Abstract
Objective
To prospectively compare the use of external ureteric stents with internal JJ stenting of the uretero-ileal anastomosis in patients undergoing laparoscopic radical cystectomy (LRC) with a Y-shaped ileal orthotopic neobladder (ON).
Patients and methods
The study included 69 patients undergoing LRC with ON. Patients were grouped according to the type of uretero-ileal stents used. An external ureteric stent was used in Group A (33 patients) and a JJ stent was used in Group B (36). We prospectively compared the duration of hospital stay, the incidence of short- and intermediate-term complications in the two study groups.
Results
The mean (SD) follow-up periods were 29.18 (3.94) and 28.19 (3.37) months for patients in Groups A and B, respectively. Perioperative patient characteristics were comparable in the two study groups. The use of JJ stenting was associated with a shorter hospital stay compared with external stenting, at a mean (SD) of 14.63 (3.74) and 6.8 (3.03) days in Groups A and B, respectively (P < 0.001). The incidence of urinary leakage was comparable in the two study groups, at 6.1% in Group A vs 8.3% in Group B (P = 1.0). Strictures of the uretero-ileal anastomosis occurred in two patients (6%) in Group A and confirmed by intravenous urography. All strictures were treated with antegrade JJ fixation.
Conclusion
JJ stents could be used as an effective alternative to external ureteric stents to support the uretero-ileal anastomosis. JJ stenting is associated with a shorter hospital stay and similar complication rates compared with external stenting in patients undergoing LRC with ON.
Abbreviations: ASA, American Society of Anesthesiologists; ON, orthotopic neobladder; (L)RC, (laparoscopic) radical cystectomy; US, ultrasonography
Keywords: Urinary diversion, Uretero-ileal anastomosis, External ureteral catheters, Internal JJ stents, Ileal neobladder
Introduction
Radical cystectomy (RC) remains the current ‘gold standard’ treatment for muscle-invasive bladder cancer [1]. An orthotopic neobladder (ON) after RC offers better body image preservation and quality of life compared with other means of urinary reconstruction [2], [3], [4], [5]. A study reported that patients tended to choose an ON for urinary reconstruction following RC [6].
Many authors recommend stenting of the uretero-ileal anastomosis to guarantee proper alignment of the anastomosis, thus preventing ureteric obstruction from oedema or ureteric leaks. The stent also acts as a mould around which the anastomosis heals, subsequently lowering the stricture rate [7], [8], [9]. One of the common techniques for stenting of the uretero-ileal anastomosis is external drainage with external ureteric catheters [10]. However, the use of indwelling JJ ureteric stents has been reported as an alternative [9], [11], [12].
To the best of our knowledge, there are few published reports on the use of JJ stents for uretero-ileal anastomosis in ON after RC, and most of these reports are retrospective [9], [11], [12]. Moreover, there are no previous published reports for the use of JJ stents in patients undergoing laparoscopic RC (LRC). We performed this prospective cohort study to compare the use of conventional externalised ureteric stents with internal JJ stenting for the uretero-ileal anastomosis in patients undergoing LRC with a Y-shaped ileal ON.
Patients and methods
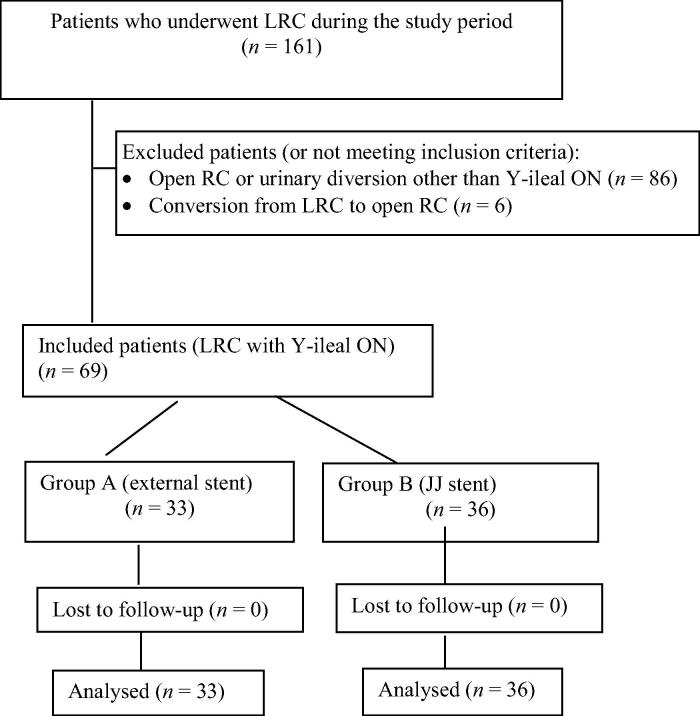
All patients with muscle-invasive TCC or high-risk and recurrent non-invasive TCC of the bladder who underwent LRC with Y-shaped ileal ON, between January 2010 and December 2012, were enrolled in this prospective cohort study. The Institutional Ethical and Research Committee approved the study, and written informed consents were obtained from all included patients. Exclusion criteria were an American Society of Anesthesiologists (ASA) score of >3, preoperative clinical evidence of lymph-node involvement, urinary diversion other than a Y-shaped ileal ON, and other contraindications for pneumoperitoneum including congestive heart failure or severe chronic obstructive lung disease. Patients with conversions to open surgery were also excluded. Additionally, patients with contraindications to ON were excluded including urethral involvement, poor liver function, and poor renal function (Fig. 1).
Figure 1.
Flow chart of patient groups and follow-up.
After performing a completely intracorporeal LRC using the technique described by Abdel Hakim et al. [13], an ileal ON and uretero-ileal anastomosis were completed extracorporeally through a 7-cm Pfannenstiel incision. The Y-shaped ileal ON was constructed using a 45-cm segment of ileum folded in a Y-shape. In all cases the ureters were implanted using a Nesbit-type anastomosis with ureteric end spatulation. The urethro-ileal anastomosis was then made intracorporeally, after closure of the Pfannenstiel incision and re-establishing pneumoperitoneum.
Two groups of patients were evaluated according to the type of uretero-ileal anastomosis stent used. In Group A, a 7-F silastic feeding tube (externalised through the ON and abdominal wall, and fixed to the skin) was used to stent the uretero-ileal anastomosis. In Group B, a polyurethane 7-F JJ stent (28 cm in length) was used to stent the uretero-ileal anastomosis. The distal end of the JJ stent was sutured to the ON mucosa with a 3/0 absorbable suture to facilitate later identification during transurethral removal and to prevent proximal migration. We did not use a suprapubic tube but the ON was drained with a 22-F silicone catheter.
Starting on the third postoperative day, ONs were irrigated using saline solution every 8 h in both groups until the catheter was removed. The tube drains were removed when output stopped. In both groups, patients were discharged when they were tolerating regular diet, ambulant, with good pain control, and with no leakage into the drains. In both groups, the Foley catheter was removed at 3 weeks after excluding extravasation by a pouchogram. In Group A, the external ureteric catheters were removed successively around the 10th postoperative day and before patient discharge. In Group B, JJ stents were cystoscopically removed at 6 weeks postoperatively. Renal ultrasonography (US) was performed during the immediate postoperative period in all patients to detect any urinary obstruction.
Postoperatively, all patients were evaluated every 3 months during the first year and every 6 months thereafter. Evaluation included clinical examination and laboratory evaluation in addition to abdominal US. CT was performed 6 months postoperatively and then yearly. IVU was performed in patients with suspected uretero-ileal anastomotic stricture. The duration of hospital stay and complications related to stent type were compared for both groups.
Sample size estimation
The sample size was calculated according to the duration of hospital stay. A previous retrospective study reported a mean duration of hospital stay of 15.2 and 9.9 days with the use of external and JJ stenting in patients undergoing conventional open RC, respectively [9]. Assuming a standard deviation (SD) of 6 days, a power of 80% and an α error of 0.05, the minimum estimated sample size in each of the two study groups was 21 patients. The PS Power and Sample Size Calculations Software, version 3.1.2 for MS Windows (William D. Dupont and Walton D. Vanderbilt, USA) was used for sample size calculation.
Statistical analysis
Student’s t-test or Mann–Whitney test was used to compare continuous data. Categorical data were compared using the chi-square test or Fisher’s exact test, as appropriate. A P < 0.05 was considered significant. SPSS software v15.0 for Windows was used for statistical analysis (SPSS Inc., Chicago, IL, USA).
Results
Group A included 33 patients and Group B 36 patients (Fig. 1). The mean patient age in the two study groups at the time of surgery was 58.2 years. The preoperative characteristics were comparable in the two study groups (Table 1). Hospitalisation was shorter (P < 0.001) in the JJ-stent group (Group B) (Table 2). External stents were removed after a mean (SD) of 12.63 (3.74) days and the JJ stents were removed after a mean (SD) of 42.83 (5.06) days. In both groups, the catheter was removed from the ON after a mean (SD) of 3.3 (0.9) weeks. The transurethral removal of JJ stents was time consuming in three patients, as the reconstructed ON was folded up on itself. In one of these patients, the stent on one side was removed via an antegrade approach under fluoroscopy guidance. After these initial three cases, we resorted to suturing the JJ stents to ON mucosa to allow easy cystoscopic visualisation and removal.
Table 1.
Preoperative characteristics of the patients.
| Variable | Group A external stent |
Group B JJ stent |
P |
|---|---|---|---|
| Number of patients | 33 | 36 | |
| ASA grade, n (%) | 0.826 | ||
| I | 5 (15.2) | 7 (19.4) | |
| II | 22 (66.7) | 24 (66.7) | |
| III | 6 (18.2) | 5 (13.9) | |
| Clinical stage, n (%) | 0.616 | ||
| Tis–T2 | 22 (66.7) | 26 (72.2) | |
| T3a–T4 | 11 (33.3) | 10 (27.8) | |
| Mean (SD; range) serum creatinine, mg/dL | 1.15 (0.28; 0.6–1.9) | 1.24 (0.27; 0.5–1.8) | 0.192 |
| Mean (SD; range) serum albumin, g/dL | 3.93 (0.28; 3.4– 4.6) | 3.95 (0.25; 3.5– 4.5) | 0.771 |
| Diabetes mellitus, n (%) | 3 (9.1) | 4 (11.1) | 1 |
| Hydronephrosis, n (%) | 16 (48.5) | 14 (38.9) | 0.422 |
Table 2.
Operative and postoperative data.
| Variable | Group A External stent |
Group B JJ stent |
P |
|---|---|---|---|
| Number of patients | 33 | 36 | |
| Mean (SD; range) | |||
| Operative time, h | 5.9 (0.94; 5–7) | 5.55 (0.73; 5–7) | 0.132 |
| Blood loss, mL | 757.57 (283.9; (300–1200) | 755.55 (281.26; (400–1300) | 0.966 |
| N (%) | |||
| Blood transfusion | 17 (51.5) | 17 (47.2) | 0.722 |
| Pathological stage | 0.972 | ||
| T0–T2N0 | 20 (60.6) | 22 (61.1) | |
| T3–T4N0 | 8 (24.2) | 8 (22.2) | |
| N + disease | 5 (15.2) | 6 (16.7) | |
| Mean (SD; range) hospital stay, days | 14.63 (3.74; 12–30) | 6.8 (3.03; 5–20) | <0.001 |
| Complications, n (%) | |||
| Urinary leakage | 2 (6.1) | 3 (8.3) | 1.0 |
| Prolonged ileus | 3 (9.1) | 2 (5.6) | 0.665 |
| Wound dehiscence | 1 (3.0) | 0 | 0.478 |
| Uretero-ileal stricture | 2 (6.1) | 0 | 0.225 |
| Antegrade stent removal | 0 | 1 (2.8) | 1 |
| Mean (SD; range) 6-month postoperative serum creatinine level, mg/dL | 1.12 (0.26; 0.7–1.6) | 1.21 (0.3; 0.5–1.8) | 0.176 |
| Recurrence, n (%) | 1 (3.0) | 1 (2.8) | 1 |
| Mortality, n (%) | 0 | 0 | – |
Early and late complications were evaluated for both groups during a mean (SD) follow-up period of 29.18 (3.94) and 28.19 (3.37) months for patients in Group A and B, respectively (P = 0.362). The patients in Group A required more frequent ON irrigation in the immediate postoperative period (five-times daily in Group A vs only three-times daily in group B). In all cases, no hydronephrosis or worsening of preoperative hydronephrosis was seen on US. Prolonged ileus (>3 days) was reported in five patients [three (9.1%) in Group A and two (5.6%) in Group B] without any significant difference between both groups (P = 0.665). The incidence of urinary leakage was comparable in the two study groups [two patients (6.1%) in Group A and three (8.3%) in Group B; P = 1.0]. An ascending cystourethrography was done for these cases to document the site of leakage, which was the urethro-ileal anastomosis in four patients (two in each group), whilst the last patient had a right uretero-ileal anastomosis leakage (in Group B). All cases of leakage were managed conservatively. As the one patient with uretero-ileal anastomosis leakage was in Group B with a JJ stent already inserted, conservative management was also sufficient with a prolonged duration of drainage and subsequent removal. Strictures of the uretero-ileal anastomosis occurred in two patients (6%) in Group A and were confirmed by IVU. All strictures were successfully treated with antegrade dilatation and JJ-stent insertion (Table 2).
Discussion
There are few reports on the use of JJ stents for uretero-ileal anastomosis after RC, which are all retrospective studies [9], [11], [12]. Moreover, there are no previous published reports on the use of JJ stents in patients undergoing LRC. Thus, we performed this prospective cohort study to compare the use of conventional externalised ureteric stents with internal JJ stenting for the uretero-ileal anastomosis in patients undergoing LRC with a Y-shaped ileal ON.
The results of the present study indicated that the use of JJ stenting was associated with a shorter hospital stay compared with the external stents without a significant difference in complications. The use of internal stents also had other advantages for our present patients. There were fewer drainage bags used (5 vs 2–3 bags for Group A and B, respectively). This gave a better chance for early ambulation with a reduction in both patient anxiety and the nursing staff’s workload as iterated in a previous study [9]. Our routine protocol is to remove the external stents successively starting from the 10th postoperative day preparing the patient for discharge with the urethral catheter only. This is similar to many centres where external stents are removed after this period [9], [14]. Our present patients are mostly of low socioeconomic status with a low educational level and come from remote rural areas where they will not have access to a qualified urologist. This prevents discharge of these particular patients with many urine collection bags to care for. Hence, when using external stents, patients are not discharged except after their removal, as these patients will not be able to receive the required care at home during this critical postoperative period. Thus, using internal stents allowed us to discharge these patients earlier without compromising the uretero-ileal anastomosis by shortening the duration of stenting.
We did not experience any case of dislodgement of the external ureteric catheters, but this is a potential risk that requires trained nursing care and good patient education [15]. On the other hand, upward migration is a known complication of internal stenting, especially if the stent is too short or the collecting system is massively dilated [16]. We did not experience this as the JJ stents used were all 28 cm in length. Additionally, ureteroscopic removal of migrated stents might be challenging in this setting [17] and antegrade removal of the migrated stent may be required. In the present study, transurethral removal of the JJ stents was time consuming in three patients, as the reconstructed ON was folded up on itself, making the search for the stents difficult. In one of these patients, the stent on one side was removed via an antegrade approach under fluoroscopy guidance. In subsequent patients, the lower ends of the stents were sutured to the ON mucosa with an absorbable suture to facilitate visualisation during transurethral removal.
Another point related to the type of stenting is the rate of ON irrigation; where we observed it to be more frequently needed in Group A patients. With the use of external stents, the mucus secreted by the ON might accumulate in a relatively dry medium until the external stents are removed, thus requiring more irrigation in these patients [18]. In contrast, the use of JJ stents, allows a continuous flow of urine in the ON during the early postoperative period. A potential problem with internal stents is encrustation. This was not seen in our present series, which may be due to the short contact time with urine [19].
Our present results are consistent with the few studies that have compared internal and external stenting in the ON, especially for hospital stay and the rate of complications [9], [11]. Varkarakis et al. [9] retrospectively assessed the use of external stents (Group A) vs JJ stents (Group B) in patients undergoing RC with ‘S-pouch’ ileal neobladders. The ureters were implanted using a simple end-to-side intramural technique. The ureteric catheters and JJ stents were removed 15 days and 3 weeks postoperatively, respectively. Complication rates were similar in both groups, except for an increased urethro-neobladder anastomotic leakage rate (10% vs 15.3%) in the JJ-stent group, which was not statistically significant. Strictures of the uretero-ileal anastomosis occurred in 6.6% and 7.6% of patients in groups A and B, respectively. All strictures were treated with open re-implantation. Consistent with our present findings, hospital stay was significantly shorter with the use of JJ stenting (9.9 vs 15.2 days). However, the fewer patients with JJ stents (13 patients) compared with the other group with external stents (30) was a limitation of that study [9]. Another retrospective study was conducted by Micali et al. [11] of 77 patients. The uretero-ileal anastomosis was made using a direct spatulated end-to-side technique to the afferent loop of a Studer ON. In Group A (45 patients), the uretero-ileal anastomosis was stented using external stents, whilst in Group B (32) a JJ stent was used. The stricture rate was comparable between the two study groups. There were nine (11.5%) uretero-ileal anastomosis strictures in Group A, and seven (11.6%) in Group B. Neobladder catheters were removed after 17 days and 14 days in Group A and Group B, respectively. Group B patients had a significantly shorter hospital stay.
Uretero-ileal anastomotic strictures have been reported to be as high as 10% [14], [20], [21], [22], [23]. We had a relatively low rate of anastomotic strictures, which may be related to our ‘intermediate’ follow-up period. A longer period of follow-up is needed for more reliable conclusions. Hautmann et al. [24] also reported a 17% stricture rate in patients undergoing a modified Le Duc uretero-intestinal anti-reflux procedure compared with only 6.4% in those with an open refluxing anastomosis.
None of our present patients developed pyelonephritis after urethral catheter removal, which may be due to the antibiotic prophylaxis given to the patients at the time of catheter removal using fluoroquinolones and subsequent suppressive prophylaxis given indefinitely to all our ON patients using trimethoprim-sulphamethoxazole (TMP-SMX).
The present study is the first to prospectively compare the outcome (hospital stay, postoperative complication rate and intermediate follow-up) of external stenting vs JJ stenting of the uretero-intestinal anastomosis after LRC with ON. We believe that JJ stenting allows for the use of less urine collection bags and a shorter hospital stay, with no difference in complications. This helps to ‘fast-track’ the postoperative care in our particular group of patients. The main limitation of the present study is the deficient data regarding the assessment of the metabolic acidosis and the base excess, especially in the early postoperative period. It has been reported that externalisation of the ureteric stent will prevents reabsorption of urine by the reservoir in the postoperative period with a consequent significantly lower risk of metabolic acidosis and significantly faster recovery of bowel function [25], [26]. However, we did not find any significant difference between the two study groups regarding return of bowel activity. Another limiting factor is the follow-up period, where a longer follow-up could have provided more information on the incidence of delayed complications related to possible anastomotic stricture formation.
A bias in determining the nature of stenting is another limitation of the present study. However, there was no significant difference between both groups in the preoperative data in addition to the use of the same method for uretero-ileal anastomosis and ON in both groups. These points may ameliorate the effect of bias in the stenting method. Although four surgeons were involved in the present study, they were all of the same level of experience.
Our hospital is a university hospital where all services are free. Thus, it is difficult to perform a cost analysis for the procedure of JJ-stent removal. However, removal of a JJ stent is a simple procedure that can be performed under local anaesthesia on an outpatient basis without the need for hospital admission. Additionally, the cost of JJ-stent removal is < 6% of the cost of a RC. This percentage will be even lower when compared with the cost of a LRC. The reduction of the cost of 7 days of hospital stay that is achieved with a LRC, clearly justifies the cost of JJ-stent removal. Additionally, with the increasing use of robotics in RC, the overall costs of laparoscopy seem not to be that much different from open surgery.
Conclusion
JJ stenting of the uretero-ileal anastomosis is associated with a shorter hospital stay and similar complication rates in patients undergoing LRC and ON, when compared with external ureteric stenting.
Compliance with Ethical Standards:
-
-
This study was not funded by any grants or funds.
-
-
This article does not contain any studies with animals performed by any of the authors.
-
-
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
-
-
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
All the authors of the article declare no conflict of interest.
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Ghoneim M.A., Abdel-Latif M., El-Mekresh M., Abol-Enein H., Mosbah A., Ashamallah A. Radical cystectomy for carcinoma of the bladder: 2,720 consecutive cases 5 years later. J Urol. 2008;180:121–127. doi: 10.1016/j.juro.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 2.Lee R.K., Abol-Enein H., Artibani W., Bochner B., Dalbagni G., Daneshmand S. Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int. 2014;113:11–23. doi: 10.1111/bju.12121. [DOI] [PubMed] [Google Scholar]
- 3.El-Taji O.M., Khattak A.Q., Hussain S.A. Bladder reconstruction: the past, present and future. Oncol Lett. 2015;10:3–10. doi: 10.3892/ol.2015.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujisawa M., Isotani S., Gotoh A., Okada H., Arakawa S., Kaminodo S. Health related quality of life with orthotopic neobladder versus ileal conduit according to the SF-36 survey. Urology. 2000;55:862–865. doi: 10.1016/s0090-4295(00)00483-0. [DOI] [PubMed] [Google Scholar]
- 5.Hobisch A., Tosun K., Kinzl J., Kemmler G., Bartsch G., Höltl L. Quality of life after cystectomy and orthotopic neobladder versus ileal conduit urinary diversion. World J Urol. 2000;18:338–344. doi: 10.1007/s003450000147. [DOI] [PubMed] [Google Scholar]
- 6.Saika T., Arata R., Tsushima T., Nasu Y., Suyama B., Takeda K. Health-related quality of life after radical cystectomy for bladder cancer in elderly patients with an ileal conduit, ureterocutaneostomy, or orthotopic urinary reservoir: a comparative questionnaire survey. Acta Med Okayama. 2007;61:199–203. doi: 10.18926/AMO/48338. [DOI] [PubMed] [Google Scholar]
- 7.Finney R.P. Double-J and diversion stents. Urol Clin North Am. 1982;9:89–94. [PubMed] [Google Scholar]
- 8.Tal R., Bachar G.N., Baniel J., Belenky A. External-internal nephro-ureteroileal stents in patients with an ileal conduit: long-term results. Urology. 2004;63:438–441. doi: 10.1016/j.urology.2003.09.062. [DOI] [PubMed] [Google Scholar]
- 9.Varkarakis I.M., Delis A., Papatsoris A., Deliveliotis C. Use of external ureteral catheters and internal double J stents in a modified ileal neobladder for continent diversion: a comparative analysis: a comparative analysis. Urol Int. 2005;75:139–143. doi: 10.1159/000087168. [DOI] [PubMed] [Google Scholar]
- 10.Smith A.D. The universal ureteral stent. Urol Clin North Am. 1982;9:103–340. [PubMed] [Google Scholar]
- 11.Micali S., De Carli P., Miano R., O’Sullivan D., Lamanna L., Micali F. Double-J ureteral stents: an alternative to external urinary stents in orthotopic bladder substitution. Eur Urol. 2001;39:575–579. doi: 10.1159/000052506. [DOI] [PubMed] [Google Scholar]
- 12.Shah S.H., Movassaghi K., Skinner D., Dalag L., Miranda G., Cai J. Ureteroenteric strictures after open radical cystectomy and urinary diversion: The University of Southern California Experience. Urology. 2015;86:87–91. doi: 10.1016/j.urology.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Abdel-Hakim A., Bassiouny F., Abdel Azim M.S., Rady I., Mohey T., Habib I. Laparoscopic radical cystectomy with orthotopic neobladder. J Endourol. 2002;16:377–381. doi: 10.1089/089277902760261428. [DOI] [PubMed] [Google Scholar]
- 14.Neuzillet Y., Yonneau L., Lebret T., Herve J.M., Butreau M., Botto H. The Z-shaped ileal neobladder after radical cystectomy: an 18-year experience with 329 patients. BJU Int. 2011;108:596–602. doi: 10.1111/j.1464-410X.2010.10000.x. [DOI] [PubMed] [Google Scholar]
- 15.Herdiman O., Ong K., Johnson L., Lawrentschuk N. Orthotopic bladder substitution (Neobladder): part II: postoperative complications, management, and long-term follow-up. J Wound Ostomy Continence Nurs. 2013;40:171–180. doi: 10.1097/WON.0b013e31827e8499. [DOI] [PubMed] [Google Scholar]
- 16.Ahallal Y., Khallouk A., El Fassi M.J., Farih M.H. Risk factor analysis and management of ureteral double-j stent complications. Rev Urol. 2010;12:e147–e151. [PMC free article] [PubMed] [Google Scholar]
- 17.Abdel-Hakim A.M., El-Feel A.S., Abdel-Hakim M.A. Difficulties in laparoscopic radical cystectomy. In: Al-Kandari A., Gill I., editors. Difficult conditions in laparoscopic urologic surgery. Springer; London, UK: 2011. pp. 285–294. [Google Scholar]
- 18.Ong K., Herdiman O., Johnson L., Lawrentschuk N. Orthotopic bladder substitution (neobladder): part I: indications, patient selection, preoperative education, and counseling. J Wound Ostomy Continence Nurs. 2013;40:73–82. doi: 10.1097/WON.0b013e31827759ea. [DOI] [PubMed] [Google Scholar]
- 19.Rana A.M., Sabooh A. Management strategies and results for severely encrusted retained ureteral stents. J Endourol. 2007;21:628–632. doi: 10.1089/end.2006.0250. [DOI] [PubMed] [Google Scholar]
- 20.Schöndorf D., Meierhans-Ruf S., Kiss B., Giannarini G., Thalmann G.N., Studer U.E. Ureteroileal strictures after urinary diversion with an ileal segment-is there a place for endourological treatment at all? J Urol. 2013;190:585–590. doi: 10.1016/j.juro.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 21.Stenzl A., Sherif H., Kuczyk M. Radical cystectomy with orthotopic neobladder for invasive bladder cancer: a critical analysis of long term oncological, functional and quality of life results. Int Braz J Urol. 2010;36:537–547. doi: 10.1590/s1677-55382010000500003. [DOI] [PubMed] [Google Scholar]
- 22.Ballouhey Q., Thoulouzan M., Lunardi P., Bellec L., Huyghe E., Plante P. Prospective study of the results of ureterointestinal anastomosis in 100 patients after the Hautmann ileal neobladder with double chimney. Prog Urol. 2012;22:255–260. doi: 10.1016/j.purol.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Nassar O.A., Alsafa M.E. Experience with ureteroenteric strictures after radical cystectomy and diversion: open surgical revision. Urology. 2011;78:459–465. doi: 10.1016/j.urology.2011.01.040. [DOI] [PubMed] [Google Scholar]
- 24.Hautmann R.E., de Petriconi R.C., Volkmer B.G. 25 years of experience with 1000 neobladders: long-term complications. J Urol. 2011;185:2207–2212. doi: 10.1016/j.juro.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 25.Varol C., Studer U.E. Managing patients after an ileal orthotopic bladder substitution. BJU Int. 2004;93:266–270. doi: 10.1111/j.1464-410x.2004.04599.x. [DOI] [PubMed] [Google Scholar]
- 26.Mattei A., Birkhaeuser F.D., Baermann C., Warncke S.H., Studer U.E. To stent or not to stent perioperatively the ureteroileal anastomosis of ileal orthotopic bladder substitutes and ileal conduits? Results of a prospective randomized trial. J Urol. 2008;179:582–586. doi: 10.1016/j.juro.2007.09.066. [DOI] [PubMed] [Google Scholar]