | ||
| N=21,340 | N=20883 (98%) |
N=457 (2%) |
20334 (95%) |
N=1006 (5%) |
18583 (87%) |
2757 (13%) |
15942 (75%) |
5398 (25%) |
||
| Age, mean (SD) | 79 (8) | 78.7 (8) | 77.5 (8) | 78.7 (8) | 78.0 (8) | 78.6 (8) | 78.7 (8) | 78.5 (8.4) | 79.0 (8) | 0.001, 0.01,0.98, 0.0002 |
| Sex, Male (%) | 7,419 (35) | 7232 (35) | 187 (41) | 7024 (35) | 395 (39) | 6308 (34) | 1111 (41) | 5389 (34) | 2030 (38) | 0.005, 0.002, <0.0001, <0.0001 |
| Race/Ethnicity | <.0001, <.0001, <.0001, <.0001 | |||||||||
| White (%) | 17,549 (82) | 17201 (82) | 348 (76) | 16756 (82) | 793 (79) | 15350 (83) | 2199 (80) | 13227 (83) | 4322 (80) | |
| Black (%) | 1,251 (6) | 1216 (6) | 35 (8) | 1178 (6) | 73 (8) | 1041 (6) | 210 (8) | 812 (5) | 439 (8) | |
| Hispanic (%) | 888 (4) | 843 (4) | 45 (10) | 806 (4) | 82 (8) | 719 (4) | 169 (6) | 581 (4) | 307 (6) | |
| Asian (%) | 433 (2) | 424 (2) | 9 (2) | 419 (2) | 14 (1) | 390 (2) | 43 (2) | 355 (2) | 78 (1) | |
| Other (%) | 242 (1) | 236 (1) | 6 (1) | 232 (2) | 10 (1) | 211 (1) | 31 (1) | 191 (1) | 51 (1) | |
| Unknown (%) | 977 (5) | 963 (5) | 14 (3) | 943 (5) | 34 (3) | 872 (5) | 105 (4) | 776 (5) | 201 (4) | |
| Primary Language | ||||||||||
| English (%) | 18,865 (88) | 18453 (88) | 412 (90) | 17967 (88) | 898 (8) | 16429 (88) | 2436 (88) | 14080 (88) | 4785 (89) | 0.24, 0.38, 0.94, 0.52 |
| Median Income, mean (SD) | 70,152 (25,778) | 70240 (25771) | 66136 (25782) | 70327 (25816) | 66636 (24742) | 70522 (25853) | 67658 (25126) | 71129 (25995) | 67283 (24912) | .0009, <0.0001, <0.0001, <0.0001 |
| Insurance Medicare (%) | 15,808 (74) | 15451 (74) | 357 (78) | 15033 (74) | 775 (77) | 13716 (74) | 2092 (76) | 11674 (73) | 4134 (77) | 0.79, 0.013, 0.94, 0.52 |
| Private (%) | 3,024 (14) | 2973 (14) | 51 (11) | 2917 (14) | 107 (11) | 2714 (15) | 310 (11) | 2434 (15) | 590 (11) | |
| Medicaid/Commonwealth (%) | 577 (3) | 564 (3) | 13 (3) | 554 (3) | 23 (2) | 502 (3) | 75 (3) | 417 (3) | 160 (3) | |
| Self pay (%) | 358 (2) | 356 (2) | 2 (.4) | 342 (2) | 16 (2) | 304 (2) | 54 (2) | 266 (2) | 92 (2) | |
| Other/missing (%) | 1,573 (7) | 1539 (7) | 34 (.4) | 1488 (7) | 85 (8) | 1347 (7) | 226 (8) | 1151 (7) | 422 (8) | |
| Primary care physician listed (%) | 21,263 (100) | 20809 (100) | 454 (99) | 20263 (100) | 1000 (99) | 18520 (100) | 2743 (99) | 15885 (100) | 5378 (100) | |
| Charlson Comorbidity, mean (SD) | 2.7 (3) | 2.7 (2.8) | 3.2 (3.2) | 2.6 (2.8) | 3.3 (3.2) | 2.5 (2.7) | 3.7 (3.2) | 2.3 (2.6) | 3.8 (3.2) | 0.0007, <0.0001, <0.0001, <0.0001 |
| Injury Severity Score, mean (SD) | 5.8 (6) | 5.9 (5.6) | 3.5 (3.5) | 5.9 (5.6) | 4.4 (4.5) | 5.8 (5.6) | 5.8 (5.6) | 6.0 (5.7) | 5.2 (5.2) | 0.0007, <0.0001, <0.0001, <0.0001 |
| Index ED visit disposition | ||||||||||
| Admitted (%) | 9191 (43) | 9148 (43.8) | 43 (9.4) | 8951 (44.0) | 240 (23.9) | 8034 (43.2) | 1157 (42.0) | 6979 (43.8) | 2122 (41.0) | |
| Hospital (%) | 7977 (37) | 7957 (38.1) | 20 (4.4) | 7797 (38.3) | 180 (17.9) | 6982 (37.6) | 995 (36.1) | 6083 (38.2) | 1894 (35.1) | <0.0001, <0.0001, 0.13, <0.0001 |
| Observation unit (%) | 1214 (6) | 1191 (5.7) | 23 (5.0) | 1154 (5.7) | 60 (6.0) | 1052 (5.7) | 162 (5.9) | 896 (5.6) | 318 (5.9) | 0.54, 0.70, 0.65, 0.46 |
| Discharged | 12,149 (57) | 11735 (56.2) | 414 (90.6) | 11383 (56.0) | 766 (76.1) | 10549 (56.8) | 1600 (58.0) | 8963 (56.2) | 3186 (59.0) | |
| % Return to ED with fall diagnosis, (n) | 38.1 (174/457) | 31.4 (316/1006) | 24.6 (678/2757) | 29.0 (1567/5398) | ||||||
| % Return to ED the hospitalized | 29.8 (136/457) | 34.5 (347/1006) | 45.1 (1244/2757) | 54.5 (2937/5398) | ||||||
| % Return to the ED then admitted to observation unit | 7.4 (34/457) | 7.1 (71/1006) | 6.2 (171/2757) | 9.5 (515/5398) | ||||||
| % Return to the ED and hospitalized related to fall | 9.6 (44/457) | 8.6 (87/1006) | 7.7 (212/2757) | 10.0 (539/5398) | ||||||
| %Return to the ED and admitted to observation related to fall | 4.2 (19/457) | 2.6 (26/2006) | 1.5 (42/2757) | 1.9 (103/5398) | ||||||
Death rates increased from 1.2% at 3 days to 15% at 1 year. Similarly male sex, ethnicity, comorbidity, and ISS were associated with death at each date compared to those who had not died. Age and hospital admission on the index ED visit were also associated with death (see Table 3).
Table 3.
Characteristics of older adult fall patients who died at various time intervals after their initial ED visit, N=21,340, February 1, 2005-December 31, 2011
| Incident Visit | Accumulated Death rate by 3 days | Accumulated Death rate by 7 days | Accumulated Death rate by 30 days | Accumulate Death rate by 1 year | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | P | ||
| N=21,340 | N=21084 (99%) | N=256 (1.2%) | N=20923 (98%) | N=417 (2%) | 20405 (96%) | 935 (4.4) | 18105 | 3235 (15) | ||
| Age, mean (SD) | 79 (8) | 78.6 (8.3) | 82.1 (8.0) | 78.6 (8.3) | 82.7 (8.0) | 78.5 (8.3) | 82.7 (8.3) | 78.0 (8.2) | 82.1 (8.3) | <0.0001, <0.0001, <0.0001, <0.0001 |
| Sex, Male (%) | 7,419 (35) | 7292 (35) | 127 (50) | 7224 (34) | 195 (47) | 6985 (34) | 434 (37) | 5984 (33) | 1435 (44) | <0.0001, <0.0001, <0.0001, <0.0001 |
| Race/Ethnicity | 0.004, <0.0001, <0.0001, <0.0001 | |||||||||
| White (%) | 17,549 (82) | 17325 (82) | 224 (88) | 17180 (82) | 369 (88) | 16712 (82) | 837 (90) | 14723 (81) | 2826 (87) | |
| Black (%) | 1,251 (6) | 1247 (6) | 4 (2) | 1245 (6) | 6 (1) | 1227 (6) | 24 (3) | 1112 (6) | 139 (4) | |
| Hispanic (%) | 888 (4) | 883 (4) | 5 (2) | 878 (4) | 10 (2) | 871 (4) | 17 (2) | 823 (5) | 65 (2) | |
| Asian (%) | 433 (2) | 431 (2) | 2 (0) | 430 (2) | 3 (1) | 422 (2) | 11 (1) | 380 (2) | 53 (2) | |
| Other (%) | 242 (1) | 239 (1) | 3 (1) | 237 (1) | 5 (1) | 234 (1) | 8 (1) | 222 (1) | 20 (.1) | |
| Unknown (%) | 977 (5) | 959 (5) | 18 (7) | 953 (5) | 24 (6) | 939 (5) | 38 (4) | 845 (5) | 132 (4) | |
| Primary Language | ||||||||||
| English (%) | 18,865 (88) | 18630 (8) | 235 (92) | 18484 (88) | 381 (91) | 18008 (88) | 857 (92) | 15881 (88) | 2984 (92) | 0.09, 0.06, 0.001, <0.0001 |
| Median Income, mean (SD) | 70,152 (25,778) | 70134 (25805) | 71670 (23381) | 70106 (25811) | 72480 (23979) | 70033 (25824) | 72746 (24614) | 69998 (25918) | 71009 (24969) | 0.31, 0.05, 0.001, 0.04 |
| Insurance Medicare (%) | 15,808 (74) | 15620 (74) | 188 (73) | 15489 (74) | 319 (76) | 15097 (74) | 711 (76) | 13291 (73) | 2517 (78) | 0.23, 0.03, 0.001, <0.0001 |
| Private (%) | 3,024 (14) | 2978 (14) | 46 (18) | 2955 (14) | 69 (17) | 2880 (14) | 144 (15) | 2612 (14) | 412 (13) | |
| Medicaid/Commonwealth (%) | 577 (3) | 574 (3) | 3 (1) | 573 (3) | 4 (1) | 565 (3) | 12 (1) | 532 (3) | 45 (0) | |
| Self pay (%) | 358 (2) | 355 (2) | 3 (1) | 352 (2) | 6 (1) | 336 (2) | 22 (2) | 257 (1) | 101 (1) | |
| Other (%) | 1,573 (7) | 1517 (7) | 16 (6) | 1514 (7) | 19 (5) | 1487 (7) | 46 (5) | 1373 (8) | 160 (5) | |
| Primary care physician listed (%) | 21,263 (100) | 21009 (100) | 254 (95) | 20848 (100) | 415 (100) | 20330 (100) | 933 (100) | 18036 | 3227 (100) | |
| Charlson Comorbidity, mean (SD) | 2.7 (3) | 2.7 (2.8) | 3.4 (2.8) | 2.6 (2.8) | 3.6 (2.8) | 2.6 (2.8) | 3.9 (3.1) | 2.4 (2.6) | 4.3 (3.3) | <.0001, <0.0001, <0.0001, <0.0001 |
| Injury Severity Score, mean (SD) | 5.8 (6) | 5.7 (5.5) | 12.9 (6.6) | 5.7 (5.5) | 12.7 (6.5) | 5.6 (5.4) | 11.3 (6.9) | 5.4 (5.3) | 8.3 (6.7) | <0.0001, <0.0001, <0.0001, <0.0001 |
| Index ED visit disposition | ||||||||||
| Admitted (%) | 9191 (43) | 9008 (42.7) | 183 (71.5) | 8882 (42.5) | 309 (74.1) | 8510 (41.7) | 681 (72.8) | 7246 (40.0) | 1945 (60.1) | |
| Hospital (%) | 7977 (37) | 7797 (37.0) | 180 (70.3) | 7675 (36.7) | 302 (72.4) | 7315 (35.8) | 662 (70.8) | 6151 (34.0) | 1826 (56.4) | <0.0001, <0.0001, <0.0001, <0.0001 |
| Observation unit (%) | 1214 (6) | 1211 (5.7) | 3 (1.2) | 1207 (5.8) | 7 (1.7) | 1195 (5.9) | 19 (2.0) | 1095 (6.0) | 119 (3.7) | 0.002, 0.0004, <0.0001, <0.0001 |
| Discharged | 12,149 (57) | 12076 (57.3) | 73 (28.5) | 12041 (57.5) | 108 (25.9) | 11895 (58.3) | 254 (27.1) | 10859 (60.0) | 1290 (39.9) | |
In multivariable logistic regression, male sex and comorbidities increased the odds of for both ED revisits and death (Table 4 and 5). Hispanic ethnicity also increased the odds of ED revisits while age and ISS increased the likelihood of death. The c-statistics for 3, 7, 30 days and 1 year were 0.73, 0.66, 0.62 and 0.67 for ED revisit and 0.84, 0.84, 0.81 and 0.78 for death.
Table 4.
Multivariable regression, ED revisits at 3, 7, 30 days and 1 year after older adult ED visit for fall
| 3 day | 7 day | 30 day | 1 year | |
|---|---|---|---|---|
| Age | 1.00 (0.98-1.01) | 1.00 (0.99-1.01) | 1.00 (1.00-1.01) | 1.01 (1.00-1.01) |
| Sex reference female | 1.24 (1.00-1.54) | 1.16 (1.00-1.34) | 1.23 (1.12-1.35) | 1.11 (1.03-1.19) |
| Race (reference white) | ||||
| Black | 1.14 (0.76-1.71) | 1.10 (0.82-1.47) | 1.18 (0.97-1.43) | 1.31 (1.13-1.53) |
| Hispanic | 3.55 (2.23-5.65) | 2.28 (1.61-3.23) | 1.69 (1.33-2.15) | 1.55 (1.27-1.89) |
| Asian | 1.63 (0.78-3.40) | 0.97 (0.54-1.72) | 0.96 (0.68-1.36) | 0.84 (0.64-1.11) |
| Other | 1.46 (0.53-4.05) | 0.81 (0.36-1.86) | 0.85 (0.52-1.38) | 0.74 (0.50-1.09) |
| Unknown | 1.00 (0.54-1.84) | 0.83 (0.54-1.27) | 0.94 (0.74-1.20) | 1.00 (0.84-1.21) |
| English (reference English) | 0.36 (0.22-0.57) | 0.61 (0.45-0.82) | 0.89 (0.75-1.06) | 0.86 (0.75-0.99) |
| Insurance (private reference) | ||||
| Medicare | 1.30 (0.94-1.80) | 1.33 (1.06-1.67) | 1.25 (1.08-1.44) | 1.29 (1.15-1.44) |
| Medicaid/ Commonwealth | 1.16 (0.58-2.32) | 0.99 (0.60-1.66) | 1.03 (0.75-1.42) | 1.33 (1.05-1.69) |
| Self pay | 0.42 (0.10-1.76) | 1.33 (0.73-2.44) | 1.50 (1.04-2.15) | 1.45 (1.08-1.97) |
| Other | 1.14 (0.70-1.87) | 1.35 (0.98-1.87) | 1.31 (1.06-1.61) | 1.29 (1.09-1.52) |
| Pcp (reference have pcp) | - | 2.09 (0.49-8.96) | 2.43 (1.13-5.23) | 2.12 (1.07-4.24) |
| Admitted hospital | 0.09 (0.05-0.14) | 0.38 (0.31-0.47) | 0.91 (0.81-1.01) | 0.90 (0.82-0.98) |
| Observation | 0.52 (0.32-0.85) | 0.80 (0.59-1.08) | 1.06 (0.87-1.29) | 0.97 (0.83-1.13) |
| Median income (10,000 interval) | 0.96 (0.92-1.01) | 0.97 (0.94-1.00) | 0.97 (0.96-0.99) | 0.96 (0.95-0.97) |
| Charlson comorbidity | 1.07 (1.04-1.11) | 1.08 (1.06-1.11) | 1.13 (1.11-1.15) | 1.20 (1.18-1.21) |
| Injury severity | 0.98 (0.95-1.01) | 0.98 (0.97-1.00) | 1.00 (1.00-1.01) | 0.98 (0.97-0.99) |
Table 5.
Multivariate regression of death at 3, 7, 30 days and 1 year of older adult patients who visited the ED for a fall
| 3 day | 7 day | 30 day | 1 year | |
|---|---|---|---|---|
| Age | 1.04 (1.03-1.06) | 1.05 (1.04-1.07) | 1.06 (1.05-1.07) | 1.06 (1.06-1.07) |
| Sex reference female | 1.54 (1.17-2.02) | 1.39 (1.12-1.73) | 1.41 (1.21-1.65) | 1.46 (1.34-1.61) |
| Race (reference white) | ||||
| Black | 0.25 (0.06-1.01) | 0.15 (0.04-0.60) | 0.45 (0.26-0.78) | 0.70 (0.55-0.89) |
| Hispanic | 1.05 (0.35-3.15) | 1.27 (0.58-2.74) | 0.87 (0.49-1.55) | 0.72 (0.51-1.01) |
| Asian | 0.51 (0.12-2.16) | 0.42 (0.13-1.35) | 0.46 (0.22-0.96) | 0.93 (0.65-1.32) |
| Other | 1.25 (0.38-4.10) | 1.23 (0.48-3.19) | 0.88 (0.40-1.84) | 0.68 (0.40-1.15) |
| Unknown | 1.53 (0.89-2.65) | 1.17 (0.72-1.88) | 0.83 (0.57-1.21) | 0.95 (0.76-1.19) |
| English | 0.72 (0.40-1.29) | 0.89 (0.57-1.39) | 0.94 (0.69-1.28) | 0.77 (0.64-0.93) |
| Insurance (private reference) | ||||
| Medicare | 0.66 (0.47-0.93) | 0.78 (0.58-1.05) | 0.76 (0.61-0.93) | 0.93 (0.81-1.06) |
| Medicaid/ Commonwealth | - | 0.11 (0.01-0.80) | 0.44 (0.21-0.93) | 0.64 (0.43-0.94) |
| Self pay | 0.64 (0.19-2.13) | 0.90 (0.37-2.17) | 1.36 (0.79-2.32) | 2.50 (1.80-3.47) |
| Other | 0.58 (0.31-1.11) | 0.49 (0.28-0.88) | 0.59 (0.40-0.85) | 0.57 (0.46-0.72) |
| Pcp (reference have pcp) | 2.22 (0.48-10.32) | 1.30 (0.29-5.86) | 0.62 (0.14-2.72) | 1.07 (0.46-2.46) |
| Admitted to hospital | 1.32 (0.95-1.84) | 1.47 (1.13-1.92) | 1.82 (1.52-2.19) | 1.52 (1.37-1.69) |
| Observation | 0.18 (0.04-0.75) | 0.36 (0.15-0.82) | 0.43 (0.25-0.74) | 0.66 (0.52-0.83) |
| Median income (10,000 interval) | 0.96 (0.91-1.01) | 0.97 (0.93-1.01) | 0.99 (0.97-1.02) | 0.99 (0.97-1.01) |
| Charlson comorbidity | 1.12 (1.07-1.17) | 1.14 (1.10-1.18) | 1.16 (1.13-1.18) | 1.24 (1.23-1.26) |
| Injury severity | 1.15 (1.13-1.18) | 1.15 (1.13-1.17) | 1.12 (1.10-1.13) | 1.06 (1.05-1.07) |
Overall – older, male, higher cci, iss more have higher likelihood of death.
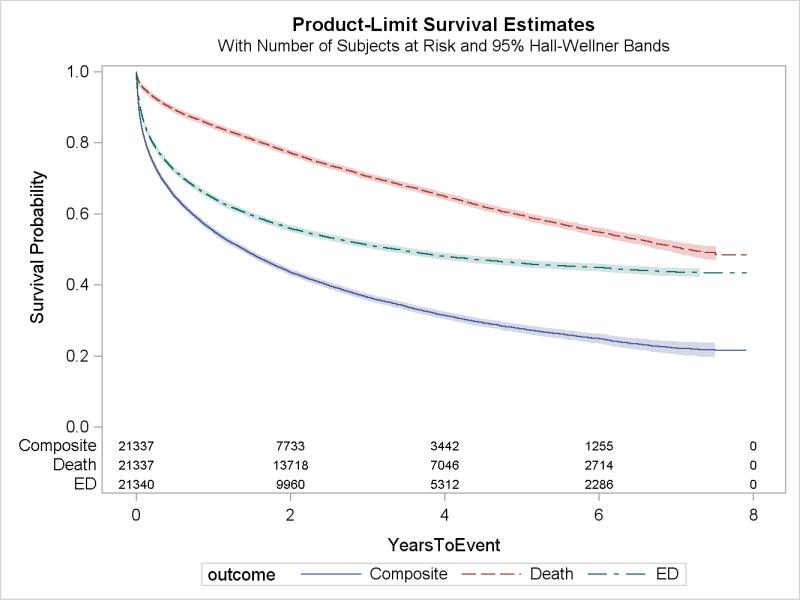
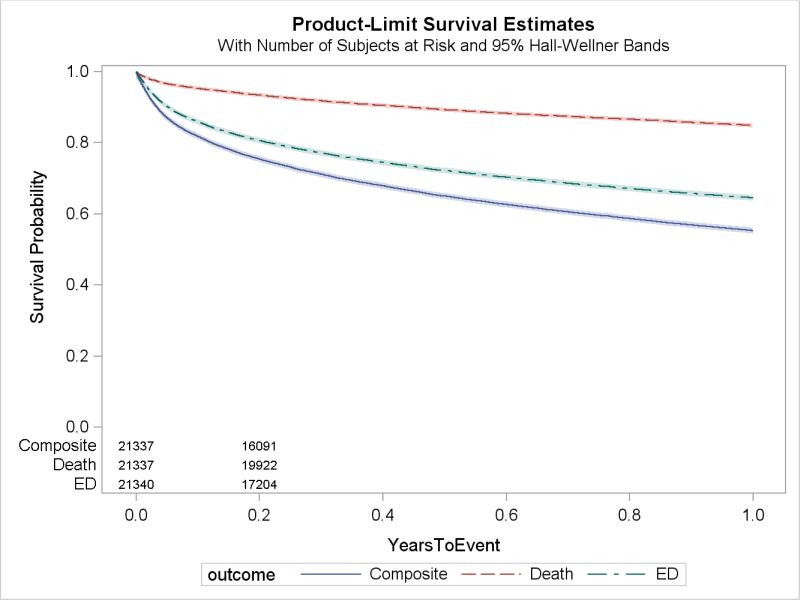
Figures 1 and 2 show survival curves for ED revisits, deaths and a composite of ED revisits and death and indicate a steep slope after the index ED visit, particularly the first several months.
Figure 1.
Survival curve for ED revisit, death and composite (ED revisit+death) for older adult ED fall patients 2/1/2005-12/31/2011.
Figure 2.
1 Year survival curve for ED revisit, death and composite (ED revisit+death) for older adult ED fall patients 2/1/2005-12/31/2011 (Censored at the end of one year).
4. Discussion
This study is the first to examine ED revisits and death after older adult fall patients present to the ED. We found that over a third of older adult ED fall patients had an ED revisit or died within one year; our outcomes increased with age, male gender and comorbidities. Older adults revisit the ED frequently and have high post-ED death rates; our findings show that falls are one of the geriatric syndromes that contribute to such high rates. Because we did not compare outcomes with other elderly ED diagnoses, we could not determine whether falls increased the risk of ED revisits or mortality.
Our finding that a quarter of older adult ED fall patients returned to the ED within a year and over half over our 7 year study period further supports the notion that older adults are high risk patients and that falls are one of the geriatric syndromes that contribute to ED visits and death rates. Given 10% of older adult patients discharged from the ED fall again within approximately 20 days,17 it is not surprising that over a fifth of our patients revisited the ED with a fall-related diagnosis. While we did not compare ED revisits with non-fall patients, our revisit findings are within the wide range of overall older adult ED revisit rates and similar to a recent study reporting a 30-day ED revisit rate among fallers of 13.6%.18 McCusker's study of patients aged 65 and above who were discharged from the ED found 19.3% of patient made an ED revisit within 30 days and over 40% within 6 months.19 Friedmann's single site cohort study of elderly patients who were discharged from the ED found a 12% revisit rate at 30 days among older adult ED discharged patients and a 19% ED revisit rate at 90 days.20 They found that physical functioning was the only consistent independent predictor of revisit, hospitalization or death at 30 and 90 days. Friedmann also noted the Charlson comorbidity score predicted 90 day hospitalization or death but not 30 day outcomes; age, gender, race and diagnosis were not significant predictors in their multivariate model. Women are more likely to fall and sustain a fracture and have an associated decline in level of functioning after a fall,21 resulting in more health service use such as hospitalizations and ED visits than males, contrary to our findings.21,22 On the other hand, a prospective Dutch cohort study found that gender was not a predictor of recurrent falls.23 Furthermore, one-third of patients were admitted to the hospital on their first ED revisit. While previous studies have examined the outcomes related to the index fall visit, this is the first study to follow these patients over time to examine their future ED use as well as mortality.24,25
Our study's death rates were consistent with other studies. Our 4% death rate at 30 days was higher than Friedmann's 1.5% 30 day older adult ED death rate as well as Mccusker's 1% 30-day death rate.20,26 However, those studies examined discharged patients and did not focus on fall patients. Our one year death rate of 15% is similar to what Donald et al9 found in their UK community cohort of older adult patients (average one year mortality rate of 16.4% for fallers compared with 8.5% for non-fallers). Their study's mortality was overall higher for those who reported greater than one fall in the previous 3 months -- mortality was not increased for those who reported only falling once. Ayoung-Chee, et al found a 33% 1 year mortality rate, but their study focused on outcomes after fall patients were hospitalized.25 Sise et al found that fall-related mortality increased by 46% from 2002 to 2010 and was associated with advanced age. They further commented that if trends continued, fall-related deaths would surpass motor vehicle deaths and firearm mortality.27 In terms of gender, males suffer higher levels of mortality after an initial fall,3,28 consistent with our findings. This may be due to males sustaining worse injuries after falling from greater heights such as a ladder or be in poorer health than women of similar age.28
Elderly patients frequently revisit the ED and have high mortality rates – falls are among the various geriatric syndromes that not only are multifactorial in etiology but can contribute to other geriatric syndromes (e.g. delirium). Emergency physicians (EP) should continue to evaluate patient's fall-related injuries, but efforts should also be made to prevent future falls, determine the etiology of the fall, and improvement management of the underlying etiology of the fall. The recently published Geriatric ED Guidelines29 can assist EPs in how to evaluate fall patients. However, given the limited time EPs have, efforts will need to be made to collaborate with geriatricians and primary care physicians to manage older adult fall patients’ fall risks as well as their fall etiology. EPs and/or case managers may need to screen for home safety evaluations, home services and/or improve communication with PCP's to refer to fall clinics/community fall programs. Furthermore, efforts should be made on how to identify those patients at greatest risk for poor outcomes.
Limitations
Our study was limited in several ways. We did not compare our outcomes with other reasons for elderly ED visits; hence, we could not determine if falls increased the risk for ED revisits or mortality. We used a database to obtain our retrospective cohort using ICD-9 codes. Patients may have been overlooked if they did not have correct coding or if the diagnosis of fall was omitted from the chart. We were unable to determine the causes of the fall and our logistic regression was limited in terms of variables that could be obtained from our database. For example, we were unable to include whether the patient was demented, community dwelling, or took various types of medications which may have impacted outcomes. Furthermore, this was only limited to two hospitals, potentially making it difficult to generalize to other hospitals. Also, we only identified patients who returned to the ED where the patients were first seen. Finally, 15% of patients had missing ISS though it is not clear that this would bias our results in one way or another.
Conclusion
Older adults revisit the ED frequently and have high post-ED death rates; falls are one of the geriatric syndromes that contribute to such high rates. Future research should focus on determining whether falls increase the risk of such outcomes as well as whether guidelines or other fall related programs can prevent future falls, morbidity and death.
References
- 1.Center for Disease Control and Prevention [1/1/2013]; http://www.cdc.gov/injury/wisqars.
- 2.Sterling DA, O'Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–9. doi: 10.1097/00005373-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12:290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boele van Hensbroek P, van Dijk N, van Breda GF, et al. The CAREFALL Triage instrument identifying risk factors for recurrent falls in elderly patients. Am J Emerg Med. 2009;27:23–36. doi: 10.1016/j.ajem.2008.01.029. [DOI] [PubMed] [Google Scholar]
- 5.Carpenter CR, Scheatzle MD, D'Antonio JA, Ricci PT, Coben JH. Identification of fall risk factors in older adult emergency department patients. Acad Emerg Med. 2009;16:211–9. doi: 10.1111/j.1553-2712.2009.00351.x. [DOI] [PubMed] [Google Scholar]
- 6.Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P. Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol. 2001;54:837–44. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- 7.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet. 1999;353:93–7. doi: 10.1016/S0140-6736(98)06119-4. [DOI] [PubMed] [Google Scholar]
- 8.O'Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- 9.Donald IP, Bulpitt CJ. The prognosis of falls in elderly people living at home. Age Ageing. 1999;28:121–5. doi: 10.1093/ageing/28.2.121. [DOI] [PubMed] [Google Scholar]
- 10.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997-2007. JAMA. 2010;304:664–70. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Population Studies Center . University of Michigan; [1/1/12]. http://www.psc.isr.umich.edu/dis/census/Features/tract2zip/index.html). [Google Scholar]
- 12.Clark DE, Ahmad S. Estimating injury severity using the Barell matrix. Inj Prev. 2006;12:111–6. doi: 10.1136/ip.2005.010058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gabayan GZ, Derose SF, Asch SM, et al. Patterns and predictors of short-term death after emergency department discharge. Ann Emerg Med. 2011;58:551–8. e2. doi: 10.1016/j.annemergmed.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sklar DP, Crandall CS, Loeliger E, Edmunds K, Paul I, Helitzer DL. Unanticipated death after discharge home from the emergency department. Annals of emergency medicine. 2007;49:735–45. doi: 10.1016/j.annemergmed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 15.Kefer MP, Hargarten SW, Jentzen J. Death after discharge from the emergency department. Ann Emerg Med. 1994;24:1102–7. doi: 10.1016/s0196-0644(94)70239-x. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–92. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 17.Russell MA, Hill KD, Day LM, et al. A randomized controlled trial of a multifactorial falls prevention intervention for older fallers presenting to emergency departments. J Am Geriatr Soc. 2010;58:2265–74. doi: 10.1111/j.1532-5415.2010.03191.x. [DOI] [PubMed] [Google Scholar]
- 18.Bond CM, Freiheit EA, Podruzny L, et al. The emergency to home project: impact of an emergency department care coordinator on hospital admission and emergency department utilization among seniors. Int J Emerg Med. 2014;7:18. doi: 10.1186/1865-1380-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCusker J, Cardin S, Bellavance F, Belzile E. Return to the emergency department among elders: patterns and predictors. Acad Emerg Med. 2000;7:249–59. doi: 10.1111/j.1553-2712.2000.tb01070.x. [DOI] [PubMed] [Google Scholar]
- 20.Friedmann PD, Jin L, Karrison TG, et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med. 2001;19:125–9. doi: 10.1053/ajem.2001.21321. [DOI] [PubMed] [Google Scholar]
- 21.Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age Ageing. 2004;33:58–65. doi: 10.1093/ageing/afh028. [DOI] [PubMed] [Google Scholar]
- 22.Hendrie D, et al. Injury in Western Australia: the health system cost of falls in older adults in Western Australia. Western Australian Government; Perth, Western Australia: 2003. [Google Scholar]
- 23.Stalenhoef PA, Diederiks JPM, Knottnerus JA, et al. A risk model for the prediction of recurrent falls in community-dwelling elderly. J Clin Epi. 55:1088–94. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 24.Owens PL, Russo CA, Spector W, et al. Emergency Department Visits for Injurious Falls among the Elderly, 2006: Statistical Brief #80. 2006 [PubMed] [Google Scholar]
- 25.Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, Maier RV. Long-term outcomes of ground-level falls in the elderly. J Trauma Acute Care Surg. 2014;76:498–503. doi: 10.1097/TA.0000000000000102. discussion. [DOI] [PubMed] [Google Scholar]
- 26.McCusker J, Roberge D, Vadeboncoeur A, Verdon J. Safety of discharge of seniors from the emergency department to the community. Healthc Q. 2009:12. doi: 10.12927/hcq.2009.20963. Spec No Patient:24-32. [DOI] [PubMed] [Google Scholar]
- 27.Sise RG, Calvo RY, Spain DA, Weiser TG, Staudenmayer KL. The epidemiology of trauma-related mortality in the United States from 2002 to 2010. J Trauma Acute Care Surg. 2014;76:913–9. doi: 10.1097/TA.0000000000000169. discussion 20. [DOI] [PubMed] [Google Scholar]
- 28.National Council on Ageing Research review papers in Falls free: Promoting a national falls prevention action plan. 2005 [Google Scholar]
- 29. [3/1/2014];Geriatric Emergency Department Guidelines. (2014, at http://www.saem.org/docs/education/geri_ed_guidelines_final.pdf?sfvrsn=2.)