Abstract
Rapid and definitive diagnosis of viral respiratory infections is imperative in patient triage and management. We compared the outcomes for adult patients with positive tests for respiratory viruses at a tertiary care center across two consecutive influenza seasons (winters of 2010-2011 and 2012). Infections were diagnosed by conventional methods in the first season and by multiplex PCR (FilmArray) in the second season. FilmArray decreased the time to diagnosis of influenza compared to conventional methods (median turnaround times of 1.7 h versus 7.7 h, respectively; P = 0.015); FilmArray also decreased the time to diagnosis of non-influenza viruses (1.5 h versus 13.5 h, respectively; P < 0.0001). Multivariate logistic regression found that a diagnosis of influenza by FilmArray was associated with significantly lower odds ratios (ORs) for admission (P = 0.046), length of stay (P = 0.040), duration of antimicrobial use (P = 0.032), and number of chest radiographs (P = 0.005), when controlling for potential confounders. We conclude that the rapid turnaround time, multiplex nature of the test (allowing simultaneous detection of an array of viruses), and superior sensitivity of FilmArray may improve the evaluation and management of patients suspected of having respiratory virus infections.
INTRODUCTION
Respiratory viruses can cause not only mild upper respiratory tract infections but severe pneumonia, especially in immunocompromised hosts. Rapid and definitive diagnosis is critical in the management of viral respiratory infections and in timely isolation of infected patients. The 2009 H1N1 pandemic revealed the need for better diagnostic tests for influenza viruses. In addition, overlapping clinical presentations impede clinicians' ability to predict causative pathogens (whether bacterial or viral) and may lead to unnecessary antimicrobial use (1, 2). Nucleic acid amplification testing (NAAT)-based methods for detection of viral pathogens are increasingly used due to their excellent sensitivity and specificity and their ability to detect a wide spectrum of viral agents. Therefore, NAAT has many potential advantages over traditional methods, such as rapid antigen testing (which is <40 to 60% sensitive for influenza in adults), direct fluorescent-antibody (DFA) testing (which requires specialized laboratory training), or viral culture (which can take up to 10 days for a result) (3). Multiplex PCR using FilmArray (BioFire Diagnostics, Inc., a bioMérieux company, Salt Lake City, UT) is an NAAT method which can detect multiple viral pathogens with a single test (4). The FilmArray respiratory viral panel (RVP) was FDA cleared in May 2011 to detect 15 respiratory viral pathogens: influenza A virus and subtypes (influenza A H1, influenza A H1 2009, and influenza A H3 viruses), influenza B virus, parainfluenza 1 virus, parainfluenza 2 virus, parainfluenza 3 virus, parainfluenza 4 virus, respiratory syncytial virus (RSV), human metapneumovirus, adenovirus, rhinovirus/enterovirus, coronavirus NL63, and coronavirus HKU1.
In February 2012, the FilmArray RVP was implemented in the New York-Presbyterian Hospital/Weill Cornell Medical Center (NYP/WC) clinical microbiology laboratory. Due to the rapid turnaround time for FilmArray RVP, its excellent sensitivity and specificity, and a wider spectrum of detected viral targets, it replaced the combination of other viral diagnostic methods for nasopharyngeal swab or bronchoalveolar lavage (BAL) fluid specimens in the NYP/WC microbiology laboratory.
As emerging technologies are increasingly implemented in clinical microbiology laboratories for detection of respiratory viruses, studies are needed to identify the diagnostic tests that will lead to improved patient outcomes and more appropriate use of antimicrobial agents (1). The current study sought to evaluate the clinical impact of a laboratory-confirmed diagnosis of respiratory virus in patients ≥18 years old tested within 48 h of arrival at the hospital by FilmArray compared to conventional methods of diagnosis. Diagnostic methods included conventional methods in the first respiratory season compared to FilmArray the following year. We hypothesized that the use of FilmArray would be associated with fewer admissions and reductions in length of stay (LOS), duration of antimicrobial use, time to initiation of oseltamivir in influenza-positive patients, and ancillary testing.
MATERIALS AND METHODS
Study population.
The study was a retrospective cohort study of emergency department (ED) patients and inpatients ≥18 years old testing positive for a respiratory virus in the NYP/WC clinical microbiology laboratory, and whose respiratory specimen was received by the microbiology laboratory within 48 h of hospital arrival, in two consecutive influenza seasons (winter of 2010 to 2011 and winter of 2012). The available diagnostic tests for respiratory viruses during each influenza season are summarized in Table 1. FilmArray RVP replaced the earlier conventional methods, i.e., rapid antigen testing (BD Directigen EZ Flu A+B and BD Directigen EZ RSV; BD, Sparks, MD), Prodesse ProFlu+ PCR (for detection of influenza A/B viruses and RSV; Gen-Probe, Inc., San Diego), Luminex PCR (Luminex Corporation, Toronto, Canada), direct fluorescent-antibody testing (Diagnostic Hybrids, Inc., Athens, OH), and viral culture (consisting of a combination of R-mix [Diagnostic Hybrids] and conventional tube cell culture). In season 1, clinicians were able to order any of the available tests, all of which were performed on site except for Luminex PCR (sent out), which was typically reserved for immunocompromised or intensive care unit (ICU) patients requiring a more thorough diagnostic evaluation. Rapid antigen testing was available 24 h a day and 7 days a week, and Prodesse testing was performed in batches (1 to 3 times daily); details of test characteristics are provided in Table 1. In season 2, clinicians could order a full-panel FilmArray, limited testing for influenza virus/RSV (combined), or individual influenza virus or RSV FilmArray, which were available 24 h a day, 7 days a week. A list of patients with positive specimens from both study periods was obtained. Patients were excluded if they had a known positive test for a respiratory virus before being tested at NYP/WC or if their respiratory specimen was received by the microbiology laboratory more than 48 h after hospital arrival.
TABLE 1.
Available diagnostic tests for respiratory viruses in seasons 1 and 2
| Season | Test and comments |
|---|---|
| 1 (1 November 2010–31 March 2011) | Rapid antigen testing strategy |
| Rapid antigen test | |
| Detection of 3 viruses (influenza A and B viruses, RSV); turnaround time, 15–60 min | |
| Prodesse ProFlu+ PCR | |
| Detection of 3 viruses (influenza A and B viruses, RSV); turnaround time, 8–24 h, batched 1–3 times daily (extraction step required over 4 h) | |
| All negative rapid antigen tests were reflexed to Prodesse PCR due to low sensitivity of rapid antigen test | |
| During low-prevalence periods (early and late in the respiratory virus season), all positive rapid antigen tests were reflexed to Prodesse PCR | |
| Rapid antigen testing and Prodesse PCR were the two most commonly used viral diagnostic tests in season 1 | |
| Luminex PCR | |
| Detection of 12 viruses (influenza A virus, influenza A H1 virus, influenza A H3 virus, influenza B virus, parainfluenza 1 virus, parainfluenza 2 virus, parainfluenza 3 virus, RSV A, RSV B, human metapneumovirus, adenovirus, rhinovirus); turnaround time, 48 h (send-out test) | |
| Used in a minority of patients | |
| Direct fluorescent-antibody testing | |
| Detection of 3 viruses (influenza A and B viruses, RSV); turnaround time, 2–4 h | |
| Infrequently performed in our laboratory | |
| Viral culture | |
| Detection of 8 viruses (influenza A virus, influenza B virus, parainfluenza 1 virus, parainfluenza 2 virus, parainfluenza 3 virus, human metapneumovirus, RSV, adenovirus); turnaround time, 2–10 days | |
| 2 (29 February 2012–2 June 2012) | FilmArray PCR |
| Detection of 15 viruses (influenza A H1 virus, influenza A H1 2009 virus, influenza A H3 virus, influenza B virus, parainfluenza 1 virus, parainfluenza 2 virus, parainfluenza 3 virus, parainfluenza 4 virus, RSV, human metapneumovirus, adenovirus, rhinovirus/enterovirus, coronavirus NL63, coronavirus HKU1); turnaround time, 1–2 h | |
| Replaced all prior diagnostic methods for respiratory viruses used in season 1 | |
| Individual orders for FilmArray PCR for influenza virus or RSV were used in a minority of patients |
All patients in the study were tested by nasopharyngeal swabbing or bronchoalveolar lavage as part of routine medical care; no additional testing was done for research purposes.
Data abstraction.
Data were reviewed in a retrospective fashion after patients were discharged from NYP/WC. Data were collected from inpatient and outpatient electronic medical records (EMR) systems and the clinical microbiology laboratory database for time of specimen receipt. A data collection sheet was used for chart abstraction, and data were entered into an open-source, password-protected electronic database (ClinvestiGator). The study was approved by the Institutional Review Board at Weill Cornell Medical College.
Demographics (age, sex, racial or ethnic background, and zip code) and dates and times of key variables (test order, receipt in microbiology laboratory, and result availability in EMR) were collected. If a rapid antigen test was performed, data were also collected on reflex Prodesse testing whenever done (date and time of Prodesse result in EMR). Dates and times of admission and discharge from each hospital unit were collected (e.g., ED, inpatient ED [admitted patients in ED awaiting an inpatient bed], or medical ward). To determine the impact of FilmArray when used in the ED, the decision to admit or discharge a patient before or after the test result became available was documented. When a negative rapid antigen test result was followed by positive reflex Prodesse testing (defined as “discordant”), it was documented whether the patient's positive reflex test result was available in relation to the time of decision to admit or discharge. Previous health care exposures were captured (hospitalization in past 90 days, residence in long-term-care facility, or receiving care in a hemodialysis clinic in past 30 days). The patient's presenting symptoms, the presence or absence of prior antibiotic use, and the reason for admission were documented, as was the emergency severity index, for patients presenting in the ED (5). Presence of asthma or reactive airway disease and immunodeficient states was documented (HIV positivity, receipt of stem cell or solid organ transplant, or chronic corticosteroid or immunosuppressant medication). The Charlson comorbidity index (CCI) was used to summarize other comorbidities. Illness severity was assessed by documenting the most abnormal vital signs within 24 h of testing and the need for mechanical ventilation or intensive care unit admission.
Laboratory data that were captured included white blood cell count, absolute neutrophil count, absolute lymphocyte count, and positive microbiologic specimens from any site, for which the patient was treated. Documentation of ancillary testing included radiologic testing (chest radiographs and chest computed tomography [CT]), bronchoscopies, and types of abnormalities when present. Adjunctive treatment with corticosteroids and the administration of immunosuppressant medications during the hospital stay were documented. The name of and indication for any antimicrobial administered during the hospital visit or prescribed on discharge for coverage of the acute respiratory or febrile episode and the date and time of administration were documented. Antimicrobials given for chronic conditions (e.g., antivirals for HIV suppression or bacterial prophylaxis), perioperative prophylaxis, treatment of thrush or oral lesions, and any other antimicrobial use with an indication clearly unrelated to the acute episode being evaluated by viral testing were excluded (e.g., metronidazole administered for giardiasis). Data on antivirals used for respiratory viruses while in the hospital and on discharge were also captured (name of antiviral, dose, indication, and date and time of administration).
Definitions.
Turnaround time was defined as the difference from the time of specimen receipt in the clinical microbiology laboratory to the time of result availability in the EMR. The laboratory phoned clinicians with results of a positive influenza virus or RSV test in both seasons; the time of notification was usually a few minutes before the test result appeared in the EMR. If clinicians placed an individual order for influenza virus or RSV FilmArray PCR and the panel revealed a different target, the clinicians were notified and the full panel was revealed in the EMR to include results for all viruses. The turnaround time for negative rapid antigen tests followed by positive reflex Prodesse tests was defined as the time from specimen receipt in the laboratory (for rapid antigen testing) to the time of Prodesse result in the EMR. The time of admission was the time of the bed request order in the EMR. The time to discharge or admit was defined as the time of first entry to the ED either until the bed request order or until ED discharge (whichever came first). Patients were considered “tested in the ED” if the viral test was ordered in the ED before the bed request time or discharge time (regardless of time of specimen receipt in the microbiology laboratory). If patients returned to the ED <48 h after discharge, the repeat visit(s) was counted as part of the same admission (i.e., length of stay was calculated from the first ED entry to the last discharge). The duration of antimicrobial use was the time from administration of the first antimicrobial dose until administration of the last antimicrobial dose during the hospital stay. If two or more distinct antimicrobial courses were administered, the total duration included the duration of the first course added to the duration of the second course. In influenza virus-positive patients, the time to oseltamivir was the time of specimen receipt in the microbiology laboratory until the first administration of oseltamivir.
Statistical analyses.
Statistical analyses were completed using STATA version 10 (StataCorp LP, College Station, TX). Categorical variables were compared using the chi-square or Fisher exact test. Continuous variables were compared using the Student t test (for parametric data) or Wilcoxon rank sum test (for nonparametric data), as appropriate. Multivariate logistic and linear regression models were used to evaluate key outcomes among patients tested with FilmArray (season 2) relative to those tested using conventional methods (season 1), while adjusting for potential risk factors. Negative-binomial regression was used to compare the numbers of chest radiographs between groups. For all analyses, a P value of ≤0.05 was considered statistically significant.
RESULTS
Population characteristics.
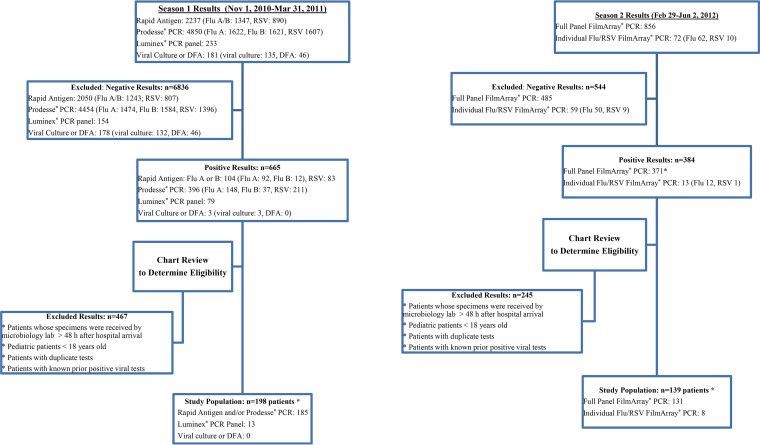
A total of 198 adult patients were included in the study during season 1, and 139 patients were included during season 2 (Fig. 1). The majority of positive viral tests in season 1 were performed by rapid antigen and/or Prodesse testing (n = 185), with some patients positive for a respiratory virus by Luminex (n = 13). During the second respiratory season, 131 distinct patients tested positive for a virus on the full-panel FilmArray PCR, while 8 patients tested positive using the individual orders for FilmArray PCR (for influenza virus or RSV only). Table 2 summarizes the demographic and clinical characteristics of both groups according to the virus that tested positive (influenza virus versus non-influenza respiratory viruses). The groups were generally comparable in demographics, illness severity, and laboratory parameters, with the exception of a higher rate of hospitalization in the past 90 days in the non-influenza virus group in season 1 (17/40 [43%] versus 20/85 [24%]; P = 0.03). Patients in season 2 who had an order placed for an individual influenza virus FilmArray PCR and had a detected virus other than influenza virus were included in the “non-influenza virus” group analysis.
FIG 1.
Flow diagram of all respiratory viral tests during season 1 and season 2 (excluding tests ordered in clinic). *, patients with coinfections at any time point were counted once for this figure.
TABLE 2.
Demographic and clinical characteristics of adults tested within 48 h of hospital arrival
| Characteristica | Value in patients positive for: |
|||||
|---|---|---|---|---|---|---|
| Influenza virus only |
Non-influenza viruses |
|||||
| Season 1 (n = 158) | Season 2 (n = 54) | P value | Season 1 (n = 40) | Season 2 (n = 85) | P value | |
| Age (yr), mean ± SD (range) | 55 ± 22 (18–101) | 59 ± 22 (23–91) | 0.28 | 63 ± 21 (19–91) | 57 ± 23 (18–95) | 0.13 |
| CCI, median (IQR) | 1 (0–2) | 1 (0–2) | 0.87 | 2 (1–4) | 2 (0–3) | 0.051 |
| Male sex, n (%) | 68 (43) | 21 (39) | 0.59 | 17 (43) | 35 (41) | 0.89 |
| Race or ethnic group, n (%) | 0.95 | 0.044 | ||||
| White | 77 (49) | 25 (46) | 21 (53) | 44 (52) | ||
| Black | 25 (16) | 8 (15) | 7 (18) | 12 (14) | ||
| Hispanic | 27 (17) | 12 (22) | 3 (8) | 12 (14) | ||
| Asian | 13 (8) | 4 (7) | 5 (13) | 1 (1) | ||
| Other or unknown | 18 (11) | 6 (11) | 4 (10) | 16 (19) | ||
| Asthma or reactive airway disease, n (%) | 25 (16) | 13 (24) | 0.17 | 7 (18) | 11 (13) | 0.50 |
| Immunosuppressed status, n (%)b | 38 (24) | 11 (20) | 0.58 | 20 (50) | 34 (40) | 0.29 |
| Previous antibiotic treatment, n (%) | 34 (22) | 16 (30) | 0.23 | 13 (33) | 24 (28) | 0.63 |
| Duration of symptoms (days), median (IQR); n | 3 (2–5); 156 | 3 (2–5) | 0.86 | 4 (2–7) | 4 (3–7); 83 | 0.30 |
| Symptoms, n (%) | ||||||
| Cough | 142 (90) | 48 (89) | 0.84 | 35 (88) | 75 (88) | 0.91 |
| Increased work of breathing | 83 (53) | 32 (59) | 0.39 | 32 (80) | 56 (66) | 0.11 |
| Vital signs within 24 h of testing, n (%) | ||||||
| Temp ≥ 38°C | 69 (44) | 30 (56) | 0.14 | 18 (45) | 25 (29) | 0.087 |
| Heart rate ≥ 100 bpm | 100 (63) | 31 (57) | 0.44 | 23 (58) | 42 (49) | 0.40 |
| Respiratory rate > 24 | 42 (27) | 16 (30) | 0.65 | 19 (48) | 28 (33) | 0.12 |
| Hypoxia (pulse oximetry < 93%) | 42 (27) | 14 (26) | 0.93 | 20 (51) | 35 (41) | 0.29 |
| Hypotension (SBP ≤ 90 mm Hg) | 21 (13) | 8 (15) | 0.78 | 14 (35) | 18 (21) | 0.099 |
| Emergency severity index, median (range); n | 3 (1–5); 145 | 3 (2–4); 50 | 0.33 | 3 (2–4); 36 | 3 (2–5); 78 | 0.15 |
| Respiratory viral testing only test performed, n (%) | 16 (10) | 3 (6) | 0.41 | 1 (3) | 4 (5) | 1 |
| CBC performed, n (%) | 139 (88) | 50 (93) | 0.45 | 39 (98) | 79 (93) | 0.43 |
| WBC (103/μl), median (IQR); n | 7.7 (5.6–10.3); 124 | 6.5 (5.5–8.3); 48 | 0.032 | 7.9 (5.4–12.4); 37 | 8.3 (5.5–11.6); 76 | 0.74 |
| ANC (103/μl), median (IQR) | 6 (4.4–8.6) | 5.2 (3.3–7.1) | 0.059 | 6 (4.9–9.6) | 5.5 (3.7–9.4) | 0.40 |
| ALC (103/μl), median (IQR) | 0.8 (0.5–1.1) | 0.7 (0.4–1.1) | 0.21 | 0.8 (0.4–1.3) | 1 (0.6–1.7) | 0.17 |
| Hospitalization in past 90 days, n (%) | 34 (22) | 11 (20) | 0.86 | 17 (43) | 20 (24) | 0.030 |
| Admitted to intensive care unit, n (%)c | 15 (9) | 8 (15) | 0.28 | 13 (33) | 16 (19) | 0.091 |
| Mechanical ventilation, n (%)c | 7 (4) | 4 (7) | 0.48 | 7 (18) | 6 (7) | 0.074 |
| Died during hospitalization, n (%)c | 2 (1) | 1 (2) | 1 | 3 (8) | 5 (6) | 0.71 |
IQR, interquartile range; CBC, complete blood count; WBC, white blood cell count; ANC, absolute neutrophil count; ALC, absolute lymphocyte count; CCI, Charlson comorbidity index; SBP, systolic blood pressure.
Immunosuppressed status if any of the following were present: history of AIDS, HIV, leukemia, lymphoma, metastatic cancer, hematopoietic stem cell transplant, solid organ transplant, corticosteroid use (equivalent of ≥5 mg prednisone) for at least 2 weeks before testing, immunosuppressant use for at least 2 weeks before testing, or immunosuppressant use during admission.
Variable related to current emergency department visit/hospital admission.
Influenza A and B viruses were the predominant viruses identified in season 1 (158/198 [80%]) and season 2 (54/139 [39%]), followed by RSV (15%) in season 1 and rhinovirus/enterovirus (30%) and metapneumovirus (19%) in season 2 (Table 3). The majority of patients had nasopharyngeal swab testing; in season 1, there were 3/198 (1.5%) patients with BAL fluid positive for respiratory viruses, compared to 1/139 (0.7%) patients in season 2 (P = 0.65). Viral coinfections were more common in season 2 (three double coinfections and one triple coinfection) than in season 1 (one double coinfection). Overall, there were high false-negative rates with rapid antigen testing in season 1. Among the 78 patients who were tested by both rapid antigen testing and Prodesse PCR, 73 were positive for influenza virus, with 82% of these being discordant (negative rapid antigen test followed by positive Prodesse test), and five were positive for RSV, with 80% of these discordant. The overall discordance rate for influenza virus or RSV was 82% (64/78).
TABLE 3.
Results of positive respiratory virus tests over two consecutive influenza seasons
| Characteristic | No. (%) in season: |
|
|---|---|---|
| 1 (n = 198) | 2 (n = 139) | |
| Positive test result | ||
| Rapid antigen (alone) | 51 (26) | |
| Prodesse (alone) | 56 (28) | |
| Rapid antigen with reflex to Prodessea | 78 (39) | |
| Discordant (rapid antigen negative, Prodesse positive) | 64 | |
| Concordant (rapid antigen positive, Prodesse positive) | 14 | |
| Luminex | 13 (7) | |
| Full-panel FilmArray | 131 (94) | |
| Individual orders for influenza virus or RSV FilmArray | 8 (6) | |
| Viruses detected | ||
| Influenza A virus | 142 (72)b | 36 (26)c |
| Influenza B virus | 16 (8) | 18 (13) |
| RSV | 29 (15) | 9 (6) |
| Human metapneumovirus | 3 (2) | 27 (19) |
| Rhinovirus/enterovirus | 8 (4) | 42 (30) |
| Adenovirus | 1 (0.5) | 1 (0.7) |
| Coronavirus NL63 | NAd | 4 (3) |
| Coronavirus HKU1 | NA | 2 (1) |
| Parainfluenza virus 1 | 0 | 0 |
| Parainfluenza virus 2 | 0 | 1 (0.7) |
| Parainfluenza virus 3 | 0 | 3 (2) |
| Parainfluenza virus 4 | NA | 1 (0.7) |
| Viral coinfection | ||
| Double | 1 (0.5)e | 3 (2)f |
| Triple | 0 | 1 (0.7)g |
No patients had a positive rapid antigen test followed by a negative Prodesse PCR. Of the 78 patients who were tested by both the rapid antigen and Prodesse tests, 73 were positive for influenza virus (60 were discordant, and 13 concordant) and 5 were positive for RSV (4 were discordant and 1 was concordant).
One hundred forty-one patients tested positive for influenza A virus with the subtype not specified; one tested positive for influenza A virus H3.
Twenty-one patients tested positive for influenza A virus H3, 14 tested positive for influenza A virus H1 2009, and 1 tested positive for influenza A virus with the subtype not specified.
NA, not applicable.
Double coinfection with human metapneumovirus and rhinovirus.
Double coinfections with rhinovirus/enterovirus and parainfluenza virus 3, rhinovirus/enterovirus and human metapneumovirus, and human metapneumovirus and parainfluenza virus 2.
Triple coinfection with influenza A virus H1 2009, rhinovirus/enterovirus, and coronavirus NL63.
Impact on ED admission decisions, LOS, and turnaround times.
The majority of the influenza virus-positive patients in both season 1 and season 2 had a viral test ordered in the ED before the decision to admit or discharge (64% versus 57%, respectively; P = 0.39) (Table 4). The proportions of patients tested in the ED (before the decision to admit or discharge) were comparable between seasons 1 and 2 in the groups testing positive for influenza or non-influenza viruses. The influenza patients tested by FilmArray had a trend toward higher discharge rates from the ED than the rapid antigen test group, which included all testing options in season 1 (rapid antigen, Prodesse, and Luminex): 61% versus 50% (P = 0.25). This difference in discharge rates became more pronounced and significant when comparing the influenza patients tested by FilmArray to the influenza patients with discordant results in season 1 (61% versus 37%; P = 0.036). There was also a trend toward higher rates of discharge from the ED for patients testing positive for non-influenza viruses on FilmArray than for the rapid antigen group (44% versus 17%; P = 0.067). Significantly more patients who tested positive by FilmArray for non-influenza viruses were discharged from the ED before arrival on the ward, despite being initially slated for admission (21% versus 5%; P = 0.049). Study outcomes were not analyzed separately for the patients tested in the ED versus patients tested after arrival on the wards, since we included only patients whose specimen was received by the microbiology laboratory within 48 h of hospital arrival, to minimize confounding by patients who developed onset of symptoms during a hospital admission and who may have been admitted for reasons unrelated to the acute respiratory illness. The most common reasons for admission for the patients tested on the wards in both seasons were related to their acute respiratory illness: either dyspnea/shortness of breath/hypoxia or pneumonia/workup pneumonia.
TABLE 4.
Admit decisions, lengths of stay, turnaround times, and ancillary testing
| Characteristica | Value in patients positive for: |
|||||
|---|---|---|---|---|---|---|
| Influenza virus only |
Non-influenza viruses |
|||||
| Season 1 (n = 158) | Season 2 (n = 54) | P value | Season 1 (n = 40) | Season 2 (n = 85) | P value | |
| Test ordered in ED before decision to admit or discharge, n (%) | 101 (64) | 31 (57) | 0.39 | 18 (45) | 32 (38) | 0.43 |
| Discharged from ED, n (%) | 50 (50) | 19 (61) | 0.25 | 3 (17) | 14 (44) | 0.067 |
| After test result | 39 (39) | 13 (42) | 0 (0) | 9 (28) | ||
| Before test result | 11 (11) | 6 (19) | 0.083 | 3 (17) | 5 (16) | 0.054 |
| Discordant subgroup discharged from ED, n (%) | 17/46 (37) | 0.036b | ||||
| Admitted from ED, n (%) | 51 (51) | 12 (38) | 15 (83) | 18 (57) | ||
| After test result | 26 (26) | 2 (6) | 2 (11) | 4 (13) | ||
| Before test result | 25 (25) | 10 (32) | 13 (72) | 14 (44) | ||
| Time (h) to discharge or admit if test ordered in ED, median (IQR); n | 5.0 (3.4–7.7); 101 | 5.7 (4.1–7.9); 31 | 0.54 | 3.6 (2.7–5.8); 18 | 4.6 (2.9–6.8); 32 | 0.36 |
| Admitted as inpatient (irrespective of time of test order), n (%) | 109 (69) | 35 (65) | 0.57 | 37 (93) | 71 (84) | 0.26 |
| Slated for admission but discharged from ED after first test result | 26/109 (24) | 13/35 (37) | 0.12 | 2/37 (5) | 15/71 (21) | 0.049 |
| Time (h) to floor bed if specimen received while in ED, median (IQR); n | 30.2 (16.7–51.9); 62 | 35.3 (9.6–50.4); 11 | 0.87 | 31.9 (20.0–51.3); 16 | 25.4 (11.3–46.2); 32 | 0.36 |
| Length of stay (h), median (IQR) | 49.8 (9.6–134.4) | 38.8 (8.2–116.2) | 0.63 | 122.1 (62.2–215.1) | 85.2 (25.5–191.8) | 0.065 |
| Discordant subgroup | 56.8 (12.8–123.3) | 0.26b | ||||
| Turnaround time (h) of positive viral test, median (IQR) | 7.7 (0.8–14) | 1.7 (1.6–2.2) | 0.015 | 13.5 (8.4–38.7) | 1.5 (1.4–2.1) | <0.0001 |
| Discordant subgroup | 13.3 (10–16.9) | <0.0001b | ||||
| Discharged from hospital before positive result, n (%) | 26 (16) | 5 (9) | 0.27 | 7 (18) | 7 (8) | 0.13 |
| Discordant subgroup | 17/60 (28) | 0.016b | ||||
| CXR performed, n (%) | 139 (88) | 49 (91) | 0.80 | 36 (90) | 77 (91) | 1 |
| No. of CXRs per patient, median (IQR) | 1 (1–2) | 1 (1–1) | 0.40 | 2 (1–5.5) | 1 (1–2) | 0.036 |
| Chest CT performed, n (%) | 38 (24) | 9 (17) | 0.26 | 15 (38) | 24 (28) | 0.30 |
| No. of CTs per patient, median (IQR) | 1 (1–1) | 1 (1–1) | 0.90 | 1 (1–1) | 1 (1–1) | 0.12 |
| Bronchoscopies performed, n (%) | 9 (6) | 3 (6) | 1 | 4 (10) | 8 (9) | 1 |
| No. of bronchoscopies per patient, median (IQR) | 1 (1–2) | 1 (1–2) | 1 | 1 (1–1) | 1 (1–3.5) | 0.18 |
| Radiographic abnormalities on chest imaging, n (%) | 54/141 (38) | 14/49 (29) | 0.22 | 24/38 (63) | 36/78 (46) | 0.085 |
IQR, interquartile range; CXR, chest radiograph; CT, computed tomography.
P value for comparisons between discordant subgroup (season 1) and FilmArray (season 2).
The median length of stay (LOS) among the influenza patients tested by FilmArray versus those tested in the rapid antigen group was 38.8 versus 49.8 h (P = 0.63); the difference became more pronounced when comparing the influenza patients tested by FilmArray to the influenza patients with discordant results in season 1 (38.8 versus 56.8 h; P = 0.26). The median LOS among patients in the FilmArray group with a non-influenza virus compared to the rapid antigen group was 85.2 versus 122.1 h (P = 0.065). The median turnaround time for a positive viral test was significantly longer in the rapid antigen group than in the FilmArray group, i.e., 7.7 versus 1.7 h for patients with influenza viruses (P = 0.015), with an even longer median turnaround time in the discordant subgroup (13.3 versus 1.7 h; P < 0.001) and among patients with non-influenza viruses (13.5 versus 1.5 h; P < 0.001). There was a trend toward more patients being discharged from the hospital before a positive influenza test result became available in the rapid antigen group than in the FilmArray group (16% versus 9%; P = 0.27); there was a significant difference when comparing the discordant subgroup to the FilmArray group (28% versus 9%; P = 0.016). There was a similar trend in more patients being discharged before a positive test result for a non-influenza virus became available in the rapid antigen group (18% versus 8%; P = 0.13).
Antimicrobial use.
Rates of antimicrobial use in the hospital were similar between groups in the influenza and non-influenza virus categories. In both seasons 1 and 2, 56% of patients testing positive for influenza virus received at least 1 antimicrobial dose in the hospital (89/158 versus 30/54; P = 0.92). Similarly, 32/40 (80%) of patients in season 1 and 62/85 (73%) of patients in season 2 testing positive for non-influenza viruses received at least 1 antimicrobial dose in the hospital (P = 0.39). There was no statistically significant difference between the time of the viral test order and the start time for any antimicrobial (including a one-time order) between the two seasons (P = 0.70) or in the start time of a standing antimicrobial course (P = 0.94). The median duration of use of antimicrobials in influenza patients was 48.1 h in season 1 versus 23.7 h in season 2 (P = 0.24). There was a trend toward a significantly longer duration of antimicrobial use in influenza patients with discordant results in season 1 versus season 2 (58.1 versus 23.7 h; P = 0.17) and in patients with non-influenza viruses (123.7 versus 89.2 h; P = 0.061). There was also a trend toward a significantly higher rate of antimicrobial use on discharge in influenza patients in the discordant subgroup in season 1 than in season 2 (37% versus 24%; P = 0.15) and in patients with non-influenza viruses (35% versus 24%; P = 0.18). The planned duration of discharge antimicrobial use in influenza patients was 5 days in season 1 versus 4 days in season 2 (P = 0.27), and it was 6 days versus 5 days in patients with non-influenza viruses (P = 0.78).
The most commonly used antimicrobials in season 1 versus season 2 were azithromycin (63% versus 68%), ceftriaxone (45% versus 33%), intravenous (i.v.) vancomycin (38% versus 36%), piperacillin-tazobactam (34% versus 36%), and levofloxacin (23% versus 24%). The most common indications for antimicrobials were pneumonia (including empirical therapy), sepsis (including empirical therapy), and chronic obstructive pulmonary disease (COPD) exacerbation/bronchitis. There was no significant difference in the numbers of patients with bacterial coinfections between seasons 1 and 2: 29/198 (14.6%) versus 15/139 (10.8%), respectively (P = 0.30). There was also no significant difference in the numbers of patients with BAL fluid positive for bacteria between seasons 1 and 2: 5/198 (2.5%) versus 2/139 (1.4%), respectively (P = 0.70). A comparison of outcomes between sources (nasopharyngeal swab versus BAL fluid) would not be useful given the limited number of BAL fluid samples.
Influenza patients and oseltamivir use.
The rates of antiviral treatment in patients with influenza were similar in seasons 1 and 2, with 61% of patients in both groups receiving at least 1 dose of oseltamivir or inhaled zanamivir in the hospital (96/158 versus 33/54; P = 0.96); there were also similar median times to first dose of an antiviral (9.5 versus 5.2 h, respectively; P = 0.74). However, the discordant subgroup with influenza in season 1 had a significantly longer median time to the first dose of an antiviral than those in season 2 (15.9 versus 5.2 h; P = 0.013), lower rates of antiviral treatment on discharge (19/60 [32%] versus 30/54 [56%]; P = 0.010), and overall lower rates of antiviral treatment either in the hospital or on discharge (33/60 [55%] versus 40/54 [74%]; P = 0.034).
Multivariate analyses.
On multivariate logistic regression, patients with influenza virus positive by FilmArray had a significantly lower odds ratio (OR) for being admitted if tested in the ED, when adjusted for age, immunosuppressed status, asthma, and emergency severity index (OR, 0.32 [95% confidence interval {CI}, 0.1 to 0.98]; P = 0.046). Similarly, patients with influenza virus positive by FilmArray had a significantly lower LOS (P = 0.040), antimicrobial duration (P = 0.032), and number of chest radiographs (P = 0.005), when adjusted for age, immunosuppressed status, asthma, and ICU admission (Table 5).
TABLE 5.
Univariate and multivariate linear regressions for outcomes using FilmArray PCR compared to conventional testinga
| Outcome | Patients positive for influenza virus (n = 212) |
Patients positive for non-influenza viruses (n = 125) |
||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted coefficient (95% CI) | P value | Adjusted coefficient (95% CI) | P value | Unadjusted coefficient (95% CI) | P value | Adjusted Coefficient (95% CI) | P value | |
| Length of stay | −0.12 (−0.62, 0.37) | 0.63 | −0.37 (−0.73, −0.018) | 0.040 | −0.57 (−1.11, −0.016) | 0.044 | −0.091 (−0.52, 0.34) | 0.68 |
| Duration of antimicrobial useb | −0.61 (−1.28, 0.061) | 0.074 | −0.68 (−1.29, −0.060) | 0.032 | −0.091 (−0.69, 0.51) | 0.76 | 0.12 (−0.43, 0.67) | 0.66 |
| No. of chest radiographsc | −0.43 (−0.80, −0.067) | 0.020 | −0.42 (−0.72, −0.13) | 0.005 | −0.32 (−0.78, 0.13) | 0.16 | 0.022 (−0.33, 0.38) | 0.90 |
| Time to anti-influenza treatmentd | −0.18 (−0.69, −0.33) | 0.48 | −0.20 (−0.65, 0.25) | 0.37 | NAe | |||
All outcomes in multivariate analyses were adjusted for age, immunosuppressed status, asthma, and admission to ICU. Length of stay, duration of antimicrobial use, and time to anti-influenza treatment were analyzed using the natural log of data due to nonnormal distributions. The number of chest radiographs was analyzed using negative binomial regression.
Patients positive for influenza virus who received antimicrobials, n = 96 of 119 due to logarithmic transformation (only values above 0 could be transformed). Patients positive for non-influenza viruses who received antimicrobials, n = 84 of 94 due to logarithmic transformation.
Patients positive for influenza virus who had a chest radiograph, n = 188. Patients positive for non-influenza viruses who had a chest radiograph, n = 113.
Patients who received anti-influenza treatment, n = 123 of 129 due to logarithmic transformation.
NA, not applicable.
DISCUSSION
We compared the outcomes for adult patients with positive tests for respiratory viruses at a tertiary-care center across two influenza seasons who were diagnosed by conventional methods in the first season and with multiplex PCR in the second season. We found a significantly decreased time to positive viral test results with FilmArray compared to conventional methods. Our findings indicate that diagnosis of influenza by multiplex PCR (FilmArray) was associated with significantly lower ORs for admission, length of stay, duration of antimicrobial use, and number of chest radiographs, when controlling for potential confounders. The rapid turnaround time and superior sensitivity of FilmArray, along with its multiplex array for detecting other respiratory viruses, can allow earlier discontinuation of antimicrobials.
A significant drawback of the rapid antigen test is its low sensitivity and high discordance with NAAT. In the present study, 82% of patients testing positive for influenza virus had discordant test results when tested by both rapid antigen test and Prodesse PCR. This discordant subgroup with influenza also had significantly lower rates of discharge from the ED than the multiplex PCR group, significantly longer turnaround times for laboratory results, a trend toward longer duration of antimicrobial use in the hospital with higher rates of antimicrobial use on discharge, significantly lower rates of antiviral treatment, and a longer time to antiviral initiation (likely due to a longer time to positive results).
Our study is the only one to our knowledge that compared outcomes in the adult population using FilmArray versus conventional methods during two consecutive respiratory virus seasons (winters of 2010-2011 and 2012). A study by Xu et al. evaluated outcomes in pediatric patients up to 21 years old after the implementation of FilmArray RVP in a general (core) laboratory from 14 December 2011 to 19 April 2012 (6). The median turnaround time was 1.4 h (comparable to the medians of 1.5 and 1.7 h in our study for influenza and non-influenza viruses, respectively). Their retrospective chart review of 97 patients testing positive for influenza virus on FilmArray in March 2012 revealed that 44/97 (45%) of these patients had a positive test result available before ED discharge, compared to 13/19 (68%) of patients tested by FilmArray in our study. Furthermore, 81% of patients were treated with oseltamivir in the study by Xu et al., which is comparable to the 74% in our study; however, their study did not include a comparison group before FilmArray for rates of oseltamivir treatment or other patient-related outcomes.
Another retrospective study, by Rogers et al., evaluated outcomes in pediatric patients (3 months to 21 years old) admitted to the hospital with an acute respiratory illness before and after implementation of FilmArray (7). Pre-FilmArray methods included primarily batched PCR analysis for influenza A and B viruses and RSV (Focus Diagnostics, Cypress, CA), with a minority of patients (11%) also tested by Prodesse for parainfluenza viruses 1 through 3 and human metapneumovirus (<1%). As in our study, the authors found that the use of FilmArray decreased the duration of antibiotic use and the length of inpatient stay.
A study by Gelfer et al. compared outcomes in adult patients with community-acquired pneumonia and included additional diagnostic testing with FilmArray versus conventional methods (8). The authors found that detection of a viral pathogen in conjunction with a low serum procalcitonin level resulted in fewer days of antibacterial therapy. This effect, however, was offset by the incomplete response of providers in that antibacterials were discontinued in only 4 of 18 patients with apparent viral infections despite a mean turnaround time of 1.8 h, thus highlighting a potential need for real-time communication of results between a member of an antibiotic stewardship team and treating physicians.
A study by Nelson et al. evaluated the cost-effectiveness of rapid multiplex PCR assays for influenza virus (FilmArray) compared to traditional PCR, DFA, and rapid antigen tests in children presenting to the ED (9). The incremental cost-effectiveness of rapid multiplex PCR compared to rapid antigen tests was $115,556 per quality-adjusted life year (QALY) for children 3 to 36 months old and $228,000 per QALY for older children 3 to 18 years old. The rapid multiplex PCR strategy was the most effective testing strategy in both pediatric age groups.
A major limitation of our study is the retrospective, nonrandomized design. There may have been factors that could have influenced clinician behavior between the two respiratory seasons that were not accounted for in our analysis. Furthermore, the incidence of various respiratory viruses may have varied across the two seasons. The 2011-2012 flu season (season 2) began late and was mild compared to season 1, with fewer cases of influenza A or B and a predominance of non-influenza viruses. The severity of season 1 compared to season 2 could have been a significant unmeasured confounder in possibly affecting some of the study outcomes (such as turnaround time or length of stay), as the ED or microbiology laboratory may have been busier in season 1 than in season 2. There were also no data collected on patients with negative final test results.
In conclusion, the use of a sensitive, rapid, multiplex PCR to diagnose influenza in adults was associated with decreased admission rates, shorter lengths of stay, shorter durations of antimicrobial therapy, and fewer chest radiographs than the use of conventional methods.
ACKNOWLEDGMENTS
S. G. Jenkins received a research grant from BioFire for support of a clinical trial on the FilmArray blood culture identification system. The other authors report no conflicts of interest.
Funding Statement
T.J.W. serves as investigator of the Save Our Sick Kids Foundation and as a scholar in emerging infectious diseases of the Sharp Family Foundation.
REFERENCES
- 1.Caliendo AM. 2011. Multiplex PCR and emerging technologies for the detection of respiratory pathogens. Clin Infect Dis 52(Suppl 4):S326–S330. doi: 10.1093/cid/cir047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Archimbaud C, Chambon M, Bailly JL, Petit I, Henquell C, Mirand A, Aublet-Cuvelier B, Ughetto S, Beytout J, Clavelou P, Labbé A, Philippe P, Schmidt J, Regagnon C, Traore O, Peigue-Lafeuille H. 2009. Impact of rapid enterovirus molecular diagnosis on the management of infants, children, and adults with aseptic meningitis. J Med Virol 81:42–48. doi: 10.1002/jmv.21330. [DOI] [PubMed] [Google Scholar]
- 3.Harper SA, Bradley JS, Englund JA, File TM, Gravenstein S, Hayden FG, McGeer AJ, Neuzil KM, Pavia AT, Tapper ML, Uyeki TM, Zimmerman RK, Expert Panel of the Infectious Diseases Society of America. 2009. Seasonal influenza in adults and children–diagnosis, treatment, chemoprophylaxis, and institutional outbreak management: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis 48:1003–1032. doi: 10.1086/598513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poritz MA, Blaschke AJ, Byington CL, Meyers L, Nilsson K, Jones DE, Thatcher SA, Robbins T, Lingenfelter B, Amiott E, Herbener A, Daly J, Dobrowolski SF, Teng DH, Ririe KM. 2011. FilmArray, an automated nested multiplex PCR system for multi-pathogen detection: development and application to respiratory tract infection. PLoS One 6:e26047. doi: 10.1371/journal.pone.0026047 (Erratum, doi:.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elshove-Bolk J, Mencl F, van Rijswijck BT, Simons MP, van Vugt AB. 2007. Validation of the Emergency Severity Index (ESI) in self-referred patients in a European emergency department. Emerg Med J 24:170–174. doi: 10.1136/emj.2006.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu M, Qin X, Astion ML, Rutledge JC, Simpson J, Jerome KR, Englund JA, Zerr DM, Migita RT, Rich S, Childs JC, Cent A, Del Beccaro MA. 2013. Implementation of FilmArray respiratory viral panel in a core laboratory improves testing turnaround time and patient care. Am J Clin Pathol 139:118–123. doi: 10.1309/AJCPH7X3NLYZPHBW. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers BB, Shankar P, Jerris RC, Kotzbauer D, Anderson EJ, Watson JR, O'Brien LA, Uwindatwa F, McNamara K, Bost JE. 2015. Impact of a rapid respiratory panel test on patient outcomes. Arch Pathol Lab Med 139:636–641. doi: 10.5858/arpa.2014-0257-OA. [DOI] [PubMed] [Google Scholar]
- 8.Gelfer G, Leggett J, Myers J, Wang L, Gilbert DN. 2015. The clinical impact of the detection of potential etiologic pathogens of community-acquired pneumonia. Diagn Microbiol Infect Dis 83:400–406. doi: 10.1016/j.diagmicrobio.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson RE, Stockmann C, Hersh AL, Pavia AT, Korgenksi K, Daly JA, Couturier MR, Ampofo K, Thorell EA, Doby EH, Robison JA, Blaschke AJ. 2015. Economic analysis of rapid and sensitive polymerase chain reaction testing in the emergency department for influenza infections in children. Pediatr Infect Dis J 34:577–582. doi: 10.1097/INF.0000000000000703. [DOI] [PubMed] [Google Scholar]