Abstract
Objective
To investigate the potential bidirectional relationships between severity of inattention and depression across early childhood.
Methods
Children (N = 216) from the New York, NY, metropolitan area were recruited when they were aged 3 to 4 years (T1) and studied again at age 6 (T2) and 7 (T3) years. Child inattention symptoms were measured using the Kiddie–Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime, along with both parent and teacher reports on the Behavior Assessment System for Children, Second Edition (BASC-2). Severity of child depression was assessed at each time point using parent and teacher reports on the BASC-2. After examining correlations between child inattention and depression, structural equation modeling was used to investigate whether child inattention was longitudinally related to child depression, and whether child depression symptoms were associated with later child inattention.
Results
Severity of child inattention at T1 and T2 was longitudinally associated with increased severity of child depression at T2 and T3, respectively. Early child depression was not longitudinally associated with later child inattention.
Conclusion
Child inattention is a risk factor for increased levels of child depression. Pediatricians and clinicians who assess children’s inattention symptoms also need to investigate symptoms of depression. This study makes a case for treating children’s inattention symptoms at preschool and early childhood, before emotional problems become more severe.
Keywords: inattention, depression, attention-deficit/hyperactivity disorder, preschool, early childhood, longitudinal
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neurobehavioral disorder that affects approximately 3% to 7% of school-aged children in the United States.1 It is characterized by developmentally inappropriate levels of inattention and hyperactivity/impulsivity that factor analytic studies have shown to be separate components of ADHD.2–5 Inattention and hyperactivity/impulsivity also have different trajectories of change over the lifetime. While children’s hyperactivity tends to decline with age, inattention symptoms appear to be more stable across time.6
Children with ADHD are at increased risk for comorbid depression,7–10 and as many as 42% of preschoolers with depression may also have ADHD.11 The comorbidity between ADHD and depression is associated with greater academic and psychosocial problems than the presence of either disorder alone.9,12 Although there is substantial comorbidity between these conditions from an early age,11 it is possible that close investigation would reveal a temporal precedence of 1 of the 2 disorders. There is some suggestion in the literature that depression is secondary to ADHD,13,14 perhaps by way of failures and discouragement in the family, social group, and school, as observed among patients with ADHD in clinical settings.15,16 Difficulties with school adjustment, for instance, have been found to mediate the association between child inattention and depression among young children.17 Herman et al18 also found that among black children who live in an urban setting, inattention symptoms during first grade were associated with depression during third grade, and that this association was mediated by academic failure. However, in this study, child inattention symptoms were measured at a single time point, compromising the ability to draw conclusions about whether inattention preceded depression. It is clear that depression emerges very early in development10,19 and often goes undetected.20 Thus, there is a need to study the temporal order of change in severity of the 2 disorders, especially during early childhood, to inform our understanding of emergent comorbidities and possibilities for early intervention.
There is some research investigating the differential association between the 2 factors of ADHD (ie, inattention and hyperactivity/impulsivity) and child depression. A meta-analysis of the correlations between inattention, hyperactivity, and other disorders showed that depression was significantly more closely associated with the severity of inattention than with the severity of hyperactivity.21 Moreover, inattentive children are often characterized by slower cognitive tempo, marked by low mental alertness and lethargy,22–25 which may also be seen in children with depression.1 Children with predominantly inattentive type ADHD may also have lower scores on Wechsler Preschool and Primary Scale of Intelligence when assessing processing speed compared with children with combined type ADHD.26 This suggests that there may be underarousal, slower cognitive tempo, and sluggishness in children with inattention but not in children with both inattention and hyperactivity/impulsivity.26 Therefore, it is possible that depression symptoms may be particularly associated with inattention. Finally, while individuals with both inattentive and combined types of ADHD have higher levels of depression than individuals without ADHD,27 hyperactive/impulsive individuals are not different from those without ADHD with regard to rates of depression.28 This suggests the need to specifically consider the association between inattention and depression.
This study takes a dimensional rather than categorical view of inattention and depression. Even children who do not meet diagnostic criteria for these disorders may have problems as a result of ADHD29 and depression symptoms.30 A dimensional approach provides a measure of the magnitude of problem severity, which may be helpful in developing an understanding of the temporal association between child inattention and depression. Thus, the words “inattention” and “depression” when used throughout this article refer to symptom severity rather than diagnoses of inattentive type ADHD and depression.
Given the earlier onset of ADHD relative to depression,13,14 this study hypothesized that an increase in symptoms of inattention over time would be associated with a subsequent increase in depression symptoms during preschool and early childhood. We also examined whether the severity of depression symptoms predicted later inattention levels.
Materials and Methods
Recruitment and Subjects
Children from the New York, NY, metropolitan area were recruited through preschools, clinics, and the community into a longitudinal study of children with different levels of ADHD symptoms when they were aged 3 to 4 years.31 Parents and teachers rated inattentive and hyperactive behaviors in children using the Attention-Deficit/Hyperactivity Disorder Rating Scale, Version IV.32 To ensure inclusion of children with a range of inattention and hyperactivity, two-thirds of the children had ≥6 symptoms of inattention and/or hyperactivity as rated by either parents or teachers, and the rest of the children had <3 such symptoms as rated by both parents and teachers. Children were excluded if they had a full-scale IQ <80, as measured by the Wechsler Preschool and Primary Scale of Intelligence, Third Edition33; if they had previously been diagnosed with a pervasive developmental or neurological disorder; if they were taking medication for a chronic medical condition, including stimulants for ADHD; or if the parents were not fluent in English. Parent and teacher reports were collected at child age 3 to 4 years (T1), 6 years (T2), and 7 years (T3).
A majority of the sample (72.7%) was male. Participants were racially and ethnically diverse, with 23 Asian, 27 black, 126 white, and 40 mixed-race children; 67 children were of Hispanic ethnicity. Approximately half of the mothers participating in the study were college graduates or had a graduate degree (Table 1). The mean socioeconomic index (SEI) score (standard deviation [SD]) at baseline was 58.85 (16.31).
Table 1.
Demographic Characteristics of T1 Sample (N = 216)
| Variable | N (%) or Mean (SD) |
|---|---|
| Male sex, n (%) | 157 (72.7) |
| Age, y, mean (SD) | 4.26 (0.48) |
| Race, n (%) | |
| White | 126 (58.2) |
| Black | 27 (12.4) |
| Asian | 23 (10.6) |
| > 1 race | 40 (18.8) |
| Hispanic | 67 (31.2) |
| SEI score, mean (SD) | 58.85 (16.31) |
| Maternal education, n (%) | (N = 214) |
| < 12 years of schooling | 9 (4.2) |
| High school graduate | 28 (13.1) |
| 1- to 3-year college | 70 (32.7) |
| College graduate | 61 (28.5) |
| Graduate degree | 46 (21.5) |
Abbreviations: SD, standard deviation; SEI, socioeconomic index.
Ethics
This study was approved by the Institutional Review Board of Queens College, The City University of New York (New York, NY). A full description of the study was provided. All parents signed Institutional Review Board–approved informed consent forms.
Measures
Child Inattention Symptoms
The Kiddie–Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime (K-SADS-PL),34 a semi-structured interview, was used to assess inattention symptoms using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria. Interviewers were either PhD-level psychologists or graduate students trained in psychopathology and supervised by a psychologist. Interviewers were blind to children’s diagnostic status and history. Nine items that are on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition inattention criteria for diagnosis of ADHD were scored on a 3-point scale (absent, sub-threshold, or present with impairment). Scores on these items were summed to obtain an overall score (range, 0–18), with higher scores indicating greater severity of inattention. The coefficient alphas for inattention at T1, T2, and T3 were 0.92, 0.92, and 0.93, respectively.
Parent and teacher reports on the Attention Problems subscale of the Behavior Assessment System for Children, Second Edition (BASC-2)35 were also obtained at each time point. The BASC-2 has well-established reliability and validity for preschool and school-aged children in both clinical and normative samples.35 In the normative sample, the coefficient alphas for teacher and parent report on the Attention Problems subscale were >0.92 and >0.85, respectively, for the age groups assessed in the present study (ie, ages 3, 4, 6, and 7 years). In a sample of children with clinical levels of ADHD, the coefficient alpha for the Attention Problems subscale was 0.91 for teacher report and 0.78 for parent report. The Attention Problems subscale has good inter-rater reliability across teachers (>0.69) and across caregivers (>0.78).35 This scale is highly correlated with the Attention Problems subscale on the Child Behavior Checklist (r = 0.65 for parent report; r = 0.64 for teacher report).35 In the current sample, Cronbach’s alphas of the items on the Attention Problems subscale for the parent report at T1, T2, and T3 were 0.91, 0.91, and 0.94, respectively, and for the teacher report were 0.92, 0.95, and 0.95, respectively.
Child Depression Symptoms
The Depression subscale of the BASC-2 includes items such as “is sad,” “cries easily,” “is easily upset,” “is negative about things,” and “changes mood quickly.” Items differ somewhat for preschoolers and school-aged children. Raw scores on both parent and teacher reports were used in this study. The coefficient alpha reliability for the parent report of depression ranges from 0.78 for 2- to 3-year-olds to 0.87 for 6- to 7-year-olds.35 The coefficient alpha for the teacher report is 0.83 for 2- to 3-year-olds and 0.84 for 6- to 7-year-olds.35 Test–retest reliability for teacher-report forms is 0.81 for the preschool form and 0.88 for the child form.35 The Depression subscale on the BASC-2 is correlated with the Anxious/Depressed subscale on the Child Behavior Checklist for 6- to 18-year-olds (r = 0.64 for parent report; r = 0.51 for teacher report).35 In the current sample, the coefficient alphas for the parent report at T1, T2, and T3 were 0.80, 0.85, and 0.86, respectively, and for the teacher report were 0.88, 0.88, and 0.84, respectively.
SEI Scores
Socioeconomic index scores, based on maternal education and occupational prestige, were measured at T1.36 Using the National Opinion Research Center General Social Survey, which asked a nationally representative sample of noninstitutionalized adults to evaluate the prestige of a range of detailed occupational titles, Nakao and Treas36 calculated SEI scores for >500 categories of occupations. These scores ranged from 11 (panhandler) to 97 (physician). In the present sample, scores ranged from 25 to 97, with the modal score being 64.
Missing Data
The retention rates at T2 and T3 were 79.2% and 72.7%, respectively. There were no significant differences in sex and ethnicity between T1 participants who also participated in follow-up (T2/T3) and those who did not (P>0.10). However, differences in SEI scores between participants and nonparticipants approached significance at T2 (P = 0.05; mean [SD] of participants, 56.22 [16.95]; mean [SD] of nonparticipants, 50.55 [17.27]) and were significant at T3 (P = 0.01; mean [SD] of participants, 56.89 [16.95]; mean [SD] of nonparticipants, 50.10 [16.77]). The full-information maximum likelihood method was used to estimate missing data. This method provides more unbiased estimates when data are missing at random compared with list-wise and pair-wise deletion.37,38
Statistical Analysis
Descriptive statistics including means, SDs (Table 1), and indicators of normality for the key variables were examined. All variables in the analysis had acceptable levels of skewness and kurtosis (values<1.96). Mean levels of inattention and depression between T1 and T3 were also examined (Table 2). Correlations between parent and teacher reports (Table 3) and between inattention and depression symptoms (Table 4) were studied.
Table 2.
Mean (SD) and Range of Raw Scores on Child Depression and Inattention for the Parent and Teacher Reports From T1 to T3
| Variable | Parent Report, Mean (SD) |
Min–Max | Teacher Report, Mean (SD) |
Min–Max |
|---|---|---|---|---|
| BASC-2 child depression | ||||
| T1 | 9.20 (4.59) | 0–27 | 6.09 (5.45) | 0–25 |
| T2 | 6.41 (4.85) | 0–23 | 3.77 (4.71) | 0–20 |
| T3 | 6.23 (5.07) | 0–24 | 3.99 (4.37) | 0–19 |
| BASC-2 child inattention | ||||
| T1 | 8.73 (4.07) | 0–18 | 9.10 (5.43) | 0–18 |
| T2 | 7.79 (4.26) | 0–18 | 9.91 (5.59) | 0–21 |
| T3 | 7.49 (4.70) | 0–17 | 9.53 (5.69) | 0–21 |
| K-SADS-PL child inattention | ||||
| T1 | 8.20 (5.88) | 0–18 | – | – |
| T2 | 7.95 (6.16) | 0–18 | – | – |
| T3 | 8.63 (6.56) | 0–18 | – | – |
Abbreviations: BASC-2, Behavior Assessment System for Children, Second Edition; K-SADS-PL, Kiddie–Schedule for Affective Disorders and Schizophrenia for School- Aged Children–Present and Lifetime; SD, standard deviation.
Table 3.
Correlation Between Parent and Teacher Reports of Child Inattention and Depression
| Child Symptoms | Age 3–4 Years | Age 6 Years | Age 7 Years |
|---|---|---|---|
| Inattention | |||
| Parent and teacher reports on the BASC-2 |
0.55a | 0.49a | 0.52a |
| Parent report on the K-SADS-PL and teacher report on the BASC-2 |
0.72a | 0.62a | 0.64a |
| Depression | |||
| Parent and teacher reports on the BASC-2 |
0.34a | 0.36a | 0.26a |
P < 0.01.
Abbreviations: BASC-2, Behavior Assessment System for Children, Second Edition; K-SADS-PL, Kiddie–Schedule for Affective Disorders and Schizophrenia for School- Aged Children–Present and Lifetime.
Table 4.
Correlation Between Child Inattention and Depression Symptoms
| Child Inattention |
Child Depression | |||||
|---|---|---|---|---|---|---|
| Age 3–4 Years |
Age 6 Years |
Age 7 Years |
||||
| Parent Report |
Teacher Report |
Parent Report |
Teacher Report |
Parent Report |
Teacher Report |
|
|
Age 3–4 Years |
||||||
| K-SADS-PL | 0.26a | 0.36a | 0.20a | 0.32a | 0.31a | 0.24a |
| BASC-2 (P) | 0.46a | 0.33a | 0.39a | 0.35a | 0.45a | 0.19c |
| BASC-2 (T) | 0.12b | 0.45a | 0.16c | 0.40a | 0.18c | 0.33a |
| Age 6 Years | ||||||
| K-SADS-PL | 0.26a | 0.27a | 0.39a | 0.38a | 0.35a | 0.28a |
| BASC-2 (P) | 0.36a | 0.32a | 0.50a | 0.30a | 0.46a | 0.21c |
| BASC-2 (T) | 0.02 | 0.11 | 0.17 c | 0.38a | 0.06 | 0.15 |
| Age 7 Years | ||||||
| K-SADS-PL | 0.33a | 0.31a | 0.28a | 0.34a | 0.39a | 0.41a |
| BASC-2 (P) | 0.38a | 0.29a | 0.41a | 0.40a | 0.52a | 0.30a |
| BASC-2 (T) | 0.11 | 0.18c | 0.21c | 0.33a | 0.19c | 0.41a |
P < 0.01.
P < 0.10.
P < 0.05.
Abbreviations: BASC-2, Behavior Assessment System for Children, Second Edition; K-SADS-PL, Kiddie–Schedule for Affective Disorders and Schizophrenia for School-Aged Children–Present and Lifetime; P, parent report; T, teacher report.
Data were aggregated to combine parent and teacher reports on inattention and depression. Inattention symptoms for the parent and teacher reports on the BASC-2 and on the K-SADS-PL were combined into a latent variable of inattention symptoms. A mean of parent and teacher reports on child depression was created for each time point. An observed mean score of child depression based on parent and teacher report was preferred over a latent variable because 2 indicators may contribute to poor model fit.39 Moreover, a mean was preferred as an observed variable because it may provide more valid estimates than the use of statistical or clinical weights.40
Structural equation modeling (SEM) was conducted to examine the longitudinal associations between depression and inattention from T1 to T2 and from T2 to T3. In preliminary linear regression analyses, child sex and SEI score were not longitudinally associated with child inattention or depression, and were therefore not included in the later analyses. To assess the fit of the model, a nonsignificant chi-square test result, comparative fit index (CFI) > 0.90, and root mean square error of approximation (RMSEA) < 0.08 were considered indices of good fit.41,42 As the chi-square statistic is known to be sensitive to small deviations from a perfectly causal model,43,44 the chi-square/degrees of freedom (df) ratio was considered. Models with a ratio < 3.00 were considered acceptable.45 In the SEM, the measurement error of each indicator of inattention was allowed to co-vary with the measurement error of the same indicator at every other time point. This strategy may help to account for the systematic method and reporter variance associated with each particular indicator.46
Results
Mean levels of inattention and depression from T1 to T3 are shown in Table 2. There was considerable stability in both child inattention and depression scores. Most children in the study had relatively low levels of depression. There were significant correlations between parent and teacher reports of both inattention and depression at each time point (Table 3). Each of the measures of child inattention was significantly associated with child depression both at the same time point and with later time points, except for parent and teacher reports of child depression at age 3 to 4 years with teacher report of inattention at age 6 years; parent report of depression at age 3 to 4 years with teacher report of inattention at age 7 years; and teacher report of inattention at age 6 years with parent and teacher reports of depression at age 7 years (Table 4).
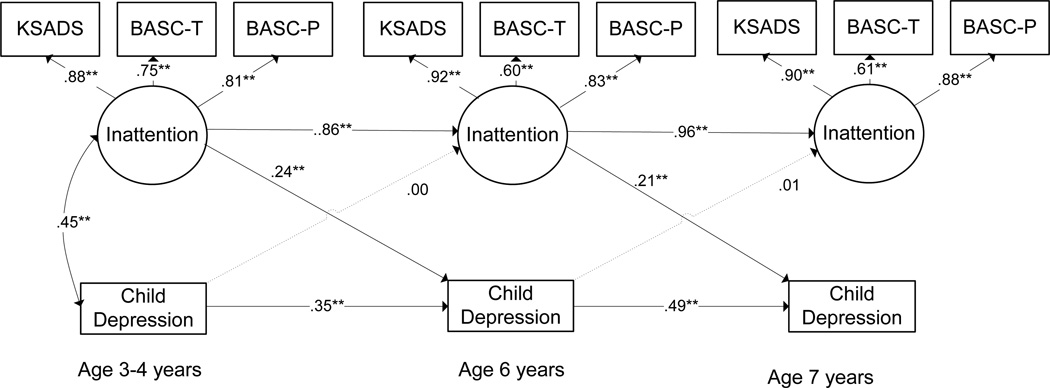
Structural equation modeling was used to investigate the bidirectional relationships between inattention and depression across all 3 time points (Figure 1). This model showed an acceptable fit to the data (chi-square [df], 113.92 [42]; P < 0.001; CFI, 0.95; RMSEA, 0.08; chi-square/df ratio, 2.71). While the RMSEA was just at the generally accepted limit, recent research suggests that there is little evidence to support use of fixed-point cutoffs for the RMSEA, which should be evaluated in tandem with other indicators of fit.47
Figure 1.
Relation between child depression and inattention symptoms
**p<.01; *p<.05
KSADS: The Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version;
BASC-T: Behavior Assessment System for children - Teacher Report;
BASC-P: Behavior Assessment System for children - Parent Report.
This model showed that there was considerable stability of child inattention and depression between age 3 to 4 years and age 6 years (β [standardized coefficient], 0.86; P < 0.001), and between age 6 to 7 years (β [standardized coefficient], 0.96; P < 0.001). It also provided evidence to support the longitudinal association between the severity of child inattention and the severity of child depression between age 3 to 4 years and age 6 years (β [standardized coefficient], 0.24; P = 0.002), and between age 6 and 7 years (β [standardized coefficient], 0.21; P = 0.003). Child depression was not longitudinally associated with child inattention at either age 6 or 7 years after controlling for earlier levels of child inattention (β [standardized coefficient] < 0.02; P > 0.90).
Post Hoc Analyses
Using procedures identical to those described in the previous section, we tested whether child hyperactivity/impulsivity symptoms were similarly associated with child depression. Child hyperactivity/impulsivity symptoms rated by parent and teacher reports on the BASC-2 and by parent report on the K-SADS-PL at T1, T2, and T3 were used to create a latent variable of child hyperactivity/impulsivity symptoms. The same variable created as a mean of parent and teacher reports on child depression (as used in an earlier model with inattention symptoms) was used. This model, which included child hyperactivity/impulsivity, provided a poor fit to the data (chi-square [df], 249.99 [42]; P < 0.001; CFI, 0.87; RMSEA, 0.15; chi-square/df ratio, 5.95).
Discussion
Children’s inattention symptoms were longitudinally associated with increased levels of depression symptoms during early childhood. This study did not find evidence to support the association between early depressive symptoms and later inattention symptoms. To our knowledge, the longitudinal associations between inattention and depression, and between depression and inattention during preschool and early childhood, have not been studied together in the same model.
This study used prospective, longitudinal data covering age 3 to 4 years and age 7 years, when children are adjusting to preschool and elementary school. Navigating this transition and meeting the increased social, academic, and behavioral demands of formal school is a major developmental task of early childhood.48,49 As discussed earlier, school maladjustment may mediate the association between child inattention and depression.17 It is important to identify children who have trouble regulating their behaviors and emotions at these stages, as this may be associated with difficulties with long-term adjustment.50–52
Another strength of this study was the use of a sample that was selected for displaying a range of inattentive behaviors. This variability in inattention severity may have enabled us to more effectively test the impact of child inattention on depression. Finally, using a dimensional approach to measuring child behaviors enabled us to consider changes in the severity of both inattention and depression. The value of a dimensional approach to measuring variance in child psychopathology is becoming increasingly evident.53 Recognizing child inattention symptoms and providing early intervention may preempt the development of severe symptoms and alter the course of depression54,55 and ADHD.56
A limitation of this study is that it did not consider other problem behaviors that might coexist with child inattention, including conduct problems and oppositionality. Although this study tested whether child hyperactivity/impulsivity was longitudinally associated with child depression, the poor fit of the model suggests that child hyperactivity may not be directly related to child depression. Future studies with different samples need to test whether this lack of fit suggests that there may be behavioral or parenting variables that moderate this association. For instance, child hyperactivity/impulsivity may be associated with child depression in the presence of parent stress or negative parenting. This study used the full-information maximum likelihood method to estimate missing data. Although this method is recommended in the presence of missing data,37,38 it is unclear whether this may influence the results of the study.
It needs to be noted that children who were treated with medications for behavioral problems at age 3 to 4 years were excluded from this study. These children were most likely to have had greater severity of inattention and/or hyperactivity/impulsivity. Although none of the children in the study were taking medications at T1, 26 children were taking medications for treatment of ADHD at T3. It is not clear how the use of medications may impact the association between inattention and depression. Stimulants have been associated with emotional lability and low affect.57 While some research suggests that children who are treated with stimulants may have a lower risk of developing depression in adulthood,58 data also suggest that such treatment during childhood does not affect rates of depression in adolescents.59 The present study did not consider how medication treatment may influence child inattention or depression.
This study sets the stage for an exploration of the biological and neurocognitive similarities between inattention and depression. Both ADHD60 and depression61 are heritable, although multiple factors may be involved in their onset and persistence. Hippocampal volume reduction has been posited both in ADHD62 and depression.63 A dysregulation of the frontostriatal region may play a role in the development of ADHD,64 as well as depression.61 Moreover, a subgroup of inattentive children have been noted to experience low levels of alertness and slow cognitive tempo.5,65 This subgroup may have elevated levels of depression and withdrawal compared with those who have faster cognitive tempos.66 Thus, studying the emergent association between child inattention and depression may pave the way for a better understanding of both inattention and depression in children.
Conclusion
This study provides evidence that higher levels of child inattention during the preschool years are associated with greater child depression during early school age. It suggests that pediatricians and other practitioners who assess the level of inattention in children may also want to investigate emergent child depression. Factors such as parenting, behavior management, medications, and other early interventions that attenuate children’s inattention severity may have secondary benefits in reducing the severity of depression symptoms during childhood.
Acknowledgments
This project was supported by award number R01MH068286 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH.
Footnotes
Conflict of Interest Statement
Khushmand Rajendran, PhD, MSW, Sarah O’Neill, PhD, and Jeffrey M. Halperin, PhD, disclose no conflicts of interest.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 2.Hudziak JJ, Heath AC, Madden PF, et al. Latent class and factor analysis of DSM-IV ADHD: a twin study of female adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37(8):848–857. doi: 10.1097/00004583-199808000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Bauermeister JJ. Factor analyses of teacher ratings of attention-deficit hyperactivity and oppositional defiant symptoms in children aged four through thirteen years. J Clin Child Psychol. 1992;21(1):27–34. [Google Scholar]
- 4.DuPaul GJ, Power TJ, Anastopoulos AD, Reid R, McGoey K, Ikeda MJ. Teacher ratings of attention-deficit/hyperactivity disorder symptoms: factor structure and normative data. Psychological Assessment. 1997;9(4):436–444. doi: 10.1037/pas0000166. [DOI] [PubMed] [Google Scholar]
- 5.Lahey BB, Pelham WE, Schaughency EA, et al. Dimensions and types of attention deficit disorder. J Am Acad Child Adolesc Psychiatry. 1988;27(3):330–335. doi: 10.1097/00004583-198805000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry. 2000;157(5):816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- 7.Mayes SD, Calhoun SL, Chase GA, Mink DM, Stagg RE. ADHD subtypes and co-occurring anxiety, depression, and oppositional-defiant disorder: differences in Gordon diagnostic system and Wechsler working memory and processing speed index scores. J Atten Disord. 2009;12(6):540–550. doi: 10.1177/1087054708320402. [DOI] [PubMed] [Google Scholar]
- 8.Angold A, Costello EJ, Erklani A. Comorbidity. J Child Psychol Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- 9.Jensen PS, Shervette RE, 3rd, Xenakis SN, Richters J. Anxiety and depressive disorders in attention deficit disorder with hyperactivity: new findings. Am J Psychiatry. 1993;150(8):1203–1209. doi: 10.1176/ajp.150.8.1203. [DOI] [PubMed] [Google Scholar]
- 10.Wilens TE, Biederman J, Brown S, et al. Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. J Am Acad Child Adolesc Psychiatry. 2002;41(3):262–268. doi: 10.1097/00004583-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Luby JL, Heffelfinger AK, Mrakotsky C, et al. The clinical picture of depression in preschool children. J Am Acad Child Adolesc Psychiatry. 2003;42(3):340–348. doi: 10.1097/00004583-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53(5):437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- 13.Kovacs M, Akiskal HS, Gatsonis C, Parrone PL. Childhood-onset dysthymic disorder. Clinical features and prospective naturalistic outcome. Arch Gen Psychiatry. 1994;51(5):365–374. doi: 10.1001/archpsyc.1994.03950050025003. [DOI] [PubMed] [Google Scholar]
- 14.Biederman J, Faraone S, Mick E, Lelon E. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? J Am Acad Child Adolesc Psychiatry. 1995;34(5):579–590. doi: 10.1097/00004583-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Solanto MV, Marks DJ, Wasserstein J. Diagnostic evaluation of ADHD in adults. In: Solanto MV, editor. Cognitive-Behavioral Therapy for Adult ADHD: Targeting Executive Dysfunction. New York, NY: Guilford Press; 2011. pp. 23–39. [Google Scholar]
- 16.Carr A. The Handbook of Child and Adolescent Clinical Psychology: A Contextual Approach. 2nd. New York, NY: Taylor and Francis; 2006. [Google Scholar]
- 17.Herman KC, Ostrander RO. The effects of attention problems on depression: developmental, academic, and cognitive pathways. School Psychol Q. 2007;22(4):483–510. [Google Scholar]
- 18.Herman KC, Lambert SF, Ialongo NS, Ostrander R. Academic pathways between attention problems and depressive symptoms among urban African American children. J Abnorm Child Psychol. 2007;35(2):265–274. doi: 10.1007/s10802-006-9083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Luby JL, Si X, Belden AC, Tandon M, Spitznagel E. Preschool depression: homotypic continuity and course over 24 months. Arch Gen Psychiatry. 2009;66(8):897–905. doi: 10.1001/archgenpsychiatry.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luby JL. Preschool depression: the importance of identification of depression early in development. Curr Dir Psychol Sci. 2010;19(2):91–95. doi: 10.1177/0963721410364493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willcutt EG, Nigg JT, Pennington BF, et al. Validity of DSM-IV attention deficit/hyperactivity disorder symptom dimensions and subtypes. J Abnorm Psychol. 2012;121(4):991–1010. doi: 10.1037/a0027347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frick PJ, Lahey BB, Applegate B, et al. DSM-IV field trials for the disruptive behavior disorders: symptom utility estimates. J Am Acad Child Adolesc Psychiatry. 1994;33(4):529–539. doi: 10.1097/00004583-199405000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Lahey BB, Carlson C. Validity of the diagnostic category of attention deficit disorder without hyperactivity: a review of the literature. J Learn Disabil. 1991;24(2):110–120. doi: 10.1177/002221949102400208. [DOI] [PubMed] [Google Scholar]
- 24.Hartman CA, Willcutt EG, Rhee SH, Pennington BF. The relation between sluggish cognitive tempo and DSM-IV ADHD. J Abnorm Child Psychol. 2004;32(5):491–503. doi: 10.1023/b:jacp.0000037779.85211.29. [DOI] [PubMed] [Google Scholar]
- 25.McBurnett K, Pfiffner LJ, Frick PJ. Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. J Abnorm Child Psychol. 2001;29(3):207–213. doi: 10.1023/a:1010377530749. [DOI] [PubMed] [Google Scholar]
- 26.Calhoun SL, Mayes SD. Processing speed in children with clinical disorders. Psychol Schools. 2005;42(4):333–343. [Google Scholar]
- 27.Power TJ, Costigan TE, Eiraldi RB, Leff SS. Variations in anxiety and depression as a function of ADHD subtypes defined by DSM-IV: do subtype differences exist or not? J Abnorm Child Psychol. 2004;32(1):27–37. doi: 10.1023/b:jacp.0000007578.30863.93. [DOI] [PubMed] [Google Scholar]
- 28.Faraone S, Biederman J, Weber W, Russell RL. Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of attention-deficit/hyperactivity disorder: results from a clinically referred sample. J Am Acad Child Adolesc Psychiatry. 1998;37(2):185–193. doi: 10.1097/00004583-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Coghill D, Spiel G, Baldursson G, et al. ADORE Study Group. Which factors impact on clinician-rated impairment in children with ADHD? Eur Child Adolesc Psychiatry. 2006;15(suppl 1):I30–I37. doi: 10.1007/s00787-006-1005-x. [DOI] [PubMed] [Google Scholar]
- 30.Pickles A, Rowe R, Simonoff E, Foley D, Rutter M, Silberg J. Child psychiatric symptoms and psychosocial impairment: relationship and prognostic significance. Br J Psychiatry. 2001;179:230–235. doi: 10.1192/bjp.179.3.230. [DOI] [PubMed] [Google Scholar]
- 31.Healey DM, Miller CJ, Castelli KL, Marks DJ, Halperin JM. The impact of impairment criteria on rates of ADHD diagnoses in preschoolers. J Abnorm Child Psychol. 2008;36(5):771–778. doi: 10.1007/s10802-007-9209-1. [DOI] [PubMed] [Google Scholar]
- 32.DuPaul G, Power TJ, Anastopoulos AD, Reid R. ADHD Rating Scale IV: Checklists, Norms, and Clinical Interpretation. New York, NY: Guilford Press; 1998. [Google Scholar]
- 33.Wechsler D. Wechsler Preschool and Primary Scale of Intelligence. 3rd. San Antonio, TX: Psychological Corporation; 2002. [Google Scholar]
- 34.Kaufman J, Birmaher B, Brent D, Rao U, Ryan N. The Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version. Pittsburgh, PA: University of Pittsburgh School of Medicine; 1996. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds CR, Kamphaus RW. Behavior Assessment System for Children. 2nd. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- 36.Nakao K, Treas J. Updating occupational prestige and socioeconomic scores: how the new measures measure up. Sociol Methodol. 1994;24:1–72. [Google Scholar]
- 37.Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling: Issues and Techniques. Hillsdale, NJ: Lawrence Erlbaum Associates; 1996. pp. 243–278. [Google Scholar]
- 38.Little RJ, Rubin DB. Statistical Analysis with Missing Data. 2nd. New York, NY: John Wiley and Sons, Inc.; 2002. [Google Scholar]
- 39.Marsh HW, Hau KT, Balla JR, Grayson D. Is more ever too much? The number of indicators per factor in confirmatory factor analysis. Multivariate Behav Res. 1998;33(2):181–220. doi: 10.1207/s15327906mbr3302_1. [DOI] [PubMed] [Google Scholar]
- 40.Piacentini JC, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: are complex algorithms better than simple ones? J Abnorm Child Psychol. 1992;20(1):51–63. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- 41.Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Pers Indiv Differ. 2007;42(5):893–898. [Google Scholar]
- 42.Kline RB. Principles and Practice of Structural Equation Modeling. 2nd. New York, NY: Guilford Press; 2005. [Google Scholar]
- 43.Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. 2nd. New York, NY: Taylor and Francis; 2004. [Google Scholar]
- 44.Byrne BM. Structural Equation Modeling With AMOS: Basic Concepts, Applications, and Programming. New York, NY: Taylor and Francis; 2010. [Google Scholar]
- 45.Carmines EG, McIver JP. Analyzing models with unobserved variables. In: Bohrnstedt GW, Borgatta EF, editors. Social Measurement: Current Issues. Beverly Hills, CA: Sage Publications; 1981. pp. 65–115. [Google Scholar]
- 46.Pitts SC, West SG, Tein JY. Longitudinal measurement models in evaluation research: examining stability and change. Eval Program Plan. 1996;19(4):333–350. [Google Scholar]
- 47.Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Methods Res. 2008;36(4):462–494. doi: 10.1177/0049124108314720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Campbell SB, von Stauffenberg C. Child characteristics and family processes that predict behavioral readiness for school. In: Booth A, Crouter AC, editors. Disparities in School Readiness: How Do Families Contribute to Transitions Into School? New York, NY: Lawrence Erlbaum Associates; 2008. pp. 225–258. [Google Scholar]
- 49.Rimm-Kaufman SE, Pianta RC. An ecological perspective on the transition to kindergarten: a theoretical framework to guide empirical research. J Appl Dev Psychol. 2000;21(5):491–511. [Google Scholar]
- 50.Caspi A, Silva PA. Temperamental qualities at age three predict personality traits in young adulthood: longitudinal evidence from a birth cohort. Child Dev. 1995;66(2):486–498. doi: 10.1111/j.1467-8624.1995.tb00885.x. [DOI] [PubMed] [Google Scholar]
- 51.Caspi A, Harrington H, Milne B, Amell JW, Theodore RF, Moffitt TE. Children’s behavioral styles at age 3 are linked to their adult personality traits at age 26. J Pers. 2003;71(4):495–513. doi: 10.1111/1467-6494.7104001. [DOI] [PubMed] [Google Scholar]
- 52.Pulkkinen L. Proactive and reactive aggression in early adolescence as precursors to anti- and prosocial behavior in young adults. Aggressive Behavior. 1996;22(4):241–257. [Google Scholar]
- 53.Hudziak JJ, Achenbach TM, Althoff RR, Pine DS. A dimensional approach to developmental psychopathology. Int J Methods Psychiatr Res. 2007;16(suppl 1):S16–S23. doi: 10.1002/mpr.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Beardslee WR, Gladstone TR. Prevention of childhood depression: recent findings and future prospects. Biol Psychiatry. 2001;49(12):1101–1110. doi: 10.1016/s0006-3223(01)01126-x. [DOI] [PubMed] [Google Scholar]
- 55.Dadds MR, Holland DE, Laurens KR, Mullins M, Barrett PM, Spence SH. Early intervention and prevention of anxiety disorders in children: results of a 2-year follow-up. J Consult Clin Psychol. 1999;67(1):145–150. doi: 10.1037//0022-006x.67.1.145. [DOI] [PubMed] [Google Scholar]
- 56.McGoey KE, Eckert TL, Dupaul GJ. Early intervention for preschool-age children with ADHD: a literature review. J Emot Behav Disord. 2002;10(1):14–28. [Google Scholar]
- 57.Wilens TE, Spencer TJ. The stimulants revisited. Child Adolesc Psyciatr Clin N Am. 2000;9(3):573–603. viii. [PubMed] [Google Scholar]
- 58.Biederman J, Monuteaux MC, Spencer T, Wilens TE, Faraone SV. Do stimulants protect against psychiatric disorders in youth with ADHD? A 10-year follow-up study. Pediatrics. 2009;124(1):71–78. doi: 10.1542/peds.2008-3347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Staikova EA, Marks DJ, Miller CJ, Newcorn JH, Halperin JM. Childhood stimulant treatment and teen depression: is there a relationship? J Child Adolesc Psychopharmacol. 2010;20(5):387–393. doi: 10.1089/cap.2009.0107. [DOI] [PubMed] [Google Scholar]
- 60.Albayrak O, Friedel S, Schimmelmann BG, Hinney A, Hebebrand J. Genetic aspects in attention-deficit/hyperactivity disorder. J Neural Transm. 2008;115(2):305–315. doi: 10.1007/s00702-007-0839-9. [DOI] [PubMed] [Google Scholar]
- 61.Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM. Neurobiology of depression. Neuron. 2002;34(1):13–25. doi: 10.1016/s0896-6273(02)00653-0. [DOI] [PubMed] [Google Scholar]
- 62.Plessen KJ, Bansal R, Zhu H, et al. Hippocampus and amygdala morphology in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63(7):795–807. doi: 10.1001/archpsyc.63.7.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Videbech P, Ravnkilde B. Hippocampal volume and depression: a meta-analysis of MRI studies. Am J Psychiatry. 2004;161(11):1957–1966. doi: 10.1176/appi.ajp.161.11.1957. [DOI] [PubMed] [Google Scholar]
- 64.Johansen EB, Aase H, Meyer A, Sagvolden T. Attention-deficit/hyperactivity disorder (ADHD) behaviour explained by dysfunctioning reinforcement and extinction processes. Behav Brain Res. 2002;130(1–2):37–45. doi: 10.1016/s0166-4328(01)00434-x. [DOI] [PubMed] [Google Scholar]
- 65.McBurnett K, Pfiffner LJ, Frick PJ. Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. J Abnorm Child Psych. 2001;29(3):207–213. doi: 10.1023/a:1010377530749. [DOI] [PubMed] [Google Scholar]
- 66.Carlson CL, Mann M. Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. J Clin Child Adolesc Psychol. 2002;3(1):123–129. doi: 10.1207/S15374424JCCP3101_14. [DOI] [PubMed] [Google Scholar]