Abstract
Background:
Displaced fractures of the distal clavicle are inherently unstable and lead to nonunion in a high percentage of cases. The optimal surgical management remains controversial.
Hypothesis:
Indirect osteosynthesis with a closed-loop double endobutton construct would result in reliable fracture union and obviate the need for additional surgery.
Study Design:
Case series; Level of evidence, 4.
Methods:
Eight patients with an acute unstable Neer type IIB distal clavicle fracture were treated with a closed-loop double endobutton implant. Mean follow-up averaged 3.4 years (range, 1-9 years). Two patients were lost to follow-up. The remaining 6 patients underwent a detailed functional and radiologic evaluation.
Results:
Definitive fracture healing was achieved in all patients. There were no complications, and no patients required additional surgery related to the index procedure. The mean Constant score was 97 at final follow-up.
Conclusion:
The closed-loop double endobutton technique was reliable and effective in achieving fracture union in all patients with unstable Neer type IIB fractures of the distal clavicle. This technique obviates the need for late hardware removal that is often necessary when direct osteosynthesis is used and avoids potential complications associated with coracoclavicular cerclage constructs that require knot fixation.
Keywords: clavicle, coracoclavicular, distal clavicle fracture, Neer type II, cortical button
Fractures of the clavicle are a common clinical problem, with an incidence of approximately 200,000 cases per year nationally. Twenty-one percent of these cases involve the distal third of the clavicle, lateral to the attachments of the coracoclavicular (CC) ligaments.45 The majority of these cases can be successfully managed nonoperatively.4 However, 1 specific subtype, the Neer type IIB, poses a more challenging problem. The Neer IIB pattern comprises a fracture between the CC ligaments with complete rupture of the conoid ligament.43 These fractures can be significantly displaced as a result of strong deforming forces—the trapezius muscle pulling the medial fragment superiorly and posteriorly and the weight of the arm on the shoulder girdle pulling the distal fragment inferiorly and anteriorly. Consequently, nonunion is common, with rates reported between 25% and 44% with nonoperative management.12,43,46,50–52 In addition, while nonsurgical treatment may ultimately result in acceptable outcomes in many patients, the recovery period can be prolonged and return to function delayed.44 As a result, a significant number of patients initially managed nonoperatively seek delayed surgical treatment. Acute surgical management of the Neer IIB fracture is therefore an attractive alternative that has been advocated by Neer43 and other authors.12,15,46,47
Currently, there is no consensus concerning the optimal surgical approach for managing unstable type IIB fractures of the distal clavicle. Although various techniques have been described, they fall into 1 of 2 general categories: either direct osteosynthesis with plate or wire fixation or indirect stabilization of the CC interval with suture, screw, or cable fixation. The latter functions by neutralizing the deforming forces on the fracture and effectively converting an unstable type IIB to a stable type I pattern, thereby permitting secondary fracture healing to occur without direct fixation. Recent meta-analyses demonstrate that modern techniques, regardless of approach or fixation construct, achieve fracture union 97% to 100% of the time.47,56 However, morbidity varies widely between techniques. The hook plate construct has been associated with high complication rates.47,56 Direct osteosynthesis with standard plating techniques is challenging and often impossible due to distal fragment size and/or comminution. Furthermore, fixation with plate and screw constructs may require a second operation to treat or avoid late hardware-associated complications. In contrast, indirect techniques relying on CC stabilization circumvent the need for a second operation. In 1990, Neer42 described a technique using CC cerclage for indirect fixation of unstable distal clavicle fractures. Since then, several authors have described variations of this technique employing different constructs to achieve high union rates with low complication and reoperation rates.7,8,19,34,37,48,49,53–55,61
The current study presents a novel technique for fixation of unstable type IIB distal clavicle fractures based on the original indirect CC stabilization technique described by Neer. The technique has been adapted from the closed-loop double endobutton reconstruction initially described for management of acromioclavicular (AC) joint dislocations.57 The technique has been demonstrated to have excellent clinical outcomes,58 while the fixation construct has been validated in biomechanical studies.20 The current study evaluates the clinical and radiographic outcomes of the closed-loop double endobutton technique for the repair of acute unstable distal clavicle fractures. We hypothesized that the technique would achieve high rates of fracture union with low complication rates by avoiding knot slippage and abrasion as well as obviating the need for secondary procedures to remove hardware.
Methods
After approval from our institutional review board, all patients undergoing surgical treatment by the senior author (S.S.) for acute Neer type IIB fractures of the distal clavicle between November 2004 and July 2014 were identified. Patients with fractures more than 4 weeks old were excluded.
Demographics
During the study period, 8 consecutive open reduction and internal fixation (ORIF) procedures with the closed-loop double endobutton technique were performed in 8 patients: 5 (63%) males and 3 (37%) females. At the time of surgery, the mean age was 43 years (range, 20-67 years). The mean time from injury to surgery spanned 14 days (range, 6-27 days). Five patients (63%) were right-handed and 3 (37%) were left-handed. The dominant arm was injured in 6 patients (75%). The reported mechanism of injury was acute trauma in all cases, including a motor vehicle accident in 2 patients (25%), pedestrian struck by a motor vehicle in 2 patients (25%), bicycle injury in 2 patients (25%), skiing injury in 1 patient (12%), and falling down stairs in 1 patient (12%). One patient had an associated distal ulna fracture. Mean body mass index (BMI) was 26.0 kg/m2 (range, 21.5-37.1 kg/m2). Patients were otherwise healthy at the time of surgery. Only 1 patient had an Elixhauser comorbidity (diabetes mellitus). Insurance was private for 4 patients (50%) and no fault for 4 patients (50%). There were no workers’ compensation cases.
Surgery
All patients underwent the same ORIF procedure utilizing the continuous loop double endobutton technique previously described for AC joint reconstruction.57 Arthroscopy was not included in the procedure. In all cases, the double endobutton construct was further enhanced by additional suture fixation of fracture fragments (see the Video Supplement).
A deltoid-splitting incision was used to expose the coracoid surface and provide access to the fracture site. The deltotrapezial fascia was incised, and the fracture fully exposed and anatomically reduced. With the fracture reduced, a 2.4-mm drill hole was made into the top of the clavicle midway between the anterior and posterior border and directly in line with the base of the coracoid. After drilling through the coracoid, it was reamed over with a 4.5-mm cannulated reamer. A second 2.5-mm drill hole was placed in the clavicle 1 cm lateral to the central drill hole. Loop length was determined with the clavicle anatomically reduced by measuring the channel length from the superior surface of the clavicle to the inferior surface of the coracoid with a depth gauge. The continuous loop comes in 5-mm increments. If the measured distance was within 1 mm of the standard loop size, a regular endobutton (EndoButton; Smith & Nephew) was used on the cortical surface of the clavicle. If the measured length was more than 1 mm longer than a standard loop size, the next larger continuous loop size was chosen and excess loop filled with a thicker button (Xtendobutton; Smith & Nephew) to ensure reduction to within 1 mm of the measured channel. Two No. 5 braided polyethylene sutures (Ethibond; Ethicon) were placed into the endobutton and 1 placed into the loop. The endobutton was pushed through the drill holes and deployed. With the joint held reduced, the loop stitch was pulled up until only the tip protruded from the clavicular hole and a free endobutton was slid into the loop and stabilized by passing the 2 free suture limbs into the holes of the implant on either side of the loop and tied, securing the button (Figure 1). The “trapezoid” stitch was then placed by passing 1 limb from the other No. 5 braided polyethylene suture into the second drill hole and tying, completing the repair. Once the reconstruction was complete, attention was turned back to the fracture site. The reduction was again assessed, and, if necessary, additional sutures were placed across the fracture site to gain additional stability and fracture apposition.
Figure 1.
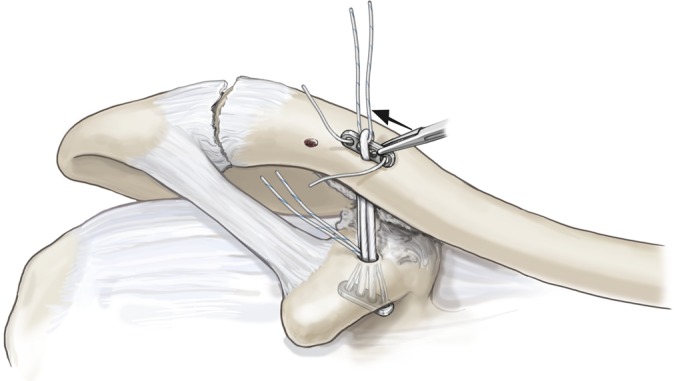
Illustration of the double endobutton construct demonstrating placement of the second endobutton under the continuous loop on the superior surface of the clavicle. Note that the fracture is anatomically reduced at this step.
Postoperative Treatment
Patients were placed in a sling for 4 weeks. Passive external rotation with the arm at the side was encouraged, and pendulum exercises began at 2 weeks. At 4 weeks, the sling was discontinued and active movement of the shoulder was encouraged. Full return to activity and/or sports was allowed at 4 to 6 months depending on progress.
Clinical Follow-up
A comprehensive clinical evaluation, including a detailed patient interview and physical examination, was performed by the same physician who was not the surgeon. Range of motion was measured with use of a goniometer. Multiple validated outcome measures, including the modified University of California at Los Angeles (UCLA) shoulder scale,13 American Shoulder and Elbow Society (ASES) score,29 Simple Shoulder Test (SST),35 and Constant score,10 were collected. Objective strength was measured for the Constant score with a digital spring scale as originally described by Constant and Murley and in accordance with the updated guidelines by Constant et al.11 The final Constant score was normalized by age and sex.28 Failure was defined as reoperation or revision for any reason.
Radiographic Follow-up
Postoperative radiographs of the injured shoulder, consisting of anteroposterior and axillary lateral views, were obtained. Ipsilateral and contralateral Zanca views of the clavicle and AC joint, taken with a 10° to 15° cephalic tilt, were also obtained for comparison. Fractures were assessed for radiographic union or nonunion. Nonunion was defined based on Neer’s original description as “lack of bone bridging for more than 12 months after injury.”43
Statistical Analysis
No statistical analysis was necessary to compare outcome data. Results are expressed as the mean ± standard deviation (SD) unless otherwise specified.
Results
Clinical Outcomes
Follow-up was obtained on 6 of the 8 patients (75%) at a mean 3.4 years (range, 1-9 years). Two patients (25%) were unreachable and lost to follow-up. Mean functional outcomes scores are reported in Table 1. All patients were satisfied with the results and agreed that they would choose to undergo the procedure again. Five of 6 patients had excellent results at final follow-up. The patient without excellent functional results was found to have a symptomatic ipsilateral partial rotator cuff tear and underwent arthroscopic rotator cuff debridement and repair 9 months after the initial procedure and 19 months prior to final follow-up. Excluding this patient from data analysis reveals a mean raw Constant score of 97 and normalized Constant score of 99.
TABLE 1.
Functional Outcome Scores After Closed-Loop Double Endobutton Repair of Unstable Distal Clavicle Fracturesa
| Scoring System | Score |
|---|---|
| UCLA | 32.5 ± 3.7 |
| ASES | 92.5 ± 15.4 |
| SST | 11.2 ± 1.6 |
| Constant | |
| Raw | 93.2 ± 10.1 |
| Normalized | 95.6 ± 8.4 |
aResults reported as mean ± SD. ASES, American Shoulder and Elbow Society; SST, Simple Shoulder Test; UCLA, University of California, Los Angeles.
Radiographic Outcomes
At a minimum 1-year follow-up, all patients had achieved radiographic union. There were no cases of nonunion or osteolysis. Radiographs and computed tomography scan images demonstrating fracture union are displayed in Figures 2 and 3. There were no hardware-associated complications, including breakage or fracture, detected on follow-up radiographs.
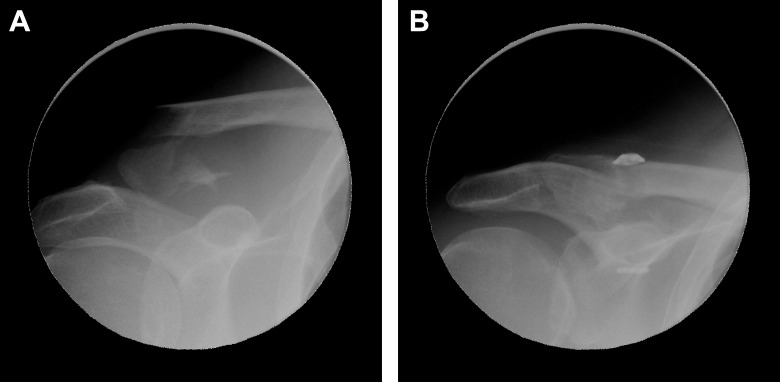
Figure 2.
(A) Preoperative and (B) postoperative radiographs of an unstable type IIB distal clavicle fracture. The postoperative radiograph was obtained 2 years after coracoclavicular stabilization using the double endobutton continuous loop construct and demonstrates fracture union.
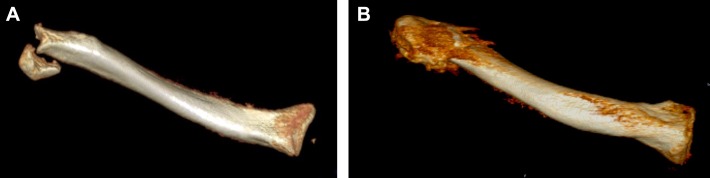
Figure 3.
Three-dimensional computed tomography reconstruction of an unstable type IIB distal clavicle fracture obtained (A) preoperatively and (B) 2 years postoperatively demonstrating fracture union.
Complications
During the follow-up period, 1 patient had temporary wound breakdown, which resolved with local wound care. No surgical site infections or perioperative fractures were observed. No patients complained of hardware irritation or prominence. There were no cases of reoperation or revision.
Discussion
The clinical results of this limited series of patients validate the use of the closed loop double endobutton for type IIB distal clavicle fractures. Fracture union was obtained in all cases, and there were no complications or second operations. Excellent clinical results were obtained in 5 cases. Good results observed in 1 case were likely the result of concomitant rotator cuff injury requiring surgical repair.
Traditionally, unstable distal clavicle fractures were treated surgically with direct osteosynthesis. Early techniques utilized transacromial Kirschner wires, which were associated with high rates of hardware-related complications.30,33 In addition, transarticular fixation with pins spanning the AC joint resulted in postoperative arthritis of the AC joint.15 The hook plate was later introduced as an alternative to Kirschner wire fixation. In 2002, Flinkkila et al17 found that although union rates were similar to traditional Kirschner wire fixation techniques (88% for hook plate vs 91% for Kirschner wire fixation), complication rates were dramatically less with the hook plate (6% vs 55%).17 Subsequent studies confirmed excellent union rates from 95% to 100% but also reported complication rates of 8% to 18%.18,21,27,41 Painful subacromial impingement frequently occurs with hook plates, reported in 68% of patients. In addition, implant migration is common, leading most authors to recommend routine removal of the hook plate in all patients once fracture healing is confirmed.9
Direct osteosynthesis of the distal clavicle using a locking distal radius plate has been described as an alternative to the hook plate. Specialized plates that allow multiple locking screws to be placed in the small distal clavicle fragment have been shown to have excellent union rates while avoiding trauma to the AC joint and acromion.2,26,32,60 Despite these excellent results, the need for additional surgery remains, as plate removal is required in 40% to 53% of cases.31,38 Furthermore, this technique may not be feasible in all cases. Comminution may prevent adequate purchase or fixation of the distal fragment. Largo et al31 recommended the use of CC augmentation to address the problem of a small and/or comminuted distal fragment. Reduction of the proximal clavicle limits the high shearing forces at the fracture site. A PDS (polydioxansulfate) cable was placed through a drill hole in the coracoid and then looped over the clavicle and tied. Early union was achieved in 19 of 20 cases, with 1 case of delayed healing. Hardware removal was performed in 53% of cases, and 1 patient required additional surgery for plate breakage. The authors concluded that the CC augmentation was an important component in ensuring the success of the procedure.31 More recently, Hohmann et al22 reported on using a suture button device in conjunction with a distal radius locking plate and achieved early union in 30 of 31 patients.
The alternative to direct osteosynthesis is CC stabilization as a stand-alone procedure without the use of plate fixation. With this approach, rigid fracture fixation is not achieved. Rather, fracture fragments are reduced and indirectly stabilized thereby converting the unstable Neer type IIB pattern into a stable type I pattern. Once stabilized in this manner, secondary fracture healing can be expected to proceed uneventfully. This approach has a number of advantages relative to traditional osteosynthesis. Surgical dissection is minimized as the exposure is limited to only the fracture site and the base of the coracoid. In our experience, reoperation for hardware removal has not been needed. In the event of a nonunion, the associated complications of hardware pullout or breakage are avoided. Bishop et al, in a recent biomechanical study, showed that fixation failure with a plate construct was more likely to result in the need for additional surgery than failure of a suture-only construct.6
Neer42 first described the technique of CC stabilization using braided polyethylene suture as a definitive surgical procedure in 1990. Since then, numerous authors, beginning with Goldberg et al19 in 1997, have reported the results of CC stabilization as a stand-alone procedure for unstable type IIB fractures.7,8,34,37,48,49,55,61 The cerclage materials vary and include a range of suture materials, composed of polyethylene, polyglactin, polydioxanone, and combinations thereof. In most techniques, the cerclage material is looped under the coracoid and around the clavicle and then tied, although some modify this by passing the material through a drill hole in the clavicle. Using these techniques, fracture union was achieved in 93% to 100% of cases, with more than half of the studies reporting perfect union rates. Only 4 patients of the nearly 200 total cases required reoperation, 3 of which were for complications related to the knot in the suture material. Only 1 patient required additional surgery for nonunion.55 CC stabilization utilizing a CC screw has been reported by several authors, and while union rates were nearly 100% in 4 separate studies, the need for a second operation for hardware removal was not eliminated.3,25,36,62 When utilized for distal clavicle fractures, screw loosening and loss of reduction has also been described.14,25 Furthermore, the use of screw fixation for AC joint dislocations has been complicated by iatrogenic clavicle and coracoid fracture.39
Because of the infrequency of this particular fracture, most clinical series are relatively small case series. This problem has been addressed by 2 recent meta-analyses.47,56 Oh et al47 pooled the results from 21 different studies, including 365 surgical cases. Healing rates were uniformly high, with 98.4% of all surgically treated cases achieving fracture union. Complication rates varied widely between methods, however, with the hook plate showing a 41% complication rate compared with a 4.8% rate for CC stabilization. The authors concluded that CC stabilization was preferable.47 These results were echoed by the meta-analysis by Stegeman et al56 in 2013, which included 350 surgical cases from 21 studies. These authors reported a fracture union rate of 98% and found similar differences in complication rates, with the hook-plate demonstrating a 24-fold increased risk of complications compared with suture-based methods. They concluded that the hook-plate should be avoided as a treatment for this fracture.56
Although the results of the many different studies using coracoclavicular stabilization have shown high union rates and very low reoperation rates, a true gold standard technique has not been established, as many of the techniques are prone to suture-based complications. Braided polyethylene fiber sutures have been associated with wound problems from prominent knots and bone abrasion from suture material.16,40 Partial loss of reduction during the healing process has been observed, and nonunions, while uncommon, still occur.
CC stabilization procedures for type IIB distal clavicle fractures using standard suture button configurations that require knot fixation have been reported by others. While union rates and clinical results have been excellent, complications of fracture slippage and nonunion have been reported.16,59
The continuous-loop double endobutton technique was designed to address these shortcomings. In this small series of 6 cases, the technique was successful in achieving reliable fracture union without complications. The use of the continuous loop eliminates any of the knot-related complications of wound issues, breakage, or slippage that have been reported with other techniques. This technique has also been applied to both acute and chronic AC joint dislocations with excellent clinical and radiographic results.58 The use of the secondary “trapezoid” stitch provides valuable biplanar stability, as shown by Grantham et al20 in a recent biomechanical study, and may contribute to better fracture stability, thereby reducing the chance of delayed union or nonunion. Finally, by placing the device through drill holes close to the anatomic attachments of the CC ligament, 2 additional potential problems are minimized. First, passing cerclage material into rather than under the coracoid prevents anterior overreduction of the clavicle. Second, materials that loop either around or through the clavicle have been shown to abrade and ultimately erode through bone, predisposing to late fractures.24
The mechanical properties of the continuous endobutton loop are ideally suited for stabilizing the coracoclavicular interval. The loop has similar stiffness (142 N) and more than double the strength (1063 N) of the native ligament.23 Perhaps more important, the loop is particularly resistant to creep under cyclical load, demonstrating only a 1.3-mm change in length with cyclic loading of up to 250 N at 4500 cycles.5 In a study by Barrow et al,5 both the knotted constructs and the self-locking loops had clinical failure (defined as 3-mm elongation) well before 5000 cycles (1349 and 1680 cycles, respectively). In a study by Abbi et al,1 constructs with knots also demonstrated the potential to either slip or fail when subjected to cyclical loads. Ultrahigh–molecular weight polyethylene (UHMWPE) braided sutures, in particular, have frictional properties that lead to slippage at loads significantly below their failure threshold. Ilahi et al23 also demonstrated that braided UHMWPE fiber suture tied with 5 square knots exhibited 3 mm of slippage at only 60% of the ultimate failure load.
Unfortunately, we are not able to draw conclusions about which characteristics of the study population are associated with superior outcomes with the double endobutton technique versus other strategies. The sample size is too small to meaningfully stratify into different subsets and achieve statistical significance. In theory, distal clavicle fractures with significant distal comminution are challenging to treat with direct osteosynthesis and would be more amenable to CC ligament fixation reconstruction with the double endobutton technique. There are no absolute contraindications to the double endobutton technique. One relative contraindication may be a distal clavicle fracture with medial extension that would interfere with clavicle drill hole placement. Another potential contraindication would be a concomitant coracoid fracture that precludes coracoid fixation. Finally, a low-demand or high–surgical risk patient may be better treated nonoperatively.
The current study was not without limitations. This was a retrospective study with prospective follow-up and thus suffers from potential selection bias. Results were uniformly promising; however, the small sample size prevents multivariate analysis. There was no control group or comparative arms, so conclusions related to other treatment strategies cannot be definitively drawn. Midterm follow-up was obtained in all cases, but outcomes at long-term follow-up remain to be seen.
Conclusion
In this series of patients, the use of the continuous-loop double endobutton resulted in consistent results and no complications. Further study with larger case numbers is warranted.
Supplementary Material
Footnotes
A Video Supplement for this article is available at http://ojsm.sagepub.com/supplemental.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Abbi G, Espinoza L, Odell T, Mahar A, Pedowitz R. Evaluation of 5 knots and 2 suture materials for arthroscopic rotator cuff repair: very strong sutures can still slip. Arthroscopy. 2006;22:38–43. [DOI] [PubMed] [Google Scholar]
- 2. Andersen JR, Willis MP, Nelson R, Mighell MA. Precontoured superior locked plating of distal clavicle fractures: a new strategy. Clin Orthop Relat Res. 2011;469:3344–3350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ballmer F, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br. 1991;73:291–294. [DOI] [PubMed] [Google Scholar]
- 4. Banerjee R, Waterman B, Padalecki J, Robertson W. Management of distal clavicle fractures. J Am Acad Orthop Surg. 2011;19:392–401. [DOI] [PubMed] [Google Scholar]
- 5. Barrow AE, Pilia M, Guda T, Kadrmas WR, Burns TC. Femoral suspension devices for anterior cruciate ligament reconstruction: do adjustable loops lengthen? Am J Sports Med. 2014;42:343–349. [DOI] [PubMed] [Google Scholar]
- 6. Bishop JY, Roesch M, Lewis B, Jones GL, Litsky AS. A biomechanical comparison of distal clavicle fracture reconstructive techniques. Am J Orthop (Belle Mead NJ). 2013;42:114–118. [PubMed] [Google Scholar]
- 7. Checchia SL, Doneux PS, Miyazaki AN, Fregoneze M, Silva LA. Treatment of distal clavicle fractures using an arthroscopic technique. J Shoulder Elbow Surg. 2008;17:395–398. [DOI] [PubMed] [Google Scholar]
- 8. Chen C-H, Chen W-J, Shih C-H. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma Acute Care Surg. 2002;52:72–78. [DOI] [PubMed] [Google Scholar]
- 9. Chen CY, Yang SW, Lin KY, et al. Comparison of single coracoclavicular suture fixation and hook plate for the treatment of acute unstable distal clavicle fractures. J Orthop Surg Res. 2014;9:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Constant C, Murley A. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 11. Constant CR, Gerber C, Emery RJ, Søjbjerg JO, Gohlke F, Boileau P. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17:355–361. [DOI] [PubMed] [Google Scholar]
- 12. Edwards D, Kavanagh T, Flannery M. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23:44–46. [DOI] [PubMed] [Google Scholar]
- 13. Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68:1136–1144. [PubMed] [Google Scholar]
- 14. Esenyel CZ, Ceylan HH, Ayanoglu S, Kebudi A, Adanir O, Bulbul M. Treatment of Neer Type 2 fractures of the distal clavicle with coracoclavicular screw. Acta Orthop Traumatol Turc. 2011;45:291–296. [DOI] [PubMed] [Google Scholar]
- 15. Eskola A, Vainionpaa S, Korkala O, Rokkanen P. Acute complete acromioclavicular dislocation. A prospective randomized trial of fixation with smooth or threaded Kirschner wires or cortical screw. Ann Chir Gynaecol. 1987;76:323–326. [PubMed] [Google Scholar]
- 16. Flinkkilä T, Heikkilä A, Sirniö K, Pakarinen H. TightRope versus clavicular hook plate fixation for unstable distal clavicular fractures. Eur J Orthop Surg Traumatol. 2014;25:465–469. [DOI] [PubMed] [Google Scholar]
- 17. Flinkkila T, Ristiniemi J, Hyvonen P, Hamalainen M. Surgical treatment of unstable fractures of the distal clavicle: a comparative study of Kirschner wire and clavicular hook plate fixation. Acta Orthop Scand. 2002;73:50–53. [DOI] [PubMed] [Google Scholar]
- 18. Flinkkila T, Ristiniemi J, Lakovaara M, Hyvonen P, Leppilahti J. Hook-plate fixation of unstable lateral clavicle fractures: a report on 63 patients. Acta Orthop. 2006;77:644–649. [DOI] [PubMed] [Google Scholar]
- 19. Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg. 1997;6:380–382. [DOI] [PubMed] [Google Scholar]
- 20. Grantham C, Heckmann N, Wang L, Tibone JE, Struhl S, Lee TQ. A biomechanical assessment of a novel double endobutton technique versus a coracoid cerclage sling for acromioclavicular and coracoclavicular injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24:1918–1924. [DOI] [PubMed] [Google Scholar]
- 21. Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. [DOI] [PubMed] [Google Scholar]
- 22. Hohmann E, Hansen T, Tetsworth K. Treatment of Neer type II fractures of the lateral clavicle using distal radius locking plates combined with TightRope augmentation of the coraco-clavicular ligaments. Arch Orthop Trauma Surg. 2012;132:1415–1421. [DOI] [PubMed] [Google Scholar]
- 23. Ilahi OA, Younas SA, Ho DM, Noble PC. Security of knots tied with ethibond, fiberwire, orthocord, or ultrabraid. Am J Sports Med. 2008;36:2407–2414. [DOI] [PubMed] [Google Scholar]
- 24. Jerosch J, Filler T, Peuker E, Greig M, Siewering U. Which stabilization technique corrects anatomy best in patients with AC-separation? An experimental study. Knee Surg Sports Traumatol Arthrosc. 1999;7:365–372. [DOI] [PubMed] [Google Scholar]
- 25. Jin CZ, Kim H-K, Min B-H. Surgical treatment for distal clavicle fracture associated with coracoclavicular ligament rupture using a cannulated screw fixation technique. J Trauma. 2006;60:1358–1361. [DOI] [PubMed] [Google Scholar]
- 26. Kalamaras M, Cutbush K, Robinson M. A method for internal fixation of unstable distal clavicle fractures: early observations using a new technique. J Shoulder Elbow Surg. 2008;17:60–62. [DOI] [PubMed] [Google Scholar]
- 27. Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–164. [DOI] [PubMed] [Google Scholar]
- 28. Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14:279–285. [DOI] [PubMed] [Google Scholar]
- 29. King GJ, Richards RR, Zuckerman JD, et al. A standardized method for assessment of elbow function. Research Committee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999;8:351–354. [DOI] [PubMed] [Google Scholar]
- 30. Kona J, Bosse MJ, Staeheli JW, Rosseau RL. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4:115–120. [DOI] [PubMed] [Google Scholar]
- 31. Largo RD, Rudin MA, Hotz TK, Valderrabano V, Käch KK. Anatomic reconstruction of unstable lateral clavicular fractures. J Trauma Acute Care Surg. 2011;71:1348–1351. [DOI] [PubMed] [Google Scholar]
- 32. Lee SK, Lee JW, Song DG, Choy WS. Precontoured locking plate fixation for displaced lateral clavicle fractures. Orthopedics. 2013;36:801–807. [DOI] [PubMed] [Google Scholar]
- 33. Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33:1401–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li Y, Shi S, Ou-Yang Y-P, Liu T-L. Minimally invasive treatment for Neer IIb distal clavicle fractures with titanium cable. J Trauma Acute Care Surg. 2011;71:E37–E40. [DOI] [PubMed] [Google Scholar]
- 35. Lippitt S, Harryman D, Matsen F, Fu F, Hawkins R. A practical tool for evaluating function: the simple shoulder test In: Matsen FA, Fu FH, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993:501–518. [Google Scholar]
- 36. Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28:693–696. [DOI] [PubMed] [Google Scholar]
- 37. Mall JW, Jacobi CA, Philipp AW, Peter FJ. Surgical treatment of fractures of the distal clavicle with polydioxanone suture tension band wiring: an alternative osteosynthesis. J Orthop Sci. 2002;7:535–537. [DOI] [PubMed] [Google Scholar]
- 38. Martetschläger F, Kraus TM, Schiele CS, et al. Treatment for unstable distal clavicle fractures (Neer 2) with locking T-plate and additional PDS cerclage. Knee Surg Sports Traumatol Arthrosc. 2013;21:1189–1194. [DOI] [PubMed] [Google Scholar]
- 39. Milewski MD, Tompkins M, Giugale JM, Carson EW, Miller MD, Diduch DR. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40:1628–1634. [DOI] [PubMed] [Google Scholar]
- 40. Moneim MS, Balduni FC. Coracoid fracture as a complication of surgical treatment by coracoclavicular tape fixation: a case report. Clin Orthop Relat Res. 1982;168:133–135. [PubMed] [Google Scholar]
- 41. Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127:191–194. [DOI] [PubMed] [Google Scholar]
- 42. Neer CS. Shoulder Reconstruction. Philadelphia, PA: WB Saunders Company; 1990. [Google Scholar]
- 43. Neer CS., 2nd Fracture of the distal clavicle with detachment of the coracoclavicular ligaments in adults. J Trauma. 1963;3:99–110. [DOI] [PubMed] [Google Scholar]
- 44. Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 45. Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994;300:127–132. [PubMed] [Google Scholar]
- 46. Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture: 15 (11-21) year follow-up of 110 cases. Acta Orthop. 1993;64:87–91. [DOI] [PubMed] [Google Scholar]
- 47. Oh JH, Kim SH, Lee JH, Shin SH, Gong HS. Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg. 2011;131:525–533. [DOI] [PubMed] [Google Scholar]
- 48. Othman A. Internal fixation of lateral clavicle fractures with Vicryl tape. Eur J Orthop Surg Traumatol. 2002;12:129–131. [DOI] [PubMed] [Google Scholar]
- 49. Robinson C, Akhtar M, Jenkins P, Sharpe T, Ray A, Olabi B. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92:811–816. [DOI] [PubMed] [Google Scholar]
- 50. Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg. 2004;86:778–782. [DOI] [PubMed] [Google Scholar]
- 51. Robinson CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg. 2004;86:1359–1365. [DOI] [PubMed] [Google Scholar]
- 52. Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Joint Dis. 2002;61:32–39. [PubMed] [Google Scholar]
- 53. Shan-Wei Y, Li Chun L, Shwu Jen C, Shyh Ming K, Lain-Chyr H. Treatment of acute unstable distal clavicle fractures with single coracoclavicular suture fixation. Orthopedics. 2011;34:e172–e177. [DOI] [PubMed] [Google Scholar]
- 54. Shin S-J, Roh KJ, Kim JO, Sohn H-S. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40:1308–1312. [DOI] [PubMed] [Google Scholar]
- 55. Soliman O, Koptan W, Zarad A. Under-coracoid-around-clavicle (UCAC) loop in type II distal clavicle fractures. Bone Joint J. 2013;95:983–987. [DOI] [PubMed] [Google Scholar]
- 56. Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB. Surgical treatment of Neer type-II fractures of the distal clavicle: a meta-analysis. Acta Orthop. 2013;84:184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Struhl S. Double endobutton technique for repair of complete acromioclavicular joint dislocations. Tech Shoulder Elbow Surg. 2007;8:175–179. [Google Scholar]
- 58. Struhl S, Wolfson TS. Continuous loop double endobutton reconstruction for acromioclavicular joint dislocation. Am J Sports Med. 2015;43:2437–2444. [DOI] [PubMed] [Google Scholar]
- 59. Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for Neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132:399–403. [DOI] [PubMed] [Google Scholar]
- 60. Tan HL, Zhao JK, Qian C, Shi Y, Zhou Q. Clinical results of treatment using a clavicular hook plate versus a T-plate in neer type II distal clavicle fractures. Orthopedics. 2012;35:e1191–e1197. [DOI] [PubMed] [Google Scholar]
- 61. Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury. 2000;31:175–179. [DOI] [PubMed] [Google Scholar]
- 62. Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22:366–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.