Abstract
In order to increase uptake of measles, mumps and rubella (MMR) vaccine, a domiciliary immunization service was established in Dudley primary care trust in England in 2010. Parents of unimmunized children were offered vaccines at home. Uptake of MMR vaccine among 2 year olds rose from 89% in 2007/08 to 96.9% in 2015. Children were also given any other outstanding immunizations. The domiciliary immunization service reached vulnerable unimmunized children who may otherwise have remained unprotected against life threatening childhood illnesses. Domiciliary immunization service was set up in 2010 to reduce inequalities in uptake of MMR vaccine among children aged between 2 and 5 years.
Keywords: immunization, domiciliary, inequalities, MMR, measles, children
Introduction
There are a number of factors which influence poor uptake of childhood vaccines. The loss of confidence in the MMR vaccination program has resulted in passive and active refusal by parents/guardians since the late 1990s. In addition, groups within society who find traditional service hard to reach, and regional areas where there may be poor provision, have contributed to reduced vaccine uptake. Uptake of the first MMR dose at 24 months of age was recorded in Dudley as 89% in 2007/08. A Dudley Primary Care Trust (PCT) Strategic Plan was published in 2008, setting a target to increase uptake to 95% by April 2011.
In response, a number of initiatives to improve uptake were established with investment as part of the Local Development Plan (LDP). Data cleansing between Child Health Information System (CHIS) and GP systems was instigated. Increased promotional activity regarding the benefits of vaccination was undertaken in the Borough of Dudley. The Domiciliary Immunization Project was started. In addition an Inequalities Assessment was completed to establish the factors affecting uptake.
Inequalities Assessment
The inequalities assessment of the childhood immunization program (2011) considered 2 primary factors, the population invited for immunization and the providers who administer the immunizations. It found that inequality in uptake was not associated with population factors such as level of deprivation or ethnic origin but that inequalities were associated with provider provision. It concluded that the limiting step was hard to reach services and not hard to reach groups.
Domiciliary Immunization
The Domiciliary Immunization (DI) Service targets those parents/guardians who had not responded to previous invitations for their children's first MMR vaccination, offering for the child to be immunized in their own home. The DI project commenced in January 2010 and was formalised as a service in the Dudley Borough from April 2011. An initial target cohort was defined as children without their first MMR who were about to turn 2 y of age. Subsequently an iterative approach to defining the target cohort has been adopted, currently each month the cohort is identified using data from the CHIS. Those children identified as eligible are offered MMR and any other missing vaccines at home.
The DI service is provided by an independent experienced nurse employed for 25.5 hours per week, hosted and co-located with the Office of Public Health Communicable Disease Team.
The process of the DI program commences with checks made on immunization history and accuracy of demographic data. This involves utilizing GP and Health Visitor records, CHIS and National Summary Care Records. Following this the parents and guardians of the identified child will be contacted. This will occur firstly by telephone followed by cold call or letter hand delivered and via Royal Mail.
There are a number of challenges commonly faced in delivering vaccinations via the DI program. Difficulties were experienced in finding the children, either the child had moved out of area, new residents were found at registered address or the house was empty or even demolished. If the child was located there were additional challenges from refusal to vaccinate, both active and passive.
Outcomes
In quarter 1 of 2015 the DI service contributed 3.5 percentage points and GPs contributed 93.4 percentage points to the total percentage of children, aged 2, vaccinated against MMR (Fig. 1).
Figure 1.
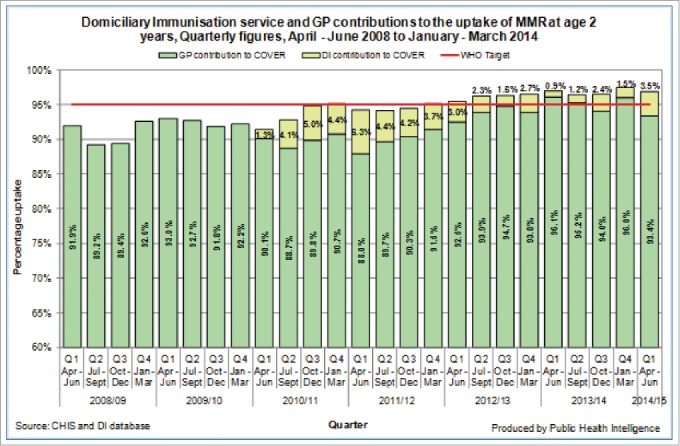
MMR uptake by quarter and domiciliary immunization service contribution, quarterly COVER data April – June 2008 to April – June 2014 (Dudley CHIS and DI bespoke database, produced by the PH Intelligence Team in Dudley).
Although the DI service targets children missing their first dose of MMR the service also offers those children any other vaccination that is outstanding. For example, in 2013/14, 0.4% of the Hib/Men C coverage in children aged 2 y was administered via the DI service (Table 1).
Table 1.
DI service estimated contribution to the coverage of MMR and other immunizations at age 2 years, annual contribution since 2010/11 and quarter 1 2014/15 in the Dudley Clinical Commissioning Group (CCG) 1
| Number of vaccines given (Percentage contribution to total coverage) |
|||||
|---|---|---|---|---|---|
| MMR | PCV | Dtap/IPV/Hib | Men C | Hib/Men C | |
| 2010/11 | 131 (3.7%) | 38 (1.1%) | 6 (0.2%) | <5 (0.1%) | 14 (0.4%) |
| 2011/12 | 170 (4.6%) | 96 (2.6%) | 35 (1%) | 26 (0.7%) | 37 (1%) |
| 2012/13 | 86 (2.4%) | 52 (1.4%) | 17 (0.5%) | 15 (0.4%) | 37 (1%) |
| 2013/14 | 57 (1.5%) | 10 (0.3%) | 5 (0.1%) | <5 (N/;A)* | 16 (0.4%) |
| Q1 2014/15 | 26 (3%) | 17 (1.8%) | <5 (0.1%) | 0 (N/;A)* | 16 (1.7%) |
| Total | 479 (2.6%) | 213 (1.4%) | 64 (0.4%) | 48 (0.3%) | 120 (0.8%) |
Vaccine is no longer recorded in Cover Data.
In April 2014, older children aged 3, 4 and 5 y were added to the DI caseload and parents/guardians offered vaccination for their children. Additionally, the DI service took opportunities to vaccinate older siblings if they were discovered to have also missed vaccinations. In quarter 1 of that year the DI service gave 11 vaccines to older children.
Not all children on the DI service caseload are able to be immunized by the domiciliary immunizer, 23% of the parents refuse the vaccine either actively or passively. Other outcomes of the DI service are also shown in Figure 2; the definitions of all of these are given in appendix 1.
Figure 2.
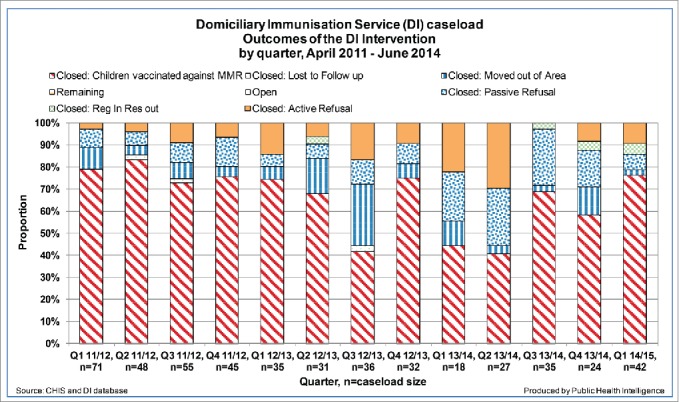
Outcomes from the domiciliary immunization service's interventions since April 2011 (Dudley CHIS and DI bespoke database, produced by the PH Intelligence Team in Dudley).
On average the DI service makes approximately 5 contacts per child on the caseload, either with the child's parents, GP, Health Visitor, Home visit or Child Health Records Team. Due to data cleansing undertaken as part of the implementation of the new CHIS in July 2011 (Quarter 2 2011/12) and the reduction in the childhood immunizations waiting lists, fewer children are becoming part of the DI caseload. Although there are now fewer children on the caseload, the number of contacts the DI service makes with these children has increased as these children are more difficult to contact and in genuine need of the service.
Costs of the DI Service
A breakdown of costs shows £ 440 per MMR vaccination, £ 200 per vaccine (whether MMR or another childhood vaccine) and £ 65 per DI contact. The National Institute for Health and Clinical Excellence (NICE) has stated that economic modeling showed at current levels of immunization, efforts to increase uptake of the measles vaccine were highly cost effective in groups with both high and low immunization coverage.2 Increasing uptake among low coverage groups was shown to be marginally more efficient than increasing uptake among high-coverage groups. (This is true if the cost per child were the same in each group.) It would also do more to reduce health inequalities. The modeling suggested that home visits (likely to be the most expensive means of increasing coverage by one percentage point) would be a cost effective use of NHS resources. The implication is that almost any method of increasing coverage would be cost effective. The model underestimated the cost effectiveness of the MMR vaccine because it did not ascribe any benefits to the concurrent prevention of mumps and rubella infection. The vaccine offers simultaneous protection against 3 different infections.2
Conclusion
The DI service provided by Dudley Public Health has increased childhood vaccination uptake not only for the target children but also their siblings. NICE supports the use of a DI program as a cost effective use of NHS resources in increasing measles vaccine uptake. The DI program in Dudley demonstrates the efficacy of the DI model for reaching vulnerable children who may otherwise remain unprotected from life-threatening childhood illnesses.
Disclosure of Potential Conflicts of Interest
There are no conflicts of interest.
Supplemental Material
Supplemental data for this article can be accessed on the publisher's website.
References
- 1.HSCIC reports, PHE COVER data and DI database Available at: https://www.gov.uk/government/statistics/cover-of-vaccination-evaluated-rapidly-cover-programme-2013-to-2014-quarterly-figures.
- 2.National Institute for Health and Clinical Excellence (NICE) (September 2009) Reducing differences in the uptake of immunizations (including targeted vaccines) among children and young people aged under 19 years [PH21]. Available at: https://www.nice.org.uk/guidance/ph21/resources/guidance-reducing-differences-in-the-uptake-of-immunizations-pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


