Abstract
Background
This study aimed to evaluate the efficacy of transforaminal endoscopic discectomy (TED) in the treatment of obese patients with lumbar disc herniation (LDH).
Material/Methods
A total of 69 obese patients with LDH (35 males and 34 females; age range, 24 to 43 years; median age, 34 years) were included in this study. These patients had undergone TED from March 2011 to December 2015 in the Third Hospital of Hebei Medical University. Their clinical and follow-up data were prospectively analyzed. The degree of pain and disability were measured on the basis of the Visual Analog Scale (VAS) at 1 day before surgery, immediately after surgery, and 3 months after surgery. Neurologic functions were measured on the basis of the Japanese Orthopaedic Association (JOA) system 1 day before surgery and 3 months after surgery. The MacNab score at last follow-up was recorded to evaluate the early clinical efficacy. Complications during and after the operation were recorded to evaluate the safety of surgery.
Results
Two patients experienced abnormal sensations in the export nerve root zone postoperatively, which disappeared after 3 days of treatment with dehydration and administration of hormone (dexamethasone). Three cases of recurrence were observed at 6 months, 7 months, and 9 months postoperatively; they were scheduled to receive total laminectomy combined with bone grafting internal fixation. A total of 67 patients were followed up for 3–23 months and mean follow-up was 11.8 months. The VAS scores at postoperative 3 months and 1 year were significantly reduced compared to that before the operation, with significant differences between them (t=43.072, P<0.05; t=43.139, P<0.05). The JOA scores at last follow-up postoperatively was significantly higher than that before surgery (t=−60.312, P<0.05). At the last follow-up, 17 cases (25.3%) had excellent outcomes, 39 (58.2%) good, 7 (10.4%) fair, and 4 (5.9%) poor. Overall, 83.5% of patients had excellent or good rates.
Conclusions
The early efficacy of TED is relatively good and safe for the selected obese patients with LDH in this study. Larger-sample studies with longer duration and follow-up are required to detect the safety and effectiveness of TED.
MeSH Keywords: Diskectomy, Percutaneous; Endoscopy; Osteoarthritis, Spine
Background
Lumbar disc herniation (LDH) is a common ailment that produces medical and economic burdens for families and society [1,2]. When expectant treatment fails, surgical treatment is often required, which includes open surgery and minimally invasive surgery [3,4]. The large incision and extensive peeling off of soft tissue in traditional open surgery often leads to great trauma, much blood loss, and muscle denervation and atrophy [5], and there may still be long-term lumbodorsal muscular pains postoperatively. These factors seriously affect the clinical curative effect and patient satisfaction [6].
It has been reported that there is a significant correlation between LDH and fat [7,8]. When traditional open surgery was used to treat obese patients with LDH, the operative incision needs to be lengthened, which may result in greater injury of muscle and soft tissue, as well as increased bleeding and the infection risk [9,10]. Therefore, spine surgeons are confronted with enormous challenges in reducing the operative incision for obese patients with LDH and decreasing perioperative complications, as well as improving clinical curative effect and patient satisfaction.
With the rapid development of minimally invasive spine surgery, the technique of spinal endoscopy has made revolutionary progress, especially for percutaneous transforaminal endoscopic discectomy (PTED), which is widely recognized as having the advantages of minimal invasiveness, greater accuracy, and quicker recovery [11,12]. PTED also sheds light on the treatment of obese patients with LDH. However, few studies have specifically aimed at determining the effect of transforaminal endoscopic discectomy (TED) on the treatment of obese patients, the safety and effectiveness of which are still unclear.
Therefore, we analyzed the data of 69 obese patients with LDH treated with TED, aiming to explore the effectiveness of TED on the treatment of obese patients with LDH.
Material and Methods
General Materials
A total of 69 obese patients with LDH (35 males and 34 females; age range, 24 to 43 years; median age, 34 years) were included in this study. These patients had undergone TED from March 2011 to December 2015 in the Third Hospital of Hebei Medical University. The course of disease ranged from 6 to 23 months, with an average time of 7.3 months. There were 43 patients with a herniated disc at the L4/L5 level, and 26 patients with a herniated disc at the L5/S1 level. Written informed consent was obtained from all patients. The obese patients included in this study did not include patients with far lateral disc, migrated disc, any recurrent disc, failed back case, or lateral recess syndrome. The study protocol was approved by the Ethics Committee of the Third Hospital of Hebei Medical University.
We used the following inclusion criteria: (1) degenerative changes of a single segment lumbar intervertebral disc with different degrees of unilateral lower limb nerve root pain, imaging performance consistent with clinical symptoms and signs; (2) receiving at least 6 months of expectant treatment before the operation and poor curative effect of expectant treatment; (3) no instability of lumbar spine according to the preoperative X-ray examination on lumbar spine dynamic position; and (4) body mass index (BMI) ≥28 kg/m2. Exclusion criteria were: (1) obvious degenerative deformities, instability, disc calcification, lumbar spinal canal, and intervertebral foramen; and (2) severe prolapse and dissociation of nucleus pulposus, and with extreme lateral LDH. Every enrolled patient met all the inclusion criteria and did not meet any of the exclusion criteria.
Surgical technique
All the operations were performed by the same surgeon. Patients received a local and potentiated anesthesia (1% lidocaine). The anaesthetic was titrated to allow the patient to communicate with the surgeon throughout the procedure (Figure 1). The patient was placed in the lateral position with the affected side upwards and the uninjured side was blocked up. Before the operation, the X-ray frontal fluoroscopic angle paralleled the lesion segment end plate. The diseased intervertebral disk plane and the posterior midline of spinal process were marked. The entry point and side open distance depended on the patients’ physique and type of LDH. The entry point was generally 12–14 cm from the safety margin, which was the line of the superior margin of the zygapophyseal, marked by lateral X-ray, and the spinal needle could not be lower than the safety margin to avoid causing major organ and vessel injury in the abdomen.
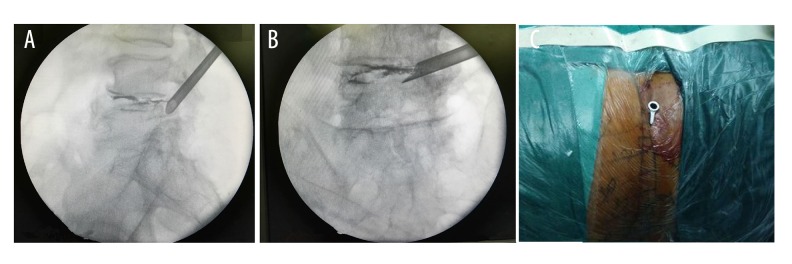
Figure 1.
Patients received a local and potentiated anesthesia.
The surgical approach was a lateral approach. A long 18-gauge spinal needle was inserted from the entry point and punctured under the guidance of C-arm radiograph. The needlepoint reached the anterior inferior border of the zygapophyseal. A long 22-gauge spinal needle was taken from the 18-gauge spinal needle and a guidewire was inserted into the needle. When the position was correct according to fluoroscopic guidance, the spinal needle was taken out. Taking the entry point as the center, an 8-mm incision was made on the skin. The guide bar was inserted along the guidewire and the surgical channel was expanded through step-by-step expansion of the catheter. Followed by gradually taking out the dilating catheter, a serrated reamer was inserted along the guide bar. Partial sclerotin on the outer edges of superior articular process was removed under the guidance of C-arm radiography. This process was foraminoplasty. The serrated reamer never exceeded the inner edge of the pedicle of the vertebral arch to protect the dura mater and nerve from injury. After taking out the trephine, working casing was placed along the guide bar (Figure 2). When the position was correct according to fluoroscopic guidance, the endoscope was placed. The ruptured disk and its debris were observed under the endoscope (Figure 3). The degenerative nucleus pulposus was extracted by proprietary nucleus pulposus forceps through the intervertebral foramen. Clearly visible dura under endoscopy and dura with the heart beat were the significant signs for thoroughly decompressing and terminating the surgery (Figure 4). The negative result of straight-leg raising test further illustrates the effectiveness of thorough decompression. Crinkle plasty was performed on a fiber ring tear opening with a RF bipolar electrode. Coagulation hemostasis was used to stop the bleeding. Working casing was rotated to examine the bleeding and debris. After confirming there was no abnormality, the endoscope and working casing were removed.
Figure 2.
(A, B) Lateral radiographs and normal radiographs showing placement of the working channel. (C) Working channel in body.
Figure 3.
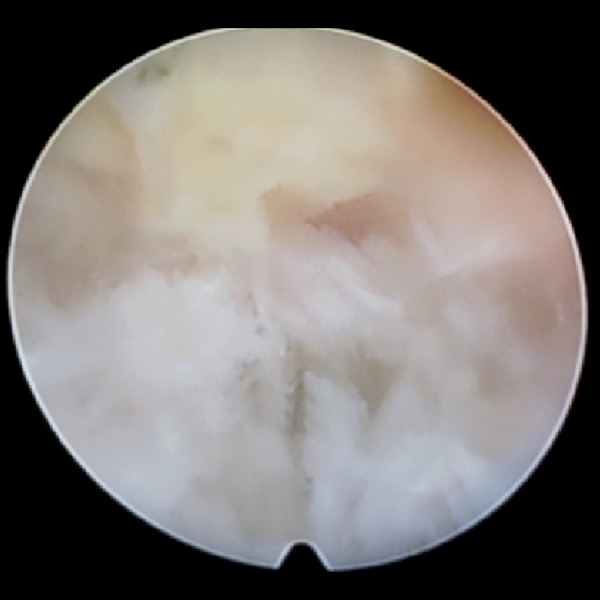
The ruptured disk and its debris were observed under endoscopy.
Figure 4.
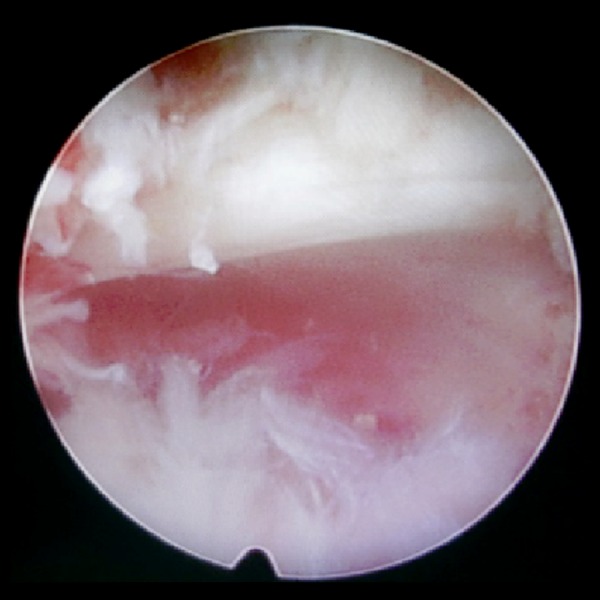
Clearly visible nerve root impulse under endoscopy.
Postoperative treatment
Postoperatively, patients rested for 1–2 days and had the option to ambulate through wearing a waistline, after which patients practiced back muscle exercises and straight-leg raising exercises. After 1 week, patients could do some light manual labor. Treatment with dehydration, hemostasis, and nutritional nerve agents were used as needed with specific conditions.
Assessment of clinical outcome
The degree of pain and disability in the leg was measured by the visual analog scale (VAS) 1 day before surgery, immediately after surgery, and 3 months after surgery. Neurologic functions were measured on the basis of the Japanese Orthopaedic Association (JOA) system 1 day before surgery and 3 months after surgery. The MacNab score at last follow-up was recorded to evaluate the early clinical efficacy: excellent indicating no pain in waist and legs and no limitation of motion; good indicating occasional pain in waist or legs, but not enough to interfere with work; fair indicating function has improved, with intermittency of pain and patients must change their work and life; and poor indicating no improvement in pain and function. Complications during and after the operation were recorded to evaluate the safety of surgery. These assessments were performed by an independent observer.
Statistical analysis
We used SPSS 19.0 (SPSS, USA) to analyze all data. Measurement data were compared using the t test or analysis of variance. A positive significance level was assumed at a probability of less than 0.05.
Results
A total of 67 patients were followed up for 3–23 months and mean follow-up was 11.8 months. Lower limb pain was relieved immediately after surgery in 66 patients and 1 patient had no significant improvement after the operation and was scheduled to receive total laminectomy combined with bone grafting internal fixation. Puncture failed owing to the blocking of crista iliaca during the operation in 2 patients with a herniated disc at the L5/S1 level. These patients then underwent microendoscopic discectomy (MED).
Two patients experienced abnormal sensation in the export nerve root zone postoperatively, which disappeared after 3 days of treatment with dehydration and administration of hormone (Dexamethasone, 10 mg, 1 time/day). Three cases of recurrence were observed at postoperative 6 months, 7 months and 9 months. They were scheduled to receive total laminectomy combined with bone grafting internal fixation.
VAS scores
The preoperative VAS scores of 67 patients was 7.12±0.70, at postoperative 3 months it was 2.46±0.68, and at postoperative 1 year it was 2.27±0.74. The VAS scores at postoperative 3 months and 1 year were significantly reduced compared to that of pre-operation, with significant differences between them (t=43.072, P<0.05; t=43.139, P<0.05).
JOA scores
The preoperative JOA scores of 67 patients was 13.7±0.87, and postoperative last follow-up was 22.1±0.79. The JOA scores at last follow-up postoperatively was significantly higher than that before surgery (t=−60.312, P<0.05).
Clinical curative effect
For the MacNab evaluation, 17 cases (25.3%) had excellent outcomes, 39 (58.2%) good, 7 (10.4%) fair, and 4 (5.9%) poor. Overall excellent and good rate was 83.5%.
Imaging findings
Thirty-five patients had MRI review of the lumbar spine postoperatively (Figure 5). Compared to the preoperative lumbar spine, the ruptured disk significantly rebounded and disappeared (Figure 6).
Figure 5.
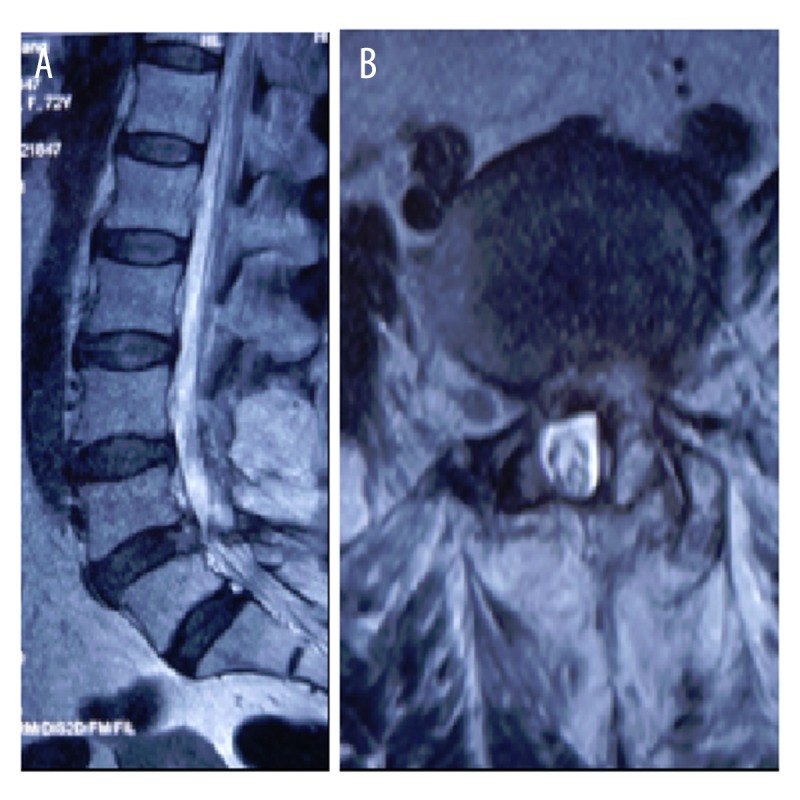
Postoperative sagittal MRI (A) and cross-section MRI (B) showing LDH.
Figure 6.
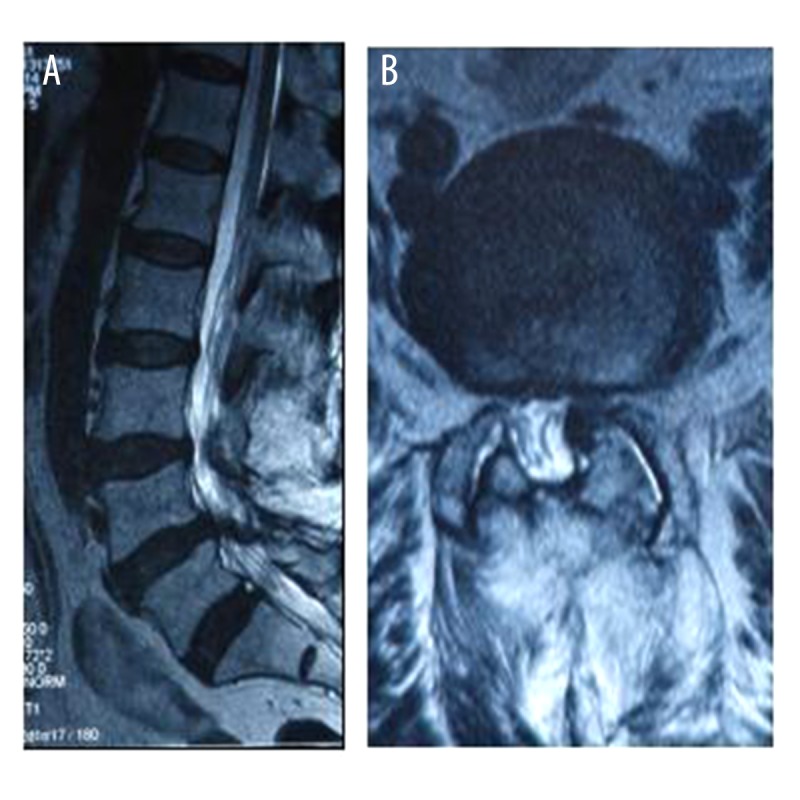
Preoperative sagittal MRI (A) and cross-section MRI (B) showing rebounded LDH.
Discussion
Research on obesity-related diseases and the harmful effects of obesity on health has become extremely popular in recent years. Degenerative disease of the lumbar intervertebral disc has become more common with the growing elderly population. At the same time, accumulating research has focused on the relationship between obesity and intervertebral disc disease. Bayramoglu et al. found that high BMI might be a cause of low back pain in women [13]. Fanuel et al. also showed that backache induced by obesity might be associated with increasing weight load [14]. However, it is difficult to use open surgery to treat obese patients with LDH, owing to the thick subcutaneous fat and deep operation location. In addition, it has been reported that obesity contributes to postoperative complications, including postoperative infection [15,16]. Poor blood supply in adipose tissue leads to slow healing and postoperative infection. Moreover, fat liquefaction caused by the electrotome during surgery might further increase the possibility of postoperative infection. Therefore, improving the postoperative therapeutic effects of lumbar surgery in obese patients is of great significance. Percutaneous transforaminal endoscopic discectomy (PTED) is an effective method to treat LDH [17–19]. Pan et al. suggested that the transforaminal endoscopic spine system (TESSYS) had clinical advantages over fenestration discectomy and entails less trauma and faster postoperative recovery [20]. Hoogland et al. reported that over 90% of LDH patients treated with TESSYS had an excellent or good result at the 2-year follow-up, with below 3% early recurrence [21]. This research sheds new light on the treatment of obese patients with LDH.
In the present study, the VAS scores at postoperative 3 months and 1 year was significantly reduced compared to that of before the operation, with significant differences between them. The JOA scores at last follow-up postoperatively were significantly higher than that before surgery. These results indicated that transforaminal endoscopic discectomy greatly attenuated the lower-limb pain and promoted the recovery of neurological functions of obese patients with LDH. Lower-limb radiation pain in obese patients with LDH is caused by mechanical compression on the nerve root and chemical irritation [22]. The key point to success in transforaminal endoscopic discectomy is the proper placement of a working channel and the full enlargement of the intervertebral foramen, which is the premise on which the technique is based. To achieve this, we used eccentric trephine technique, gradually adjusting the bar and power system under a microscope. In addition, knowledge of the operative indications is another key point. During the operation, we removed and ablated the prominent nucleus pulposus tissue with nucleus pulposus forceps and a radiofrequency knife with a bent head. This not only removed the pain irritant, but also created favorable conditions for the healing of the fibrous ring. The radiofrequency electrode can ablate the hyperergic nerve terminal receptor that grew into a fiber ring fracture. Continuous irrigation with saline can flush out the toxic metabolites in the intervertebral disc, which prevents the accumulation of the by-products of coagulation therapy in the intervertebral disc.
In the present study, 17 cases (25.3%) had excellent outcomes, 39 (58.2%) good, 7 (10.4%) fair, and 4 (5.9%) poor. Overall excellent and good rate was 83.5%. Yeung and Tsou summarized the satisfactory results in 89.3% of the cases after posterolateral endoscopic discectomy for LDH [23]. Schubert et al. showed that excellent or good results were achieved in 95.3% of patients after endoscopic transforaminal nucleotomy with foraminoplasty [24].
In this study, 2 patients experienced abnormal sensations in the export nerve root zone postoperatively, which disappeared after 3 days of treatment with dehydration and administration of hormone therapy. Postoperative hypesthesia of the neural control region is a common complication of PTED [22]. This might be related to the compression or stimulation of the nerve root. Care must be taken during the operation to avoid this injury. First, zygapophysial joints and the nerve root zone should have local anesthesia with 0.5% lidocaine, which relieves the pain when winching the zygapophysial joints and ensures patient safety. Second, the serrated reamer never exceeded the inner edge of the pedicle of the vertebral arch to protect the dura mater and nerve from injury. Third, all operations were done within the vertebral canal and nucleus pulposus tissue was removed carefully and gently under the intervertebral foramen. During the operation, staff should interact with patients to reduce the rate of neurologic damage.
Postoperative recurrence is another complication of TED. Yeung et al. found that the postoperative recurrence rate of PTED reached 3.6~5.0% [22]. The risk factors of postoperative recurrence for LDH after TED are still poorly understood. Some researchers consider it might be related to age, gender, smoking, and trauma [25]. Moliterno et al. indicated that patients with diabetes were more likely to relapse after surgery [25]. Kim et al. showed that the age and BMI of patients experiencing recurrence after TED were significantly greater than that of patients with no recurrence [26]. These data indicated that higher BMI might result in repeat herniation of the nucleus pulposus after TED. In this study, 3 cases of recurrence were observed, and their BMIs were 42.31kg/m2 (morbid obesity), 46.18 kg/m2 (morbid obesity), and 51.36 kg/m2 (super obesity). These data indicated that the recurrence rate after TED might be related to the high BMI, which needs to be verified by prospective cohort studies with larger sample sizes.
Conclusions
The early efficacy of TED is a relatively good, safe, and minimally invasive treatment for obese patients with LDH. Larger-sample studies with longer duration and follow-up are required to determine the safety and effectiveness of TED.
Footnotes
Conflict of interest
The authors have no actual or potential conflicts of interest to declare.
Source of support: Departmental sources
References
- 1.Eguchi Y, Oikawa Y, Suzuki M, et al. Diffusion tensor imaging of radiculopathy in patients with lumbar disc herniation: Preliminary results. Bone Joint J. 2016;98-b(3):387–94. doi: 10.1302/0301-620X.98B3.36036. [DOI] [PubMed] [Google Scholar]
- 2.Birbilis TA, Matis GK, Theodoropoulou EN. Spontaneous regression of a lumbar disc herniation: Case report. Med Sci Monit. 2007;13(10):CS121–23. [PubMed] [Google Scholar]
- 3.Rasouli MR, Rahimi-Movaghar V, Shokraneh F, et al. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst Rev. 2014;9:Cd010328. doi: 10.1002/14651858.CD010328.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gadjradj PS, van Tulder MW, Dirven CM, et al. Clinical outcomes after percutaneous transforaminal endoscopic discectomy for lumbar disc herniation: A prospective case series. Neurosurg Focus. 2016;40(2):E3. doi: 10.3171/2015.10.FOCUS15484. [DOI] [PubMed] [Google Scholar]
- 5.Suwa H, Hanakita J, Ohshita N, et al. Postoperative changes in paraspinal muscle thickness after various lumbar back surgery procedures. Neurol Med Chir (Tokyo) 2000;40(3):151–54. doi: 10.2176/nmc.40.151. discussion 154–55. [DOI] [PubMed] [Google Scholar]
- 6.Skolasky RL, Wegener ST, Maggard AM, Riley LH., III The impact of reduction of pain after lumbar spine surgery: The relationship between changes in pain and physical function and disability. Spine. 2014;39(17):1426–32. doi: 10.1097/BRS.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 7.Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010;10(7):575–80. doi: 10.1016/j.spinee.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Heliovaara M. Body height, obesity, and risk of herniated lumbar intervertebral disc. Spine. 1987;12(5):469–72. doi: 10.1097/00007632-198706000-00009. [DOI] [PubMed] [Google Scholar]
- 9.De la Garza-Ramos R, Bydon M, Abt NB, et al. The impact of obesity on short- and long-term outcomes after lumbar fusion. Spine. 2015;40(1):56–61. doi: 10.1097/BRS.0000000000000655. [DOI] [PubMed] [Google Scholar]
- 10.McGuire KJ, Khaleel MA, Rihn JA, et al. The effect of high obesity on outcomes of treatment for lumbar spinal conditions: Subgroup analysis of the spine patient outcomes research trial. Spine. 2014;39(23):1975–80. doi: 10.1097/BRS.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li X, Dou Q, Hu S, et al. Treatment of cauda equina syndrome caused by lumbar disc herniation with percutaneous endoscopic lumbar discectomy. Acta Neurol Belg. 2016;116(2):185–90. doi: 10.1007/s13760-015-0530-0. [DOI] [PubMed] [Google Scholar]
- 12.Choi KC, Kim JS, Park CK. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician. 2016;19(2):E291–300. [PubMed] [Google Scholar]
- 13.Bayramoglu M, Akman MN, Kilinc S, et al. Isokinetic measurement of trunk muscle strength in women with chronic low-back pain. Am J Phys Med Rehabil. 2001;80(9):650–55. doi: 10.1097/00002060-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Fanuele JC, Abdu WA, Hanscom B, Weinstein JN. Association between obesity and functional status in patients with spine disease. Spine. 2002;27(3):306–12. doi: 10.1097/00007632-200202010-00021. [DOI] [PubMed] [Google Scholar]
- 15.Burks CA, Werner BC, Yang S, Shimer AL. Obesity is associated with an increased rate of incidental durotomy in lumbar spine surgery. Spine. 2015;40(7):500–4. doi: 10.1097/BRS.0000000000000784. [DOI] [PubMed] [Google Scholar]
- 16.Meng F, Cao J, Meng X. Risk factors for surgical site infections following spinal surgery. J Clin Neurosci. 2015;22(12):1862–66. doi: 10.1016/j.jocn.2015.03.065. [DOI] [PubMed] [Google Scholar]
- 17.Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Transforaminal versus interlaminar approach. Pain Physician. 2013;16(6):547–56. [PubMed] [Google Scholar]
- 18.Gadjradj PS, Harhangi BS. Percutaneous transforaminal endoscopic discectomy for lumbar disk herniation. Clin Spine Surg. doi: 10.1097/BSD.0000000000000366. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Kim CH, Chung CK, Sohn S, et al. The surgical outcome and the surgical strategy of percutaneous endoscopic discectomy for recurrent disk herniation. J Spin Disord Tech. 2014;27(8):415–22. doi: 10.1097/BSD.0b013e3182a180fc. [DOI] [PubMed] [Google Scholar]
- 20.Pan Z, Ha Y, Yi S, Cao K. Efficacy of Transforaminal Endoscopic Spine System (TESSYS) technique in treating lumbar disc herniation. Med Sci Monit. 2016;22:530–39. doi: 10.12659/MSM.894870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoogland T, Schubert M, Miklitz B, Ramirez AL. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: A prospective randomized study in 280 consecutive cases. Spine. 2006;31(24):E890–97. doi: 10.1097/01.brs.0000245955.22358.3a. [DOI] [PubMed] [Google Scholar]
- 22.Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am. 2007;38(3):363–72. doi: 10.1016/j.ocl.2007.04.005. abstract vi. [DOI] [PubMed] [Google Scholar]
- 23.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: Surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27(7):722–31. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 24.Schubert M, Hoogland T. Endoscopic transforaminal nucleotomy with foraminoplasty for lumbar disk herniation. Oper Orthop Traumatol. 2005;17(6):641–61. doi: 10.1007/s00064-005-1156-9. [DOI] [PubMed] [Google Scholar]
- 25.Moliterno JA, Knopman J, Parikh K, et al. Results and risk factors for recurrence following single-level tubular lumbar microdiscectomy. J Neurosurg Spine. 2010;12(6):680–86. doi: 10.3171/2009.12.SPINE08843. [DOI] [PubMed] [Google Scholar]
- 26.Kim JM, Lee SH, Ahn Y, et al. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007;50(2):82–85. doi: 10.1055/s-2007-982504. [DOI] [PubMed] [Google Scholar]