Abstract
Meniscal ramp lesions are more frequently associated with anterior cruciate ligament (ACL) injuries than previously recognized. Some authors suggest that this entity results from disruption of the meniscotibial ligaments of the posterior horn of the medial meniscus, whereas others support the idea that it is created by a tear of the peripheral attachment of the posterior horn of the medial meniscus. Magnetic resonance imaging (MRI) scans have been reported to have a low sensitivity, and consequently, ramp lesions often go undiagnosed. Therefore, to rule out a ramp lesion, an arthroscopic evaluation with probing of the posterior horn of the medial meniscus should be performed. Several treatment options have been reported, including nonsurgical management, inside-out meniscal repair, or all-inside meniscal repair. In cases of isolated ramp lesions, a standard meniscal repair rehabilitation protocol should be followed. However, when a concomitant ACL reconstruction (ACLR) is performed, the rehabilitation should follow the designated ACLR postoperative protocol. The purpose of this article was to review the current literature regarding meniscal ramp lesions and summarize the pertinent anatomy, biomechanics, diagnostic strategies, recommended treatment options, and postoperative protocol.
Keywords: ramp lesion, meniscus tear, ACL, meniscocapsular, hidden lesion
Concomitant intra-articular lesions are commonly seen in patients sustaining anterior cruciate ligament (ACL) rupture.4,7 Approximately 43% of all ACL-injured patients have been reported to have an associated lateral or medial meniscal injury.23 In 1988, Strobel40 described a particular type of meniscal injury associated with ACL rupture involving the peripheral attachment of the posterior horn of the medial meniscus. Currently known as a ramp lesion, this pathology has historically been under-recognized because it is commonly located within a posteromedial “blind spot” when using standard anterolateral and anteromedial arthroscopic portals.41 This potential difficulty in diagnosis is clinically important as ramp lesions have been reported to be present in 9% to 17% of all ACL tears.5,26 Furthermore, the use of imaging modalities such as magnetic resonance imaging (MRI) to detect ramp lesions has a low reported sensitivity.5 Due to the limited utility of MRI and the difficulty of identifying ramp lesions through the standard anterior portals, it is vital to perform a systematic arthroscopic exploration to diagnose these “hidden” lesions.38
There is no consensus regarding the definition of meniscal ramp lesions, as different anatomical locations have been proposed as the site of injury. Originally, a ramp lesion was defined as a longitudinal tear of the peripheral attachment of the posterior horn of the medial meniscus at the meniscocapsular junction of less than 2.5 cm in length.26 However, recent literature has suggested that ramp lesions are associated with injury to the meniscotibial ligament attachment of the posterior horn of the medial meniscus.38 Regardless of the definition, these lesions can cause pain, dysfunction, and altered knee kinematics.38 Because of the prevalence, potential importance, and diagnostic challenges associated with these injuries, we present a review of the currently available literature on ramp lesions using searches of PubMed, MEDLINE, and Cochrane databases using the keywords ramp lesion, ramp tear, meniscocapsular, and hidden lesion.
Anatomy
The medial meniscus is a semilunar fibrocartilage structure that covers approximately 50% of the medial tibial plateau.11 It is broader posteriorly, measuring approximately 11 mm in width, and becoming narrower anteriorly toward the anterior meniscal root. Some authors divide the meniscus into 3 segments (anterior horn, body, and posterior horn) while others divide it into 5 zones that are distinguishable on an anatomical basis (anterior root [zone 1], anteromedial zone [zone 2], medial zone [zone 3], posterior zone [zone 4], and the posterior root [zone 5]).41
The anterior and posterior roots anchor the meniscus to the tibial plateau,22 and the body of the meniscus is attached to the adjacent joint capsule and to the tibia by the meniscotibial ligaments. These attachments are important for kinematics and injury patterns of the medial meniscus as tibial and femoral attachments in the posteromedial aspect of the medial meniscus make it less mobile compared with the lateral meniscus.44 The reduced mobility of the medial meniscus makes it susceptible to injuries, especially in deep flexion and with rotational trauma when the pressure is increased in the posterior horn of the medial meniscus.
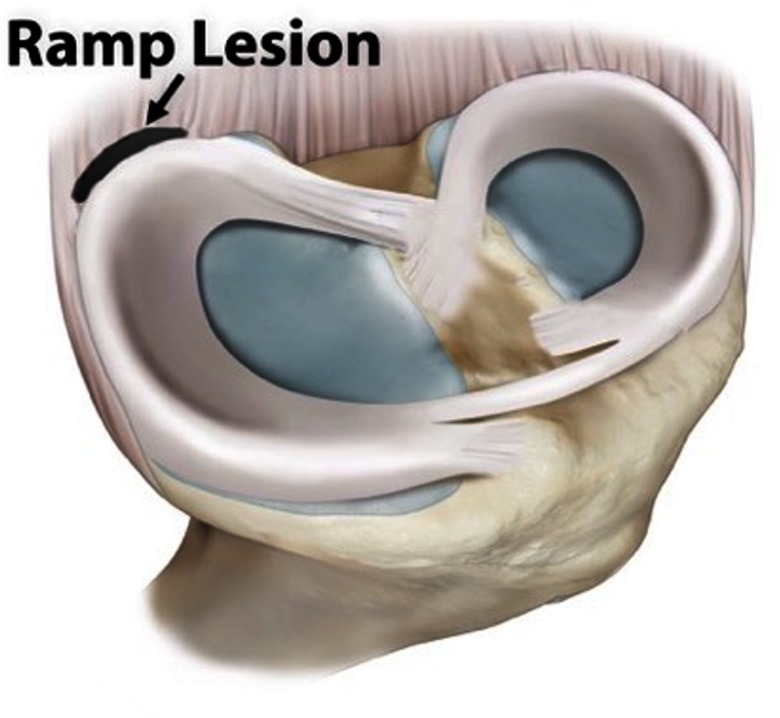
Despite a recent increase in the awareness of tears near the posterior aspect of the medial meniscus,18,25,38 clear anatomic descriptions of meniscal ramp lesions remain elusive. For the purpose of this review, ramp lesions are defined as those that involve a tear or disruption of the peripheral meniscocapsular attachments of the posterior horn of the medial meniscus (Figure 1).
Figure 1.
Schematic diagram of a left knee (disarticulated from the femur) demonstrating the location of a ramp lesion in the posteromedial meniscocapsular junction of the medial meniscus.
Epidemiology
A review of the literature demonstrated that lateral meniscal tears occur slightly more frequently than medial tears in knees with acute ACL injuries, with a mean distribution of 56% lateral to 44% medial.8,37 However, in the setting of chronic ACL deficiency, medial meniscal tears are more common.8,37 Despite these trends in the available literature, 2 recent studies noted a high prevalence of medial meniscal ramp lesions in both acutely and chronically ACL-injured patients. In a prospective descriptive study, Bollen5 found a 9.3% prevalence of medial meniscal ramp lesions in 183 consecutive patients undergoing ACL reconstruction (ACLR). However, this study was limited in its relatively small sample size. In an attempt to further classify these lesions, Liu et al26 performed an extensive study by arthroscopically evaluating for meniscal ramp lesions in 868 patients undergoing ACLR. They found an even higher prevalence of ramp lesions, noting that 16.6% of patients had this lesion. Both of these studies defined a ramp lesion as a tear of the peripheral attachment of the posterior horn of the junction between the medial meniscus and the synovium or capsule.
These studies build upon earlier literature suggesting an association between ACL injury and medial meniscal tears. Smith and Barrett37 performed a prospective study on the location of 575 meniscal tears associated with ACL injuries. They reported that peripheral posterior horn tears of the medial meniscus were the most common type of tear, comprising 40% of medial meniscus tears. Furthermore, more than 75% of medial meniscal tears in the ACL-deficient knee occurred in the peripheral posterior horn. However, they did not define whether those lesions were located at the posterior meniscocapsular junction. Regardless of the specific descriptors used to report such tears, these studies are important in demonstrating the injury risk to the medial meniscus in association with ACL rupture.
While ramp lesions are associated with ACL injury, other known risk factors have also been reported in the literature. Reported associated risk factors for sustaining a ramp lesion are age, sex, and time from ACL injury to surgery.26 Liu et al26 reported an 18.56% prevalence of ramp lesions in males compared with 11.97% in females (P = .01). Patients younger than 30 years (P < .01) also had a considerably higher prevalence of ramp lesions. However, there was no significant difference in the prevalence of ramp lesion between patients aged 10 to 20 years and 20 to 30 years, as well as between patients between 30 to 40 years and older than 40 years.26 Additionally, the prevalence of ramp lesions significantly increased as time since injury increased until 24 months after a nonsurgical ACL injury. After 24 months, the prevalence plateaued.26 Thus, a significantly higher prevalence of ramp tears was reported in patients with chronic ACL tears compared with patients with acute ACL tears.26
Biomechanics
Biomechanical studies have demonstrated the importance of the menisci, as they contribute to load transmission and distribution, joint lubrication, proprioception, cartilage nutrition, and act as a secondary stabilizing structure.2 This is especially true for the medial meniscus, which has been reported to play a key role in stabilizing the knee joint in chronically ACL-deficient knees.6,36 Hughston and Eilers20 described the close relationship that exists between the meniscus, the joint capsule, the posterior oblique ligament, and the semimembranosus tendon and how the capsular arm of the semimembranosus tendon insertion translates the posterior horn of the meniscus posteriorly during knee flexion. Moreover, Hughston and Eilers20 suggested that a contraction of the semimembranosus muscle that occurs while the medial meniscus is “wedged” between the femur and tibia would expose and stress the meniscocapsular interface and potentially result in a peripheral meniscal tear. This tear can occur in knees with either acute or chronic ACL tears.20,37 Papageorgiou et al29 reported that the forces on the medial meniscus were increased by 200% in response to anterior tibial loads with a transected ACL. Likewise, deficiency of the medial meniscus has been associated with ACLR failure.29 When a medial meniscectomy is performed with an ACLR, the in situ forces in the reconstructed ACL graft increase between 33% and 50%.29 In a human cadaveric study by Peltier et al,30 the authors reinforced the concept that the posterior horn of the medial meniscus is a secondary restraint to anterior tibial translation.
Currently, the available literature discussing the biomechanical consequences of ramp lesions is limited. It is not clear whether these lesions affect joint kinematics and loading in the medial compartment of the knee similar to ACL deficiency15,28 or posterior root lesions and complete radial tears.24 However, ramp lesions are reported to increase forces on the ACL, and lesions of the meniscotibial ligaments may increase rotatory instability of the knee.30 A recent cadaveric study by Stephen et al39 demonstrated that anterior tibial translation and external rotational laxities were significantly increased after sectioning of the posteromedial meniscocapsular junction (equivalent to a ramp lesion) in an ACL-deficient knee. Moreover, anterior and external rotational instabilities were not restored after ACLR alone but were restored with ACLR combined with posterior meniscocapsular repair.39
Imaging
While MRI is a reliable diagnostic modality for most meniscal pathologies, studies have reported low sensitivity of MRI to detect ramp lesions. Edgar et al13 reported detection of ramp lesions in 33 of 43 patients using MRI, resulting in a sensitivity of 77%. However, a prospective case series by Bollen5 reported 0 of 11 arthroscopically confirmed ramp lesions were detected on MRI. Bollen5 theorized that MRI identification of ramp lesions was limited due to the knee being in near full extension at the moment of the study, which reduces the meniscocapsular separation. This is similar to how a reduced bucket-handle tear may not be detected on MRI.5 In accordance with Bollen5, Liu et al26 concluded that preoperative confirmation of a ramp lesion was difficult, and MRI patient data did not correlate with the diagnosis of a ramp lesion.
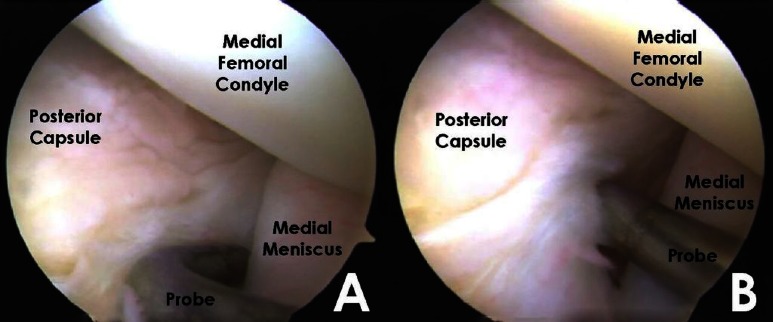
Hash17 reported that the most specific sign of a ramp lesion on MRI was the visualization of a thin fluid signal completely interposed between the posterior horn of the medial meniscus and the posteromedial capsule (Figure 2). When evaluating the medial meniscus it may be difficult to distinguish a meniscocapsular separation from a peripheral vertical tear of the posterior horn, especially when there is incomplete fluid filling adjacent to the peripheral margin of the meniscus, as would be seen with a peripheral vertical tear.17
Figure 2.
Sagittal T2 magnetic resonance image of the medial compartment of a right knee demonstrating subtle separation in the posteromedial meniscocapsular junction consistent with a ramp lesion (yellow arrow).
Hatayama et al18 reported the characteristic MRI finding of ramp lesions to be high signal irregularity of the capsular margin of the medial meniscus posterior horn on T2*-weighted gradient-echo sagittal images. Among all reports, there is a general consensus that arthroscopic evaluation is necessary to completely rule out a ramp lesion.5,17,26,38
Surgical Algorithm
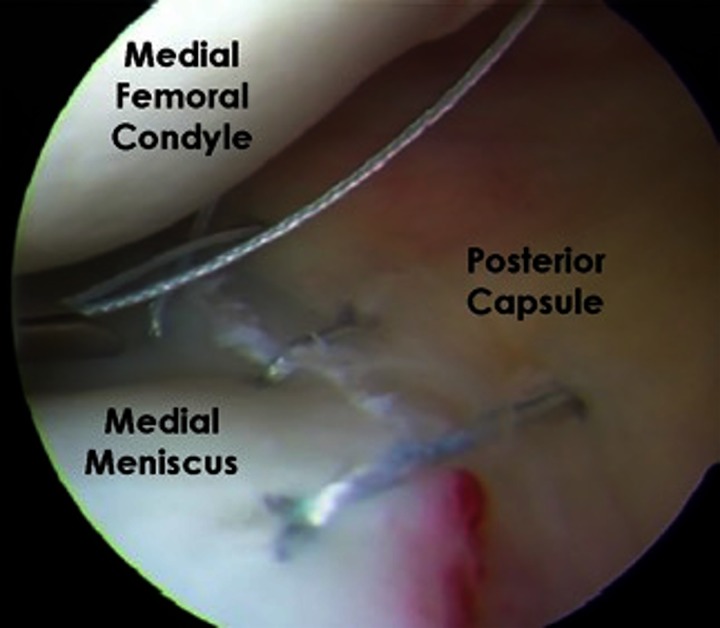
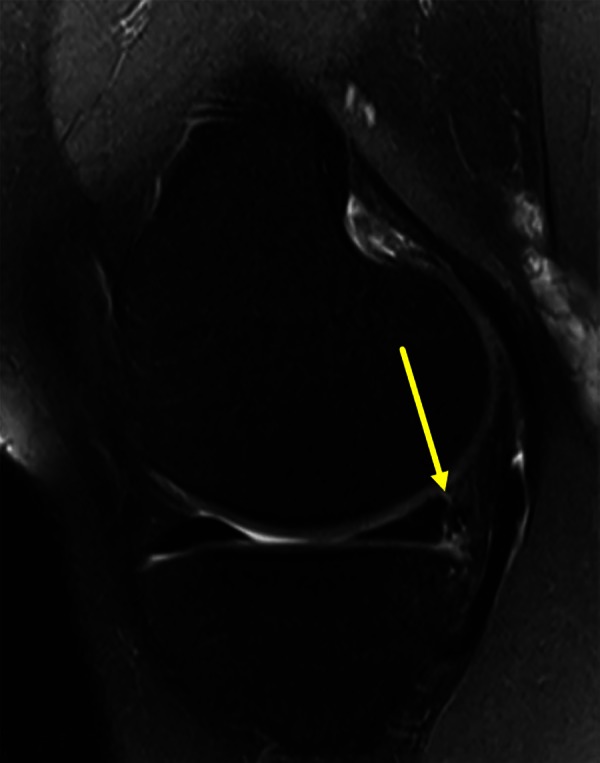
A thorough arthroscopic evaluation is important to identify and treat intra-articular pathology associated with ACL injury. Sonnery-Cottet et al38 reported that among 125 tears of the medial meniscus associated with an ACL rupture, 40% were ramp lesions. Of these, 29 (23.2%) were detected during exploration of the posteromedial compartment through a standard anterior portal, while 21 (16.8%) were not found through the anterior portals and were only discovered by probing the tear through a posteromedial portal after minimal debridement of a superficial soft tissue layer with a motorized shaver. Therefore, they suggested a systematic arthroscopic exploration38 and repair consisting of 4 steps: (1) standard arthroscopic evaluation through the anterolateral portal and probing of the meniscal tissue (Figure 3), (2) exploration of the posteromedial compartment by advancing the arthroscope through the notch and medial to the posterior cruciate ligament (PCL), (3) creation of a viewing posteromedial portal to assess for hidden lesions if necessary, and (4) medial meniscal repair (Figure 4).
Figure 3.
Arthroscopic evaluation of the meniscocapsular junction as viewed through the anteromedial portal with the probe inserted through the anterolateral portal. The scope and probe are passed medial to the posterior cruciate ligament and lateral to the medial femoral condyle. (A) Identification of the meniscocapsular junction with the arthroscopic probe. (B) Dynamic evaluation of the meniscocapsular junction revealing a ramp lesion.
Figure 4.
Inside-out meniscal repair of a meniscal ramp lesion in a left knee. Double-loaded nonabsorbable sutures were placed through the meniscal body and the posteromedial capsule. Sutures were retrieved and tied against the extra-articular aspect of the capsule.
When a ramp lesion is discovered, no clear consensus exists on the appropriate treatment of meniscal ramp lesions. Based on the available literature, there is discrepancy among authors as to the need for surgical intervention to address a ramp lesion in the setting of an acute ACLR. While there is little disagreement that ramp lesions should be repaired in the setting of chronic ACL deficiency,38 some authors suggest that a ramp lesion constitutes a stable tear pattern located in a highly vascular zone with a favorable biological environment to heal, especially in the setting of acute ACLR.26 Furthermore, previous studies have reported reasonable outcomes with similar longitudinal meniscal tear patterns left in situ without repair at the time of ACLR.12,31,35 These studies suggest that nonsurgical management may be reasonable. However, Ahn et al1 hypothesized that during knee flexion and extension, the hypermobility of the detached meniscocapsular structure in ramp lesions is dissimilar from other peripheral tears and would not allow for spontaneous healing. Their study suggests that repairing the lesion would be the most effective approach.
Repair Procedure
As previously mentioned, the available literature suggests that nonsurgical management of ramp lesions may be appropriate. However, when repair is chosen as the treatment option, the anatomic location of a meniscal ramp lesion creates a technical challenge. The posteromedial location of the ramp lesion places the saphenous neurovascular bundle at increased risk when attempting the meniscus repair.32 Therefore, to avoid iatrogenic injury of the saphenous nerve during placement of meniscal fixation devices, needle passing, or suture tying, techniques that allow for direct visualization of the posterior capsule are recommended for ramp lesion repair, and outside-in repair techniques should be undertaken with caution.32
All-inside techniques and inside-out techniques have demonstrated success in the literature to treat this condition.25 Although technically demanding, the inside-out repair technique allows for a greater versatility in suture placement and increased number of sutures, thereby potentially creating a stronger construct.27 For an inside-out repair, a posteromedial approach is performed. An oblique vertical incision is made from approximately the adductor tubercle to the posterior aspect of the tibial plateau. Subcutaneous sharp dissection is performed down to the sartorius fascia, which should be incised as proximal as possible with preservation of the pes anserine tendons. An anatomic “triangle” can be observed at this point. This “triangle” is formed by the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly, and the direct arm of the semimembranosus inferiorly. A retractor is placed in this interval to protect the posterior neurovascular structures during the repair procedure.9
To initiate the ramp lesion repair, an arthroscopic self-delivery gun fitted with a cannula (single or double lumen cannulas) is used to pass double-loaded nonabsorbable sutures into the meniscus in a vertical mattress fashion. To begin passing the sutures, the knee is positioned in 20° to 30° of flexion and the meniscal needle is advanced through the superior or inferior aspect of the posterior horn of the medial meniscus. The corresponding portion of the meniscofemoral or meniscotibial capsule is then penetrated with the second needle of the suture. To help the assistant retrieve the needle, the knee can be flexed to 70° to 90° after the meniscal needle is advanced a few millimeters. The assistant then retrieves the needles through the posteromedial surgical interval, the needles are cut from the sutures, and the suture ends are clamped while maintaining slight tension. The same process is repeated with sutures both in the superior and inferior borders of the posterior horn of the medial meniscus placed between 3 to 5 mm apart. The meniscal sutures are tied with the knee at 90° of flexion, being careful not to overtighten the posteromedial structures.9
A similar procedure can be performed using all-inside devices. The steps of the repair will depend on the device used. Overall, advantages of all-inside sutures include the ease of use, less neurovascular risks, and no additional incisions. However, the all-inside technique is not exempt from complications such as irritation from anchors, meniscal body tears resulting from bigger holes created from device insertion, and implant failure.16
Biological Augmentation
Regardless of the treatment option chosen, improved overall outcomes have been reported for meniscus tears associated with ACL injury that were repaired at the time of ACLR. These findings have been hypothesized to be related to the biological augmentation of the repair from factors in the bone marrow released within the joint.21 Moreover, a recent study reported that the local release of vascular endothelial growth factor (VEGF) and its angiogenetic receptor vascular endothelial growth factor receptor 2 (VEGFR2) were significantly higher after ACLR than after partial meniscectomy, indicating a better vasculogenic potential for enhanced meniscus healing capabilities associated with ACLR tunnel reaming.14 Because of this, it may be reasonable to consider biological augmentation such as the addition of platelet-rich plasma (PRP) or performing a bone marrow stimulation technique by using a pick to create holes into the notch, releasing similar factors as when treating ramp lesions not associated with ACL injury. However, it is unclear whether this is necessary as a ramp lesion has a favorable eccentric and peripheral location in the red-red zone that enhances the biological potential.
Outcomes
There are few short- or long-term outcomes studies after the identification and treatment of ramp lesions. Because of this, treatment recommendations and the decision for surgical or nonsurgical management is based on a limited number of studies. While there are no reported outcomes after nonsurgical treatment, Choi et al10 previously demonstrated that both all-inside and inside-out repair approaches to medial meniscal lesions can provide similar results. Li et al25 specifically reported on 23 ramp lesions treated with an all-inside device with a mean follow-up of 14 months. In their study, the mean Lysholm score improved from 64.4 ± 4.5 preoperatively to 91.2 ± 4.6 postoperatively.25 These studies reinforce aforementioned studies, suggesting that repair can be performed by means of an inside-out repair38 or with all-inside devices25 depending on the surgeon’s preference, as either may provide appropriate outcomes for patients.
Rehabilitation
Currently, there is no universal consensus on the postoperative rehabilitation protocol regarding meniscal ramp lesions. Therefore, general principles of rehabilitation after meniscal repair are typically utilized. Currently, there are no evidence-based protocols available, and therefore, therapy programs should be applied and individualized on a case-by-case basis. Furthermore, when a concomitant knee injury occurs with a meniscal ramp lesion, the rehabilitation will be partially dictated by the concurrent operative procedure.43
Rehabilitation after a ramp lesion repair depends on whether the repair is isolated or performed concurrently with ACLR.3 When performed with an ACLR, the rehabilitation is followed according to the ACL rehabilitation protocol. Weightbearing is initiated as tolerated, and patients may wean off crutches as soon as they can ambulate without a limp. No limits on knee motion are prescribed, and knee motion is increased as tolerated.
Goals for isolated meniscal ramp repair include edema control, knee range of motion, and quadriceps-activation exercises, which are initiated on the first day postoperatively.19 Primarily, the focus is to prevent excessive weightbearing and joint compressive forces that could lead to undue traction and shearing stress, resulting in disruption of meniscal healing.19,33 Stress is believed to increase 10-fold during knee flexion exceeding 90°. Therefore, it is recommended to restrict passive flexion to 90° for the first 2 weeks postoperatively and to avoid all active flexion.33 The medial meniscus has been shown to be highly mobile during knee rotation in the first 30° of flexion; therefore, patients with ramp lesions should avoid knee rotation during the first 3 postoperative weeks.42 Pivot and contact activities, as well as squatting and lifting exercises involving maximum knee flexion while weightbearing, should not be performed for at least 4 to 6 months.33
Patients who have repairs of peripheral meniscus tears, such as ramp lesions, are generally progressed more rapidly than those who have repairs of tears extending in the central one-third region or those who undergo meniscal transplantation.19 Most authors agree that patients can return to sports or strenuous activities when the clinical examination reveals a nontender joint line, absence of pain and effusion, restored muscle strength, and full range of motion, particularly full extension.34,45
Conclusion
Ramp lesions constitute a common but often missed entity in ACL-deficient knees, both in an acute and chronic setting. Biomechanical studies have reported that a ramp lesion produces significant anterior tibial translation and external rotational instability in ACL-deficient knees that is not reestablished with an isolated ACLR but with a concomitant meniscal repair. MRIs have been reported to have low sensitivity to detect ramp lesions; therefore, a systematic arthroscopic algorithm should be utilized to fully identify these lesions. If present, it is highly recommended to repair these lesions to avoid the previously mentioned unwanted biomechanical consequences. In cases of isolated ramp lesions, a standard meniscal repair rehabilitation protocol should be followed. However, when a concomitant ACLR is performed, the rehabilitation should follow the designated ACLR postoperative protocol. Meniscal ramp tears are more common than previously thought; as a result, it is important to be vigilant regarding the high prevalence of these lesions, especially in the setting of an ACL tear.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.F.L. is a consultant for and receives royalties from Arthrex, Ossur, and Smith & Nephew.
References
- 1. Ahn JH, Wang JH, Yoo JC. Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament–deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy. 2004;20:936–945. [DOI] [PubMed] [Google Scholar]
- 2. Allen AA, Caldwell GL, Jr, Fu FH. Anatomy and biomechanics of the meniscus. Oper Tech Orthop. 1995;5:2–9. [Google Scholar]
- 3. Barber FA, Click SD. Meniscus repair rehabilitation with concurrent anterior cruciate reconstruction. Arthroscopy. 1997;13:433–437. [DOI] [PubMed] [Google Scholar]
- 4. Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41:1801–1807. [DOI] [PubMed] [Google Scholar]
- 5. Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br. 2010;92:222–223. [DOI] [PubMed] [Google Scholar]
- 6. Bonnin M, Carret JP, Dimnet J, Dejour H. The weight-bearing knee after anterior cruciate ligament rupture. An in vitro biomechanical study. Knee Surg Sports Traumatol Arthrosc. 1996;3:245–251. [DOI] [PubMed] [Google Scholar]
- 7. Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39:1889–1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62:259–270. [PubMed] [Google Scholar]
- 9. Chahla J, Serra Cruz R, Cram TR, Dean SC, LaPrade RF. Inside-out meniscal repair: medial and lateral approach. Arthrosc Tech. 2016;5:e163–e168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: inside-out versus all-inside repair. Am J Sports Med. 2009;37:2144–2150. [DOI] [PubMed] [Google Scholar]
- 11. Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983;65:538–547. [PubMed] [Google Scholar]
- 12. Duchman KR, Westermann RW, Spindler KP, et al. The fate of meniscus tears left in situ at the time of anterior cruciate ligament reconstruction: a 6-year follow-up study from the MOON cohort. Am J Sports Med. 2015;43:2688–2695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Edgar C, Ware J, Obopilwe E, Ziegler C, Reed D, Arciero RA. Posteromedial meniscocapsular tear: prevalence, detection sensitivity, biomechanics, and repair technique. http://aaos2015.conferencespot.org/58906-aaos-1.1965581/t004-1.1971711/f004-1.1971712/a096-1.1971713/se81-1.1971728#tab_0=0. Accessed June 13, 2016.
- 14. Galliera E, De Girolamo L, Randelli P, et al. High articular levels of the angiogenetic factors VEGF and VEGF-receptor 2 as tissue healing biomarkers after single bundle anterior cruciate ligament reconstruction. J Biol Regul Homeost Agents. 2011;25:85–91. [PubMed] [Google Scholar]
- 15. Gardner EJ, Noyes FR, Jetter AW, Grood ES, Harms SP, Levy MS. Effect of anteromedial and posterolateral anterior cruciate ligament bundles on resisting medial and lateral tibiofemoral compartment subluxations. Arthroscopy. 2015;31:901–910. [DOI] [PubMed] [Google Scholar]
- 16. Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40:459–468. [DOI] [PubMed] [Google Scholar]
- 17. Hash TW., 2nd Magnetic resonance imaging of the knee. Sports Health. 2013;5:78–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hatayama K, Kimura M, Ogoshi A, Takagishi K. Ramp lesion associated with anterior cruciate ligament rupture. https://www.isakos.com/meetings/2013congress/onsite/AbstractView?EventID=7751. Accessed June 13, 2016.
- 19. Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports Phys Ther. 2006;36:795–814. [DOI] [PubMed] [Google Scholar]
- 20. Hughston JC, Eilers AF. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55:923–940. [PubMed] [Google Scholar]
- 21. Hutchinson ID, Moran CJ, Potter HG, Warren RF, Rodeo SA. Restoration of the meniscus: form and function. Am J Sports Med. 2014;42:987–998. [DOI] [PubMed] [Google Scholar]
- 22. Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. [DOI] [PubMed] [Google Scholar]
- 23. Keene GC, Bickerstaff D, Rae PJ, Paterson RS. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med. 1993;21:672–679. [DOI] [PubMed] [Google Scholar]
- 24. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. [DOI] [PubMed] [Google Scholar]
- 25. Li WP, Chen Z, Song B, Yang R, Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27:56–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–837. [DOI] [PubMed] [Google Scholar]
- 27. Nelson CG, Bonner KF. Inside-out meniscus repair. Arthrosc Tech. 2013;2:e453–e460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Noyes FR, Jetter AW, Grood ES, Harms SP, Gardner EJ, Levy MS. Anterior cruciate ligament function in providing rotational stability assessed by medial and lateral tibiofemoral compartment translations and subluxations. Am J Sports Med. 2015;43:683–692. [DOI] [PubMed] [Google Scholar]
- 29. Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29:226–231. [DOI] [PubMed] [Google Scholar]
- 30. Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:2967–2973. [DOI] [PubMed] [Google Scholar]
- 31. Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17:396–401. [DOI] [PubMed] [Google Scholar]
- 32. Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206. [PubMed] [Google Scholar]
- 33. Seil R, VanGiffen N, Pape D. Thirty years of arthroscopic meniscal suture: what’s left to be done? Orthop Traumatol Surg Res. 2009;95(suppl 1):S85–S96. [DOI] [PubMed] [Google Scholar]
- 34. Sgaglione NA, Steadman JR, Shaffer B, Miller MD, Fu FH. Current concepts in meniscus surgery: resection to replacement. Arthroscopy. 2003;19(suppl 1):161–188. [DOI] [PubMed] [Google Scholar]
- 35. Shelbourne KD, Rask BP. The sequelae of salvaged nondegenerative peripheral vertical medial meniscus tears with anterior cruciate ligament reconstruction. Arthroscopy. 2001;17:270–274. [DOI] [PubMed] [Google Scholar]
- 36. Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am. 1986;68:71–79. [PubMed] [Google Scholar]
- 37. Smith JP, 3rd, Barrett GR. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med. 2001;29:415–419. [DOI] [PubMed] [Google Scholar]
- 38. Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921–926. [DOI] [PubMed] [Google Scholar]
- 39. Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400–408. [DOI] [PubMed] [Google Scholar]
- 40. Strobel M. Manual of Arthroscopic Surgery. New York, NY: Springer; 1988. [Google Scholar]
- 41. Strobel MJ. Manual of Arthroscopic Surgery. Berlin, Germany: Springer; 2013. [Google Scholar]
- 42. Tienen TG, Buma P, Scholten JG, van Kampen A, Veth RP, Verdonschot N. Displacement of the medial meniscus within the passive motion characteristics of the human knee joint: an RSA study in human cadaver knees. Knee Surg Sports Traumatol Arthrosc. 2005;13:287–292. [DOI] [PubMed] [Google Scholar]
- 43. VanderHave KL, Perkins C, Le M. Weightbearing versus nonweightbearing after meniscus repair. Sports Health. 2015;7:399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37–41. [DOI] [PubMed] [Google Scholar]
- 45. Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res. 2014;26:68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]