Abstract
Purpose
To describe the epidemiology of thoracolumbar fractures and associated injuries in blunt trauma patients.
Methods
A systematic review and metaanalysis was performed based on a MEDLINE database search using MeSH terms for studies matching our inclusion criteria. The search yielded 21 full-length articles, each sub-grouped according to content. Data extraction and multiple analyses were performed on descriptive data.
Results
The rate of thoracolumbar fracture in blunt trauma patients was 6.90% (±3.77, 95% CI). The rate of spinal cord injury was 26.56% (±10.70), and non-contiguous cervical spine fracture occurred in 10.49% (±4.17). Associated injury was as follows: abdominal trauma 7.63% (±9.74), thoracic trauma 22.64% (±13.94), pelvic trauma 9.39% (±6.45), extremity trauma 18.26% (±5.95), and head trauma 12.96% (±2.01). Studies that included cervical spine fracture with thoracolumbar fracture had the following rates of associated trauma: 3.78% (±5.94) abdominal trauma, 21.65% (±16.79) thoracic trauma, 3.62% (±1.07) pelvic trauma, 18.36% (±4.94) extremity trauma, and 15.45% (±11.70) head trauma. A subgroup of flexion distraction injuries showed an associated intra-abdominal injury rate of 38.70% (±13.30). The most common vertebra injured was L1 at a rate of 34.40% (±15.90). T7 was the most common non-junctional vertebra injured at 3.90% (±1.09). Burst/AO type A3 fractures were the most common morphology 39.50% (±16.30) followed by 33.60% (±15.10) compression/AO type A1, 14.20% (±8.08) fracture dislocation/AO type C, and 6.96% (±3.50) flexion distraction/AO type B. The most common etiology for a thoracolumbar fracture was motor vehicle collision 36.70% (±5.35), followed by high-energy fall 31.70% (±6.70).
Conclusions
Here we report the incidence of thoracolumbar fracture in blunt trauma and the spectrum of associated injuries. To our knowledge, this paper provides the first epidemiological road map for blunt trauma thoracolumbar injuries.
Keywords: Thoracolumbar, Trauma, Epidemiology, Spine, Spinal cord injury, Abdominal injury, Thoracic injury, Fracture, Meta-analysis, Cervical spine, Blunt trauma
1. Introduction
Blunt trauma is a leading cause of death in industrialized nations.1 Although fractures of the spine occur only in small proportion of blunt trauma patients, they often have serious consequences on the medical, social and financial status of the patient.1, 2 While the overall prevalence and causation of spinal injuries varies according to region and level of urbanization, the Unites States has the highest prevalence of spinal injury globally.3 Composite epidemiological data is needed to guide emergency management, treatment, and policy development regarding spinal trauma. Currently no such comprehensive guide exists. The purpose of this study was to conduct a systematic review of the literature regarding the epidemiology of thoracolumbar trauma and to perform a meta-analysis on available data. The goals were to summarize the rate of thoracolumbar trauma in blunt trauma patients and to compile the rates of etiology, location, fracture type, and associated injuries into a single source for treating physicians. This will allow quick reference to epidemiological rates of thoracolumbar trauma and associated injuries.
2. Materials and methods
2.1. Inclusion and exclusion criteria
We used the Cochrane collaboration guidelines4 to help develop our methods and reported our results according to the PRISMA checklist.5
Inclusion criteria: English language articles published from 1980 onward were evaluated for inclusion. The study had to contain patients who sustained a spinal fracture as a result of blunt trauma (specifically the T1-L5 thoracolumbar region or C1-L5 global spine).
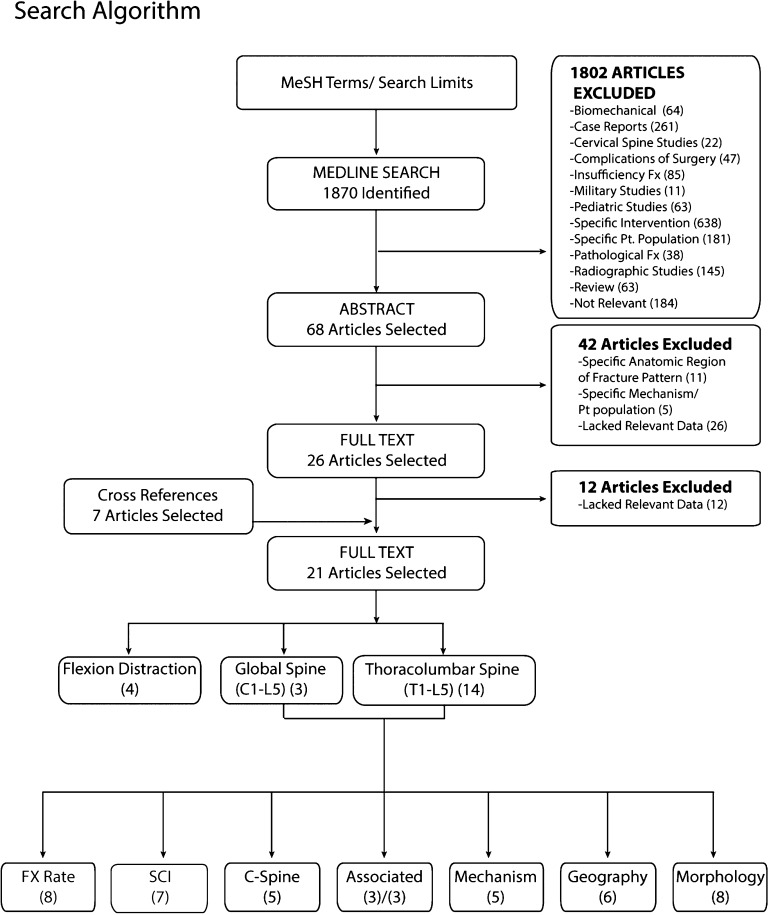
Exclusion criteria: Studies were excluded if the primary focus was: biomechanical, a case report of an individual or several incidents, the cervical spine, complications of surgery, osteoporotic or insufficiency fractures, a military based population, a pediatric population, specific interventions or treatments, other specific patient populations such as diabetics or ankylosing spondylitis patients, pathological fractures, radiographic parameter studies not containing epidemiological data, review articles, or papers not relevant to thoracolumbar trauma (Fig. 1). Elderly and pediatric patients were not specifically excluded from this paper; merely studies which were focused only on osteoporotic fractures in the elderly or only evaluated a pediatric population.
Fig. 1.
Search algorithm used to select articles for analysis. Search terms initially yielded 1870 articles, 68 of which were selected for analysis of abstract based on inclusion and exclusion criteria. Another 42 articles were removed because they were too specific in their focus or lacked relevant data. This yielded 26 articles for full text analysis. Another 7 articles were included from manual cross-referencing. From these, 12 articles lacked relevant epidemiological data and were excluded to leave 21 relevant articles that were eventually selected for analysis of the full text. Some articles were utilized twice for different analyses. Abbreviations: Fx: fracture, SCI: spinal cord injury.
2.2. Literature search and study selection
In November 2014 a comprehensive literature search was performed through the electronic database of MEDLINE (1980–2014) using medical subject headings (MeSH) terms and Boolean operators outlined in Table 1. Search limits were: (1) study date 1980–2014, (2) human species, (3) abstracts were available, (4) study was reported in English. Studies were assessed initially based on title by 3 independent reviewers. From the yield of this search, two reviewers analyzed abstracts to determine which papers to investigate and include for paper review based on title, abstract, and keywords of the references retrieved from the electronic literature search. To further ensure that no appropriate studies were missed a manual cross-reference search of citations of each included article was performed. The two independent reviewers then evaluated the eligibility of each article. All disagreements were discussed in a consensus meeting. A third party reviewer resolved disagreements, which were not resolved by the consensus meeting. If relevant epidemiological data could not be extracted from the selected full text or abstract it excluded from this review.
Table 1.
MeSH Terms and Boolean operators used for literature search.
| • Lumbar Vertebrae/radiography[MeSH Terms] |
| • OR |
| • Thoracic Vertebrae/radiography[MeSH Terms] |
| • OR |
| • Thoracic Vertebrae/injuries*[MeSH Terms] |
| • OR |
| • Lumbar Vertebrae/injuries*[MeSH Terms] |
| • OR |
| • Thoracolumbar*[MeSH Terms] |
| • AND |
| • Spinal Fractures/therapy[MeSH Terms] |
| • OR |
| • Spinal Fractures/complications[MeSH Terms] |
| • OR |
| • Spinal Fractures/epidemiology*[MeSH Terms] |
| • OR |
| • Spinal Fractures/diagnosis*[MeSH Terms] |
| • OR |
| • Spinal Fractures/surgery[MeSH Terms] |
| • OR |
| • Spinal Injuries/radiography[MeSH Terms] |
| • NOT |
| • Osteoporosis[MeSH Terms] |
| • OR |
| • Age related osteoporosis [MeSH Terms] |
2.3. Search results
A flow chart of the search algorithm used is shown in Fig. 1. From our primary search 1870 articles were identified. 1802 articles were excluded based on inclusion and exclusion criteria listed above yielding 68 articles. The abstracts of these articles were evaluated for data of interest. Based on this review another 42 studies were excluded because their focus was too specific (i.e. only concerning the lumbar spine or only blunt trauma victims from motor vehicle collisions). This left 26 articles, to which another 7 were added from references and were scrutinized for relevant data. 12 further articles were excluded because of lack of reporting of relevant or useful data. Table 2 shows the included studies with a summary of demographics and their contributions to the data pool.
Table 2.
List of included studies.
| First authors | Journal | Category | Location of study | Design of study | Period of study | Patients |
|---|---|---|---|---|---|---|
| Nelson (2012) | J Trauma Acute Care Surg | Global spine C1-L5 | National Trauma Data bank (NTDB) | Retrospective series | 2010 | 654,052 |
| Leucht (2009) | Injury | Global spine C1-L5 | Ruhr University Bochum, Bochum, Germany | Retrospective series | 1996–2000 | 562 |
| Wang (2012) | J Neurosurg Spine | Global spine C1-L5 | Third Military Medical University, Chongqing, China | Retrospective series | 2001–2010 | 3142 |
| Samuels (1993) | J Trauma | Thoracolumbar spine T1-L5 | Hanemann University Hospital, Phildelphia, PA | Retrospective series | 1989–1990 | 99 |
| Frankel (1994) | J Trauma | Thoracolumbar spine T1-L5 | Multicenter | Retrospective/prospective series | 1992–1993 | 1965 |
| Cooper (1995) | J Trauma | Thoracolumbar spine T1-L5 | Shock Trauma Center, Baltimore, Maryland | Retrospective series | Not reported | 4142 |
| Holmes (2001) | Acad Emerg Med | Thoracolumbar spine T1-L5 | UCD Sacramento Medical Center, Sarcamento, CA | Prospective observational | 1997–1998 | 2404 |
| Hsu (2002) | Injury | Thoracolumbar spine T1-L5 | Royal North Shore Hospital, St Leonards, Australia | Retrospective series | 1998–2000 | 100/29 |
| Inaba (2011) | J trauma | Thoracolumbar spine T1-L5 | Los Angeles County Hospital and University of Southern California Medical Center, CA | Prospective observational | 2008–2008 | 884 |
| Joaquim (2013) | Spine J | Thoracolumbar spine T1-L5 | University of Utah Health Sciences Center, Salt Lake City, Utah | Retrospective series, prospectively gathered data base | 2000–2010 | 20,292 |
| Gertzbein (1991) | Spine | Thoracolumbar spine T1-L5 | Multicenter | Prospective multicenter | 1986–1988 | 1019 |
| Magerl (1994) | Eur Spine J | Thoracolumbar spine T1-L5 | Multicenter | Retrospective series | Not reported | 1445 |
| Meldon (1995) | J Trauma | Thoracolumbar spine T1-L5 | Metrohealth Medical Center, Cleveland OH | Retrospective series | 1989–1992 | 145 |
| Terregino (1995) | Ann Emerg Med | Thoracolumbar spine T1-L5 | Southern New Jersey Regional Trauma Center | Retrospective series, prospectively gathered data base | 1993 | 319 |
| Saboe (1991) | J Trauma | Thoracolumbar spine T1-L5 | University of Alberta Hospitals, Alberta, Canada | Prospective longitudinal | 1983–1988 | 183 |
| Denis (1983) | Spine | Thoracolumbar spine T1-L5 | St Paul-Ramsey Medical Center, St. Paul, MN and Ottowa Civic Hospital, Ottowa, Canada | Retrospective series | Not Available | 412 |
| Dai (2004) | J Trauma | Thoracolumbar spine T1-L5 | Xinhua Hospital, Shanghai Second Medical University, Shanghai, China. | Retrospective series | 1988–1997 | 147 |
| Chapman (2008) | Spine | Thoracolumbar flexion distraction | Harborview Medical Center, Seattle, WA | Retrospective series, prospectively gathered data base | 1989–2003 | 153 |
| Anderson (1991) | J Orthop Trauma | Thoracolumbar flexion distraction | Harborview Medical Center, Seattle, WA | Retrospective series | 1954–1988 | 20 |
| Tyroch (2005) | Am Surg | Thoracolumbar flexion distraction | Multicenter | Retrospective series | 1996–2001 | 55,000 |
| LeGay (1990) | J Trauma | Thoracolumbar flexion distraction | Unknown | Retrospective series | 1983–1990 | 18 |
Overall there were three main study categories of interest. First were articles pertaining to patients who suffered a thoracolumbar fracture (T1-L5). The second were studies, which included patients that had suffered a fracture anywhere in the spinal column (C1-L5). The last group of interest was studies devoted only to patients, which had suffered a flexion distraction injury to the thoracolumbar spine (T1-L5).
2.4. Data extraction
Data was extracted in duplicate to avoid anthropic mistakes. Data extracted included publication information, hospital location and trauma level, patient demographics, number of blunt trauma patients, number of patients with a thoracolumbar fracture, geographic location of fractures, morphology of fractures, presence of neurologic injury, non contiguous cervical spine injury, associated injuries (thoracic, abdominal, head, extremity, and pelvic) and mechanism of injury.
Fracture morphology was classified using either the Denis or AO classification systems with the following conversions compression fractures (Denis A or AO type A), burst fractures (Denis anterior and middle or AO type A3), flexion distraction fractures (Denis middle and posterior or AO type B), fracture dislocation (Denis anterior, middle and posterior or AO type C).
Spinal cord injury was classified as either present (ASIA type A–D or Frankel type A–D) or absent.
Associated injuries were classified as abdominal, extremity injury, head injury, pelvic injury or thoracic injury.
Mechanisms of injury were classified as motor vehicle collision (MVC), motorcycle collision (MCC or ATV related accident), fall (fall from height greater than 2 m), pedestrian struck, or other (sports related, industrial, cyclist).
2.5. Statistical analysis
The presence of heterogeneity was tested using the I2 statistic with an I2 statistic of 25% low heterogeneity 50% moderate heterogeneity and 75% high heterogeneity.6 A random effects model was used to synthesize rates for all analyses except those containing less than 3 studies for which a fixed-effects method was used. The mean rate was calculated for all categories. The meta analysis was carried out using Excel software (Microsoft, V12.3.6).7
3. Results
3.1. Rate of thoracolumbar fracture in all-comers blunt trauma
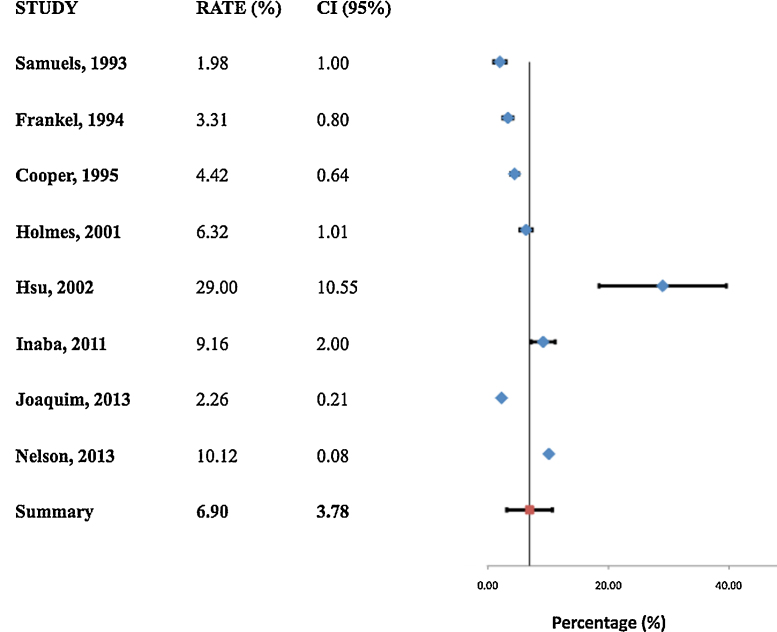
A total of 8 studies8, 9, 10, 11, 12, 13, 14, 15 (684,595 patients) were included in this meta-analysis visible. The heterogeneity was measured as I2 = 0 indicating low heterogeneity. The rate of thoracolumbar fracture in blunt trauma patients was found to be 6.9% (95% CI 3.2%, 10.6%) (Fig. 2). One study from the global spine group of articles was included as data compatible with the thoracolumbar data could be extracted.15
Fig. 2.
Random effects model of the rate of thoracolumbar fractures in blunt trauma patients. Summary effect highlighted in red, individual studies in blue.
3.2. Spinal cord injury in thoracolumbar trauma
7 studies10, 12, 14, 16, 17, 18 were included (3146 patients) for analysis of the rate of neurologic spinal cord injury in thoracolumbar fracture patients. One study12 which contained a poly trauma group and a specifically thoracolumbar trauma group was broken down and compiled as two separate studies. The heterogeneity was measures as I2 = 0 indicating low heterogeneity. The rate of spinal cord injury was 26.5% (95% CI 15.8%, 37.2%) in patients who had sustained a thoracolumbar fracture.
3.3. Concomitant non-contiguous cervical spine fractures in thoracolumbar trauma
Five studies9, 10, 12, 18, 19 were included (531 patients) for the analysis of the rate of non-contiguous cervical spine fractures in patients who had thoracolumbar spine fractures. The heterogeneity was measured as I2 = 44 indicating moderate heterogeneity. The rate of non-contiguous cervical spine fracture 10.49% (95% CI 6.29%, 14.7%).
3.4. Associated injury in thoracolumbar trauma
Six studies8, 15, 20, 21, 22, 23 total were included for the analysis of associated injuries in thoracolumbar trauma patients. 3 studies were of patients who only had fractures of the thoracolumbar region (381 patients) and another 3 included patients with fractures from C1-L5 (87,042 patients).
The rate of associated injury was 12.96% (95% CI 10.9%, 14.9%) for head trauma, 18.26% (95% CI 12.31%, 24.21%) for extremity trauma, 9.39% (95% CI 2.94% 15.84%) for pelvic trauma, 22.64% (95% CI 8.74%, 36.54%) for thoracic trauma, and 7.62% (95% CI 0, 17.36%) for abdominal trauma. This was contrasted with papers which included cervical spine fracture with thoracolumbar fracture and had the following rates of associated trauma: 15.4% (95% CI 3.7%, 27.1%) for head trauma, 18.36% (95% CI 13.43%, 23.29%) for extremity trauma, 3.38% (95% CI 2.79%, 3.97%) for pelvic trauma, 21.64% (95% CI 4.84%, 38.44%) for thoracic trauma, and 3.78% (±5.94, 95% CI 0, 9.72%) for abdominal trauma.
3.5. Intraabdominal injury associated with flexion distraction injuries
Four studies24, 25, 26, 27 total were included (270 patients) to analyze the rate of intraabdominal injury in patients with flexion distraction injuries. The heterogeneity was measured as I2 = 54 indicating moderate heterogeneity. This subgroup of flexion distraction injuries showed an associated intra-abdominal injury rate of 38.7% (95% CI 25.4%, 52%).
3.6. Specific vertebral involvement in thoracolumbar trauma
Five studies8, 11, 17, 22, 28 were included for this analysis. The most common vertebra injured was L1 at a rate of 34.4% (95% CI 18.2%, 50.3%). T7 was the most common non-junctional vertebra injured at 3.9% (95% CI 2.81%, 4.99%). T2 was the least injured vertebrae at 0.26% (95% CI 0, 0.56%).
3.7. Fracture morphology in thoracolumbar trauma
Six studies9, 14, 16, 17, 28, 29 were included (3546 patients) in this analysis. The heterogeneity was measured as follows: I2 statistic: 98 (A), 98 (A3), 92 (B), 97 (C). The rates of fracture morphology were 39.5% (95% CI 23.2%, 55.8%) burst/AO type A3, 33.6% (95% CI 18.5%, 48.7%) compression/AO type A1, 14.2% (±8.08, 95% CI 6.12%, 22.28%) fracture dislocation/AO type C, and 6.96% (95% CI 3.46%, 10.46%) flexion distraction (AO type B).
3.8. Mechanisms of injury resulting in thoracolumbar trauma
Nine studies8, 11, 12, 13, 16, 18, 19, 21 were included in the analysis of the rates of different mechanisms of injury which resulted in thoracolumbar fracture. One study9 which contained a poly trauma group and a specifically thoracolumbar trauma group was broken down and compiled as two separate studies. Heterogeneity was measured as follows: I2 statistic = 47% (MVC), 65% (MCC), 70% (Pedestrian), 72% (Falls), 63% (other). The most common etiology for a thoracolumbar fracture was motor vehicle collision 36.7% (95% CI 31.35%, 42.0%) followed by high-energy fall 31.7% (95% CI 25%, 38.4%). Motor cycle collision accounted for 10.05%, other for 9.06%, and pedestrian struck for 4.83%.
4. Discussion
More than 160,000 spinal injuries occur per year in North America and have high rates of morbidity and mortality.30 Spinal fractures are usually the result of high-energy trauma, which tend to leave patients with a constellation of injuries. A thorough understanding of the epidemiology and associated injury patterns of thoracolumbar spine injuries helps guide the evaluation and management of blunt trauma patients both in the emergency and operating rooms. To the best of our knowledge this is the first meta-analysis of the epidemiology of thoracolumbar fractures that attempts to summarize the spectrum of pathology resulting from blunt trauma.
Since 1990 there has been a decrease in the rate of MVC related injuries owning to increased rates of seatbelt use, behavior modification, improved safety design of cars.31 Despite this there have been reports of increasing rates of spinal trauma from MVC accidents.32 Indeed, Doud et al. showed increases in the rate of thoracolumbar injury incidence across the nation from 1998 to 2011.33 The improved automotive safety measures combined with the aggressive use of surveillance imaging techniques seem responsible for this paradoxical trend.34, 35 Moreover, more previously fatal injuries are perhaps reaching the emergency room now than in previous decades. With improved safety measures there may be a trade off between death for an increased rate of serious injuries. Thos epidemiological study allows clinicians to identify high yield constellations of injuries to quickly triage and treat patients involved in blunt trauma.
In this study the rate of injury to the thoracolumbar spine was 6.9% in patients presenting to level 1 trauma centers following blunt trauma. The most common mechanism was a motor vehicle accident, which accounted for 36.7% of fractures. This was followed by falls from height, which accounted for 31.7%. The most common fracture morphology was the burst fracture, occurring at a rate of 40% in this study. The most common geographic location was L1 occurring at 34.4%. The thoracolumbar junction (T11-L2) is biomechanically prone to injury as it marks the transition from the rigid thoracic spine to the flexible lumbar spine.36
Within this group of patients there were a host of associated injuries. For example, 26% of patients with a fracture of the thoracolumbar spine had a coexisting fracture of the cervical spine. This is a similar number to prior reports which have shown that patients with cervical spine fractures have a 20% risk of a secondary fracture somewhere else in the spine.37
Following this, 22% had injury to the thoracic region, which is predictable as a significant amount of force is directed through this area to the spine. In addition 18.2% of patients suffered a fracture or dislocation of an extremity. The next most frequent injuries were to the neurological system. 13% had head injuries which 10% had spinal or neurological injury (excluding head injury). Lastly 7.6% of patients with a thoracolumbar fracture sustained an intraabdominal injury. However this number jumped to 38.7% when looking only at flexion distraction type fractures.
In addition we found that compared to studies, which included the entire spine, thoracolumbar fractures had a lower rate of associated head trauma (12.96% vs 15.4%) and a higher rate of pelvic trauma (9.38% vs 3.38%).
4.1. Limitations
Some limitations must be recognized in our meta analysis. First was that some analyses had small numbers of studies. In these cases a fixed effects analysis was used to increase accuracy. Moreover, studies included in this paper range over a long period of publication times, with resulting rates of injuries perhaps changing between decades.
5. Conclusion
Our meta-analysis indicates that while fractures of the thoracolumbar spine occur at a relatively low rate, they are associated with a diverse array of injuries. To our knowledge this is the first study using meta-analysis to summarize the rates of thoracolumbar fracture in blunt trauma patients and their associated injuries. This information is valuable because the treating physician must be vigilant, and treat the whole patient. This study provides an overview of the rates of associated injury to help guide the management of these complex patients.
Conflicts of interest
The authors have none to declare.
References
- 1.Price C., Makintubee S., Herndon W., Istre G.R. Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988–1990. Am J Epidemiol. 1994;139(1):37–47. doi: 10.1093/oxfordjournals.aje.a116933. [DOI] [PubMed] [Google Scholar]
- 2.van den Berg M.E.L., Castellote J.M., de Pedro-Cuesta J., Mahillo-Fernandez I. Survival after spinal cord injury: a systematic review. J Neurotrauma. 2010;27(8):1517–1528. doi: 10.1089/neu.2009.1138. [DOI] [PubMed] [Google Scholar]
- 3.Fehlings M., Singh A., Tetreault L., Kalsi-Ryan S., Nouri A. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014:309. doi: 10.2147/CLEP.S68889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions [Internet]. Available from: http://handbook.cochrane.org/ [cited 24.04.16].
- 5.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Higgins J.P.T. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Neyeloff J.L., Fuchs S.C., Moreira L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC Res Notes. 2012;5(1):52. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuels L.E., Kerstein M.D. “Routine” radiologic evaluation of the thoracolumbar spine in blunt trauma patients: a reappraisal. J Trauma. 1993;34(1):85–89. doi: 10.1097/00005373-199301000-00016. [DOI] [PubMed] [Google Scholar]
- 9.Frankel H.L., Rozycki G.S., Ochsner M.G., Harviel J.D., Champion H.R. Indications for obtaining surveillance thoracic and lumbar spine radiographs. J Trauma. 1994;37(4):673–676. doi: 10.1097/00005373-199410000-00024. [DOI] [PubMed] [Google Scholar]
- 10.Cooper P.S. Complications of ankle and tibiotalocalcaneal arthrodesis. Clin Orthop. 2001;(391):33–44. doi: 10.1097/00003086-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Holmes J.F., Miller P.Q., Panacek E.A., Lin S., Horne N.S., Mower W.R. Epidemiology of thoracolumbar spine injury in blunt trauma. Acad Emerg Med. 2001;8(9):866–872. doi: 10.1111/j.1553-2712.2001.tb01146.x. [DOI] [PubMed] [Google Scholar]
- 12.Hsu J.M., Joseph T., Ellis A.M. Thoracolumbar fracture in blunt trauma patients: guidelines for diagnosis and imaging. Injury. 2003;34(6):426–433. doi: 10.1016/s0020-1383(02)00368-6. [DOI] [PubMed] [Google Scholar]
- 13.Inaba K., DuBose J.J., Barmparas G. Clinical examination is insufficient to rule out thoracolumbar spine injuries. J Trauma-Inj Infect. 2011;70(1):174–179. doi: 10.1097/TA.0b013e3181d3cc6e. [DOI] [PubMed] [Google Scholar]
- 14.Joaquim A.F., Daubs M.D., Lawrence B.D. Retrospective evaluation of the validity of the Thoracolumbar Injury Classification System in 458 consecutively treated patients. Spine J. 2013;13(12):1760–1765. doi: 10.1016/j.spinee.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Nelson D.W., Martin M.J., Martin N.D., Beekley A. Evaluation of the risk of noncontiguous fractures of the spine in blunt trauma. J Trauma Acute Care Surg. 2013;75(1):135–139. doi: 10.1097/ta.0b013e3182984a08. [DOI] [PubMed] [Google Scholar]
- 16.Gertzbein S.D. Scoliosis Research Society. Multicenter spine fracture study. Spine. 1992;17(5):528–540. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Magerl F., Aebi M., Gertzbein S.D., Harms J., Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 1994;3(4):184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 18.Meldon S.W., Moettus L.N. Thoracolumbar spine fractures: clinical presentation and the effect of altered sensorium and major injury. J Trauma. 1995;39(6):1110–1114. doi: 10.1097/00005373-199512000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Terregino C.A., Ross S.E., Lipinski M.F., Foreman J., Hughes R. Selective indications for thoracic and lumbar radiography in blunt trauma. Ann Emerg Med. 1995;26(2):126–129. doi: 10.1016/s0196-0644(95)70140-0. [DOI] [PubMed] [Google Scholar]
- 20.Saboe L.A., Reid D.C., Davis L.A., Warren S.A., Grace M.G. Spine trauma and associated injuries. J Trauma. 1991;31(1):43–48. doi: 10.1097/00005373-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Cooper C., Dunham C.M., Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: cognitive impairment and multiple injuries impede the detection of back pain and tenderness. J Trauma-Inj Infect. 1995;38(5):692–696. doi: 10.1097/00005373-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Leucht P., Fischer K., Muhr G., Mueller E.J. Epidemiology of traumatic spine fractures. Injury. 2009;40(2):166–172. doi: 10.1016/j.injury.2008.06.040. [DOI] [PubMed] [Google Scholar]
- 23.Lin Q., Zhou X., Wang X., Cao P., Tsai N., Yuan W. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc. 2012;21(3):474–481. doi: 10.1007/s00586-011-1961-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LeGay D.A., Petrie D.P., Alexander D.I. Flexion-distraction injuries of the lumbar spine and associated abdominal trauma. J Trauma. 1990;30(4):436–444. [PubMed] [Google Scholar]
- 25.Anderson P.A., Henley M.B., Rivara F.P., Maier R.V. Flexion distraction and chance injuries to the thoracolumbar spine. J Orthop Trauma. 1991;5(2):153–160. doi: 10.1097/00005131-199105020-00006. [DOI] [PubMed] [Google Scholar]
- 26.Tyroch A.H., McGuire E.L., McLean S.F. The association between chance fractures and intra-abdominal injuries revisited: a multicenter review. Am Surg. 2005;71(5):434–438. [PubMed] [Google Scholar]
- 27.Chapman J.R., Agel J., Jurkovich G.J., Bellabarba C. Thoracolumbar flexion-distraction injuries: associated morbidity and neurological outcomes. Spine. 2008;33(6):648–657. doi: 10.1097/BRS.0b013e318166df7b. [DOI] [PubMed] [Google Scholar]
- 28.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983;8(8):817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Dai L.-Y., Yao W.-F., Cui Y.-M., Zhou Q. Thoracolumbar fractures in patients with multiple injuries: diagnosis and treatment-a review of 147 cases. J Trauma. 2004;56(2):348–355. doi: 10.1097/01.TA.0000035089.51187.43. [DOI] [PubMed] [Google Scholar]
- 30.el-Khoury G.Y., Whitten C.G. Trauma to the upper thoracic spine: anatomy, biomechanics, and unique imaging features. AJR Am J Roentgenol. 1993;160(1):95–102. doi: 10.2214/ajr.160.1.8416656. [DOI] [PubMed] [Google Scholar]
- 31.Starnes M. Trends in non-fatal traffic injuries: 1996–2005. Natl Highw Traffic Saf Adm [Internet]. Available from: http://www-nrd.nhtsa.dot.gov/pubs/810944.pdf.
- 32.Wang M.C., Pintar F., Yoganandan N., Maiman D.J. The continued burden of spine fractures after motor vehicle crashes. J Neurosurg Spine. 2009;10(2):86–92. doi: 10.3171/SPI.2008.10.08279. [DOI] [PubMed] [Google Scholar]
- 33.Doud A.N., Weaver A.A., Talton J.W. Has the incidence of thoracolumbar spine injuries increased in the United States from 1998 to 2011? Clin Orthop. 2015;473(1):297–304. doi: 10.1007/s11999-014-3870-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hodson-Walker N.J. The value of safety belts: a review. Can Med Assoc J. 1970;102(4):391–393. [PMC free article] [PubMed] [Google Scholar]
- 35.Brown C.V.R., Antevil J.L., Sise M.J., Sack D.I. Spiral computed tomography for the diagnosis of cervical, thoracic, and lumbar spine fractures: its time has come. J Trauma. 2005;58(5) doi: 10.1097/01.ta.0000162149.89139.ff. 890-895-896. [DOI] [PubMed] [Google Scholar]
- 36.Wood K.B., Li W., Lebl D.S., Ploumis A. Management of thoracolumbar spine fractures. Spine J Off J North Am Spine Soc. 2014;14(1):145–164. doi: 10.1016/j.spinee.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 37.Sharma O.P., Oswanski M.F., Yazdi J.S., Jindal S., Taylor M. Assessment for additional spinal trauma in patients with cervical spine injury. Am Surg. 2007;73(1):70–74. [PubMed] [Google Scholar]