Abstract
Objective
To evaluate the feasibility of access sheath insertion and ureteric stent placement without image guidance in flexible ureteroscopic lithotripsy with holmium:yttrium-aluminium-garnet laser for renal stones.
Patients and methods
Between March 2014 and October 2015, 80 patients with renal stones treated with flexible ureteroscopic laser lithotripsy were evaluated. Indications for surgery were renal obstruction, failed shockwave lithotripsy (SWL), stones in polycystic kidneys, and mal-rotated kidneys. A 6.5-F Cobra flexible ureteroscope was used in all cases with an access sheath of 12 F, 35/45 cm in length. Fluoroscopy was not intended for use in all cases and postoperative JJ stenting was optional. The perioperative complications were listed and the collected data were analysed.
Results
The study included 80 patients (66 male, 14 female), with a mean (SD; range) age of 48.2 (8; 28–54) years and a stone burden of 13 (3.5; range 6–23) mm. In all, 26 patients had a stone burden of >15 mm and 48 patients had lower calyceal stones. The mean (SD; range) operative time was 71.5 (20; 25–130) min. Overall, 76 (95%) access sheath insertions were performed successfully without the use of fluoroscopy. JJ stenting was used in 22 patients (27.5%). The mean (SD; range) hospital stay was 10 (8.5; 10–36) h. After one session, a stone-free rate (SFR) of 87.5% was achieved (93.3% for stones of <15 mm). A single session was successful in 87.9% of cases with lower calyceal stones, with a SFR of 91.7% for post-SWL failure cases. The perioperative complication rate was 15%.
Conclusion
Access sheath insertion without fluoroscopic guidance is feasible. This technique reduces radiation exposure in patients requiring flexible ureteroscopy.
Abbreviations: KUB, plain abdominal radiograph of the kidneys ureters and bladder; PCNL, percutaneous nephrolithotomy; PCS, Pelvicalyceal system; SFR, stone-free rate; SWL, shockwave lithotripsy; URS, ureteroscopy; URSL, ureteroscopic laser lithotripsy; US, ultrasonography/ultrasound; YAG, yttrium-aluminium-garnet
Keywords: Renal calculi, Ureteroscopy, Ho:YAG laser, Lithotripsy
Introduction
In the last two decades, shockwave lithotripsy (SWL) has been the first-line treatment for upper ureteric calculi of <20 mm. However, these stones are increasingly being treated by flexible ureteroscopes with holmium:yttrium-aluminium-garnet (Ho:YAG) laser lithotripsy. Growing awareness of the radiation hazards associated with routine medical imaging and intraoperative exposure has prompted the search for methods to reduce patient, surgeon, and intraoperative team exposure [1]. The USA Food and Drug Administration recommend that physicians reduce radiation exposure during imaging studies and fluoroscopic-guided procedures [2]. During flexible ureteroscopic lithotripsy, the placement of a ureteric access sheath exposes the patient to significant amounts of radiation. Thus, the goal is to insert the access sheath without the use of fluoroscopy. In the present study, we evaluated the feasibility of access sheath insertion and ureteric stent placement without image guidance in flexible ureteroscopic lithotripsy with Ho:YAG laser for renal stones.
Patients and methods
Between March 2014 and October 2015, 80 patients with renal stones treated with flexible ureteroscopic laser lithotripsy (URSL) were evaluated. Indications for surgery were: renal obstruction, failed SWL, stones in polycystic kidneys, and mal-rotated kidneys, calculi in calyceal diverticula, calculi in inferior calyces with narrow, long infundibulum, calculus in a patient with severe kyphoscoliosis and presence of coagulopathy, including use of warfarin. A Cobra flexible ureteroscope (6.5 F Wolf) was used in all cases with an access sheath of 12 F, 35/45 cm in length (Fig. 1A–C), and Road runner guidewires. A fluoroscope was not intended to be used in any of the cases. Intraoperative stenting was optional and stents were inserted under direct vision using a rigid 8-F ureteroscope with a 5-F working channel. The perioperative complications were recorded.
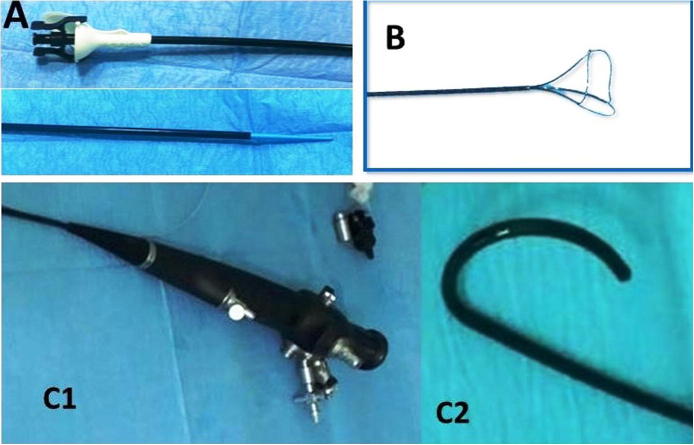
Figure 1.
(A) Access sheath 12 F, 45 cm in length. (B) The NGage stone basket. C1–C2, the flexible ureteroscope, its base and flexed tip.
Surgical procedure
All patients received prophylactic parenteral third generation cephalosporin antibiotics (Ceftriaxone) preoperatively. General anaesthesia and endotracheal intubation or laryngeal mask associated with neuromuscular blockage was used for all patients.
Briefly, after diagnostic ureteroscopy (URS), a 0.64-mm straight tip Terumo guidewire was smoothly positioned in the kidney and a 0.89-mm straight tip Road runner guidewire was inserted in the ureter up to the kidney. Ureteric dilatation was performed by the use of two semi-rigid ureteroscopes. The first ureteroscope 6–7.5 F was inserted and maintained in situ for 2 min, followed by the second larger ureteroscope 8.5–11 F under direct vision. The introduction of a 12-F access sheath after dilatation was feasible and convenient without any difficulties in most of the cases. Presence of a pre-existing stent obviated the need for dilatation. Using good lubrication, a cystoscopic sheath 18–22 F was inserted guided with the Road runner guidewire into the bladder. A technique was devised to allow placement of a ureteric access sheath without image guidance by replacing fluoroscopy with visual and tactile cues. The access sheath 12 F, 35/45 cm in length (Navigator, Boston Scientific Corp., USA) was used in all patients (Fig. 1A), as it yields direct access to the renal pelvis, better fluid irrigation, and permits removal of stone fragments. In female patients, we attempted to use the short access sheath (35 cm) without the cystoscopic sheath. We fixed an 8-F Foley catheter to maintain bladder drainage during the procedure instead the cystoscopic sheath in females.
The flexible ureteroscope (Richard Wolf Medical Instruments Corp., USA) has outer and tip diameters of 9.9 F and 6 F, respectively. This instrument has the same upwards and downwards deflection of 270°. It was introduced through the access sheath to the renal pelvis (Fig. 1C) [3]. Once the scope reaches the pelvicalyceal system, it is rotated gently on both sides with use of the deflecting mechanism, to visualise the pelvicalyceal system clearly. Continuous irrigation and/or intermittent manual pumping of normal saline ensured a clear ureteroscopic view. Once the particular calyx is identified and the calculus is seen, the Ho:YAG laser was inserted (200–272 μm fibre, Megapulse stone laser, Richard Wolf Medical Instruments Corp.) for fragmentation. The laser apparatus settings were adjusted to produce 200–4000 mJ with a pulse frequency of 3–25 Hz. After complete fragmentation, the process is stopped when only very small stone fragments (2 mm) are seen, avoiding the need for basket stone retrieval. The laser fibre was withdrawn and the calyx flushed with saline under pressure to clear the fragments. When the stone is fragmented into significant fragments (>3 mm), the fragments were removed with the zero-tip NGage basket (Cook Urological Inc., USA) (Fig. 1B).
If the lower pole calyx stones could not be fragmented, the ureteroscope was moved to a less dependent calyx position by using the NGage basket or water flush, thus facilitating stone fragmentation and removal. All collecting systems were inspected at the end of fragmentation (Fig. 2A and B).
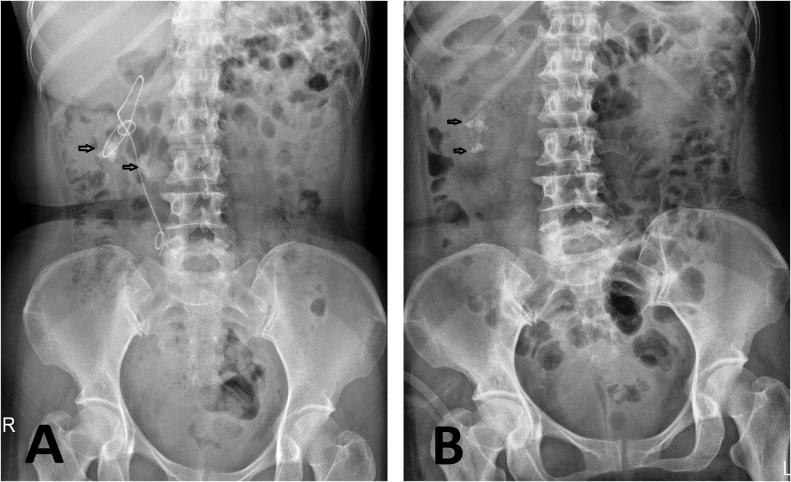
Figure 2.
(A) KUB showed a right JJ stent migrated to the kidney and multiple radiopaque shadows in the region of the right kidney. (B) KUB after flexible URS for the same patient, residual renal stones and JJ stent have been removed.
Ureteric stenting was also performed, as it is recommended after completion of ureteroscopic lithotripsy if ureteric injury, stricture, solitary kidney, renal insufficiency, or a large residual stone burden is present. A JJ 4-F ureteric stenting (Marflow AG, Soodstrasse, Zurich, Switzerland) was performed when indicated in 22 patients without the use of the fluoroscope. The ureteric stent is inserted through the 8.5–11 F ureteroscope (working channel 5 F) under direct vision after flexible URS. The upper coil is delivered easily under direct vision into the renal pelvis and the lower coil is delivered into the bladder. The stent was removed after ∼2 weeks. All patients were treated on a day-case basis, and all procedures were scheduled as outpatient procedures unless any complications occurred during the procedure.
Follow-up
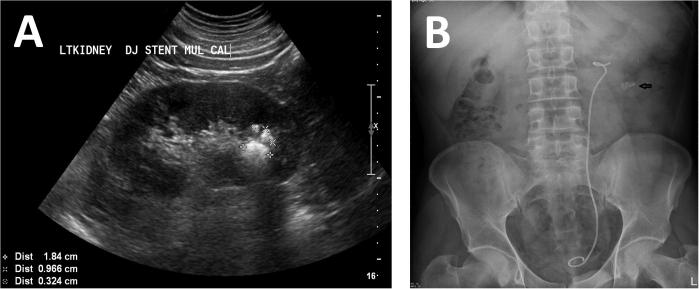
All patients were available for their 2-week and 3-month follow-ups, which consisted of imaging studies comprising of a plain abdominal radiograph of the kidneys, ureters and bladder (KUB) (Fig. 2B) and ultrasonography (US). The US, KUB or CT-KUB were used as a control for all patients at the last follow-up (Figure 3, Figure 4). Results were classified by the largest single fragment as: stone-free (no residual fragments observed or residual fragments of <3 mm), residual stone (stones >3 mm requiring a second procedure), or failure (due to intraoperative complications or technical problems).
Figure 3.
(A) Renal US showed multiple lower pole stones and the tip of the JJ stent intrarenal. (B) KUB for the same patient showed multiple radiopaque shadows in the region of left kidney and a left JJ stent in situ.
Figure 4.

CT KUB (Coronal film) with reconstruction techniques for urolithiasis showed bilateral renal calyceal stones.
Complications were categorised into intraoperative (limited to ureteric perforation) or postoperative complications (hospitalisation extension for >12 h for pain or haematuria).
Statistical analysis
Data were statistically analysed using SPSS V. 21 for Windows and Epi info program, with a P < 0.05 considered statistically significant for all results. Data are shown as the mean (SD) and range, 95% CI, frequency and percentage. The chi-squared test was used for qualitative variable analysis, along with Fischer’s exact test for 2 × 2 tables, when the expected cell count was <5 in >25% of cases. Student’s t-test was used for normally distributed quantitative variables to measure means and SDs. The Z-test was also performed. The Kolmogorov–Smirnov Z-test indicated that most of the data was normally distributed, allowing parametric tests to be performed to establish associations.
Results
The study included 80 patients (66 male, 14 female), with a mean (SD; range) age of 48.2 (8; 28–54) years, with a stone burden of 13 (3.5; 6–23) mm. A stone burden of >15 mm, lower calyceal stones, and a single renal stone were reported in 26 (32.5%), 48 (60%) and 52 (65%) patients, respectively. Ureteric stones were seen in association with renal stones in 13 (16.3%) patients. These patients were managed first with ureteroscopic lithotripsy and JJ-stent insertion followed by the flexible URS procedure for renal stones after 2 weeks. Only 10 patients had bilateral renal stones (Table 1). Indications for surgery were failure of SWL in 36 patients (45%), pain in 28 (35%), UTIs in four (5%), and calcular obstruction in eight (10%). Three patients (3.75%) had polycystic kidney disease and another patient was using acetylsalicylic acid. The mean (SD; range) operative time was 71.5 (20; 25–130) min. Fluoroscopy guidance was used in four cases only (5%) due to failure of our technique, whilst 22 (27.5%) patients required JJ stenting at the end of the procedure. The mean (SD; range) hospital stay was 10 (8.5; 10–36) h (Table 2).
Table 1.
Demographics of patients treated with flexible URSL with Ho:YAG laser for renal calculi.
| Variable | Value | Test of sig. Z-test | P |
|---|---|---|---|
| Mean (SD; range) age, years | 48.2 (8; 28–54) | ||
| Male/female, n | 66/14 | 8.3 | <0.001 |
| Right/left, n | 18/62 | 8.1 | <0.001 |
| Symptomatic/asymptomatic, n | 72/8 | 10.1 | <0.001 |
| Associated ureteric stones, n (%) | 13 (16.3) | 8.6 | <0.001 |
| Bilateral/unilateral, n | 10/70 | 9.4 | <0.001 |
| Single/multiple, n | 52/28 | 3.8 | <0.001 |
| Lower calyx/different calyces, n | 48/32 | 2.5 | 0.01 |
| Mean (SD; range) stone size, mm | 8.4 (2.6; 3–23) | 3.4 | <0.001 |
| Mean (SD; range) stone number | 2.2 (0.3; 3–8) | 2.9 | 0.001 |
| Mean (SD; range) stone burden, mm | 13 (2.5; 6–23) | 4.3 | <0.001 |
| Stone burden (mm), n (%) | |||
| <15 | 64 (80) | 7.6 | <0.001 |
| ⩾15 | 26 (20) | 7.6 | <0.001 |
| Localisation, n (%) | |||
| Lower calyx | 58 (72.5) | 5.8 | <0.001 |
| Other calyces | 18 (22.5) | 6.8 | <0.001 |
| Pelvis | 4 (5) | 11.4 | <0.001 |
Table 2.
Operative data.
| Variables | Value | Test of sig. | P |
|---|---|---|---|
| Mean (SD; range) operative time, min | 71.5 (20; 25–130) | 1.7⁎ | 0.09 |
| Use of fluoroscopy guidance, n (%) | 4 (5) | 11.99† | 0.001 |
| JJ stenting, n (%) | 22 (27.5) | ||
| No stenting, n (%) | 58 (72.5) | 0.2† | 0.47 |
| Mean (SD; range) hospital stay, h | 10 (8.5; 10–36) | 2.24⁎ | 0.02 |
| SFR, n/N (%) | |||
| <15 mm | 60/64 (93.3) | ||
| >15 mm | 10/16 (62.5) | 8.75† | 0.003 |
| Lower calyx | 51/58 (87.9) | ||
| Different calyces | 16/18 (94.4) | 0.09† | 1 |
| Pelvis | 3/4 | ||
| After SWL | 33/36 (91.7) | 0.03† | 0.36 |
t-Test.
Fisher’s exact test.
Stone-free rate (SFR)
A SFR of 87.5% (70/80 patients) was achieved. A single session was successful in 87.9% (51/58) of patients with lower calyceal stones and 91.7% (33/36) of patients after SWL failure. However, overall stone clearance occurred in 62.5% (10/16) and 93.3% (60/64) of patients, with stone sizes of >15 and <15 mm, respectively (Table 2).
Complications
The overall complication rate was 15% (Table 3), with four patients (5%) having intraoperative complications due to failure of the insertion of the access sheath, as a result of kinks in the ureter or a small calibre ureter. Prolonged gross haematuria occurred in eight patients (10%) postoperatively and was managed conservatively with bed rest, haemostatic drugs, and i.v. fluids; if urine was not cleared within 12 h we extended the patient stay until the urine became clear. One patient developed a UTI and fever, and was hospitalised and managed with i.v. antibiotic and fluids, according to the urine and blood culture. Following the procedure, 76 patients (95%) were discharged at ⩽12 h and only four (5%) required a longer stay due to pain or haematuria.
Table 3.
Postoperative complications.
| Postoperative complications | n/N (%) | Test of sig. Z-test | P |
|---|---|---|---|
| Failure of access sheath insertion | 4/80 (5) | 11.4 | <0.001 |
| Ureteric perforation | – | 12.6 | <0.001 |
| Prolonged haematuria | 8/80 (10) | 10.1 | <0.001 |
| UTI | 1/80 (1.3) | 9.4 | <0.001 |
Discussion
Flexible URS is an efficient therapeutic tool, benefiting from reduced ureteroscope size, greater working channel size, and small stone baskets for stone extraction and holmium laser fibres for stone fragmentation. The active deflection of the flexible ureteroscope into acute angles enables access to all calyces, including the lower calyx [4]. Flexible URS is usually performed under general anaesthesia [3], [4]. In our present study, all patients underwent general anaesthesia and neuromuscular blockage to facilitate stone access.
A ureteric sheath allows fast, safe, and multiple accesses to the upper urinary tract, as well as increasing ureteroscope lifespan, whilst decreasing intra-renal pressure by continuous drainage [3], [4], [5]. More effective irrigant flow also increases visibility. The use of normal saline with continuous drainage of the irrigant fluid decreases any risk of hyper-absorption of the fluid. In our present study, the use of a cystoscope sheath during the procedure also ensured continuous bladder drainage, whilst supporting the access sheath. We used a 35-cm length without a cystoscope sheath for females and 45-cm length with a cystoscope sheath of 16–20 F for male patients. We replaced the cystoscope sheath in females with an 8-F Foley catheter to maintain bladder drainage during the procedure.
Wu et al. [6] described a technique using fluoroscopy for positioning the proximal and distal stent coils. In our institution, fluoroscopy free access sheath placement has evolved, as we use progressively less fluoroscopy during endoscopic cases. We believe that this technique could be easily adapted to any urological practice and will facilitate fluoroscopy reduction in all patients undergoing ureteroscopic lithotripsy.
The impetus to perform fluoroscopy free procedures is not unique to urology. McGee et al. [7] have performed sacral neuromodulation without fluoroscopic guidance. In urology, many centres have replaced fluoroscopy with the US-guided percutaneous nephrolithotomy (PCNL) technique [8]. Mandhani et al. [9] have successfully performed distal URS in three patients using a fluoro-less method. However, our present study is the first to describe and quantify the results of a technique for ureteric access sheath placement without any form of image guidance.
Our goal was to reduce the amount of fluoroscopy required during ureteroscopic lithotripsy, as up to 3% of annual cancer cases globally are linked to ionising radiation from medical imaging, which is cumulative. Radiation levels 0.01 Sv above background may cause one in 1000 patients to develop neoplasia [1], which may result from ureteroscopic lithotripsy using fluoroscopy [10]. Therefore, efforts should be made to limit such radiation exposure. According to Söylemez et al. [11], whilst 96% of urologists in Turkey use fluoroscopy guidance as the initial choice for PCNL, only 2.8% and 1% use US guidance and CT-guided access, respectively. Moreover, only 46% of urologists always use thyroid shields during fluoroscopy, as these are considered impractical.
The development of the Ho:YAG laser and its application in urology has expanded the use of flexible URS for upper urinary tract stones. Laser energy is rapidly absorbed by water and has minimal tissue effect through a 200-pm core sized fibre. This small fibre allows greater ureteroscope deflection without compromising irrigant flow and consequently visibility [12].
We claim that operative times can be reduced in patients undergoing the fluoroscopy free technique due to the free movement of the team, the lack of use of aprons, protective shields and the avoidance of moving the fluoroscope in and out of the operating table. However, our present operative time is not statistically different from that previously reported [4], [13]. In the future, we plan to conduct a prospective study to compare the operative time, radiation exposure, and complication rate between the fluoroscopic and fluoroscopy free technique.
SFR
Stone-free status after a single procedure is directly related to stone burden. SWL should be considered the first line of therapy for stones of <10 mm, as it has 85% success rate after one procedure [14]. Although success rates of flexible URS may be similar, the more invasive nature of endoscopic surgery counteracts this advantage. The presence of residual fragments after SWL, necessitating multiple procedures, is often associated with stones of >20 mm and lower calyceal location. Owing to the effectiveness of the holmium laser in fragmenting unresponsive stones, flexible retrograde URS can be considered for salvage therapy after SWL failure. Grasso et al. [15] reported that 76% of 45 patients with renal stones of >20 mm that underwent URS were stone free after a single procedure. After second-stage procedures, the success rate increased to 91% without intraoperative complications in 15 patients.
In our present study, fluoroscopy free flexible URSL was successful in 87.5% cases, with 91.7% noted for flexible URSL (33 patients) after failure of SWL. Moreover, the results were related to stone size, especially for stones >15 mm (P = 0.003). A single session was successful in 60 patients (93.3%) with stones of <15 mm and 10 patients (62.5%) with stones of >15 mm. However, we noted that better clearance was achieved for middle and upper calyceal stones (94.4%) compared with lower calyx stones (87.9%, the difference was not statistically significant, P = 0.09). A renal pelvis stone was cleared in only three out of four patients. Our findings are congruent with those reported in the literature [16]. In addition, larger stones required longer operative time [13]. SFRs were also strongly influenced by definition of success (residual fragments of <3 mm). Portis et al. [12] reported a 94.6% SFR based on fragments of <4 mm.
Ureteric stents were placed in prolonged procedures (>60 min), when large amounts of stone debris or evident ureteric oedema/trauma were present [4]. Thus, 22 patients (27.5%) were indicated for stenting, which was performed without fluoroscopy guidance. A new technique was developed by inserting the 4-F stents through the semi-rigid ureteroscope under direct vision.
The 15% complication rate we noted is comparable with other studies. In four cases, we failed to insert the access sheath without fluoroscopic guidance due to ureteric kinks or strictures. In addition, eight patients had postoperative gross haematuria and were treated in hospital with bed rest, haemostatic drugs, and i.v. fluids. It was not clear what the cause of the haematuria was, whether it was due to the non-fluoroscopy guided access sheath insertion or not. Further evaluation is needed to determine the site and the cause of the haematuria. Only one patient had a postoperative UTI, but improved following conservative management.
However, according to Takazawa et al. [17], the success of flexible URS decreases when the treated stone burden increases. In their study, they reported 67% of stones >40 mm required almost two procedures (1.8 procedures), whereas all stones between 20 and 40 mm in size required 1.3 procedures to clear all stones. Thus, PCNL should be the preferential treatment for stones of >40 mm. Recently, the ‘mini-perc’ or ‘tubeless PCNL’ technique was developed, which has a smaller calibre of nephrostomy tract, and would be expected to decrease the risk of perioperative complications. PCNL has an excellent success rate in clearing large renal stones. However, its invasiveness counteracts non-negligible major complication rates. A recent global study of PCNL outcomes reported 7.8% cases of significant bleeding, 3.4% renal pelvis perforation, and 1.8% hydrothorax. Blood transfusions were required in 5.7% of cases, and high-grade fever occurred in 10.5% of the patients [18].
The new robot for flexible URS produced by Elmed-Turkey was recently used in Ankara, Paris, and Heilbronn. Rassweiler et al. [19] reported that Avicenna Roboflex is feasible and suitable for the flexible URS procedure with improved ergonomics, as it is more comfortable to be sitting at a control unit with an armrest and free control of all functions.
A drawback of our new technique is that it needs experienced surgeons and is not suitable for residents and surgeons in training. Moreover, the insertion of the access sheath is a blind procedure, which may cause renal and ureteric injuries. The need for two semi-rigid ureteroscopes for ureteric dilatations under direct vision may not be affordable for all centres, as it increases the cost of the procedure.
The present study, despite a small number of cases, provides valuable evidence of access sheath insertion and JJ stenting without fluoroscopic guidance. Nonetheless, further randomised controlled studies are needed to draw firm conclusions.
Conclusion
Access sheath insertion without fluoroscopic guidance is feasible and reduces the risk of radiation exposure. Fluoroscopy free flexible URSL with Ho:YAG laser for the treatment of renal calculi is a safe and effective option. In addition, it achieved >93% stone clearance in stones of <15 mm.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the Institution and/or National Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all the patients.
Conflict of interest
The author declares no conflict of interest.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Berrington de González A., Darby A. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345–351. doi: 10.1016/S0140-6736(04)15433-0. [DOI] [PubMed] [Google Scholar]
- 2.USA Food and Drug Administration. Initiative to reduce unnecessary radiation exposure from medical imaging. Available at: <http://www.fda.gov/Radiation-EmittingProducts/RadiationSafety/RadiationDoseReduction/ucm2007191.htm> [accessed April 2016].
- 3.Doddamani D., Sinha T., Talwar R. Efficacy of flexible fibreoptic ureteroscopy and Holmium laser in retrograde intrarenal surgery for calyceal calculi. MJAFI. 2011;67:217–220. doi: 10.1016/S0377-1237(11)60044-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khoder W.Y., Bader M., Sroka R., Stief C., Waidelich R. Efficacy and safety of Ho:YAG laser lithotripsy for ureteroscopic removal of proximal and distal ureteral calculi. BMC Urol. 2014;8:14–62. doi: 10.1186/1471-2490-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.L’esperance J.O., Ekeruo W.O., Scales C.D., Jr., Marguet C.G., Springhart W.P., Maloney M.E. Effect of ureteral access sheath on stone-free rates in patients undergoing ureteroscopic management of renal calculi. Urology. 2005;66:252–255. doi: 10.1016/j.urology.2005.03.019. [DOI] [PubMed] [Google Scholar]
- 6.Wu N.Z., Auge B.K., Preminger G.M. Simplified ureteral stent placement with the assistance of a ureteral access sheath. J Urol. 2001;166:206–208. [PubMed] [Google Scholar]
- 7.McGee S.M., Routh J.C., Granberg C.F., Roth T.J., Hollatz P., Vandersteen D.R. Sacral neuromodulation in children with dysfunctional elimination syndrome: description of incisionless first stage and second stage without fluoroscopy. Urology. 2009;73:641–644. doi: 10.1016/j.urology.2008.10.067. [DOI] [PubMed] [Google Scholar]
- 8.Gamal W.M., Hussein M., Aldahshoury M., Hammady A., Osman M., Moursy E. Solo ultrasonography-guided percutaneous nephrolithotomy for single stone pelvis. J Endourol. 2011;25:593–596. doi: 10.1089/end.2010.0558. [DOI] [PubMed] [Google Scholar]
- 9.Mandhani A., Chaudhury H., Gupta N., Singh H.K., Kapoor R., Kumar A. Is fluoroscopy essential for retrieval of lower ureteric stones? Urol Int. 2007;78:70–72. doi: 10.1159/000096938. [DOI] [PubMed] [Google Scholar]
- 10.National Research Council . National Academies Press; Washington DC: 2006. Health risk from exposure to low levels of ionizing radiation: BEIR VII phase 2; pp. 7–8. [Google Scholar]
- 11.Söylemez H., Altunoluk B., Bozkurt Y., Sancaktutar A.A., Penbegül N., Atar M. Radiation exposure. Do urologists take it seriously in Turkey? J Urol. 2012;187:1301–1305. doi: 10.1016/j.juro.2011.11.110. [DOI] [PubMed] [Google Scholar]
- 12.Portis A.J., Rygwall R., Holtz C., Pshon N., Laliberte M. Ureteroscopic laser lithotripsy for upper urinary tract calculi with active fragment extraction and computerized tomography follow up. J Urol. 2006;175:2129–2134. doi: 10.1016/S0022-5347(06)00311-9. [DOI] [PubMed] [Google Scholar]
- 13.Cocuzza M., Colombo J.R., Cocuzza A.L., Mascarenhas F., Vicentini F., Mazzucchi E. Outcomes of flexible ureteroscopic lithotripsy with holmium laser for upper urinary tract calculi. Int Braz J Urol. 2008;34:143–150. doi: 10.1590/s1677-55382008000200003. [DOI] [PubMed] [Google Scholar]
- 14.Netto N.R., Claro J.F., Lemos G.C., Cortado P.L. Renal calculi in lower pole calices: what is the best method of treatment? J Urol. 1991;146:721–723. doi: 10.1016/s0022-5347(17)37905-3. [DOI] [PubMed] [Google Scholar]
- 15.Grasso M., Conlin M., Bagley D. Retrograde ureteropyeloscopic treatment of 2 cm or greater upper urinary tract and minor staghorn calculi. J Urol. 1998;160:346–351. [PubMed] [Google Scholar]
- 16.Sofer M., Watterson J.D., Wollin T.A., Nott L., Razvi H., Denstedt J.D. Holmium:YAG laser lithotripsy for upper urinary tract calculi in 598 patients. J Urol. 2002;167:31–34. doi: 10.1016/s0022-5347(05)65376-1. [DOI] [PubMed] [Google Scholar]
- 17.Takazawa R., Kitayama S., Tsujii T. Successful outcome of flexible ureteroscopy with holmium laser lithotripsy for renal stones 2 cm or greater. Int J Urol. 2012;19:264–267. doi: 10.1111/j.1442-2042.2011.02931.x. [DOI] [PubMed] [Google Scholar]
- 18.De la Rosette J., Assimos D., Desai M., Gutierrez J., Lingeman J., Scarpa R. The clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–17. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 19.Rassweiler J., Saglam R., Traxer O., Kabakci A.S., Tokatli Z., Imamoglu A. V6-01 Robot assisted flexible ureteroscopic laser lithotripsy with Avicenna Roboflex. J Urol. 2015;193(Suppl.):576–577. [Google Scholar]