Abstract
Pneumomediastinum and epidural pneumatosis are rare complications of diabetic ketoacidosis (DKA). These result from the emesis and hyperventilation associated with DKA which lead to alveolar rupture and air escape into the mediastinal and epidural spaces. These complications are often asymptomatic and resolve with the correction of the underlying metabolic abnormality. Oesophageal contrast studies are only required if oesophageal perforation is suspected in patients presenting with persistent vomiting and chest pain. We report the rare association of pneumomediastinum and epidural pneumatosis complicating DKA in a 19-year-old female patient.
Case presentation
A 19-year-old female patient with type 1 diabetes mellitus (diagnosed at 2 years of age) presented to the emergency department with a 3-day history of vomiting, and neck pain for the preceding 24 hours. She omitted taking her insulin the day prior to admission as she was not eating. Her medications included insulin glargine 26 units at night and premeal insulin lispro, ∼24 units per day. She attended outpatient clinics and took her insulin regularly, but had an erratic diet and declined structured education (Dose Adjustment for Normal Eating, DAFNE). Her diabetes control was suboptimal with a most recent glycated haemoglobin (HbA1c) of 74 mmol/L (8.9%), and she showed evidence of background retinopathy at her last retinal screening visit. She did not have any history of underlying respiratory conditions, such as asthma or pneumothorax, and she was a non-smoker.
On clinical examination, she was dehydrated with rapid shallow Kussmaul breathing at a rate of 34 breaths/min. She was tachycardic at 120 bpm and her blood pressure was 149/99 mm Hg, temperature 36.9°C and oxygen saturation 91% in room air. She was drowsy, opening her eyes only to commands. She had palpable crepitus on examination of the neck. The rest of her examination was unremarkable.
Investigations
Capillary blood glucose was 24 mmol/L and ketones were 5.9 mmol/L; arterial blood gas analysis revealed a metabolic acidosis with pH of 7.24 and bicarbonate of 12.3 mmol/L. There was a raised white cell count at 38.8×109 cells/L and a haemoglobin count of 16.5 g/dL. There was evidence of acute kidney injury with creatinine at 143 mmol/L and urea level at 10.6 mmol/L.
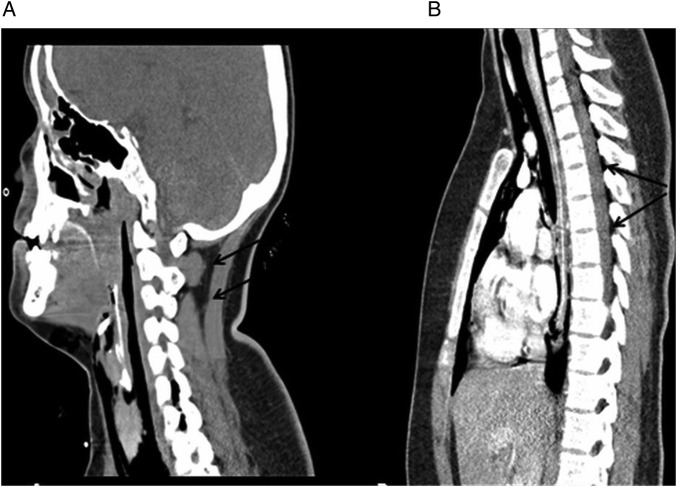
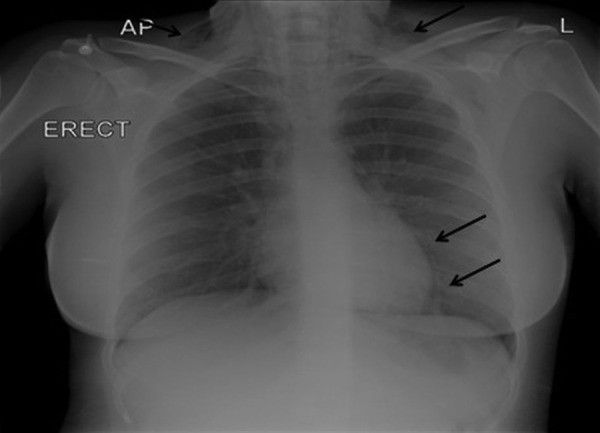
Chest radiograph demonstrated a pneumomediastinum (PM) as well as cervical subcutaneous emphysema (figure 1). CT of the thorax confirmed a PM, and revealed epidural pneumatosis with air extension up to the base of the skull (figure 2). Oesophageal contrast studies showed no perforation of the oesophagus (Boerhaave's syndrome).
Figure 1.
Chest X-ray demonstrating a thin line of radiolucency along the left heart border indicating the presence of pneumomediastinum and subcutaneous bilateral cervical surgical emphysema (arrows).
Figure 2.
CT scan showing (A) air extension up to the base of skull, and (B) epidural pneumatosis, with air tracking posteriorly into the extradural space of the spinal canal (arrows).
Treatment
She was admitted to the intensive care unit for monitoring. Her ketoacidosis resolved within 24 hours following initiation of insulin and fluids as per diabetic ketoacidosis (DKA) protocol, and her neck pain settled within 48 hours of admission.
Outcome and follow-up
She was discharged home after 4 days with a plan for early review at the diabetes day centre, and she was booked to attend the DAFNE course in the summer holiday.
Discussion
PM or mediastinal emphysema is a rare condition characterised by the presence of free air in the mediastinum due to conditions leading to alveolar overdistension and barotrauma. These can result in alveolar rupture and as a result, air leaks into the pulmonary interstitium, dissecting through the bronchovascular bundles into the mediastinum.1 Air can also track up into the pleural space, subcutaneous soft tissues of the neck and pericardium leading to pneumothorax, soft tissue emphysema and pneumopericardium, respectively.2
Spontaneous PM, which was first described in 1937 by Hamman,3 has been reported in conditions leading to high intrathoracic pressure swings such as vomiting, labour, seizures, excessive shouting, coughing, asthma exacerbation and sneezing.4
PM complicating DKA is rarely reported in the medical literature.4 The exact pathophysiology is unknown; however, it is believed that Kussmaul respiration leads to a significant 20–30 mm Hg rise in intra-alveolar pressure and this may result in alveolar rupture.5 Furthermore, vomiting can predispose to alveolar rupture through increasing intrathoracic pressure.5 More recently, alveolar histological changes and fibrosis have been described as part of the ‘diabetic lung’ in patients with poorly controlled diabetes.6 Whether these changes can predispose to alveolar rupture and PM is not yet known, but may help explain this phenomenon.
Spontaneous PM is a self-limiting condition and no further investigations are required in most cases; however, oesophageal perforation (Boerhaave's syndrome) should be suspected in cases presenting with persistent vomiting and chest pain. This is extremely rare; in a review of 40 cases of DKA associated PM, oesophageal rupture was not detected in any of the cases.4
Epidural pneumatosis is the presence of air in the epidural space and has been reported following trauma, strenuous exercise, lumbar puncture and epidural analgesia.5 Epidural pneumatosis complicating spontaneous PM is rare, and results from the posterior dissection of the PM through the intervertebral space into the epidural canal.4 Epidural pneumatosis in DKA-induced PM is exceptionally rare. To date, only six cases of such presentation have been reported.4 5 7–9 The average age of patients was 23 years (range 18–31), 58% were males, and all patients had vomiting and metabolic acidosis on admission. Three of the seven patients (42%), including our case, had neck pain at presentation; however, there were no associated neurological manifestations. Six patients underwent contrast studies to rule out oesophageal perforation, and these were all normal. In all the cases, conservative management and treatment of DKA resulted in spontaneous resolution.
Recurrence of spontaneous PM is extremely rare. Among 12 patients reported in the literature to have recurrent PM, only one case was associated with DKA due to excess alcohol.10 Healthcare providers should be aware of this exceptional but possible complication when counselling these patients.
In summary, epidural pneumatosis complicating DKA is very rare. It should be suspected in patients with DKA and neck pain at presentation. No further investigations are required in most cases, and symptoms resolve spontaneously with the appropriate treatment of DKA.
Learning points.
Spontaneous pneumomediastinum (PM) is a rare complication of diabetic ketoacidosis (DKA), and results from the increased intra-alveolar pressure and alveolar rupture due to vomiting and ketotic breathing associated with DKA.
Spontaneous PM is asymptomatic and resolves with conservative management in most cases; however, in cases presenting with persistent vomiting and chest pain, more sinister conditions—such as Boerhaave's syndrome—should be excluded.
Epidural pneumatosis complicating DKA-induced PM is extremely rare, and results from air dissecting into the epidural space. It can present with neck pain; however, no neurological sequelae have been reported to date.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Abolink I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest 1991;100:93–5. 10.1378/chest.100.1.93 [DOI] [PubMed] [Google Scholar]
- 2.Panacek EA, Singer AJ, Sherman BW et al. Spontaneous pneumomediastinum: clinical and natural history. Ann Emerg Med 1992;21:1222–7. 10.1016/S0196-0644(05)81750-0 [DOI] [PubMed] [Google Scholar]
- 3.Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp 1939;64:1–21. [Google Scholar]
- 4.Pauw RG, van der Werf TS, van Dullemen HM et al. Mediastinal emphysema complicating diabetic ketoacidosis: plea for conservative diagnostic approach. Neth J Med 2007;65:368–71. [PubMed] [Google Scholar]
- 5.Pooyan P, Puruckherr M, Summers JA et al. Pneumomediastinum, pneumopericardium, and epidural pneumatosis in DKA. J Diabetes Complications 2004;18:242–7. 10.1016/S1056-8727(03)00059-X [DOI] [PubMed] [Google Scholar]
- 6.Dario P, Leonello F, Emanuele GC et al. The diabetic lung: a new target organ? Rev Diabet Stud 2012;9:23–35. 10.1900/RDS.2012.9.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hall WB, Aris RM. Epidural pneumatosis and diffuse soft tissue free air as a complication of diabetic ketoacidosis. Am J Respir Crit Care Med 2012;185:e5 10.1164/rccm.201105-0916IM [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ripley P, Wilson EJ, Meller MT. Pneumorrhachis: a rare complication of diabetic ketoacidosis. Diabet Med 2009;26:566–7. 10.1111/j.1464-5491.2009.02703.x [DOI] [PubMed] [Google Scholar]
- 9.Hung Hui L, Shu-Chaiang H, Chih-Teng C et al. Diabetic ketoacidosis complicated with pneumomediastinum and pneumorrhachis: a case report. J Emer Crit Care Med 2012;23:56–9. [Google Scholar]
- 10.Natale C, D'Journo XB, Duconseil P et al. Recurrent spontaneous pneumomediastinum in an adult. Eur J Cardiothorac Surg 2012;41:1199–201. 10.1093/ejcts/ezr135 [DOI] [PubMed] [Google Scholar]