Abstract
Background
Although sex differences in hepatocellular carcinoma (HCC) risk are well known, it is unclear whether sex differences also exist in clinical presentation and survival outcomes once HCC develops.
Methods
We performed a retrospective cohort study of 1886 HCC patients seen in a US medical centre in 1998–2015. Data were obtained by chart review with survival data also by National Death Index search.
Results
The cohort consisted of 1449 male and 437 female patients. At diagnosis, men were significantly younger than women (59.9±10.7 vs 64.0±11.6, p<0.0001). Men had significantly higher rates of tobacco (57.7% vs 31.0%, p<0.001) and alcohol use (63.2% vs 35.1%, p<0.001). Women were more likely to be diagnosed by routine screening versus symptomatically or incidentally (65.5% vs 58.2%, p=0.03) and less likely to present with tumours >5 cm (30.2% vs 39.8%, p=0.001). Surgical and non-surgical treatment utilisation was similar for both sexes. Men and women had no significant difference in median survival from the time of diagnosis (median 30.7 (range=24.5–41.3) vs 33.1 (range=27.4–37.3) months, p=0.84). On multivariate analysis, significant predictors for improved survival included younger age, surgical or non-surgical treatment (vs supportive care), diagnosis by screening, tumour within Milan criteria and lower Model for End-Stage Liver Disease score, but not female sex (adjusted HR=1.01, CI 0.82 to 1.24, p=0.94).
Conclusions
Although men have much higher risk for HCC development, there were no significant sex differences in disease presentation or survival except for older age and lower tumour burden at diagnosis in women. Female sex was not an independent predictor for survival.
Keywords: HEPATOCELLULAR CARCINOMA, SURVEILLANCE, SCREENING
Summary box.
What is already known about this subject?
-
▸
Hepatocellular carcinoma (HCC) is the sixth most prevalent cancer worldwide.
-
▸
HCC generally occurs in the setting of liver cirrhosis of any aetiology or with chronic hepatitis B, even in the absence of cirrhosis.
-
▸
Men have a 2–4 times higher risk for developing HCC than women.
What are the new findings?
-
▸
Sex is not an independent predictor for survival among patients diagnosed with HCC.
-
▸
At diagnosis, men had more advanced liver disease, with larger and more tumour nodules.
-
▸
Women were more likely to be diagnosed with HCC on routine screening.
-
▸
Despite men having a higher tumour burden at diagnosis, men and women received curative HCC treatments at equal rates.
How might it impact on clinical practice in the foreseeable future?
-
▸
Increased compliance to screening recommendations should be emphasised, especially among at-risk men.
-
▸
Disparities in treatment of men and women with HCC should be addressed.
-
▸
Survival can be improved in both sexes if disparity in HCC screening and surveillance and treatment utilisation can be addressed for both groups.
Background
Hepatocellular carcinoma (HCC) is the sixth most prevalent cancer worldwide, but its aggressive nature makes it the third highest cause of cancer-related mortality.1–4 It affects ∼600 000 people annually, with the highest incidence rates in Sub-Saharan Africa and East Asia.3–5 However, in recent years, its incidence has also been increasing in developed regions, including North America and many European countries.6
There are sex disparities regarding the incidence of HCC, with a much higher rate in men. The role of sex hormones, including the protective role of oestrogen and the upregulation of androgen receptors in tumour tissues, may impact the development of HCC in men and women and differentially affects men.7–10 Although male sex has long been known to be a major risk factor for HCC and the natural history of HCC has been compared among patients with different aetiologies and ethnicities, the impact of sex on the presentation and natural history of HCC has not been studied extensively.8 9 11 As previously mentioned, it is known that HCC disproportionately affects men compared to women.12 Men are diagnosed with HCC with an average region-dependent ratio of 2:1 to 4:1 when compared to women.3 In certain regions of the world, this ratio is as high as 8.7:1.12 This is consistent with the finding that HCC is the second leading cause of worldwide cancer-related deaths among men and the sixth leading cause of cancer-related deaths among women.13 Notably, while HCC affects men more than women, the rate of HCC among women has been increasing, and it is important to understand its natural history in both sexes.12
Not only is HCC more prevalent among men, but its characteristics also vary by sex. Indeed, women are diagnosed with HCC at a significantly older age than men.11 14 Women are also more likely to be diagnosed by screening methods rather than symptomatically and while they are at an earlier stage of disease with fewer and smaller tumours.11 Finally, it has been proposed that female sex is prognostic for better overall survival, especially among younger cohorts, but results from limited studies are inconsistent.7 11 15
The purpose of our study is to examine disease aetiology, clinical presentation, treatment utilisation, and long-term overall survival in men and women already diagnosed with HCC.
Methods
Study design and patient population
This retrospective cohort study consists of 1886 consecutive adult HCC patients who were seen at Stanford University Medical Center from January 1998 to July 2015. An electronic query using International Classification of Diseases-9 (ICD-9) code was used to identify patients with HCC. Manual chart review was used to verify the diagnosis and to obtain demographic and clinical data of all patients. A National Death Index search and an individual chart review were used to obtain data for long-term survival, including the death date and the date of last contact. This study was approved by the Institutional Review Board at Stanford University, Stanford, California, USA.
To confirm HCC diagnosis, cytological or pathologic diagnosis from a tumour biopsy was used. If no tumour biopsy was obtained, non-invasive criteria recommended by the American Association for the Study of Liver Diseases using characteristic imaging on CT or MRI were used. Radiology and pathology reports were also reviewed to determine tumour characteristics, including size, number, and lobar involvement (tumours present in left, right, or both lobes). Demographic information from patients' charts, including age at HCC diagnosis, aetiology, baseline laboratory values, social history, co-morbidities, diagnosis scenario, and treatments received, were abstracted using a case report form. Events marking liver decompensation such as gastrointestinal bleed, ascites, and encephalopathy were also recorded.
Alcohol and tobacco uses were defined as any use of these substances prior to HCC diagnosis. Alcoholic aetiology was defined as prolonged alcohol abuse leading to the development of alcoholic cirrhosis. Hepatitis B status was determined by the presence of HBsAg, HBV DNA, or documented history of HBV infection. Hepatitis C status was determined by the presence of hepatitis C antibody (anti-HCV), HCV RNA, or documented history of HCV infection.
Diagnosis scenario was categorised as either via screening, symptomatic, or incidental. Screening refers to patients diagnosed on a routine imaging study, including those diagnosed by primary surveillance. Primary surveillance refers to screening in at-risk patients who have not yet developed cancer. ‘Symptomatic’ refers to patients who presented with symptoms such as hepatic decompensation, abdominal pain, fatigue, weight loss, jaundice, or other liver-related problems that ultimately lead to their diagnosis. ‘Incidental’ refers to asymptomatic patients who were found to have HCC while being examined for another, unrelated condition. Diagnosis via screening refers to diagnosis made by routine screening or surveillance tests as noted in clinical records.
Patients who received treatment were divided into two categories based on the primary treatment received: surgical or non-surgical. Primary treatment referred to the highest level of HCC treatment received by the patient, with the highest being liver transplant (OLT), followed by surgical resection, liver-directed therapy (transarterial chemoembolisation (TACE) and radiofrequency ablation (RFA)), and systemic therapy. The surgical group consisted of patients who received a resection or transplant as their primary HCC treatment. The non-surgical group consisted of patients who received liver-directed therapies or systemic therapy as their primary HCC treatment.
The Barcelona Clinic Liver Cancer (BCLC) staging system was used to determine the tumour stage, and eligibility for liver transplantation was assessed by the Milan criteria.16 17 The Child-Pugh-Turcotte (CPT) and Model for End-Stage Liver Disease (MELD) scores were used to determine the degree of decompensation and cirrhosis.18 19
Statistical analysis
The data analysis and statistical software, Stata/SE 11.1 (College Station, Texas, USA), was used to perform all analysis. Statistical significance was defined as a two-tailed p value of <0.05. The Student's t-test was used to analyse continuous variables. These variables were reported as a mean±SD if normally distributed or as a median and range if skewed. The χ2 test was used to analyse categorical variables. These variables were reported as a proportion (%) of the overall cohort.
The Kaplan–Meier method was used to approximate the overall survival, and the significance of survival differences between the sexes was determined using the log-rank test. Differences in survival among men and women within different diagnosis scenarios and aetiologies, including hepatitis B, hepatitis C, and non-viral diseases were also evaluated using the Kaplan-Meier method and log-rank test. A stepwise multivariate Cox proportional regression was used to estimate HRs with a 95% CI, which related patient survival to baseline predictors that were found to have a significant effect on survival during univariate analysis.
Results
Demographic and clinical laboratory characteristics
The demographic and clinical values of the patients are listed in table 1.
Table 1.
Demographic and clinical values, by sex
| Demographic and clinical values | Overall cohort (n=1886) | Females (n=437) | Males (n=1449) | p Value |
|---|---|---|---|---|
| Ethnicity (n=1870) | 0.05 | |||
| Asian | 792 (42.4%) | 192 (44.3%) | 600 (41.8%) | |
| White | 726 (38.8%) | 150 (34.6%) | 576 (40.1%) | |
| Hispanic | 292 (15.6%) | 69 (15.9%) | 223 (15.5%) | |
| Black | 31 (1.7%) | 12 (2.8%) | 19 (1.3%) | |
| Other | 29 (1.6%) | 10 (2.3%) | 19 (1.3%) | |
| Aetiology | ||||
| Age at HCC diagnosis (n=1886) | 60.8±11.1 | 64.0±11.6 | 59.9±10.7 | <0.0001 |
| BMI (n=744) | 26.5±5.7 | 26.1±6.3 | 26.6±5.6 | 0.30 |
| History of alcohol use (n=1838) | 1040 (56.6%) | 150 (35.1%) | 890 (63.2%) | <0.001 |
| History of tobacco use (n=1854) | 954 (51.5%) | 132 (31.0%) | 822 (57.7%) | <0.001 |
| HCV (n=1886) | 914 (48.5%) | 224 (51.3%) | 690 (47.6%) | 0.18 |
| Asian HCV (n=789) | 271 (34.4%) | 85 (44.5%) | 186 (31.1%) | 0.001 |
| Non-Asian HCV (n=1097) | 642 (58.6%) | 139 (56.5%) | 503 (59.3%) | 0.45 |
| HBV (n=1886) | 446 (23.7%) | 90 (20.6%) | 356 (24.6%) | 0.09 |
| Asian HBV (n=789) | 415 (52.6%) | 83 (43.5%) | 332 (55.5%) | 0.004 |
| Non-Asian HBV (n=1097) | 31 (2.8%) | 7 (2.9%) | 24 (2.8%) | 0.98 |
| Alcoholic liver disease (n=1781) | 114 (6.4%) | 14 (3.5%) | 100 (7.3%) | 0.006 |
| Co-morbidities | ||||
| HTN (n=1666) | 821 (49.3%) | 200 (51.8%) | 621 (48.5%) | 0.26 |
| Hyperlipidaemia (n=1664) | 209 (12.6%) | 46 (11.9%) | 163 (12.8%) | 0.66 |
| DM (n=1670) | 520 (31.1%) | 118 (30.6%) | 402 (31.3%) | 0.78 |
| CAD (n=1665) | 114 (6.9%) | 24 (6.2%) | 90 (7.0%) | 0.58 |
| COPD (n=1666) | 57 (3.4%) | 16 (4.2%) | 41 (3.2%) | 0.37 |
| Advanced liver disease | ||||
| Cirrhosis (n=1886) | 1572 (83.4%) | 366 (83.8%) | 1206 (83.2%) | 0.80 |
| Ascites (n=1869) | 674 (36.1%) | 167 (38.6%) | 507 (35.3%) | 0.20 |
| Encephalopathy (n=1864) | 354 (19.0%) | 89 (20.7%) | 265 (18.5%) | 0.32 |
| GI bleed (n=1325) | 332 (25.1%) | 68 (21.4%) | 264 (26.2%) | 0.08 |
| Decompensation (n=1886) | 862 (45.7%) | 194 (44.4%) | 668 (46.1%) | 0.53 |
Bolded p values indicate significant difference (p<0.05).
ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CR, creatinine; DM, diabetes mellitus; GI, gastrointestinal; HCC, hepatocellular carcinoma; HCV, chronic hepatitis C; HBV, chronic hepatitis B; HGB, haemoglobin; HTN, hypertension; INR, international normalised ratio; PLT, platelet; TB, tuberculosis.
The cohort consisted of 1449 male HCC patients and 437 female HCC patients. Overall, 792 patients were Asian, 726 were white, 292 were Hispanic, 31 were black, 29 were other, and 16 were unknown. The male cohort had a significantly younger age of HCC diagnosis than the female cohort (59.9±10.7 vs 64.0±11.6 years, p<0.0001). There were no significant differences in men and women with regard to body mass index (BMI) at presentation (26.6±5.6 vs 26.1±6.3, p=0.30) or the presence of co-morbidities such as diabetes mellitus (31.3% vs 30.6%, p=0.78), hypertension (48.5% vs 51.8%, p=0.26), coronary artery disease (7.0% vs 6.2%, p=0.58), chronic obstructive pulmonary disease (3.2% vs 4.2%, p=0.37), or hyperlipidaemia (12.8% vs 11.9%, p=0.66).
In terms of HCC aetiologies, the proportions of men and women with chronic hepatitis B (24.6% vs 20.6%, p=0.09) and chronic hepatitis C (47.6% vs 51.3%, p=0.18) were similar. However, when the sexes were subdivided into Asian and Non-Asian groups, Asian women were found to have significantly higher levels of chronic hepatitis C (44.5% vs 31.1%, p=0.001), whereas Asian men were found to have significantly higher levels of chronic hepatitis B (24.6% vs 20.6%, p=0.004). The male cohort displayed significantly higher rates of tobacco use (57.7% vs 31.0%, p<0.001) as well as alcohol use (63.2% vs 35.1%, p<0.001). The vast majority of patients, both men and women, presented with cirrhosis (83.2% vs 83.8%, p=0.80), and there were similar rates of decompensation manifested with the presence of ascites (35.3% vs 38.6%, p=0.20), encephalopathy (18.5% vs 20.7%, p=0.32), and gastrointestinal bleed (26.2% vs 21.4%, p=0.08) between the groups.
Baseline laboratory values
The baseline laboratory values and measures of liver disease severity with CPT and MELD scores are shown in table 2.
Table 2.
Baseline laboratory values, by sex
| Laboratory values | Overall cohort (n=1886) | Females (n=437) | Males (n=1449) | p Value |
|---|---|---|---|---|
| AFP (n=1478) | 41 (1–7 400 000) | 60 (1–7 400 000) | 38 (1–1 194 376) | 0.05 |
| HGB (n=1417) | 13.2 (4.7 to 18) | 12.5 (4.7 to 16.1) | 13.5 (5.2 to 18) | <0.0001 |
| PLT (n=1689) | 119 (17–693) | 111 (28–693) | 123 (17–664) | 0.09 |
| CR (n=1661) | 0.93 (0.39–8.5) | 0.8 (0.4–6.8) | 1 (0.39–8.5) | <0.0001 |
| TB (n=1696) | 1.1 (0–41.4) | 1.1 (0.2–25.8) | 1.2 (0–41.4) | 0.08 |
| ALB (n=1677) | 3.3 (0.5–5) | 3.3 (1.1–4.5) | 3.3 (0.5-5) | 0.25 |
| ALT (n=1540) | 66 (6–1349) | 60 (13–458) | 68 (6–1349) | 0.006 |
| AST (n=1547) | 82 (12–2198) | 79 (12–1076) | 83 (14–2198) | 0.30 |
| INR (n=1529) | 1.2 (0.7–6.1) | 1.2 (0.9–6.1) | 1.2 (0.7–5.5) | 0.22 |
| MELD (n=1461) | 10.3 (6.4–50.2) | 10.2 (6.4–50.2) | 10.3 (6.4–45.4) | 0.21 |
| CPT (n=1450) | 0.79 | |||
| Class A | 718 (49.5%) | 163 (48.1%) | 555 (50.0%) | |
| Class B | 556 (38.3%) | 132 (38.9%) | 424 (38.2%) | |
| Class C | 176 (12.2%) | 44 (13.0%) | 132 (11.9%) |
Bolded p values indicate significant difference (p<0.05).
AFP, α-fetoprotein; ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CAD, coronary artery disease; COPD, chronic obstructive pulmonary disease; CPT, Child-Pugh-Turcotte score; CR, creatinine; DM, diabetes mellitus; GI, gastrointestinal; HGB, haemoglobin; HTN, hypertension; INR, international normalised ratio; MELD, Model for End-Stage Liver Disease; PLT, platelet; TB, tuberculosis.
Women had lower values than men for haemoglobin (12.5 (4.7–16.1) vs 13.5 (5.2–18), p<0.0001), creatinine (0.8 (0.4–6.8) vs 1 (0.39–8.5), p<0.0001), and ALT (60 (13–458) vs 68 (6–1349), p<0.006). Men were found to have lower α-fetoprotein (AFP) levels than women (38 (1–1 194 376) vs 60 (1–7 400 000), p=0.05).
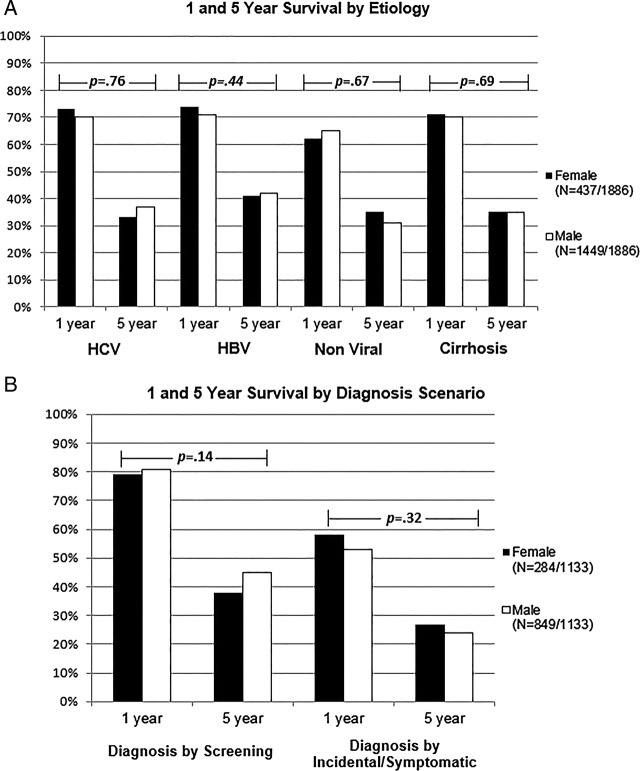
Diagnosis scenario
The diagnosis scenario for men and women is depicted in figure 1. Women were more likely than men to be diagnosed by routine screening versus symptomatically or incidentally (65.5% vs 58.2%, p=0.03). Furthermore, there was a trend indicating that women were more likely to be diagnosed while still asymptomatic than men (75.7% vs 70.4%, p=0.09).
Figure 1.
Proportion of HCC patients presenting without symptoms or via screening/surveillance, by sex. Asymptomatic diagnosis includes patients diagnosed by screening/surveillance or incidentally. HCC, hepatocellular carcinoma.
Tumour characteristics
The tumour characteristics from the radiographic imaging studies obtained at the time of HCC diagnosis are provided in table 3.
Table 3.
Tumour characteristics, by sex
| Tumour characteristics | Overall cohort (n=1886) | Females (n=437) | Males (n=1499) | p Value |
|---|---|---|---|---|
| Within Milan (n=1882) | 823 (43.7%) | 225 (51.6%) | 598 (41.4%) | <0.001 |
| Vascular invasion (n=1715) | 191 (11.1%) | 36 (8.8%) | 155 (11.9%) | 0.08 |
| BCLC (n=1004) | <0.001 | |||
| Class A | 455 (45.3%) | 137 (56.2%) | 318 (41.8%) | |
| Class B | 248 (24.7%) | 42 (17.2%) | 206 (27.1%) | |
| Class C/D | 301 (29.9%) | 65 (26.8%) | 236 (31.1%) | |
| Maximum tumour diameter (n=1767) | 3.7 (0.38–21.1) | 3.2 (0.6–20.1) | 3.8 (0.38–21.1) | 0.001 |
| Tumour ≥5 cm (n=1886) | 709 (37.6%) | 132 (30.2%) | 577 (39.8%) | 0.001 |
| Unifocal (n=1823) | 991 (54.4%) | 241 (56.6%) | 750 (53.7%) | 0.32 |
| Number of tumours (n=1823) | 0.040 | |||
| 1–2 | 1342 (73.6%) | 331 (77.5%) | 1011 (72.4%) | |
| ≥3 | 481 (26.4%) | 96 (22.5%) | 385 (27.6%) | |
| Lobar involvement (n=1525) | 0.57 | |||
| Left lobe | 453 (29.7%) | 105 (28.8%) | 348 (30.0%) | |
| Right lobe | 809 (53.1%) | 202 (55.3%) | 607 (52.3%) | |
| Both lobes | 263 (17.3%) | 58 (15.9%) | 205 (17.7%) |
Bolded p values indicate significant difference (p<0.05).
AFP, α-fetoprotein; BCLC, Barcelona Clinic Liver Cancer staging classification.
Men were more likely to present with tumours larger than 5 cm (39.8% vs 30.2%, p=0.001) and had larger maximum tumour sizes (3.8 cm (0.38–21.1) vs 3.2 cm (0.6–20.1), p=0.001). They also were more likely than women to present with three or more tumours (27.6% vs 22.5%, p=0.04). In addition, women presented with higher proportions of early-stage BCLC class A disease (56.2% vs 41.8%, p<0.001) and were more likely to be within the Milan liver transplant criteria (51.6% vs 41.4%, p=<0.001). There was no significant difference in tumour lobar involvement.
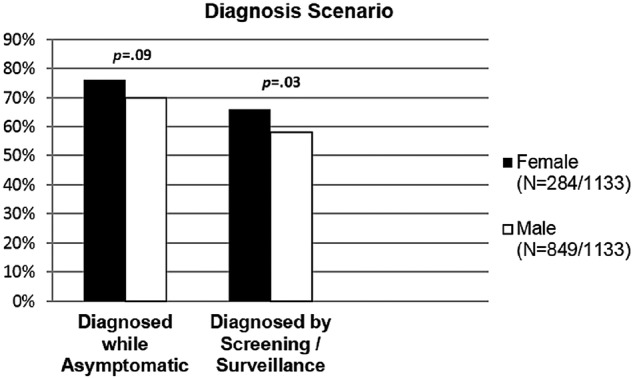
HCC treatment outcomes
The primary treatments received by the cohorts are shown in figure 2. The proportion of men and women who did not receive any treatment for their HCC was similar (24.2% vs 24.3%, p=0.99). For those who did receive treatment, there was no significant difference in the type of primary treatment received by the two cohorts. As their primary HCC treatment, women and men underwent liver transplantation (12.1% vs 13.8%, p=0.56), resection (14.2% vs 14.0%, p=0.38), chemoembolisation (43.9% vs 41.8%, p=0.43), RFA (1.8% vs 1.9%, p=0.96), and other systemic treatments, including sorafenib (3.7% vs 4.4%, p=0.52) at similar rates. Similarly, there was no difference between the number of men and women receiving surgical treatments (26.3% vs 27.8%, p=0.56) as their primary HCC treatment. There was an equal percentage of men and women listed for liver transplantation (30.8% vs 29.9%, p=0.72) and who received liver transplantation (14.8% vs 13.7%, p=0.59) at any point after their HCC diagnosis.
Figure 2.
Treatment utilisation in patients with HCC, by sex. Primary treatment refers to the highest level of HCC treatment received by the patient, with the highest being liver transplant, followed by surgical resection, liver-directed therapy (TACE and RFA), and systemic therapy. HCC, hepatocellular carcinoma; OLT, orthotopic liver transplantation; TACE, transartial chemoembolisation; RFA, radiofrequency ablation.
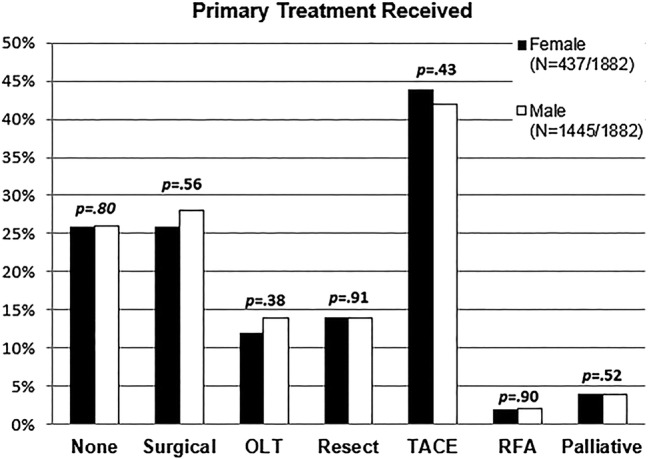
Long-term overall survival and predictors of survival
Figure 3 depicts the overall survival of the cohorts. There was no significant difference in median survival between the male and female cohorts from the time of HCC diagnosis (median 30.7 (24.5–41.3) vs 33.1 (27.4–37.3) months, p=0.84). However, a significantly higher proportion of women were found to have extended long-term 10–15-year survival rate with 10-year survival in women versus men of 25.4% (19.9% to 31.3%) vs 23.5% (20.5% to 26.6%) and 15-year survival in women versus men of 23.4% (17.8% to 29.5%) vs 15.5% (12.1% to 19.3%); p=0.04.
Figure 3.
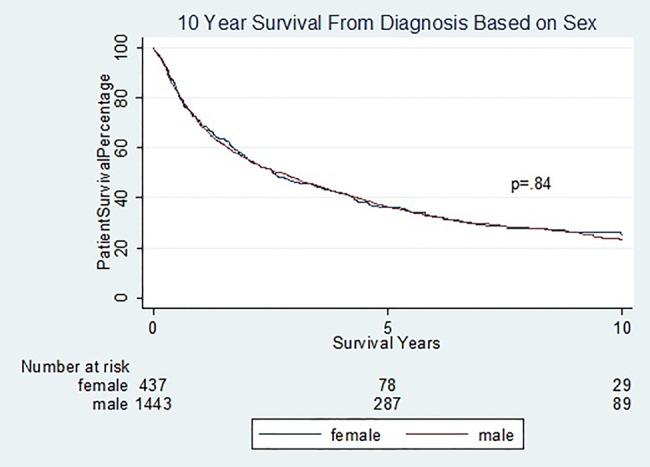
Overall survival of HCC patients, by sex. HCC, hepatocellular carcinoma.
There were no significant differences in 1-year and 5-year survival when men were compared to women on subgroups by aetiologies viral (HBV+HCV) (37.4% vs 36.7%, p=0.76), HBV (41.6% vs 41.4%, p=0.44), HCV (36.7% vs 33.2%, p=0.38), presence of cirrhosis (35.3% vs 35.4%, p=0.74), rates of diagnosis via screening (44.9% vs 38.3%, p=0.14), and rates of symptomatic/incidental diagnosis (24.4% vs 27.0%, p=0.32). These results are depicted in figure 4A,B. However, patients diagnosed by screening had higher median survival than those diagnosed symptomatically or incidentally in both sexes (median 45.0 (range 37.4–56.6) vs 15.0 (range11.8–19.3) months, p<0.0001).
Figure 4.
(A) Cumulative 1-year and 5-year overall survival by aetiologies of underlying liver disease, by sex. HCV, chronic hepatitis C; HBV, chronic hepatitis B; non-viral, alcoholic liver disease, non-alcoholic fatty liver disease, autoimmune, and metabolic liver diseases. (B) Cumulative 1-year and 5-year overall survival by diagnosis scenario, by sex.
Univariate and multivariate analyses were used to identify predictors for a better long-term survival. These results are provided in table 4.
Table 4.
Predictors for overall survival
| Univariate (n=1880) |
Multivariate (n=922) |
|||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Male sex (n=1880) | 1.04 | 0.90 to 1.20 | 0.61 | 1.01 | 0.82 to 1.24 | 0.94 |
| Age at HCC diagnosis (n=1880) | 1.01 | 1.01 to 1.02 | <0.001 | 1.02 | 1.01 to 1.03 | <0.001 |
| Non-surgical first treatment (n=1874) | 0.38 | 0.33 to 0.43 | <0.001 | 0.41 | 0.34 to 0.50 | <0.001 |
| Surgical first treatment (n=1874) | 0.20 | 0.16 to 0.25 | <0.001 | 0.24 | 0.16 to 0.35 | <0.001 |
| No screening (n=1132) | 1.98 | 1.69 to 2.33 | <0.001 | 1.48 | 1.23 to 1.79 | <0.001 |
| Cirrhosis (n=1880) | 1.10 | 0.93 to 1.28 | 0.27 | 1.02 | 0.73 to 1.44 | 0.89 |
| Milan (n=1880) | 0.51 | 0.45 to 0.57 | <0.001 | 0.54 | 0.44 to 0.65 | <0.001 |
| MELD (n=1458) | 1.06 | 1.05 to 1.07 | <0.001 | 1.06 | 1.05 to 1.08 | <0.001 |
| Asian (n=1870) | 0.78 | 0.69 to 0.88 | <0.001 | |||
| OLT (n=1868) | 0.21 | 0.17 to 0.27 | <0.001 | |||
| CPT (n=1446) | 1.52 | 1.39 to 1.67 | <0.001 | |||
| BCLC (n=1003) | 1.79 | 1.62 to 1.98 | <0.001 | |||
Bolded p values indicate significant differences (p<0.05).
BCLC, Barcelona Clinic Liver Cancer staging classification; CPT, Child-Pugh-Turcotte score; HCC, hepatocellular carcinoma; MELD, Model for End-Stage Liver Disease; OLT, orthotopic liver transplantation.
On univariate analysis, younger age, Asian ethnicity, absence of cirrhosis, liver transplantation, surgical therapy (vs non-surgical), lower MELD score, lower CPT score, lower BCLC staging, and meeting Milan criteria were significant predictors for improved survival for patients. After using multivariate analysis to adjust for age at HCC diagnosis, male sex, treatment (surgical, non-surgical vs none), diagnosis scenario (screening vs symptomatic or incidental diagnosis), cirrhosis, tumour within Milan criteria, and MELD score, significant independent predictors for better survival included younger age at HCC diagnosis, surgical treatment, non-surgical treatment, diagnosis by screening, tumour within Milan criteria, and lower MELD score.
Discussion
It is well known that men are diagnosed with HCC at a much higher rate than women, which suggests higher HCC risk in men.3 12 Although past studies have explored the impact of sex on the development of HCC in at-risk patients, there is a lack of studies analysing sex differences among patients who have already been diagnosed with HCC.6–8 Furthermore, among studies that have addressed this question, the results are inconclusive.11 20–23
The current study helps address this area of controversy by analysing sex differences in the presentation, progression, and long-term outcomes of a large, well-characterised consecutive cohort of HCC patients seen at a university medical centre. There was no significant difference in overall survival between men and women, and sex was not found to be an independent predictor of survival on either univariate or multivariate analysis. However, important differences in the presentation of male and female patients were found.
On diagnosis, men had more advanced liver disease with larger and more numerous tumours. This may result from men being less frequently diagnosed by routine screening. This allowed their HCC to progress further before being detected either symptomatically or incidentally. Diagnosis of HCC at an early stage has been shown to improve survival outcomes, likely because more curative treatment options would be available at early stage.7 24 25 This is supported by result of the current study, which found that survival was markedly longer in patients diagnosed via screening compared to survival in those diagnosed symptomatically or incidentally, irrespective of sex.
Compliance to screening recommendations is a modifiable factor and should be emphasised in all at-risk patients, especially men. While the older age at HCC diagnosis and higher rates of diagnosis by screening in female patients may suggest that women have more access to care than men, we believe that failure to adhere to screening recommendations can also be due to poor communication between physicians and patients, patient non-compliance, or physician non-adherence to HCC screening and surveillance recommendations. Underlying factors accounting for reduced screening adherence in men should be further studied.
Women in the current study were significantly older than their male counterparts at the time of diagnosis. This suggests that female sex may play a protective role, preventing HCC from developing in women until later in life. Women may have also been diagnosed at a younger age and with earlier disease stage than men because they may have been more compliant with HCC screening/surveillance. However, while age was found to be an independent predictor for survival in the current study as in several past studies, sex was not.
In addition, one would expect women, who on average present with earlier disease stage, to undergo more liver transplantation and curative resection. However, this is not the case in our study. Despite men having a higher tumour burden, men and women received curative HCC treatments at the same rate. This suggests a disparity between how men and women are being treated. Women may be being offered different treatment options based on either their older age at diagnosis or their female sex. The older age of women may result in curative treatment options being less desirable or practical to the patient and the physician. On the other hand, one cannot exclude the possibility that women are being treated less aggressively based solely on the basis of their sex.26
Another interesting observation was the finding that there were more Asian men with HBV-related HCC and more Asian women with HCV-related HCC. This is consistent with prior studies that have shown that the majority of Asian HBV-related HCC patients are male, while the percentage of women in HCV-related HCC cohorts is generally higher than the percentage of women in western cohorts.27 This is likely due to the iatrogenic mode of transmission of HCV in developing countries, and women may be more likely to be exposed to blood and blood products due to childbirth.28
One of the limitations of this study is its retrospective nature. However, our study focused on objective variables such as age, sex, treatments received, tumour characteristics, and long-term survival outcomes which are clearly documented in patients' histories and obtained through manual, individual chart review and verified by the National Death Index database. In addition, since the majority of the study patients had either HBV or HCV infection (72%), results of this study may not be generalisable for HCC patients of non-viral aetiologies, especially alcoholic liver disease which was uncommon at only 6% in the study population of this study.
Conclusion
Male sex has long been known to be a major risk factor for HCC among at-risk patients. However, among those already diagnosed with HCC, there were no significant differences in long-term survival outcomes between the sexes. Women were diagnosed at a significantly older age than men. Women were also more likely to be diagnosed via screening without symptoms and to present with lower tumour stage. Older age, advanced tumour stage, no screening history, and received surgical or palliative therapy were significant independent predictors of survival, but sex was not. There are two modifiable disparities between the sexes that may lead to better survival if targeted. The first is the lower rate of diagnosis via screening in men. The second is the lower rates of surgical treatment in women for similar tumour stage as men. Further studies are needed to examine factors contributing to such disparities.
Footnotes
Contributors: MRL participated in study design; performed data collection, data analysis, and data interpretation; and drafted the manuscript. NGK and PN contributed to data collection, data interpretation, and critical review of the manuscript. MLS and GG participated in data review and interpretation and critical review of the manuscript. MHN conceived the study; developed study design and data analysis plan; and participated in data collection, data interpretation, and critical revision of the manuscript.
Competing interests: None declared.
Ethics approval: Stanford University Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Jemal A, Bray F, Center MM, et al. Global cancer statistics. Cancer J Clin 2011;61:69–90. doi:10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11. Lyon, France: International Agency for Research on Cancer, 2013. [Google Scholar]
- 3.Schutte K, Bornschein J, Malfertheiner P. Hepatocellular carcinoma—epidemiological trends and risk factors. Dig Dis 2009;27:80–92. [DOI] [PubMed] [Google Scholar]
- 4.Yang JD, Roberts LR. Epidemiology and management of hepatocellular carcinoma. Infect Dis Clin North Am 2010; 24:899–919. doi:10.1016/j.idc.2010.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Venook A, Papandreou C, Furuse J, et al. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 2010;15:5–13. doi:10.1634/theoncologist.2010-S4-05 [DOI] [PubMed] [Google Scholar]
- 6.Evans AA, Chen G, Ross EA, et al. Eight-year follow-up of the 90,000-person Haimen City cohort: I. Hepatocellular carcinoma mortality, risk factors, and gender differences. Cancer Epidemiol Biomarkers Pre 2002;11:369–76. [PubMed] [Google Scholar]
- 7.Dohmen K, Shigematsu H, Irie K, et al. Longer survival in female than male with hepatocellular carcinoma. J Gastroenterol Hepatol 2003;18:267–72. doi:10.1046/j.1440-1746.2003.02936.x [DOI] [PubMed] [Google Scholar]
- 8.Naugler WE, Sakurai T, Kim S. Gender disparity in liver cancer due to sex differences in MyD88-dependent IL-6 production. Science 2007;317:121–4. doi:10.1126/science.1140485 [DOI] [PubMed] [Google Scholar]
- 9.Giannitrapani L, Soresi M, La Spada E, et al. Sex hormones and risk of liver tumor. Ann N Y Acad Sci 2006;1089:228–36. doi:10.1196/annals.1386.044 [DOI] [PubMed] [Google Scholar]
- 10.Nagasue N, Kohno H, Chang YC, et al. Androgen and estrogen receptors in hepatocellular carcinoma and the surrounding liver in woman. Cancer 1989;63:112–16. doi:10.1002/1097-0142(19890101)63:1<112::AID-CNCR2820630118>3.0.CO;2-P [DOI] [PubMed] [Google Scholar]
- 11.Farinati F, Sergio A, Giacomin A, et al. Is female sex a significant favorable prognostic factor in hepatocellular carcinoma? Eur J Gastroenterol Hepatol 2009;21:1212–18. doi:10.1097/MEG.0b013e32831a86f8 [DOI] [PubMed] [Google Scholar]
- 12.Lam CM, Yong JL, Chan AO, et al. Better survival in female patients with hepatocellular carcinoma: oral contraceptive pills related? J Clin Gastroentero 2005;39:533–9. doi:10.1097/01.mcg.0000165670.25272.46 [DOI] [PubMed] [Google Scholar]
- 13.Torre L, Bray F, Siegal R, et al. Global cancer statistics, 2012. CA 2015;65:87–108. [DOI] [PubMed] [Google Scholar]
- 14.Yang D, Hanna DL, Usher J, et al. Impact of sex on the survival of patients with hepatocellular carcinoma: a surveillance, epidemiology, and end results analysis. Cancer 2014;120:3707–16. doi:10.1002/cncr.28912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen WT, Chau GY, Lui WY, et al. Recurrent hepatocellular carcinoma after hepatic resection: prognostic factors and long-term outcome. Eur J Surg Oncol 2004;30:414–20. doi:10.1016/j.ejso.2004.01.013 [DOI] [PubMed] [Google Scholar]
- 16.Forner A, Reig ME, de Lope R, et al. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis 2010;30:61–74. doi:10.1055/s-0030-1247133 [DOI] [PubMed] [Google Scholar]
- 17.Yao FY. Liver transplantation for hepatocellular carcinoma: beyond the Milan criteria. Am J Transplant 2008;8:1982–9. doi:10.1111/j.1600-6143.2008.02351.x [DOI] [PubMed] [Google Scholar]
- 18.Christensen E. Prognostic models including the Child-Pugh, MELD and Mayo risk scores—where are we and where should we go? J Hepatol 2004;41:344–50. doi:10.1016/j.jhep.2004.06.005 [DOI] [PubMed] [Google Scholar]
- 19.Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology 2001;33:464–70. doi:10.1053/jhep.2001.22172 [DOI] [PubMed] [Google Scholar]
- 20.El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007;132:2557–76. doi:10.1053/j.gastro.2007.04.061 [DOI] [PubMed] [Google Scholar]
- 21.Buch SC, Kondragunta V, Branch RA, et al. Gender-based outcomes differences in unresectable hepatocellular carcinoma. Hepatol Int 2008;2:95–101. doi:10.1007/s12072-007-9041-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akashi Y, Koreeda C, Enomoto S, et al. Prognosis of unresectable hepatocellular carcinoma: an evaluation based on multivariate analysis of 90 cases. Hepatology 1991;14:262–8. doi:10.1002/hep.1840140210 [PubMed] [Google Scholar]
- 23.Tangkijvanich P, Mahachai V, Suwangool P, et al. Gender difference in clinicopathologic features and survival of patients with hepatocellular carcinoma. World J Gastroenterol 2004;10:1547–50. doi:10.3748/wjg.v10.i11.1547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yuen MF, Cheng CC, Lauder IJ, et al. Early detection of hepatocellular carcinoma increases the chance of treatment: Hong Kong experience. Hepatology 2000;31:330–5. doi:10.1002/hep.510310211 [DOI] [PubMed] [Google Scholar]
- 25.Dohmen K, Shirahama M, Ishibashi H, et al. Differences in survival based on the type of follow-up for the detection of hepatocellular carcinoma: an analysis of 547 patients. Hepatol Res 2000;18:110–21. doi:10.1016/S1386-6346(99)00094-7 [DOI] [PubMed] [Google Scholar]
- 26.Altekruse SF, McGlynn KA, Dickie LA, et al. Hepatocellular carcinoma confirmation, treatment, and survival in surveillance, epidemiology, and end results registries 1992–2008. Hepatology 2012;55:476–82. doi:10.1002/hep.24710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yip B, Wantuck JM, Kim LH, et al. Clinical presentation and survival of Asian and non-Asian Patients with HCV-related hepatocellular carcinoma. Dig Dis Sci 2014;59:192–200. doi:10.1007/s10620-013-2948-7 [DOI] [PubMed] [Google Scholar]
- 28.Kin CK, Lin B, Ha NB, et al. High prevalence of hepatitis C virus in community Asian American patients with non-liver related complaints. J Clin Gastroenterol 2013;47:367–71. doi:10.1097/MCG.0b013e3182688b3e [DOI] [PubMed] [Google Scholar]