Abstract
Tuberculosis of the bladder is a rare pathology in the western world and often not considered as a differential when seeing patients with common urological presentations. This case illustrates a 69-year-old woman in rural England who presented with visible haematuria and was subsequently diagnosed with tuberculosis of the bladder. The case aims to highlight the significance of early diagnosis and treatment, which in turn may help prevent disease progression and organ dysfunction.
Background
It is estimated that one-third of the world's population is infected with tuberculosis. In the developing world the genitourinary tract is one of the most common extrapulmonary sites for granulomatous infiltration. Although bladder tuberculosis is a known cause of haematuria, there are few reported cases of isolated bladder tuberculosis in the western world. When identified, diagnosis is often delayed and irreversible organ dysfunction ensues.1 The aim of this article is to highlight the importance of early detection and the need to think of tuberculosis as a differential diagnosis in clinical practice.
Case presentation
A 69-year-old woman in rural England presented as a ‘2-week-referral’ with intermittent visible haematuria on a background of several years of urinary frequency, dysuria and episodes of sterile pyuria. Ultrasound and CT scans identified unilateral hydronephrosis and an isolated thickening of the bladder wall (figures 1 and 2). Pathology from the erythematous lesion (figures 3 and 4) surrounding the ureteric orifice revealed chronic inflammation and granulomatous change prompting Ziehl-Nielson staining. Tuberculosis was confirmed following three positive urine samples and antituberculosis therapy was initiated. Further investigation did not identify any extravesical disease.
Figure 1.
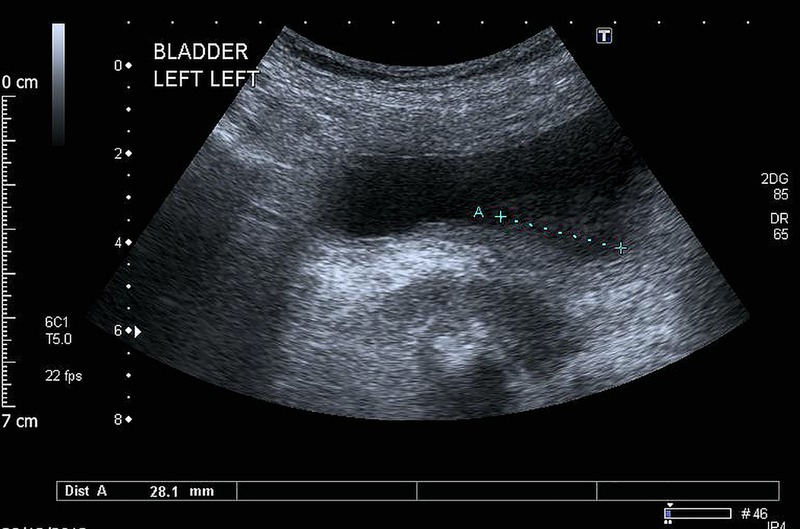
Ultrasound image demonstrating mural bladder mass.
Figure 2.
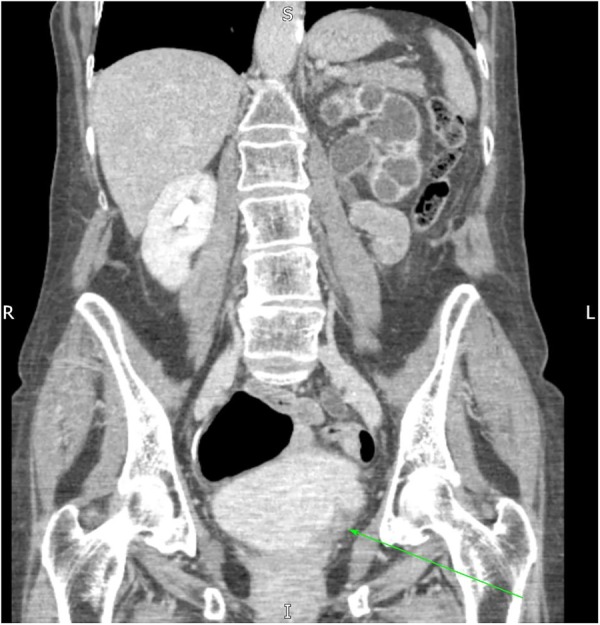
CT identifying left-sided mural bladder mass (arrow) and left-sided hydronephrosis.
Figure 3.
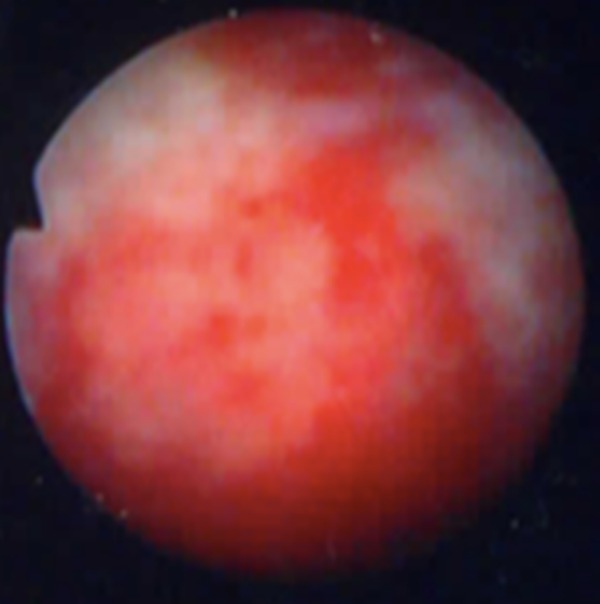
Cystocopic image of erythematous lesion.
Figure 4.
Cystocopic image of erythematous lesion.
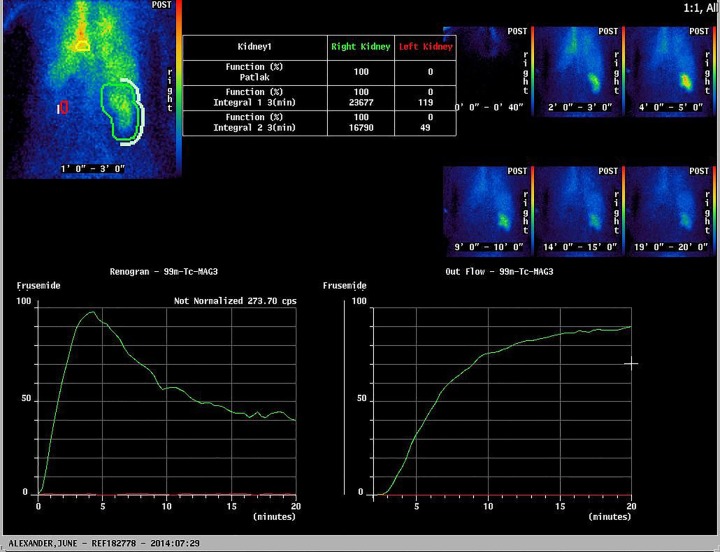
Scar tissue at the ureteric orifice led to complete ureteric obstruction. Mercaptoacetyltriglycine-3 renogram confirmed a non-functioning kidney (figure 5) and a nephrectomy was later performed due to persistent loin pain.
Figure 5.
Mercaptoacetyltriglycine-3 renogram demonstrating a non-functioning left kidney.
Discussion
Tuberculosis remains prevalent in the UK with an incidence of 12.3–35.5/100 000. Seventy-three per cent of cases diagnosed are in those born outside of the UK, and the disease remains endemic among the immunocompromised and most deprived members of our society.
Extrapulmonary tuberculosis now accounts for around half of all diagnoses, of these up to 20% are genitourinary.2 Mycobacterium tuberculosis bacilli spread to the renal parenchyma haematogenesouly where they may lay dormant for many years. Disease progression to the lower urinary tract occurs when the bacteria breach the renal medulla, here phagocyte function is impaired by its hypertonicity and the bacteria are able to flourish leading to seeding of the lower tract.
Once affected, bladder inflammation commonly causes dysuria and frequency, progression of this inflammation leads to scarring and contracture, impairing the bladders capacity to store urine, termed ‘thimble bladder’. Inflammation may cause haematuria, visible and non-visible.3 Chronic inflammation is often irreversible and there are reported cases of bladder capacity being reduced to <30 mL.4 As in the case described scarring may also be the cause of an obstructive nephropathy leading to an irreversible reduction in renal function.
Although imaging may be suggestive of genitourinary tuberculosis, diagnosis relies on microbiological evidence, typically by the detection of acid-fast bacilli in urine; tissue biopsy and PCR for M. tuberculosis may also be beneficial.5 Routine urine culture fails to identify Mycobacterium tuberculi and sterile pyuria is often reported, it is for this reason that the diagnosis, although rare, must remain a consideration, especially in those at risk.
Management is similar to that of pulmonary tuberculosis with a prolonged course of antibiotics and should be discussed with local microbiologists and respiratory physicians. Early initiation helps prevent disease progression and organ dysfunction potentially negating the need for nephrectomy or cystectomy.
Although uncommon, tuberculosis of the bladder should be considered in patients that present with storage symptoms and/or haematuria in which no other cause is identified, by keeping this in mind we may help prevent major sequelae as seen in this case.
Learning points.
Mycobacterium tuberculi can affect any organ and genitourinary tuberculosis should be considered as a differential when storage or infective symptoms are present.
Early detection of genitourinary tuberculosis can be curative and prevent irreversible disease progression.
Mycobacterium tuberculi remains prevalent in the western world and should be considered in immigrants and the immunocompromised.
Footnotes
Contributors: JAS primarily researched and wrote this manuscript. MH prepared the final manuscript and KP contributed in providing the images.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ferrie BG, Rundle JS. Genito-urinary tuberculosis in Glasgow 1970 to 1979: a review of 230 patients. Scott Med J 1985;30:30–4. [DOI] [PubMed] [Google Scholar]
- 2.Figueiredo AA, Lucon AM, Junior RF et al. Epidemiology of urogenital tuberculosis worldwide. Int J Urol 2008;15:827–32. 10.1111/j.1442-2042.2008.02099.x [DOI] [PubMed] [Google Scholar]
- 3.Kapoor R, Ansari MS, Mandhani A et al. Clinical presentation and diagnostic approach in cases of genitourinary tuberculosis. Indian J Urol 2008;24:401–5. 10.4103/0970-1591.42626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta NP, Kumar A, Sharma S. Reconstructive bladder surgery in genitourinary tuberculosis. Indian J Urol 2008;24:382–7. 10.4103/0970-1591.42622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bae EH, Heo S, Kim YH et al. Gross hematuria associated with genitourinary tuberculosis. Chonnam Med J 2013;49:48–9. 10.4068/cmj.2013.49.1.48 [DOI] [PMC free article] [PubMed] [Google Scholar]