Abstract
Cytomegalovirus (CMV) infection is the most common viral opportunistic infection in immunocompromised patients and is a rare cause of bowel perforation. It invariably requires surgical intervention and is often fatal. We report a 50-year-old Caucasian man with AIDS, presented 3 weeks after developing abdominal pain and distension. He was treated for CMV retinitis in the past. His adherence to antiretroviral therapy was poor. Examination revealed a recurrence of active CMV retinitis. His abdomen was tender and distended. The plain X-ray of the abdomen revealed a double wall sign (Rigler's sign), indicating pneumoperitoneum due to the bowel perforation. The upper endoscopy was normal. His CD4 count was 30 cells/mm3. He was treated with cidofovir infusion. He made a full recovery, without requiring any form of surgery. However, he died of adult respiratory distress syndrome 14 months later, due to iatrogenic acute pancreatitis.
Background
Cytomegalovirus (CMV) infection is the most common viral opportunistic infection, but it is a rare cause of the bowel perforation in immunocompromised patients (including in patients with HIV-positive).1 2 They invariably require surgical interventions and are often fatal.
We report a case of a 50-year-old Caucasian man who presented 3 weeks after the onset of symptoms of bowel perforation, which was confirmed by a plain X-ray of the abdomen when pneumoperitoneum (Rigler's sign) was found. Funduscopy revealed an old CMV retinitis scar and new lesions of active recurrence of CMV retinitis.
Our patient responded to medical treatment and went home without any surgical interventions. In addition, the double wall sign (Rigler's sign) is a radiological feature of pneumoperitoneum, due to bowel perforation.
To the best of our knowledge, no similar case report has been published.
Case presentation
A 50-year-old Caucasian man was treated for CMV retinitis with cidofovir infusion in 2000. He was diagnosed with HIV infection when he presented with cavitating pulmonary tuberculosis in 1995. Later, he developed non-invasive pulmonary aspergilloma.3 CMV retinitis healed 6 months after the treatment. His adherence to antiretroviral therapy (ART) was poor. In 2001, he developed abdominal pain and distension for 3 weeks but did not seek medical advice promptly. Examination of the right fundus revealed scarring of old CMV retinitis, plus a new active CMV retinitis (figure 1). His abdomen was diffusely tender and distended. He was again treated with cidofovir infusion. He was also administered intravenous fluids and broad-spectrum antibiotics. He was kept nil by mouth for 4 days. He recovered fully and went home 3 weeks after the hospital admission. He did not require any operative management of bowel perforation.
Figure 1.
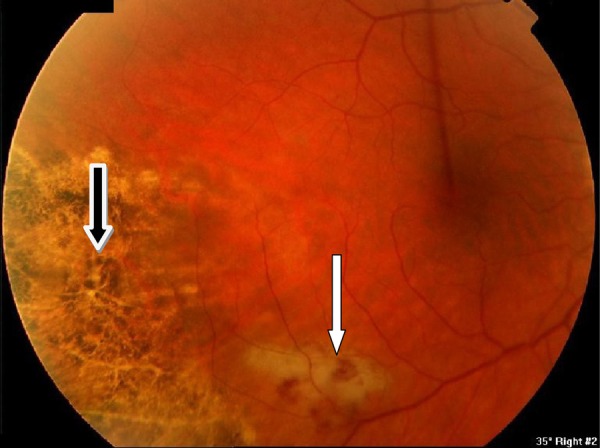
Funduscopy showing scarring of old CMV retinitis (black arrow) and a new active CMV retinitis (white arrow).
Investigations
The plain X-ray of the abdomen showed a double wall sign (Rigler's sign), indicating pneumoperitoneum (figure 2). Upper endoscopy was performed to exclude perforation of the upper intestinal tract. Results were normal. His CD4 count was 30 cells/mm3. Plasma CMV PCR was not performed as it was not available at the time.
Figure 2.
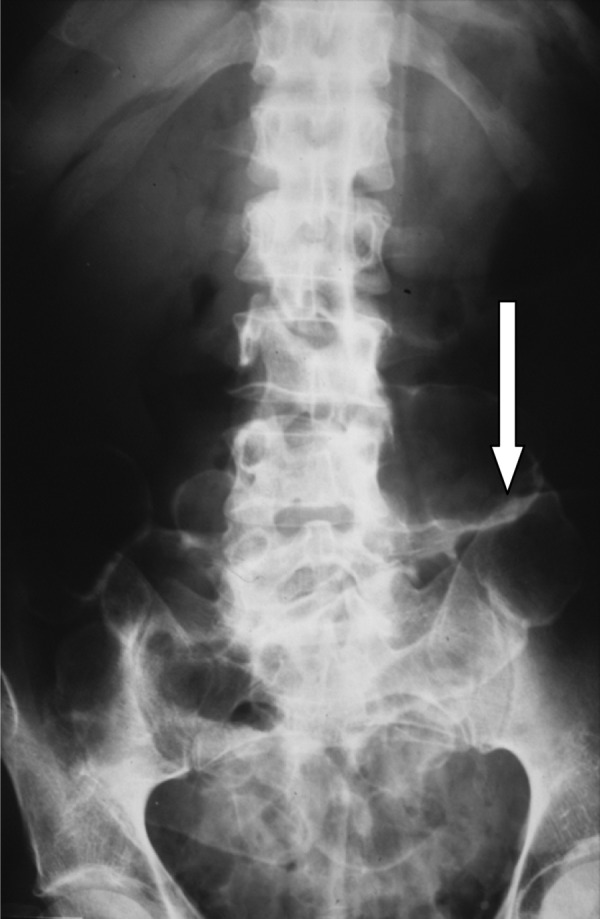
The plain X-ray of the abdomen showing the double wall sign (Rigler's sign) due to pneumoperitoneum.
Outcome and follow-up
In January 2002, his ART was changed following an HIV genotype testing to stavudine, didanosine (250 mg) and tenofovir, as his CD4 count was 20 cell/mm3 and his HIV RNA level was 194×103 copies/mL. He was admitted a month later with nausea, vomiting and abdominal pain. His serum amylase was 3972 U/L. He was managed conservatively but died of adult respiratory distress syndrome due to iatrogenic acute pancreatitis.
Discussion
Disseminated CMV is the most common viral opportunistic infection in an HIV population. It is particularly seen in patients with a CD4 count of <50 cells/mm3, as in our patient.4 The commonly involved organs are the retina, the gastrointestinal tract, the lungs, the nervous system and the adrenal glands. The colon is the most frequently involved site in the gastrointestinal tract; however, it can affect virtually any site from the mouth to the anus.5 Abdominal pain, diarrhoea, fever and weight loss are typical features. However, lower gastrointestinal tract bleeding without diarrhoea may be the initial manifestation of CMV colitis in patients with AIDS.6 Our patient developed recurrent CMV retinitis when his CD4 count was <50 cells/mm3, due to his poor adherence to ART. At the same time, he presented with lower bowel perforation as evidenced by the double wall sign (Rigler's sign). His upper endoscopy was normal. He was referred to a surgical team which decided not to operate following clinical evaluation, as he was haemodynamically stable. The surgical outcome is frequently poor in such groups with CD4 counts of this level. He responded well to anti-CMV treatment. These findings (low CD4 counts, evidence of active CMV infection and the response to anti-CMV treatment) strongly suggest that CMV infection was the cause of his bowel perforation. However, definitive diagnosis is made by mucosal biopsies showing large cells with CMV inclusion in the nucleus. This diagnosis is further augmented by immunochemistry in situ hybridisation, and by a PCR.7 No biopsy was performed as our patient did not undergo laparotomy.
The pathogenesis of CMV infection of the gut is thought to be due to submucosal vasculitis, leading to thrombosis and ischaemia, which result in ulceration, gangrene and perforation. The most common site of perforation due to CMV infection involves the area between the ileum and the splenic flexure of the colon.8 CMV infection often affects multiple sites in the gastrointestinal tract. Surgery for intestinal perforation involves segmental resection. Primary anastomosis of bowels is not recommended. Therefore, such patients often need colostomies or ileostomies.9 Toxic megacolon due to CMV infection has rarely been reported.10
The double wall sign (Rigler's sign) was first described by Leo George Rigler in 1942. It is a radiological finding of pneumoperitoneum outlining the bowel wall by the presence of air inside and outside the bowel wall. It is seen when there is a litre or more of air in the peritoneum.11
Learning points.
CMV infection is the most common viral opportunistic infection in patients with HIV who are severely immunocompromised, with CD4 counts <50 cells/mm3.
It is a rare cause of perforation of the bowel in patients with AIDS, and often involves the area between the ileum and the splenic flexure of the colon.
The double wall sign (Rigler's sign) is a feature of pneumoperitoneum due to bowel perforation.
CMV infection often affects multiple sites. Surgery involves segmental resection. Hence, primary anastomosis of bowels is not recommended, and such patients often need colostomies or ileostomies.
Surgical intervention is not always necessary in the management of CMV infection causing bowel perforation, as in our case.
Footnotes
Contributors: KTY started writing this case report when she was doing a student selected component at her final year in Cardiff University. She completed F1 and F2 and is now a student doing clinical MSc at Queen’s square, London. ARM was involved in this patient's care.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Chamberlain RS, Atkins S, Saini N et al. Ileal perforation caused by cytomegalovirus infection in a critically ill adult. J Clin Gastroenterol 2000;30:432–5. 10.1097/00004836-200006000-00016 [DOI] [PubMed] [Google Scholar]
- 2.Milanchi S, Wood D. Rigler's sign in a patient with massive pneumoperitoneum. Emerg Med J 2006;23:884 10.1136/emj.2006.039651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoganathan K. Long-term suppressive therapy for pulmonary aspergilloma in an immunocompromised man with AIDS. Is it always necessary? Int J STD AIDS 2009;20:434–6. 10.1258/ijsa.2008.008341 [DOI] [PubMed] [Google Scholar]
- 4.Yoganathan K, Austin K. Ischaemic maculopathy in zidovudine-induced anemia in an HIV-positive man. Clin Ophthalmol 2008;2:237–9. 10.2147/OPTH.S2449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacobson MA, O'Donnell JJ, Porteous D et al. Retinal and gastrointestinal disease due to cytomegalovirus in patients with the acquired immune deficiency syndrome: prevalence, natural history, and response to ganciclovir therapy. Q J Med 1988;67:473–86. [PubMed] [Google Scholar]
- 6.Escudero-Fabre A, Cummings O, Kirklin JK et al. Cytomegalovirus colitis presenting as hematochezia and requiring resection. Arch Surg 1992;127:102–4. 10.1001/archsurg.1992.01420010120019 [DOI] [PubMed] [Google Scholar]
- 7.Genta RM, Bleyzer I, Cate TR et al. In situ hybridization and immunohistochemical analysis of cytomegalovirus-associated ileal perforation. Gastroenterology 1993;104:1822–7. [DOI] [PubMed] [Google Scholar]
- 8.Kram HB, Shoemaker WC. Intestinal perforation due to cytomegalovirus infection in patients with AIDS. Dis Colon Rectum 1990;33:1037–40. 10.1007/BF02139220 [DOI] [PubMed] [Google Scholar]
- 9.Robinson G, Wilson SE, Williams RA. Surgery in patients with acquired immunodefiency syndrome. Arch Surg 1987;122:170–5. 10.1001/archsurg.1987.01400140052006 [DOI] [PubMed] [Google Scholar]
- 10.Orloff JJ, Saito R, Lasky S et al. Toxic megacolon in cytomegalovirus colitis. Am J Gastroenterol 1989;84:794–7. [PubMed] [Google Scholar]
- 11.Rubesin SE, Levine MS. Radiologic diagnosis of gastrointestinal perforation. Radiol Clin North Am 2003;41:1095–115. 10.1016/S0033-8389(03)00100-3 [DOI] [PubMed] [Google Scholar]


