Abstract
Objectives:
Psychological difficulties are a common complication among patients with respiratory disease, and are associated with poorer health outcomes and increased use of healthcare. As prevalence studies typically sample patients from community settings, this study aimed to explore the extent and nature of psychological difficulties during acute hospital admission.
Methods:
A case example of an acute respiratory ward is presented. In total, 41 acute respiratory inpatients completed standardised measures of depression, anxiety, and health anxiety.
Results:
Rates of clinically significant depression, anxiety, and health anxiety were 71%, 40%, and 21%, respectively, with 76% of participants showing clinically significant scores on at least one measure. Comparison to existing literature suggests depression rates may be elevated in the acute inpatient context. The difficulties experienced encompassed both contextual factors related to being in hospital and broader health concerns.
Conclusion:
We suggest that psychological distress may be particularly prevalent in inpatient settings and that larger-scale studies are warranted.
Keywords: Respiratory disease, anxiety, depression, health anxiety, inpatient, prevalence
Introduction
In respiratory settings, experiencing psychological difficulties is associated with poorer health outcomes including risk of mortality, lower quality of life, poorer ability to manage physical symptoms, and reduced self-care behaviours.1–4 Alongside the patient burden, there are significant service-level implications, both financially and regarding healthcare demand: patients have longer and more frequent admissions, higher emergency care attendance, and greater medication use.5–9 As a result, psychological assessment and intervention is recommended by national guidelines for respiratory conditions.10–13
Given the significance of these difficulties, it is important to understand their prevalence and nature, in order to implement effective interventions. Studies have highlighted that treatable difficulties such as anxiety and depression are common in chronic respiratory conditions. Prevalence rates, calculated using standardised screening questionnaires or diagnostic interviews, average between 32% and 65%,14–16 and estimates of anxiety, depression, or both are as high as 80%.17
As most studies use outpatient samples, the prevalence of psychological difficulties during hospital admission is unknown. One study found that 50% and 39% of patients with chronic obstructive pulmonary disease (COPD) on a rehabilitation ward showed clinically significant anxiety and depression, respectively.18 While there is some evidence that these difficulties generally improve across the admission, difficulties persisted in 9%–40% of patients.18,19 It is plausible, and perhaps assumed, that the stress of an acute admission may mean there is a higher prevalence in acute ward environments, but to the authors’ knowledge, there are to date no studies investigating this. A more detailed understanding of psychological functioning in acute respiratory contexts is therefore required.
This study investigated the frequency and nature of anxiety and depression among patients on an acute respiratory ward. It aimed to review psychological need within this patient cohort and consider support and intervention approaches.
Method
Design
Standardised measures of psychological difficulties were completed by patients on a 33-bed acute respiratory ward in a National Health Service (NHS) hospital. Data from two separate patient samples were collected 3 months apart (January and April 2015) to reduce any potential seasonal effects.
Procedure
Patients were considered eligible if their medical status and communicative ability were sufficient to complete the measures verbally or in writing. Eligible patients were approached and invited to participate. Verbal informed consent was obtained, and patients were informed that non-participation would not affect the care they received. As the measures were already being used by the clinical psychologist on the ward as part of routine practice, and that the principal aim was to evaluate the specific ward, the study was classified as service evaluation rather than research, and thus did not require additional ethical approval.20
Measures
Patient Health Questionnaire (PHQ-9):21 A widely used and validated brief measure assessing depression severity; scores ⩾5 are clinically significant, with scores 5–9, 10–14, 15–19, and 20 and above reflecting mild, moderate, moderately severe, and severe depression, respectively (maximum score 27). Cronbach’s alpha for the present sample was 0.81.
Generalised Anxiety Disorder Questionnaire (GAD-7):22 A widely used and validated brief measure assessing anxiety severity; scores ≥5 are clinically significant, with scores 5–9, 10–14, and 15 and above reflecting mild, moderate, and severe anxiety, respectively (maximum score 21). Cronbach’s alpha was 0.92.
Health Anxiety Inventory – 14 item (SHAI):23 A well-validated tool assessing health anxiety symptoms (from mild concerns to hypochondriasis); scores ⩾15 are clinically significant,24 although different cut-off scores have been used in the literature25 (maximum score 42). Health anxiety was assessed to explore the extent of symptoms such as body hypervigilance and health-related worries in this patient group. Cronbach’s alpha was 0.74.
Participants
From 66 inpatients, 44 were considered eligible, 41 of whom (93%) consented verbally to participation (21 female; mean age, 67; range, 19–86; 88% White British). A total of 25 participants (61%) had a chronic respiratory diagnosis (68% COPD; 12% asthma; 12% bronchiectasis; 4% lung cancer; 4% interstitial lung disease) with the remainder admitted for acute conditions (e.g. infection, pneumonia).
Results
The distributions of PHQ-9 (n = 41) and GAD-7 (n = 40) scores are shown in Figure 1. Totally, 71% of participants showed scores indicating depressive symptoms of mild severity or higher; the equivalent figure for anxious symptoms was 40%. For both measures, scores ranged from those indicating no symptoms through to moderate and severe symptoms.
Figure 1.
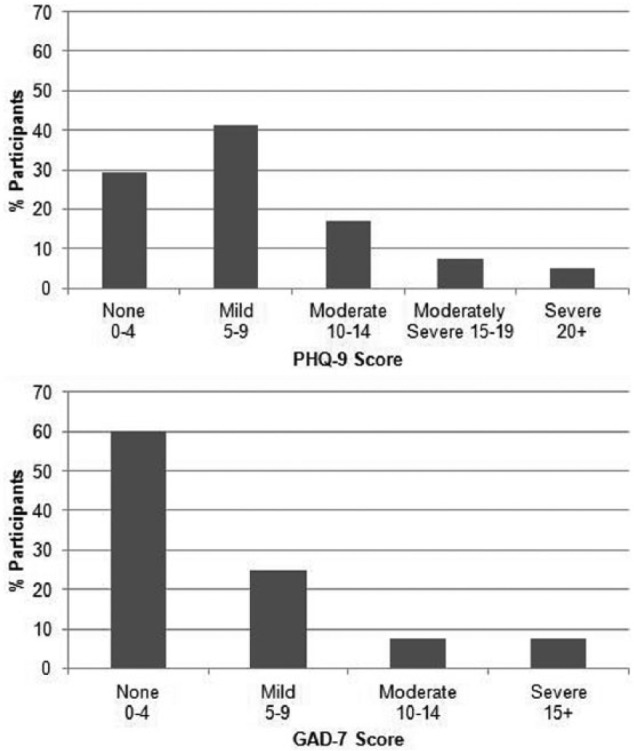
Distribution of participants’ scores on the PHQ-9 (top panel) indicating depression severity (n = 41) and the GAD-7 (bottom panel) indicating anxiety severity (n = 40).
On the SHAI (n = 38), 21% of participants scored above the clinical cut-off, indicating significant levels of health anxiety, and 76% of patients showed clinically significant scores on at least one of the three measures.
Discussion
The present results highlight high levels of anxiety, health anxiety, and particularly depression within the inpatient sample. The rates are broadly consistent with existing literature using outpatient samples, although depression symptoms may be particularly elevated in the acute setting. Given the association between psychological distress and poorer respiratory outcomes,1 the findings suggest a need to consider inpatients’ psychological functioning and its impact on their ability to cope following discharge.
When completing the questionnaires, some participants highlighted that some difficulties are context dependent, for example, low mood resulting from reduced sleep, social interaction, or activity in hospital, or anxiety driven by an increased focus on illness, and long time periods in which to worry or ruminate. We may therefore expect an improvement in some patients following discharge without a need for psychological intervention. However, two points are raised: first, the above issues often occur concurrently with broader psychological difficulties such as adjustment to illness, coping with physical limitations, and anxiety about the future. These may persist beyond discharge and could require specialised support. Second, even without these broader issues, inpatients should be supported in managing psychological distress, and it seems critical that ward staff feel sufficiently trained and confident in this aspect of patient care. This is important to prevent misunderstandings and difficulties in patient–staff communication and to deliver the compassionate and person-centred care central to the recommendations of the Francis enquiry into failures of care in Mid-Staffordshire.26
As a small-scale evaluation of a single ward, the study findings may have limited generalisability to other acute respiratory settings, and replication and large-scale controlled studies would be required to evaluate this. It is noted that the present sample had a potential overrepresentation of White British participants relative to ethnic diversity in the local population, although it is unclear if and how this may have affected the findings. Sampling throughout the year may help to further mitigate potential seasonal differences should these be present. Despite these limitations, the ability of this study to highlight and describe the psychological difficulties experienced in this patient group can be considered a strength, and it is hoped the findings may encourage larger-scale research in this area.
The high rates of psychological difficulties among respiratory inpatients mean the ward environment is an important location to identify those in need. Integrating psychology provision within inpatient multidisciplinary teams can serve to support staff in the care of distressed patients and provide clinical assessment to distinguish difficulties that are appropriate given the context from broader issues that may require further intervention without complicating medication regimes.
Acknowledgments
The authors wish to thank the study participants and ward staff.
Footnotes
Declaration of conflicting interests: The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: Ethical approval was not sought for this study because the study was classified as service evaluation rather than research.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support for the provision of clinical psychology on the ward and for publication of this article was provided by the Innovation Panel of the Royal United Hospital, Bath, UK.
Informed consent: Verbal informed consent was obtained from all subjects before the study.
References
- 1. Felker B, Bush KR, Harel O, et al. Added burden of mental disorders on health status among patients with chronic obstructive pulmonary disease. Prim Care Companion J Clin Psychiatry 2010; 12: e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hallas C, Howard C, Wray J. Understanding panic disorder in chronic respiratory disease. Br J Nurs 2009; 18: 527–529. [DOI] [PubMed] [Google Scholar]
- 3. Atlantis E, Fahey P, Cochrane B, et al. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest 2013; 144: 766–777. [DOI] [PubMed] [Google Scholar]
- 4. Blakemore A, Dickens C, Guthrie E, et al. Depression and anxiety predict health-related quality of life in chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2014; 9: 501–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Coventry PA, Gemmell I, Todd CJ. Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: a cohort study. BMC Pulm Med 2011; 11: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gudmundsson G, Gislason T, Janson C, et al. Risk factors for rehospitalisation in COPD: role of health status, anxiety and depression. Eur Respir J 2005; 26: 414–419. [DOI] [PubMed] [Google Scholar]
- 7. Kitagawa R, Yasui-Furukori N, Tsushima T, et al. Depression increases the length of hospitalization for patients undergoing thoracic surgery: a preliminary study. Psychosomatics 2011; 52: 428–432. [DOI] [PubMed] [Google Scholar]
- 8. Xu W, Collet J-P, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med 2008; 178: 913–920. [DOI] [PubMed] [Google Scholar]
- 9. Chan A, Yii A, Tay CK, et al. The impact of anxiety and depression on asthma-related health outcomes: a prospective study. Eur Respir J 2015; 46: PA5097. [Google Scholar]
- 10. Pasteur MC, Bilton D, Hill AT. British Thoracic Society guideline for non-CF bronchiectasis. Thorax 2010; 65: i1–i58. [DOI] [PubMed] [Google Scholar]
- 11. Bolton CE, Bevan-Smith EF, Blakey JD, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults: accredited by NICE. Thorax 2013; 68: ii1–ii30. [DOI] [PubMed] [Google Scholar]
- 12. National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease: clinical guideline 101. London: National Institute for Health and Care Excellence, 2010. [Google Scholar]
- 13. National Institute for Health and Care Excellence. Lung cancer: clinical guideline 121. London: National Institute for Health and Care Excellence, 2011. [Google Scholar]
- 14. Dowson C, Kuijer R, Mulder R. Anxiety and self-management behaviour in chronic obstructive pulmonary disease: what has been learned? Chron Respir Dis 2004; 1: 213–220. [DOI] [PubMed] [Google Scholar]
- 15. Mikkelsen RL, Middelboe T, Pisinger C, et al. Anxiety and depression in patients with chronic obstructive pulmonary disease (COPD): a review. Nord J Psychiatry 2004; 58: 65–70. [DOI] [PubMed] [Google Scholar]
- 16. Toms N, Greening N, Free R, et al. Prevalence and characteristics of anxiety and depression in patients with advanced COPD. Eur Respir J 2015; 46: PA3063. [Google Scholar]
- 17. Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest 2005; 127: 1205–1211. [DOI] [PubMed] [Google Scholar]
- 18. Dowson C, Laing R, Barraclough R, et al. The use of the Hospital Anxiety and Depression Scale (HADS) in patients with chronic obstructive pulmonary disease: a pilot study. N Z Med J 2001; 114: 447–449. [PubMed] [Google Scholar]
- 19. Kathol RG, Wenzel RP. Natural history of symptoms of depression and anxiety during inpatient treatment on general medicine wards. J Gen Intern Med 1992; 7: 287–293. [DOI] [PubMed] [Google Scholar]
- 20. NHS Health Research Authority. Defining research, 2013, http://www.hra.nhs.uk/resources/before-you-apply/is-it-research/
- 21. Kroencke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 23. Salkovskis PM, Rimes KA, Warwick H, et al. The Health Anxiety Inventory: development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychol Med 2002; 32: 843–853. [DOI] [PubMed] [Google Scholar]
- 24. Tang NK, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J Sleep Res 2007; 16: 85–95. [DOI] [PubMed] [Google Scholar]
- 25. Alberts NM, Hadjistavropoulos HD, Jones SL, et al. The Short Health Anxiety Inventory: a systematic review and meta-analysis. J Anxiety Disord 2013; 27: 68–78. [DOI] [PubMed] [Google Scholar]
- 26. Francis R. Report of the Mid Staffordshire NHS foundation trust: public inquiry. London: The Stationery Office, 2013. [Google Scholar]


