Highlights
-
•
Mesenteric Meckel’s diverticulum and intestinal duplication cyst both are congenital anomaly of the gastrointestinal tract.
-
•
Preoperative diagnosis is very hard to establish even after Surgery.
-
•
Ectopic gastric or pancreatic mucosa can be found in both these pathologies.
-
•
Surgical treatment is gold standard of both because of their complictions.
Abbreviations: MD, Meckel’s diverticulum; GI, gastrointestinal; IDC, intestinal duplication cyst; CT, computed tomography
Keywords: Meckel’s diverticulum, Intestinal duplication cyst, Gastric mucosa, Case report
Abstract
Introduction
A Meckel’s diverticulum (MD) is the most common congenital anomaly of the gastrointestinal (GI) tract. They arise from the middle-to-distal ileum. Contrary to MD, intestinal duplication cyst (IDC) is uncommon congenital anomaly of GI, but can occur anywhere from the tongue to the anus.
Presentation of case
Here we report an 18-year-old male who presented to the department of abdominal surgery with chronic abdominal pain, frequent vomiting and mild abdominal distension. Following radiological investigation, a laparotomy was performed with the preoperative diagnosis of a mesenteric cyst. Intraoperativelly it became apparent that the cystic mass was on the mesenteric aspect of the small bowel without intestinal communication. Resection of the cyst was performed. Histological examination of the specimen revealed the presence of gastric tissue, which resembles MD. Although, the exact diagnosis of this cystic mass is ambiguous between MD and IDC, because of similar clinical signs, their complications and presence of gastric mucosa, however surgical treatment is gold standard of both.
Conclusion
This case report underlines the necessity of how to differentiate between MD and IDC, although, surgical management is recommended for both.
1. Introduction
Meckel’s diverticulum (MD) is the most common congenital anomaly of the gastrointestinal (GI) tract. It results from incomplete obliteration of the vitelline duct leading to the formation of a true diverticulum of the small intestine [1]. MD is a true diverticulum as it contains all layers of the small bowel wall. It can occur in up to 2% of the population and can manifest as obscure GI bleeding, Meckel’s diverticulitis, obstruction, and intussusceptions [2]. Contrary to MD, intestinal duplication cyst (IDC) is uncommon congenital anomaly that can occur anywhere from the tongue to the anus [3]. Most of these cysts occur in the small bowel and about half are in the mesenteric border of the ileum [3], [4]. IDC communicates only rarely with the intestinal lumen, although the cysts are attached to the intestine and may even share a common wall with the adjacent alimentary tract [4], [5], [6]. In general, MD arises from the antimesenteric border of the middle-to-distal ileum. However, there are very few published cases of mesenteric-sided MD and several authors have suggested that what some call a mesenteric-sided MD may in fact be an IDC [7], [8], [9], [10], [11], [12]. We report a case of IDC without intestinal communication, but histopathological analysis has shown a gastric mucosa that resembles MD.
2. Presentation of case
A previously fit and healthy 18 year old man presented to the department of gastroenterology, with a two year history of chronic abdominal pain, frequent vomiting and mild abdominal distension. On examination the abdomen was soft, non-tender, bowel sounds were present and on digital rectal examination there was only soft stool. There was no history of trauma to the abdomen. All blood results were within normal range. Abdominal ultrasound showed a cystic mass measuring 9.0 × 8.0 cm in the right lower quadrant of the abdomen.
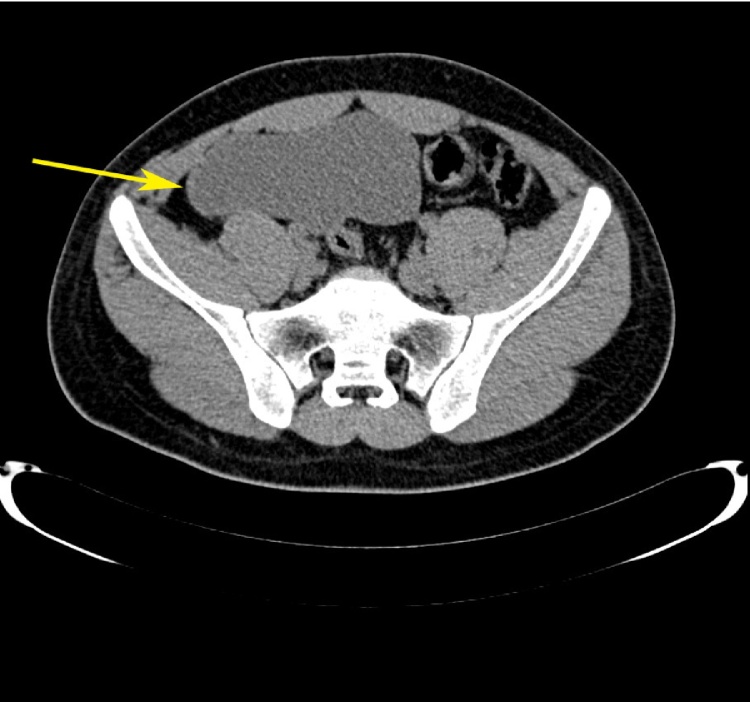
A contrast-enhanced abdominal computed tomography (CT) scan revealed a well-circumscribed peritoneal hypodense cystic mass measuring 120 × 69 × 58 mm, located in the right lower quadrant of the abdomen (Fig. 1). The patient was transferred to the department of abdominal surgery for surgical treatment.
Fig. 1.
Computed tomography (CT) revealed a well-circumscribed cystic mass located in the right lower quadrant of the abdomen (arrow).
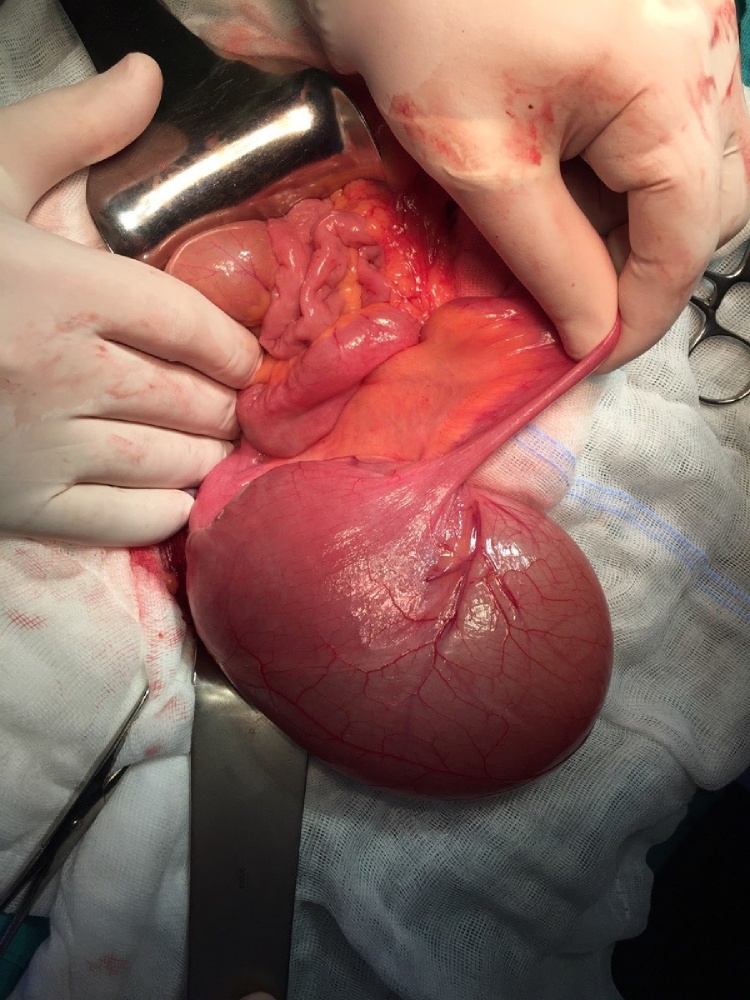
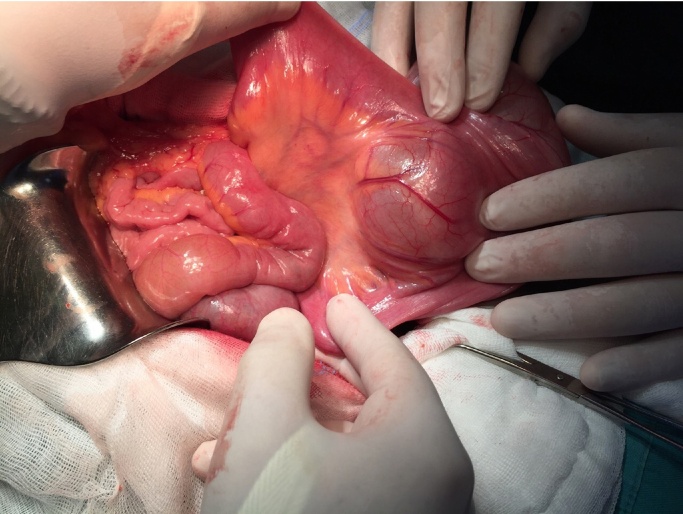
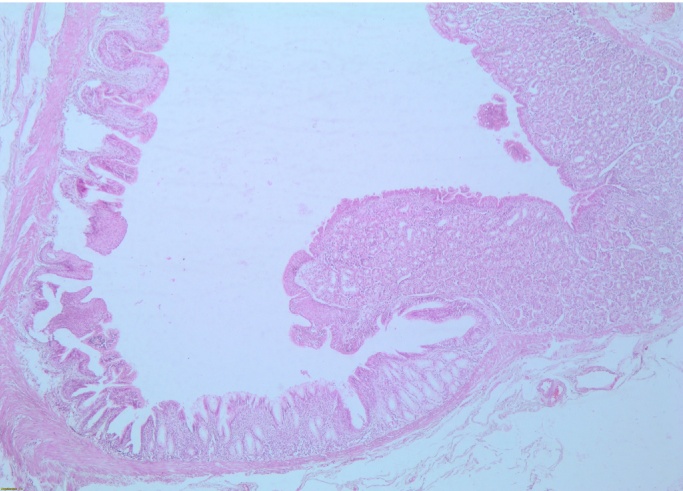
Laparotomy was performed with the preoperative diagnosis of a mesenteric cyst. At laparotomy, a large cystic mass was found in the terminal ileal mesentery (Fig. 2). The mass was attached to the intestine and shared a common wall with the adjacent alimentary tract. Incising into the cyst, clear fluid gushed out. However the cyst had no distinct communicating path with intestinal tract. The mass was excised free of surrounding soft tissue without iatrogenic injury to the surrounding intestinal and mesenteric structures. The mass had a dedicated vascular pedicle, which was ligated and removed (Fig. 3). The specimen was sent for histopathological examination. Biopsy of the cystic mass revealed ectopic gastric tissue, which resembles MD (Fig. 4, Fig. 5). The postoperative course was uneventful and the patient was discharged from hospital without any complications. This manuscript is written in accordance with the CARE (CAse Report) guidelines [13].
Fig. 2.
A cystic mass located on the mesentery of the terminal ileum attached to the intestine and shared a common wall with the adjacent alimentary tract.
Fig. 3.
Vascular pedicle of the cystic mass, which was simply ligated and removed.
Fig. 4.
Macroscopically view of cystic mass after fixation with 4% formaldehyde solution.
Fig. 5.
Histological picture showing the luminal lining of the cyst. Ectopic corpus-type gastric mucosa in the right-hand side transitioning to columnar, stratified and squamous epithelium in the left-hand side of the picture (Hematoxylinc & Eosin stain, 4 × magnification).
3. Discussion
Classical feature of MD is its location on the anti-mesenteric border of the intestine, whereas mesenteric location is very rare and only few cases have been published [8], [9], [10], [11], [12]. There are several characteristics unique to MD that aid its identification which include: location two feet proximal to the ileocecal valve, the presence of an independent vessel supplying the structure involving all the five layers of small intestine, and majority of specimens have ectopic mucosa of either gastric, pancreatic or another origin other than small intestine [7]. Regarding IDC, in general ileal duplication cysts makeup about 44% of GI tract duplications and the wall of small bowel duplication cysts can contain two-mucosal layers sharing a common muscle layer [14], [15]. Our case is an obvious example of a cystic mass in the mesenteric side of the small bowel that required cystic resection because of its clinical presentation. However, the exact diagnosis of this mass is rather ambiguous. Histological analysis revealed gastric mucosa, which resembles MD but there was no communication between cystic mass and intestine. The absence of a distinct communication of a cystic mass with adjacent intestinal lumen favors IDC. Another possible area of distinction is with ectopic gastric mucosa, which our patient had. Nevertheless, ectopic gastric or pancreatic mucosa can be found in both MD (approximately 55%) and IDC (approximately 16–39%) [2], [10]. On the other hand, theoretically we can speculate that this mass may have communicated with the lumen of adjacent bowel, but may have subsequently obliterated as a result of the cystic development process. Another definitive evidence of MD is the presence of a vitelline artery or a clear independent blood supply to a diverticulum; whereas, intestinal duplications shares the blood supply with the surrounding intestine [10]. In our case, the cystic mass had a distinct blood supply, which was identified intraoperatively. Finally, we could say that due to similar clinical presentations of MD and IDC, and their complications, often it is difficult to differentiate between them even after surgery and histopathological analysis. Although, surgical resection is mandatory of both. In addition, 23% of intestinal duplication cysts in adults were found to be ileal cancer [16].
4. Conclusion
In conclusion, this case report underlines the necessity of how to differentiate between MD and IDC however, surgical management is recommended for both symptomatic and asymptomatic patients because of potential serious complications that include; gastrointestinal bleeding, Meckel’s diverticulitis, obstruction, intussusceptions and malignancy for both these pathologies.
Competing interest
The authors have no conflicts of interests.
Source of funding
This case report is realized without any funding.
Ethical approval
There was no ethics approval required for this case report.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
AH, AK, BB and FS participated in the surgery and anesthesiology of this case. FK performed histopathological analysis. AH, AK and VZ treated the patient after surgery. AH drafted the manuscript and all authors read and approved the final manuscript.
Guarantor
Avdyl S. Krasniqi.
Acknowledgment
The authors thank Arben Imeri for his skillful technical assistance on figures preparation.
References
- 1.Sagar J., Kumar V., Shah D.K. Meckel’s diverticulum: a systematic review. J. R. Soc. Med. 2006;99(10):501–505. doi: 10.1258/jrsm.99.10.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uppal K., Tubbs R.S., Matusz P., Shaffer K., Loukas M. Meckel’s diverticulum: a review. Clin. Anat. 2011;24(4):416–422. doi: 10.1002/ca.21094. [DOI] [PubMed] [Google Scholar]
- 3.Gumus M., Kapan M., Gumus H., Onder A., Girgin S. Unusual noncommunicating isolated enteric duplication cyst in adults. Gastroenterol. Res. Pract. 2011;2011:323919. doi: 10.1155/2011/323919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J.Y., Her K.H., Kim B.S., Maeng Y.H. A completely isolated intestinal duplication cyst mimicking ovarian cyst torsion in an adult. World J. Gastroenterol. 2014;20(2):603–606. doi: 10.3748/wjg.v20.i2.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinha A., Ojha S., Sarin Y.K. Completely isolated, noncontiguous duplication cyst. Eur. J. Pediatr. Surg. 2006;16(2):127–129. doi: 10.1055/s-2006-924004. [DOI] [PubMed] [Google Scholar]
- 6.Macpherson R.I. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13(5):1063–1080. doi: 10.1148/radiographics.13.5.8210590. [DOI] [PubMed] [Google Scholar]
- 7.Walczak D.A., Falek W., Zakrzewski J. An uncommon location of Meckel’s diverticulum or small intestine duplication? Case report and literature review. Polski Przeglad Chirurgiczny. 2011;83(8):457–460. doi: 10.2478/v10035-011-0071-z. [DOI] [PubMed] [Google Scholar]
- 8.Sarioglu-Buke A., Corduk N., Koltuksuz U., Karabul M., Savran B., Bagci S. An uncommon variant of Meckel’s diverticulum. Can. J. Surg. 2008;51(2):E46–47. [PMC free article] [PubMed] [Google Scholar]
- 9.Seitun S., Vito L.D., Rossi U.G., Panetta M., Cabiddu F., Tedeschi U., Viotti A. Perforated Meckel’s diverticulitis on the mesenteric side: MDCT findings. Abdom. Imaging. 2012;37(2):288–291. doi: 10.1007/s00261-011-9733-x. [DOI] [PubMed] [Google Scholar]
- 10.Segal S.D., Albrecht D.S., Belland K.M., Elster E.A. Rare mesenteric location of Meckel’s diverticulum, a forgotten entity: a case study aboard USS Kitty Hawk. Am. Surg. 2004;70(11):985–988. [PubMed] [Google Scholar]
- 11.Kurzbart E., Zeitlin M., Feigenbaum D., Zaritzky A., Cohen Z., Mares A.J. Rare spontaneous regression of patent omphalomesenteric duct after birth. Arch. Dis. Child. Fetal Neonatal Ed. 2002;86(1):F63. doi: 10.1136/fn.86.1.F63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manukyan M.N., Kebudi A., Midi A. Mesenteric Meckel’s diverticulum: a case report. Acta Chir. Belg. 2009;109(4):510–512. doi: 10.1080/00015458.2009.11680472. [DOI] [PubMed] [Google Scholar]
- 13.Gagnier J.J., Kienle G., Altman D.G., Moher D., Sox H., Riley D., Group C. The CARE guidelines: consensus-based clinical case report guideline development. J. Clin. Epidemiol. 2014;67(1):46–51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Al-Sarem S.A., Al-Shawi J.S. Ileal duplication in adults. Saudi Med. J. 2007;28(11):1734–1736. [PubMed] [Google Scholar]
- 15.Ko S.Y., Ko S.H., Ha S., Kim M.S., Shin H.M., Baeg M.K. A case of a duodenal duplication cyst presenting as melena. World J. Gastroenterol. 2013;19(38):6490–6493. doi: 10.3748/wjg.v19.i38.6490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim Y.S., Kim D.J., Bang S.U., Park J.J. Intestinal duplication cyst misdiagnosed as Meckel’s diverticulum. Chin. Med. J. (Engl.) 2016;129(2):235–236. doi: 10.4103/0366-6999.173544. [DOI] [PMC free article] [PubMed] [Google Scholar]