Abstract
Introduction
In conjunction with the NILVAD trial, a European Multicentre Double-Blind Placebo Controlled trial of Nilvadipine in Mild-to-Moderate Alzheimer's disease (AD), there are four NILVAD substudies in which eligible NILVAD patients are also invited to participate. The main NILVAD protocol was previously published in BMJ Open (2014). The objectives of the NILVAD substudies are to determine whether frailty, cerebrospinal fluid (CSF), blood biomarker profile and Apolipoprotein E (APOE) status predict response to Nilvadipine, and to investigate the effect of Nilvadipine on cerebral blood flow and blood biomarkers.
Methods and analysis
All participants who fulfil criteria for the main NILVAD study are eligible for participation in the NILVAD substudies. Participation is subject to informed consent and whether the substudy is available at a particular NILVAD study site. Each substudy entails extra measurements during the course of the main NILVAD study. For example, in the blood and genetic biomarkers substudy, extra blood (30 mL) will be collected at week 0, week 13, week 52 and week 78, while in the cerebral blood flow substudy, participants will receive an MRI and transcranial Doppler measurements at week 0, week 26 and week 78. In the CSF substudy, 10 mL CSF is collected at week 0 and week 78.
Ethics and dissemination
All NILVAD substudies and all subsequent amendments have received ethical approval within each participating country, according to national regulations. Each participant provides written consent to participate. All participants remain anonymised throughout and the results of each substudy will be published in an international peer reviewed journal.
Trial registration number
EUDRACT 2012-002764-27; Pre-results.
Keywords: GERIATRIC MEDICINE, NEUROLOGY
Strengths and limitations of this study.
These nested NILVAD substudies will collect biomarker data to determine if biomarker status predicts response to Nilvadipine.
The substudies run in parallel with the main NILVAD trial and thus facilitate the collection of data.
This biomarker data collection in mild-to-moderate Alzheimer's disease (AD) will provide valuable insight into the in vivo effects of Nilvadipine on these parameters. In addition, these studies provide the opportunity to study the relationship between the different outcome measures.
The substudies will not necessarily be completed by all participants recruited for the main NILVAD study (500 participants). Therefore, the results are potentially less generalisable compared to the main NILVAD study. For example, the cerebral blood flow substudy will only run in one study site and aims to recruit 40 patients.
Introduction
The NILVAD study is a large European multicentre, randomised, double-blind, placebo-controlled trial investigating the efficacy and safety of Nilvadipine as a disease course modifying treatment in mild to moderate Alzheimer's disease (AD). As part of this trial, four nested substudies have been developed to investigate if frailty status, cerebrospinal fluid (CSF) and blood biomarker profiles, and Apolipoprotein (APOE) status can predict response to Nilvadipine. Furthermore, the in vivo effects of Nilvadipine on frailty, cerebral blood flow and blood biomarker status over time will be determined. The substudies have also been designed to examine other end points that are relevant to AD pathology and allow assessment of AD progression. The four substudies are detailed as follows.
Frailty substudy
Frailty is a common and important syndrome that is increasingly prevalent with advancing age. A consensus view is emerging where the physical phenotype of frailty develops as a consequence of complex biological interactions that promote cell senescence, leading to a cumulative decline in multiple physiological systems, particularly the brain, endocrine system, immune systems and skeletal muscles. Furthermore, there is accumulating evidence to support a temporal association between frailty, cognitive impairment and dementia.1 2 It has been suggested that frailty can be used as an outcome measure because of its relationship with survival and adverse outcomes such as hospitalisation in older adults.3
Thus, a substudy to measure frailty was developed aiming (1) to investigate whether baseline frailty status predicts response to treatment with Nilvadipine and (2) to determine if treatment with Nilvadipine influences frailty status. Frailty will be measured via gait speed and a frailty index.
A large study by Fried et al,4 investigating frailty in older adults, operationalised frailty using a cluster of variables: unintentional weight loss, self-reported exhaustion, low energy expenditure, weak grip strength and slow gait speed. Their study provided the basis for identifying frailty phenotypes to predict outcome. Rockwood et al5 found that slow gait speed had the strongest association with dependency, long-term care and death, indicating gait speed might be a useful single indicator of frailty. Therefore, gait speed was chosen as a prospective physical marker of frailty in this substudy.
The Rockwood frailty index (FI) was developed from part of the Canadian Study of Health and Ageing.5 It consists of multiple parameters (‘deficits’) that can be measured, and allows for calculation of the presence or absence of frailty (simple calculation of the presence or absence of each variable as a proportion of the total: for example, 20 deficits present out of a possible 70 gives a FI of 20/70=0.29). Older adults with a FI of ≤0.08 can be considered non-frail, whereas those with an FI of ≥0.25 are considered frail. Considering that parameters for the FI should be biologically sensible, accumulate with age and do not saturate too early, a list of parameters will be collected to define a valid FI before, during and after participation in the NILVAD study.6 7 They are extracted from existing questionnaires, including the Disability Assessment of Dementia (DAD), Alzheimer's Disease Assessment Scale (ADAS-Cog 12), the Lubben Social Network Scale (LSNS) and the Charlson Comorbidity Index (CCI).8–11
We expect that if Nilvadipine has a positive effect on cognition, it will also do so on frailty, with less deterioration or with possible stabilisation.
Blood and genetic biomarkers substudy
Nilvadipine has been shown to have a multimodal action, decreasing amyloid production in transgenic mouse models of AD and increasing clearance of amyloid across the blood-brain barrier (BBB) as well as having anti-inflammatory effects in in vitro models.12–14 Thus, changes in amyloid and τ fragments along with other inflammatory markers in the peripheral blood from study baseline to end point may be useful in improving our understanding of the biological effects of Nilvadipine treatment in AD.
Levels of plasma Abeta (Aβ) and τ have been suggested as possible biomarkers for detecting conversion from normal cognition to mild cognitive impairment (MCI) or AD.15 16 As such, measurement of plasma Aβ and τ could be useful as potential biomarkers for detecting disease-modifying therapeutic effects.
The APOE ε4 allele is one of the major genetic risk factors for AD and occurs in nearly 60% of all AD cases.17 Most studies investigating treatment strategies for AD now include APOE testing to determine whether treatment outcomes vary by genotype.18 In a study by Kennelly et al,19 AD indicated that non-APOE ε4 carriers showed more of a short-term benefit from Nilvadipine treatment than did ε4 carriers.
Recently, a broad lipidomic characterisation of other phospholipids (PL) showed that a ratio of arachidonic acid to docosahexaenoic acid (DHA) was increased within several PL classes in APOE ε4 carriers several years prior to diagnosis of MCI/AD.20 As such, we expect that identification of APOE status and monitoring of these PL species could assist in monitoring effects of Nilvadipine on AD progression.
Inflammation is an active component of AD pathology, with aberrant activation of microglia and astroglia resulting in prolonged exposure to proinflammatory cytokines, contributing to chronic neuroinflammation in the brains of patients with AD. Studies have shown that various proinflammatory cytokines are increased in plasma and CSF in AD compared to in control subjects.21 22 Preclinical work on Nilvadipine supports its potential anti-inflammatory action and therefore examination of proinflammatory cytokines may be useful biomarkers in determining therapeutic response to Nilvadipine.
The aim of this substudy is thus to determine whether genetic influences can modify the effect of Nilvadipine on AD pathogenesis and whether changes in plasma Aβ, τ and inflammatory markers from study baseline to end point are altered by Nilvadipine treatment.
CSF substudy
CSF biomarker levels of total τ (T), phosphorylated τ (P) and β-amyloid 1-42 (Aβ1-42), reflect, respectively, axonal nerve cell degeneration, formation of neurofibrillary tangles and disturbed β-amyloid metabolism, thus allowing identification of neurodegenerative and cerebrovascular disease mechanism. These biomarkers, T, P-τ, Aβ and the Aβ-ratio, are considered to be most closely associated with AD core pathology. A systematic review of CSF biomarkers in AD, in 2003, demonstrated a diagnostic specificity of ∼90% and a sensitivity of ∼80% for both T and P for AD.23 In addition, it has been shown that the Aβ/τ ratio can be used to predict the conversion of MCI to AD with a specificity of 85% and a sensitivity of 86%.24 Although pure AD is often regarded as the most common dementia, it is probably less common than mixed dementia (MD: presence of AD and small vessel disease).25 A different biomarker pattern is characteristic of patients with manifest MD as well as pure subcortical vascular dementia with increased levels of neurofilament light subunit, myelin basic protein and tissue inhibitor of metalloproteinases, reflecting disturbances of the subcortical regions.26 27 However, patients with mixed pathology also display deviations in the AD-related biomarkers (Aβ1-42, T and P), thus leaving these biomarkers ineffective in differentiating between these patient groups.28
In conclusion, determination of CSF biomarkers may be useful for enhanced diagnostic purposes to assess which patients display signs of pure AD, mixed type dementia or a more pure vascular profile, with expectation that the treatment response is larger in patients with vascular involvement.
Thus the aim of this CSF substudy is to explore the biomarker status of NILVAD participants at baseline as a predictor of response to Nilvadipine and investigate biomarker changes over time, with Nilvadipine treatment, possibly enhancing our understanding of the in vivo effect of Nilvadipine.
Cerebral blood flow study
Animal models indicate that AD may be associated with profound vascular changes.29 For example, cerebral autoregulation—the mechanism that aims to stabilise cerebral blood flow during changes in blood pressure—was severely impaired in the transgenic mouse model for AD.30 Specifically, Aβ may lead to both, structural and functional cerebrovascular changes that may result in an increased risk for cerebral hypoperfusion and ischaemia. A recent study found that Nilvadipine inhibited vasoconstriction elicited by Aβ and restored decreased cortical perfusion in a transgenic mouse model, overexpressing human Aβ.13 How AD affects the cerebral vasculature and cerebral autoregulation in humans remains poorly understood. Nilvadipine has been shown to significantly improve memory and regional cerebral blood flow (rCBF) deficits in the left frontal lobe in hypertensive patients with MCI, while amlodipine did not.31 In fact, regional cerebral blood flow in the temporal lobe of the amlodipine group deteriorated. The rCBF and cognitive effects were independent of the reduction in systolic and diastolic blood pressure after treatment.
In addition to the potentially beneficial cerebrovascular effects of Nilvadipine, it may also improve blood pressure (BP), with variation in systolic BP shown to be reduced by calcium-channel blockers (and non-loop diuretic drugs), but increased by ACE inhibitors, angiotensin-receptor blockers and β-blockers.32 Thus, BP variability, a factor that may enhance risk of cerebral ischaemia, could be reduced by Nilvadipine, more than by other antihypertensive drugs.
Thus this CBF substudy will investigate the effects of Nilvadipine on CBF, BP and BP variability in study participants. It is expected that Nilvadipine treatment, through direct systemic and cerebral vascular effects, will beneficially modulate these characteristics.
In summary, these substudies will provide information on the effects of Nilvadipine on physical, cardiovascular and blood flow measures in AD. The substudies will also determine whether biomarker and genetic status predicts response to Nilvadipine, and will provide clues to the mechanism of action of Nilvadipine in AD. In addition, NILVAD substudies will provide novel data on the effects of Nilvadipine on frailty. Finally, the long-term storage and retention of blood and CSF samples will contribute significantly to a unique bioresource for studies of AD in the future.
Methods and analysis
Frailty substudy
Study design
Study participants will undergo a frailty assessment at particular time points. The schedule consists of completion of the DAD, ADAS-Cog12, LSNS and CCI. Collection of data variables from these assessments will facilitate definition of a FI before, during and after participation in the NILVAD study.
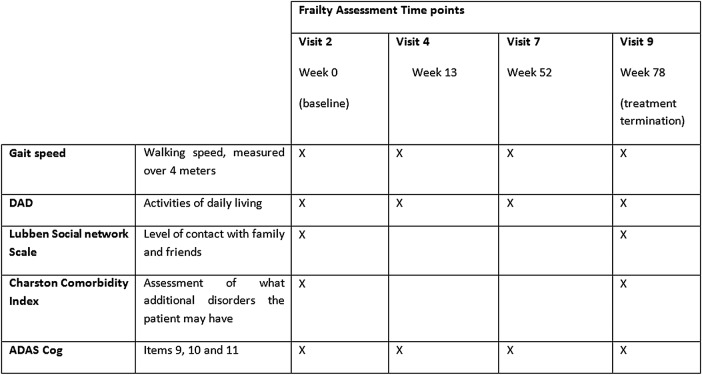
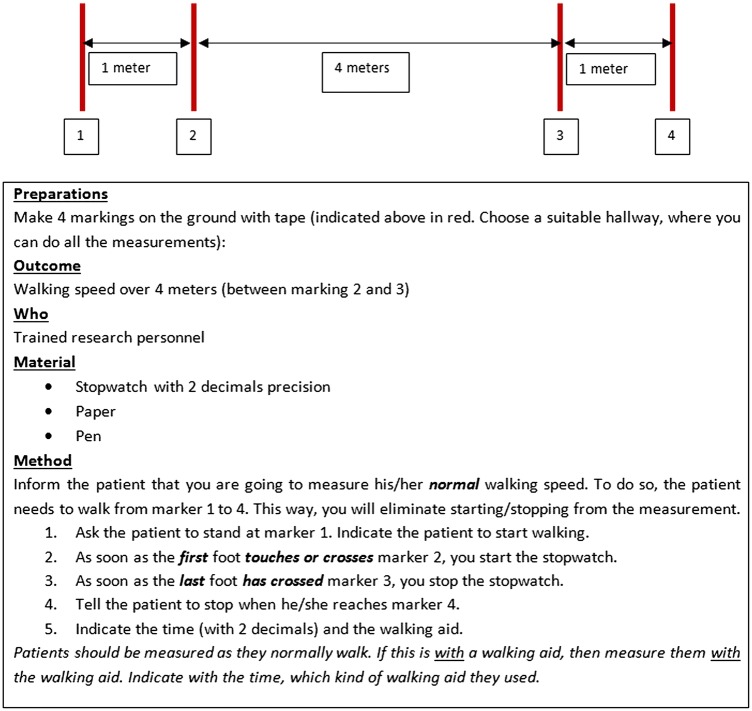
The main NILVAD study runs for a total of 82 weeks, with 78 weeks of study drug treatment (Nilvadipine or placebo). The LSNS and CCI (figure 1) are performed at study baseline (week 0) and treatment end point (week 78). The DAD and ADAS-Cog and gait speed (figure 2) are performed at week 0, 13, 52 and 78.
Figure 1.
Frailty assessment schedule. ADAS, Alzheimer's Disease Assessment Scale; DAD, Disability Assessment of Dementia.
Figure 2.
Protocol for measuring gait speed.
Inclusion/exclusion criteria
The inclusion and exclusion criteria for this substudy are as for the main NILVAD study.33
Recruitment
There are a total of 23 study sites in 9 participating European countries. Recruitment for the substudies will be undertaken locally at each study site according the local guidelines and procedures relevant to that site. All study sites will participate in the Frailty substudy, excluding Germany.
Consenting process
All consenting participants for the main NILVAD study will be invited to also provide written consent to partake in the substudies, with the option of consenting to participate in as many of the substudies as they wish, dependent on availability of the substudy at any given study site. Consent will be obtained following a full explanation of each substudy, its objectives, risks and potential benefits. A patient information leaflet and a carer's information leaflet will be provided at least 7 days prior to obtaining written consent, to allow participants and their carers time to consider enrolling. Written consent will be obtained at the main NILVAD screening visit, prior to the undertaking of any interventions or assessments.
As per the consenting process for NILVAD, when a participant has reduced decision-making capacity, the procedure for obtaining consent must follow national law and will be assessed by the relevant bodies in each of the participating countries.
Sample size calculation
The FI ranges from 0 to 1, with a natural maximum of 0.7. To calculate the sample size, we conservatively estimated the variance to be large, that is, a SD of 0.3. A sample size of 140 is adequate to allow detection of a 10% difference in FI between the NILVAD (experimental) and placebo (control) groups, and facilitate rejection of the null hypothesis that the population means of each group are equal with probability (power) 0.8. The type I error probability associated with the test of this null hypothesis is a two-sided α=0.05.
Data analysis
Data will be automatically drawn from an online Macro system, using a script in Matlab (The Mathworks, Natick, Massachusetts, USA). Then the FI will be calculated as a weighted score based on items from the ADAS-Cog (3 items), CCI (15 items), DAD (36 items), LSNS (2 items) and the gait speed (1 item). Points scored per visit are divided by the number of items applied at that visit, resulting in a FI between 0 and 1.
First, an independent samples t–test will be used to assess if there is a difference in FI between the groups at baseline, using α=0.05 as significance level. When the scores do not differ significantly, an independent samples t–test will be used to assess if there is a difference in FI between the groups at week 78, using α=0.05 as significance level. If the FI scores do differ at baseline between the groups, the data will be analysed using a mixed linear model (MLM), to examine whether Nilvadipine treatment (independent fixed factor) altered repeat measurements of FI over time (outcome factor) while controlling for random effects (each participant), again using α=0.05 as significance level.
The above analyses will be conducted on the ‘per protocol population’ (those participants who have no violations to the protocol for the duration of the study).
Blood and genetic biomarkers substudy
Study design
This substudy will involve collection of 30 mL of blood for genetic and biomarker analysis at four time points: week 0, week 13, week 52 and week 78. Whole blood (1 mL) will be aliquoted for genotyping for APOE 4 at week 0. The remaining 29 mL of the sample will be processed for biomarker analysis as per the protocol standard operating procedure (SOP), for blood processing and sample preparation (box 1).
Box 1. Standard operating procedure for blood processing for genotyping and biomarker analysis.
Sample collection
For each participant, at week 0, week 13, week 52 and week 78 visit, draw a minimum of: 2×10 mL EDTA tubes for plasma.
Use a ×10 mL serum separator tube (with silica plug) for serum.
Obtain blood samples via standard phlebotomy procedures. Please follow the guidelines from your facility for performing these procedures.
Draw the correct volume of blood allowing the vacuum in the tube to be exhausted.
Gently invert each tube to mix immediately following blood collection.
Process blood samples for genotyping, plasma and serum immediately on collection.
It is vital that blood samples are processed immediately as the biomarker proteins start to degrade if they are left for any length of time before processing.
Whole blood for genotyping (only to be carried out at week 0)
Label one 1.5 mL polypropylene cryovial per patient, with a biobanking label. This label should contain the Biobank ID, the visit number, the sample type and patient PIN.
Remove 1 mL of whole blood from one of the 10 mL EDTA tubes that were collected for plasma.
Transfer the 1 mL of whole blood into the 1.5 mL prelabelled polypropylene cryovial.
Immediately store samples at −80°C.
Fill out the electronic case report form to record the date the sample was taken and the Biobank ID numbers for each of the samples.
Plasma preparation: 2×10 mL EDTA tubes
As the serum tubes require 20–30 min standing time before processing, begin with the plasma processing.
Balance 2×10 mL EDTA tubes in the centrifuge and spin for 5 min at 1380 relative centrifugal force.
Remove tubes from centrifuge and place on ice without shaking/inverting the tubes.
Using the pipette, draw off the supernatant (upper layer) taking care not to disturb the interface, and transfer to a 15 mL polypropylene tube on ice.
Transfer the 1 mL aliquots of plasma into PRELABELED 1.5 mL polypropylene cryovials (anticipating 10 vials to be collected).
Freeze the 10 cryovials of plasma at −80°C. Do not snap freeze (ie, do not dip in liquid nitrogen to freeze).
The time taken from blood draw to freezing down the plasma samples at −80°C should not exceed 15 min.
Fill out the electronic case report form to record the date the sample was taken and the Biobank ID numbers for each of the aliquots.
Serum preparation: 1×10 mL serum separator tube
Let the serum 10 mL serum separator tube (with silica plug) stand at room temperature for 20–30 min to clot.
Balance the tube in a refrigerated centrifuge and spin for 5 min at 1380 relative centrifugal force.
Remove tube from centrifuge and place on ice without shaking/inverting the tube.
Using a pipette, draw off the supernatant (upper layer) taking care not to disturb the interface and transfer to a 15 mL polypropylene tube on ice.
Transfer the 1 mL aliquots of serum into PRELABELED 1.5 mL polypropylene cryovials (anticipating 5 vials to be collected).
Freeze the 5 cryovials of serum at −80°C. Do not snap freeze (ie, do not dip in liquid nitrogen to freeze).
The time taken from blood draw to placing the serum samples in the −80°C freezer should not exceed 35–45 min. This includes the 20–30 min of standing time required for the sample to clot.
Fill out the electronic case report form to record the date the sample was taken and the Biobank ID numbers for each of the aliquots.
Number of sample aliquots:
We shall have the following numbers of aliquots per patient at the following visits:
Visit 2 (week 0).
1.5 mL cryovial containing 1 mL of whole blood for genotyping.
1.5 mL cryovials each containing 1 mL of plasma.
1.5 mL cryovials each containing 1 mL of serum.
Visit 4 (week 13), 7 (week 52) and 9 (week 78).
1.5 mL cryovials each containing 1 mL of plasma.
1.5 mL cryovials each containing 1 mL of serum.
All samples will be collected, aliquoted and stored locally at each study site initially and then transported for final study analysis to a central study site, before transfer to a biobank for long-term storage. All samples will be stored under specific conditions and coded for identification according to the protocol SOP.
Inclusion/exclusion criteria
The inclusion and exclusion criteria for this substudy are as for the main NILVAD study.33
Recruitment
All study sites will participate in the blood and biomarker substudy except for those based in the UK and Germany.
Sample size calculations
Using the available serum data on decreases of Aβ40 observed in the phase I/II Nilvadipine study (unpublished data), we calculated an effect-size of 0.08 (based on the mean change from baseline to week 6 of the study, and the variance of Aβ40 measurements within treated and untreated participants). Given this effect size, a sample size of 254 participants is proposed to allow incorporation of 4 repeated samplings, to detect statistical significance at α=0.05 with a power of 90%.
Sample analysis
Pure Gene Kits (Gentra Systems, Minneapolis, Minnesota, USA) will be used for extracting DNA from whole blood and PCR analyses for APOE will be performed using previously established methods.34 Blood Aβ40 levels will be analysed as previously described, using commercially available ELISA kits.35 Lipidomics analysis on plasma lipid extracts will be performed using LC/MS analyses previously described.34 36 Serum levels of proinflammatory cytokines, such as tumour necrosis factor-α and IL-1β, will be examined using high-sensitivity ELISA kits as per manufacturer's instructions.
Data analysis
A MLM will also be employed to examine whether Nilvadipine treatment (independent fixed factor) altered repeat measurements of blood biomarkers over time (outcome factor) while controlling for random effects (each partcipant). MLM-based regression analysis is generally considered advantageous over other analysis of variance ANOVA due to its flexibility to accommodate fixed and random effects of the independent variables as well as incorporate dichotomous, continuous and categorical variables.37 For lipidomics analyses, principal component analysis (PCA) followed by MLM regression will be performed as described previously.36 Briefly, dimension reduction and multicolinearity issues will be resolved using PCA.
In order to ensure sampling adequacy for PCA, analysis achieving Kaiser- Mayer- Olkin (KMO) value of >0.6 and Bartlett p value <0.05 will be further investigated. Variables with eigenvalues of >1 will be retained, PCA will be used for extracting components and varimax with Kaiser normalisation will be used for rotation to simplify and clarify the data structure. The Anderson-Rubin method will be used for exporting uncorrelated scores in order to perform MLM regression analyses, as for other blood biomarkers.
The above analyses will be conducted on the ‘per protocol population’.
CSF substudy
Study design
The CSF substudy will involve collection of CSF via lumbar puncture (LP), for biomarker and inflammatory marker analysis (box 2). Patients will undergo a LP prior to start of the NILVAD study drug (ie, between the screening and baseline assessment (week 0), and again after treatment determination (week 78).
Box 2. Standard operating procedure for lumbar puncture (cerebrospinal fluid (CSF) collection and processing).
CSF sample collection and processing
The lumbar puncture will be carried out BETWEEN THE SCREENING AND BASELINE VISIT (21-day window) and TREATMENT TERMINATION, BETWEEN WEEK 78 AND WEEK 82. The lumbar puncture should be performed ideally between 8:00 and 11:00.
Local guidelines/routines for antiseptic cleansing and anaesthesia are to be followed.
Position the patient in a reclining or sitting position with back arched.
Use a Spinal Needle Quincke Type Point 0.7×75 mm (75–90 mm) for the LP.
Insert the needle through the L3/L4 or L4/L5 interspace.
-
In case of bleeding at the puncture site, the first 1 mL of CSF should be discarded and this should be recorded.
Collect 10 mL of CSF from each participant. For CSF collection, use a POLYPROPYLENE TUBE ONLY
(ie, 15 mL polypropylene tube).
MIX the CSF gently by turning the tube upside down 3–4 times (cap on).
Centrifuge the CSF in the polypropylene tube at 2000 g for 10 min at +4°C, to eliminate cells and debris.
Transfer the centrifuged CSF into another sterile polypropylene tube, being careful to avoid disturbing the pellet of cells and debris at the end of the tube.
Aliquot CSF in 1 mL aliquots into sterile 1.5 mL PRELABELED POLYPROPYLENE CRYOVIALS with a screw cap.
Place the tubes directly in a −80°C freezer. Do not snap freeze (ie, do not dip in liquid nitrogen to freeze).
Fill out the electronic case report form to record the date the sample was taken and the Biobank ID numbers for each of the aliquots.
The patient should be allowed to rest for 30 min to 1 hour after the lumbar puncture procedure.
A paired serum albumin sample will also be drawn to allow for calculation of the albumin CSF-serum ratio (box 3). The ratio of albumin in CSF to serum is an indicator of BBB integrity. An increased ratio can indicate increased permeability and it has been demonstrated that AD pathology can lead to BBB dysfunction.38 While the underlying pathological mechanisms have yet to be fully elucidated, it is thought that alterations to the BBB affects Aβ clearance and may contribute to neuroinflammation seen in AD as a result of fluctuations in homeostasis.39
Box 3. Standard operating procedure for paired serum albumin sample collection and processing.
Serum preparation
Collect 5 mL of blood in a 10 mL serum separator tube (with silica plug) and allow to stand at room temperature for 20–30 min to clot.
Balance the tube in a refrigerated centrifuge and spin for 5 min at 1380 relative centrifugal force.
Remove tube from the centrifuge and place on ice without shaking/inverting the tube.
Using a pipette, draw off the supernatant (upper layer) taking care not to disturb the interface, and transfer to a 10 mL polypropylene tube on ice.
Transfer 1 mL aliquots of serum into PRELABELED 1.5 mL polypropylene cryovials.
Freeze the 5 cryovials of serum at −80°C. Do not snap freeze (ie, do not dip in liquid nitrogen to freeze).
Fill out the electronic case report form to record the date the sample was taken and the Biobank ID numbers for each of the aliquots.
Samples will be collected, aliquoted and stored locally at each study site initially, and then transported for final analysis to a central study site, before transfer to a biobank for long-term storage. All samples will be stored under specific conditions and coded for identification according to the protocol. An SOP will be adhered to for collection and processing of the CSF sample and the blood sample.
Inclusion/exclusion criteria
For this substudy, additional specific exclusion criteria regarding contraindications to LP must be adhered to, including (1) possible raised intracranial pressure, (2) bleeding diathesis, including thrombocytopenia or treatment with anticoagulant therapy.
Recruitment
All study sites, with the exclusion of those based in the UK, Germany and Italy, will participate in the CSF substudy.
Consenting process
In the case of the CSF substudy, consent by proxy is not applicable and all participants must retain the capacity to consent to undergo an LP. Of note, patients must retain the capacity to consent to undergo a second LP at the study end point.
Sample size calculations
Observed changes in CSF Aβ42 over a 78-week period from a published study were used to calculate power for detecting potential decreases in CSF Aβ42 following Nilvadipine treatment. The effect size calculations were based on mean Aβ42 changes and associated variance observed by Salloway and colleagues.40 The resulting effect size was 0.67, which required a sample size of 98 for detecting statistically significant Aβ42 change from baseline to week 78, with a power of 90% at α=0.05.
Data analysis
Analysis of CSF will be performed according to standardised protocols. Aβ40, Aβ42, T and P 181 will be measured using a commercially available sandwich ELISA (INNOTEST; Fujirebio Europe NV, Ghent, Belgium) according to the manufacturer's instructions.
The ratio between Aβ42 and Aβ40 for each patient will be calculated as the concentration of Aβ42 divided by the concentration of Aβ40 and multiplied by 100.41
First, an independent samples t-test will be used to assess if there is a difference in Aβ-ratio between the two groups at baseline, using α=0.05 as significance level. When the scores do not differ significantly, an independent samples t-test will be used to assess if there is a difference in Aβ-ratio change between the two groups at week 78, using α=0.05 as significance level.
The above analyses will be conducted on the ‘per protocol population’.
Cerebral blood flow substudy
Study design
Participants will undergo additional measurements of blood pressure (BP), cerebral autoregulation (CA) and cerebral blood flow (CBF) via MRI at baseline, week 26 and week 72.
Participants will be provided with a home blood pressure monitor (HBPM, Microlife Watch BP Home) at the screening visit and requested to take their own BP readings twice daily (morning and evening), after a 5 min period of relaxation, the week prior to their assessment visit at baseline, week 26 and week 78, for assessment of BP variability. Participants will be blinded to the BP readings (no result visible on monitor screen) and measurements will be conducted according to the European Society of Hypertension guidelines.42 Participants will be requested to bring the HBPM with them to the baseline visit (week 0) and week 26 and 78, to facilitate downloading of the BP data.
Additionally, at these visits, each participant will undergo an MRI scan for measurement of CBF, using arterial spin labelling (ASL) with multiple inflow times (10 time points). This sequence allows for the reconstruction of the blood flow over time for each voxel. A specific scanning protocol will be adhered to according to the study protocol (box 4), including additional sequences to measure, for instance, white matter integrity and presence of microbleeds. Subsequently, all participants will undergo CA measurements, again according to the study protocol (box 5), measuring CBF velocity in the middle cerebral artery, using transcranial Doppler. In addition, near infrared spectroscopy (NIRS) will be applied. During the measurement protocol, BP will be measured continuously using servo-controlled finger photoplethysmography (Finapres) and heartbeat will be measured using ECG.
Box 4. Standard operating procedure for MRI acquisition in the cerebral blood flow (CBF) substudy.
Screening
Make sure you have an empty home blood pressure monitor (HBPM) that is set in Diagnostic mode and displays the right time of day.
At the end of the screening session, explain the use of the HBPM and instruct the patient to start the home blood pressure measurements the week before the CBF visit.
Instruct the patient to bring the monitor with him/her on the next visit.
Baseline
Read out the data of the HBPM.
Clear HBPM after checking data is saved correctly on the computer.
Give HBPM back to patient.
CBF MRI
Take the patient to the Siemens Trio scanner at the Radiology department.
Together with the laboratory-assistant, instruct the patient and make sure there is no metal on the body of the patient.
Lie the patient in the scanner and put the MRI-compatible blood pressure monitor in place.
Scan the patient according to protocol:
Scan protocol
T1-weighted anatomic scan (MP-RAGE) with 1 mm isotropic resolution. Duration 5:47.
Fluid-attenuated inversion recovery (FLAIR) (0.7×0.7×3 mm, no gap). Duration 6:50.
Susceptibility-weighted imaging (SWI) (1×1×1 mm). Duration 7:44.
Diffusion tensor imaging (DTI) (2×2×2 mm). Duration 8:25.
Arterial spin labelling (ASL) (3.4×3.4×4 mm). Duration 10:40. TI 500–2750 ms, with increments of 250 ms.
Box 5. Standard operating procedure for Cerebral Autoregulation as part of the cerebral blood flow (CBF) substudy.
Cerebral Autoregulation
After a break, take the patient to the Haemodynamics Laboratory at the Department of Geriatric Medicine (SKU, Nijmegen).
Instruct the patient and start the measurement software on the computer.
-
Put the headband in place, and then activate all the measurement equipment
Servo-controlled finger photoplethysmography (Finapres) to continuously measure blood pressure.
Transcranial Doppler (TCD) to measure CBF velocity in the middle cerebral arteries. TCD-probes will be positioned on the temporal bone.
Near-infrared-spectroscopy (NIRS) to monitor changes in cerebral cortical oxygenation. Optodes will be placed in a specially designed headband.
Protocol
Baseline measurements (5 min lying and 5 min sitting).
Single sit-stand manoeuvres (2×2 min sitting, 1 min standing+1×2 min sitting, 5 min standing).
Repeated sit-stand manoeuvres (10 s sitting, 10 s standing for 5 min).
Hyperventilation (30 s, 2 min recovery).
CO2-inhalation (30 s 3%, 30 s 4%, 3 min 5%, 1 min recovery).
Remove all equipment from the patient.
End of entire measurement.
All measurements will be taken in the morning to reduce the effect of diurnal variation in blood flow. Also, participants will have to refrain from intake of caffeine and alcohol, substances that can influence the blood flow measurement. Haematocrit level of every participant will be measured on the morning of the scan, since blood viscosity can influence the ASL measurement. This will not reduce intraindividual variation.
Inclusion/exclusion criteria
Specific contraindications to MRI must be adhered to, including (1) metal implants in situ and/or (2) suffering from claustrophobia. Patients who do not fit the MRI criteria can still participate in the CBF substudy, but without the MRI.
Recruitment
This substudy will only be undertaken in one study site, Nijmegen, in the Netherlands, to eliminate the variation introduced by the use of different MRI scanners. Also, eligible patients from another site (Arnhem, the Netherlands) can be included in the substudy. These patients will not be included in the separate randomisation process.
Sample size calculation
The total number of participants is based on the power calculation computed on the primary efficacy parameter, CBF measured with ASL, as follows:
The primary variable of the study is a continuous variable, the CBF, from independent control and experimental subjects, with 50–50 distribution between the two groups. There have been very few studies using CBF as an outcome measure in an randomised controlled trial (RCT), but a previous study where two groups were compared detected a 25% difference.43 A recent RCT (N=27 vs N=31) detected a 36% change in CBF, using pulsed ASL at 3 T.44 To detect a 15% difference in (regional) CBF (using pulsed ASL at 3 T) between two groups, a group size of 20 per group should be sufficient, to be able to reject the null hypothesis that the population means of each group are equal with probability (power) 0.8.45 The type I error probability associated with the test of this null hypothesis is a two-sided 0.05.
Data analysis
All analyses will be performed blind to participant group.
Analysis of MRI data
Structural MRI scans will be processed using BET and FAST, both packages of the publicly available image processing software FSL 5.0 (http://www.fmrib.ox.ac.uk/fsl/tbss/index.html) to identify grey matter (GM) and white matter (WM), and CSF components on the image.46 47 Total brain volume (TBV) will be calculated as the sum of GM and WM volume (in mL), and intracranial volume (ICV) as the sum of GM and WM plus CSF. The TBV/ICV ratio will then be calculated as an estimate of brain atrophy.
CBF will be calculated for the whole brain GM. The data will be analysed using MLM, to test if the change in whole brain GM CBF (maximum flow) from baseline to week 26 is different for the two intervention groups, using α=0.05 as significance level.
Brain atrophy and blood viscosity will be added as additional model parameters. Using the multiple inflow times, per voxel, the maximum flow is calculated using BASIL,48 another FSL package. To avoid brain atrophy causing artificially low CBF values, partial volume correction will be used.
The above analyses will be conducted on the ‘per protocol population’.
Ethics and dissemination
All four NILVAD Substudies will be conducted according to Good Clinical Practice guidelines and in accordance with the Declaration of Helsinki. All substudies have been submitted for approval to the relevant independent Ethics Committees in each participating country, and have also been reviewed and will be continuously monitored by the NILVAD Ethics Advisory Board, for the duration of the main NILVAD study and substudies.
It is intended that all positive, neutral or negative results for the substudies will be published in international peer-reviewed journals. Authorship and publication will be as per the agreed NILVAD study publication policy.
Substudy status
Enrolment for all substudies began with start of the main NILVAD trial, in May 2013, and the recruitment period continued until March 2015.
Footnotes
Contributors: BL is responsible for the initial study concept, design and content of the blood and genetic biomarker substudies. MOR is responsible for the initial study concept, design and content of the frailty substudy. OM is responsible for the initial study concept, design and content of the cerebral blood flow substudy. AW is responsible for the initial concept, design and content of the CSF biomarker substudy. OM, SOD, GvS, DdJ, AW and BL made substantial contribution to the initial drafting of this manuscript. All the listed authors have contributed to critical revision of the submitted manuscript and have approved the final article for submission.
Funding: The main NILVAD trial and associated substudies are funded by the European Commission Framework 7 Programme health theme collaborative project. Grant Agreement Number: 279093. The CBF substudy is funded by the Alzheimer's Drug Discovery Foundation (ADDF), Grant number: 20121210 and by the Dutch Alzheimer Society, grant number WE.03-2015-01.
Competing interests: AW is a member of the speakers’ bureau for Esai and a member of the advisory board for Nutricia. FC and MM are officers at Archers Pharmaceuticals, which has licensed the technology for the use of Nilvadipine in AD.
Ethics approval: All substudies have received ethical approval from the relevant independent Ethics Committees in each participating country.
Data sharing statement: No unpublished data are available other than to the NILVAD Data Safety Monitoring Board (DSMB). This board will be established to review and monitor all study data, and to prepare reports on data and safety monitoring.
References
- 1.Gray SL, Anderson ML, Hubbard RA et al. Frailty and incident dementia. J Gerontol A Biol Sci Med Sci 2013;68:1083–90. 10.1093/gerona/glt013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kulmala J, Nykänen I, Mänty M et al. Association between frailty and dementia: a population-based study. Gerontology 2014;60:16–21. 10.1159/000353859 [DOI] [PubMed] [Google Scholar]
- 3.de Vries NM, Staal JB, van Ravensberg CD et al. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev 2011;10:104–14. 10.1016/j.arr.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 4.Fried LP, Tangen CM, Walston J et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–56. 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 5.Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–95. 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Searle SD, Mitnitski A, Gahbauer EA et al. A standard procedure for creating a frailty index. BMC Geriatr 2008;8:24 10.1186/1471-2318-8-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010;58:681–7. 10.1111/j.1532-5415.2010.02764.x [DOI] [PubMed] [Google Scholar]
- 8.Charlson ME, Pompei P, Ales KL et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 9.Gélinas I, Gauthier L, McIntyre M et al. Development of a functional measure for persons with Alzheimer's disease: the disability assessment for dementia. Am J Occup Ther 1999;53:471–81. 10.5014/ajot.53.5.471 [DOI] [PubMed] [Google Scholar]
- 10.Lubben J, Blozik E, Gillmann G et al. Performance of an abbreviated version of the Lubben Social Network Scale among three European community-dwelling older adult populations. Gerontologist 2006;46:503–13. 10.1093/geront/46.4.503 [DOI] [PubMed] [Google Scholar]
- 11.Mohs RC, Rosen WG, Davis KL. The Alzheimer's disease assessment scale: an instrument for assessing treatment efficacy. Psychopharmacol Bull 1983;19:448–50. [PubMed] [Google Scholar]
- 12.Kagawa H, Nomura S, Ozaki Y et al. Effects of nilvadipine on cytokine-levels and soluble factors in collagen disease complicated with essential hypertension. Clin Exp Hypertens 1999;21:1177–88. 10.3109/10641969909052196 [DOI] [PubMed] [Google Scholar]
- 13.Paris D, Bachmeier C, Patel N et al. Selective antihypertensive dihydropyridines lower Abeta accumulation by targeting both the production and the clearance of Abeta across the blood-brain barrier. Mol Med 2011;17:149–62. 10.2119/molmed.2010.00180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paris D, Quadros A, Humphrey J et al. Nilvadipine antagonizes both Abeta vasoactivity in isolated arteries, and the reduced cerebral blood flow in APPsw transgenic mice. Brain Res 2004;999:53–61. 10.1016/j.brainres.2003.11.061 [DOI] [PubMed] [Google Scholar]
- 15.Abdullah L, Luis C, Paris D et al. Serum Abeta levels as predictors of conversion to mild cognitive impairment/Alzheimer disease in an ADAPT subcohort. Mol Med 2009;15:432–7. 10.2119/molmed.2009.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thambisetty M, Lovestone S. Blood-based biomarkers of Alzheimer's disease: challenging but feasible. Biomark Med 2010;4:65–79. 10.2217/bmm.09.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crean S, Ward A, Mercaldi CJ et al. Apolipoprotein E ε4 prevalence in Alzheimer's disease patients varies across global populations: a systematic literature review and meta-analysis. Dement Geriatr Cogn Disord 2011;31:20–30. 10.1159/000321984 [DOI] [PubMed] [Google Scholar]
- 18.Raber J, Huang Y, Ashford JW. ApoE genotype accounts for the vast majority of AD risk and AD pathology. Neurobiol Aging 2004;25:641–50. 10.1016/j.neurobiolaging.2003.12.023 [DOI] [PubMed] [Google Scholar]
- 19.Kennelly S, Abdullah L, Kenny RA et al. Apolipoprotein E genotype-specific short-term cognitive benefits of treatment with the antihypertensive nilvadipine in Alzheimer's patients-an open-label trial. Int J Geriatr Psychiatry 2012;27:415–22. 10.1002/gps.2735 [DOI] [PubMed] [Google Scholar]
- 20.Whiley L, Sen A, Heaton J et al. Evidence of altered phosphatidylcholine metabolism in Alzheimer's disease. Neurobiol Aging 2014;35:271–8. 10.1016/j.neurobiolaging.2013.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heneka MT, Carson MJ, El Khoury J et al. Neuroinflammation in Alzheimer's disease. Lancet Neurol 2015;14:388–405. 10.1016/S1474-4422(15)70016-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee KS, Chung JH, Choi TK et al. Peripheral cytokines and chemokines in Alzheimer's disease. Dement Geriatr Cogn Disord 2009;28:281–7. 10.1159/000245156 [DOI] [PubMed] [Google Scholar]
- 23.Blennow K, Hampel H. CSF markers for incipient Alzheimer's disease. Lancet Neurol 2003;2:605–13. 10.1016/S1474-4422(03)00530-1 [DOI] [PubMed] [Google Scholar]
- 24.Mattsson N, Zetterberg H, Hansson O et al. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA 2009;302:385–93. 10.1001/jama.2009.1064 [DOI] [PubMed] [Google Scholar]
- 25.Nägga K, Rådberg C, Marcusson J. CT brain findings in clinical dementia investigation—underestimation of mixed dementia. Dement Geriatr Cogn Disord 2004;18:59–66. 10.1159/000077737 [DOI] [PubMed] [Google Scholar]
- 26.Rosengren LE, Karlsson JE, Sjögren M et al. Neurofilament protein levels in CSF are increased in dementia. Neurology 1999;52:1090–3. 10.1212/WNL.52.5.1090 [DOI] [PubMed] [Google Scholar]
- 27.Bjerke M, Zetterberg H, Edman à et al. Cerebrospinal fluid matrix metalloproteinases and tissue inhibitor of metalloproteinases in combination with subcortical and cortical biomarkers in vascular dementia and Alzheimer's disease. J Alzheimers Dis 2011;27:665–76. 10.3233/JAD-2011-110566 [DOI] [PubMed] [Google Scholar]
- 28.Blennow K, Wallin A, Agren H et al. Tau protein in cerebrospinal fluid: a biochemical marker for axonal degeneration in Alzheimer disease? Mol Chem Neuropathol 1995;26:231–45. 10.1007/BF02815140 [DOI] [PubMed] [Google Scholar]
- 29.Claassen JA, Zhang R. Cerebral autoregulation in Alzheimers disease. J Cereb Blood Flow Metab 2011;31:1572–7. 10.1038/jcbfm.2011.69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Niwa K, Kazama K, Younkin L et al. Cerebrovascular autoregulation is profoundly impaired in mice overexpressing amyloid precursor protein. Am J Physiol Heart Circ Physiol 2002;283:H315–23. 10.1152/ajpheart.00022.2002 [DOI] [PubMed] [Google Scholar]
- 31.Hanyu H, Hirao K, Shimizu S et al. Favourable effects of nilvadipine on cognitive function and regional cerebral blood flow on SPECT in hypertensive patients with mild cognitive impairment. Nucl Med Commun 2007;28:281–7. 10.1097/MNM.0b013e32804c58aa [DOI] [PubMed] [Google Scholar]
- 32.Webb AJ, Fischer U, Mehta Z et al. Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010;375:906–15. 10.1016/S0140-6736(10)60235-8 [DOI] [PubMed] [Google Scholar]
- 33.Lawlor B, Kennelly S, O'Dwyer S et al. NILVAD protocol: a European multicentre double-blind placebo-controlled trial of nilvadipine in mild-to-moderate Alzheimer's disease. BMJ Open 2014;4:e006364 10.1136/bmjopen-2014-006364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Emmerich T, Abdullah L, Crynen G et al. Plasma lipidomic profiling in a military population of Mild Traumatic Brain Injury and Post-Traumatic Stress Disorder with APOE E ɛ4 dependent effect. J Neurotrauma 2016. [epub ahead of print]. 10.1089/neu.2015.4061 [DOI] [PubMed] [Google Scholar]
- 35.Abdullah L, Luis C, Paris D et al. High serum Abeta and vascular risk factors in first-degree relatives of Alzheimer's disease patients. Mol Med 2009;15:95–100. 10.2119/molmed.2008.00118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abdullah L, Evans JE, Ferguson S et al. Lipidomic analyses identify injury-specific phospholipid changes 3 mo after traumatic brain injury. FASEB J 2014;28:5311–21. 10.1096/fj.14-258228 [DOI] [PubMed] [Google Scholar]
- 37.Katz MH. Multivariable analysis: a practical guide for clinicians and public health researchers. Cambridge, New York: Cambridge University Press, 2011. [Google Scholar]
- 38.Erickson MA, Banks WA. Blood-brain barrier dysfunction as a cause and consequence of Alzheimer's disease. J Cereb Blood Flow Metab 2013;33:1500–13. 10.1038/jcbfm.2013.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marques F, Sousa JC, Sousa N et al. Blood-brain-barriers in ageing and in Alzheimer's disease. Mol Neurodegener 2013;8:38 10.1186/1750-1326-8-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salloway S, Sperling R, Keren R et al. A phase 2 randomized trial of ELND005, scyllo-inositol, in mild to moderate Alzheimer disease. Neurology 2011;77:1253–62. 10.1212/WNL.0b013e3182309fa5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lewczuk P, Esselmann H, Otto M et al. Neurochemical diagnosis of Alzheimer's dementia by CSF Abeta42, Abeta42/Abeta40 ratio and total tau. Neurobiol Aging 2004;25:273–81. 10.1016/S0197-4580(03)00086-1 [DOI] [PubMed] [Google Scholar]
- 42.Parati G, Stergiou GS, Asmar R et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens 2010;24:779–85. 10.1038/jhh.2010.54 [DOI] [PubMed] [Google Scholar]
- 43.Fleisher AS, Podraza KM, Bangen KJ et al. Cerebral perfusion and oxygenation differences in Alzheimer's disease risk. Neurobiol Aging 2009;30:1737–48. 10.1016/j.neurobiolaging.2008.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mozolic JL, Hayasaka S, Laurienti PJ. A cognitive training intervention increases resting cerebral blood flow in healthy older adults. Front Hum Neurosci 2010;4:16 10.3389/neuro.09.016.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murphy K, Harris AD, Diukova A et al. Pulsed arterial spin labeling perfusion imaging at 3 T: estimating the number of subjects required in common designs of clinical trials. Magn Reson Imaging 2011;29:1382–9. 10.1016/j.mri.2011.02.030 [DOI] [PubMed] [Google Scholar]
- 46.Smith SM. Fast robust automated brain extraction. Hum Brain Mapp 2002;17:143–55. 10.1002/hbm.10062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging 2001;20:45–57. 10.1109/42.906424 [DOI] [PubMed] [Google Scholar]
- 48.Chappell MA, Groves AR, Whitcher B et al. Variational Bayesian inference for a nonlinear forward model. IEEE Transactions on Signal Processing 2009;57:223–36. 10.1109/TSP.2008.2005752 [DOI] [Google Scholar]