Abstract
Objective
Although potentially traumatic events (PTEs) are established risk factors for substance use disorders among adults, little is known about associations with drug use during adolescence, an important developmental stage for drug use prevention. We examined whether childhood PTEs were associated with illicit drug use among a representative sample of US adolescents.
Method
Data were drawn from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A), which included adolescents aged 13-18 years (N=9,956). Weighted logistic regression models estimated risk ratios for lifetime use of marijuana, cocaine, nonmedical prescription drugs, other drugs, and multiple drugs.
Results
Exposure to any PTE prior to age 11 was reported by 36% of the sample and was associated with higher risk for use of marijuana (risk ratio [RR] = 1.50), cocaine (RR = 2.78), prescription drugs (RR=1.80), other drugs (RR=1.90), and multiple drugs (RR=1.74). A positive monotonic relationship was observed between number of PTEs and marijuana, other drug, and multiple drug use. Interpersonal violence was associated with all drug use outcomes. Accidents and unspecified events were associated with higher risk for marijuana, cocaine, and prescription drug use.
Conclusion
Potentially traumatic events in childhood are associated with risk for illicit drug use among US adolescents. These findings add to the literature by illustrating a potentially modifiable health behavior that may be a target for intervention; and that adolescents with a trauma history are a high-risk group for illicit drug use and may benefit from trauma-focused prevention efforts that specifically address traumatic memories and coping strategies for dealing with stressful life events.
Keywords: Substance use, illicit drugs, adolescents, childhood trauma, maltreatment
INTRODUCTION
The average age of first use of illicit drugs is during late adolescence to early adulthood,1 making adolescence an important developmental stage for education and interventions to prevent substance use and disorders.1,2 In particular, earlier age at initiation and patterns of substance use in adolescence may have a lasting influence on substance use and disorders across the life course.3,4 In order to develop and provide effective drug prevention programming to youth, it is necessary to identify adolescents at particularly high risk for illicit drug use5,6 and to investigate the factors that create this higher risk.
Although potentially traumatic events (PTEs) in childhood are established risk factors for substance use disorders in adults,7-12 scant research has examined the associations of childhood PTEs with initiation of substance use in adolescence. To our knowledge, only four previous studies explicitly examined the role of family adversity and maltreatment on substance use in adolescence. Taken together, these studies reported that aspects of family adversity were associated with earlier age of drug and alcohol use initiation,3,7,8,13 heavier alcohol use among boys reporting sexual assault,13 and drinking as a coping behavior.3 However, prior studies have been limited in several ways. First, prior studies have focused exclusively on childhood maltreatment and family dysfunction without examining other forms of trauma exposure,3,7,8,13 even though potentially traumatic events experienced outside the home are strong predictors of mental health and substance use outcomes in adult populations.14-19 Second, these studies have largely relied on the retrospective reports of adults about maltreatment and substance use in childhood and adolescence,3,7,8 which decrease in accuracy with increasing age.20-22 Third, most studies have assessed clinical or convenience samples,7,8,13 limiting the potential to provide population estimates for the efficacy of any interventions or policy changes, and precluding conclusions of whether these associations would persist among more diverse samples. Fourth, no prior studies that we are aware of have examined effects across specific types of illicit drugs that could help in understanding the etiology of drug use problems and in targeting interventions to prevent adolescent drug use.23,24 Fifth, no studies have examined whether associations between PTEs and adolescent drug use are equivalent for individuals with or without comorbid psychiatric disorders, even though there is robust evidence of multifinality following exposure to PTEs,25-27 particularly for posttraumatic stress disorder (PTSD) and substance use.28-30 Finally, prior studies have not controlled for the potential confounding or moderating effects of parental substance misuse in estimates of substance use outcomes,9,13 or have treated parental substance misuse as a direct form of adversity.3,7,10 Parental substance misuse could confound the association between childhood PTEs and adolescent drug use because of its association with exposure to a dysfunctional home environment, family violence, and other forms of trauma,31,32 as well as its influence on adolescent drug use through biological predisposition, access to drugs in the home, modeling behavior, low parental involvement, and social acceptability.3,6,33-38 Furthermore, parental substance misuse could also moderate the association between PTEs and drug use, because adolescents with a parent who misuses substances could be at higher risk for drug use due to predisposition, access, and modeling.
In summary, this is the first study to our knowledge to examine associations between a broad range of traumatic events in childhood with specific types of drug use in a nationally representative sample of adolescents, adjusting for parental substance misuse. We examine PTEs experienced during childhood and their associations with drug use in adolescence, independent of any proximal traumatic stressors occurring simultaneously with drug use. We focus on trauma exposure prior to age 11, as this is the age when most US adolescents transition from elementary to middle school, with the related exposure to older students, more independence, and potentially greater opportunities for using illicit drugs.5,6,39-41 In secondary analyses, we also assessed if any associations persist among adolescents reporting parental substance misuse, or diagnosed with distress or behavior disorders. Data were drawn from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). The primary aim of this study was to examine the association between multiple types of PTEs in childhood with use of various illicit drugs in adolescence. In addition, we also determined the role of parental substance misuse in these associations.
METHOD
Study Design and Sample
The National Comorbidity Survey–Adolescent Supplement (NCS-A) was conducted between 2001 and 2004. Adolescents were selected from households participating in the National Comorbidity Survey Replication (NCS-R) at a response rate of 86.8% (879 adolescents). An additional sample was derived from schools at a response rate of 82.6% (9,244 adolescents). The total NCS-A sample was 10,123 English-speaking adolescents, ages 13-18 years old. Data were weighted for variability in probability of selection and differential non-response based on population sociodemographic distributions. Merged weighted household and school samples were adjusted for design effects, and closely approximate the sociodemographic distribution of the 2000 US census population.42-44 Additional details about the survey design and sampling procedures are provided elsewhere.43-45 For the current study, we excluded any participant who was missing a response for any of the PTEs or survey stratification variables, creating a final analytic sample of 9,956 adolescents (98.4%). Written informed consent from parents and assent from adolescents were obtained from all participants. Study procedures were approved by Human Subjects Committees at Harvard Medical School and the University of Michigan. The current study was approved by the Human Subjects Committee at Columbia University.
Measures
Exposure: Potentially Traumatic Events
Potentially traumatic events assessed in this study included items from the Criterion A1 assessment for PTSD included in the Composite International Diagnostic Interview (CIDI) portion of the NCS-A.46 The CIDI for DSM-IV is a fully-structured diagnostic instrument administered by trained lay interviewers.47 Following prior work in this sample and others showing differential consequences of certain traumatic event types,10,44,48,49 Criterion A1 PTEs were grouped into the following categories: interpersonal violence (physical abuse by caregiver, physical assault by someone else, mugged, raped, sexually assaulted, stalked, kidnapped, or domestic violence exposure), traumatic accidents (car accident, other serious accident, natural or man-made disaster, physical illness, toxic chemical exposure, or accidentally injured someone), network or witnessing events (unexpected death of a loved one, traumatic experience of a loved one, or witnessing injury or death), and other events. This final category included a question from the PTSD instrument asking, “Did you ever experience any other extremely upsetting or life-threatening event that I haven’t asked about yet?” and a question about events that the participant did not feel comfortable disclosing to the interviewer. While we lack details of the event type for this measure, prior studies have shown this “other” category to be particularly highly associated with psychiatric disorders.44 We created a variable to assess exposure to any PTE, and a count variable assessing exposure to no PTEs, to only one PTE type, two PTE types, and three or more PTE types (due to low frequencies above this number), based on the original 19 items from the PTSD checklist.
Outcome: Lifetime Illicit Drug Use
Adolescents were asked whether they had ever used a list of illicit drugs “even once.” Respondents were asked about (1) “marijuana or hashish”; (2) “cocaine in any form, including powder, crack, free base, coca leaves, or paste”; (3) “tranquilizers, stimulants, painkillers, or other prescription drugs either without the recommendation of a health professional, or for any reason other than a health professional said you should use them”; and (4) “heroin, opium, glue, LSD, peyote, or any other drug.”45,50 We created a dichotomous variable for polydrug use by combining affirmative responses from the above list, and assigning a “yes” value if participants endorsed use of greater than one drug type.
In order to establish temporality between our exposures and outcomes, to focus on trauma experienced during childhood as a distinct developmental stage, and to capture the initiation of drug use among the vast majority of our sample, we only assessed PTEs with the first occurrence before age 11 (74% of events), and excluded drug use with first occurrence before age 11 (<1% of the sample).
Moderation and Control Variables
Baseline demographic control variables included sex, age (continuous), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other), and parent income (low income, low-middle income, high-middle income, high income). Final regression models also controlled for possible confounding by parent substance misuse (combined binary measure of adolescents’ reports of problem drinking or drug use for mothers or fathers). Interaction terms were constructed to assess moderation of the association between PTEs and drug use by parent substance misuse, as well as by lifetime distress disorder (DSM-IV diagnosis of social anxiety disorder, posttraumatic stress disorder, dysthymia, major depression, or generalized anxiety disorder) and lifetime behavior disorder (DSM-IV diagnosis of attention-deficit/hyperactivity disorder, oppositional defiant disorder, conduct disorder, anorexia nervosa, bulimia, or binge eating disorder), using classifications based on prior factor analyses in this sample.51.
Statistical Analysis
After assessing univariate and bivariate statistics for the full sample, we estimated logistic regression models for the association between PTEs and lifetime prevalence of drug use among adolescents. First, we estimated the association between any PTE and the five drugs of interest, controlling for baseline demographic variables. We then controlled for parent substance misuse in these models. We repeated these steps using a categorical variable for number of PTEs reported (0, 1, 2, 3 or more) and for specific categories of PTEs. Finally, we assessed statistical interaction between PTEs and parental substance misuse, adolescent distress disorder, and adolescent behavior disorder. For any significant interaction, regression models were stratified by the moderator of interest. Sensitivity analyses assessed whether effect estimates changed when controlling for all PTE types in the same model simultaneously.
Due to the high prevalence of some outcomes, odds ratios obtained from logistic regression models were converted to model-adjusted risk ratios using predicted marginals.52,53 Results are presented as adjusted risk ratios (RR) and 95% confidence intervals (CI)s. All analyses were conducted to account for the complex survey design of the NCS-A and included sample weights to account for differential probability of selection and to be nationally representative based on sociodemographic characteristics. Analyses were conducted using SAS-callable SUDAAN version 11.0 (Research Triangle Institute, Research Triangle Park, NC, 2012).
RESULTS
Prevalences of sociodemographic variables in this sample have been reported previously, and are representative of the 2000 US census population.54 Before age 11, 36% of participants had experienced at least one PTE, 23% reported only one type of PTE, 8% reported two, and 4% reported three or more (Table 1). Before the age of 11, 11% of participants had experienced interpersonal violence, 18% a traumatic accident, 15% had witnessed or heard about a traumatic event happening to a loved one, and 4% reported an unspecified event. For lifetime drug use, 22% had ever used marijuana, 2% cocaine, 5% prescription drugs not for medical reasons, 3% other drugs, and 6% multiple drugs.
Table 1.
Prevalencea of Potentially Traumatic Events (PTE) and Lifetime Illicit Drug Use Among Adolescents in the National Comorbidity Survey–Adolescent Supplement (N=9,956)
| Item | % (SE) | |
|---|---|---|
|
|
||
| Parent substance use problems | 19.19 (0.89) | |
| Potentially traumatic events before age 11 | Interpersonal violence | 11.06 (0.63) |
| Accident | 18.16 (0.73) | |
| Witnessing/network Event |
14.61 (0.66) | |
| Other/Non-disclosed Event |
3.85 (0.25) | |
| Any PTE | 35.60 (0.88) | |
| One PTE | 23.33 (0.57) | |
| Two PTEs | 7.67 (0.54) | |
| Three or more PTEs | 4.48 (0.31) | |
| Lifetime drug use | Marijuana | 22.44 (1.44) |
| Cocaine | 2.29 (0.33) | |
| Nonmedical Prescription Drugs |
5.11 (0.44) | |
| Other drugs | 3.07 (0.42) | |
| Multiple illicit drugs | 6.31 (0.59) | |
NOTE: Interpersonal violence includes physical abuse by caregiver, physical assault by someone else, mugged, raped, sexually assaulted, stalked, kidnapped, or domestic violence exposure. Traumatic accidents include car accident, other serious accident, natural or man-made disaster, physical illness, toxic chemical exposure, or accidentally injured someone. Network or witnessing events include unexpected death of a loved one, traumatic experience of a loved one, or witnessing injury or death. Other events include events not listed and undisclosed events.
Weighted percent (standard error).
Specific Event Types and Drug Use
Exposure to interpersonal violence before the age of 11 was associated with higher risk for lifetime use of all drug types, controlling for demographic covariates (Table 2). These effects were attenuated after controlling for parent substance misuse, but associations remained statistically significant. Interpersonal violence was associated with use of marijuana (RR=1.78, CI: 1.54-2.07), cocaine (RR=2.64, CI:1.75-3.98), nonmedical prescription drugs (RR=2.20, CI: 1.49-3.27), other drugs (RR=1.70, CI: 1.12-2.57), and multiple drugs (RR=2.31, CI:1.69-3.15).
Table 2.
Risk of Lifetime Illicit Drug Use by Exposure to Potentially Traumatic Events (PTE) Among Adolescents in the National Comorbidity Survey–Adolescent Supplement (N=9,956)
| Lifetime Substance Use (Predicted Marginal Risk Ratio, 95% CI)a | ||||||
|---|---|---|---|---|---|---|
| Potentially Traumatic Eventsb | Marijuana | Cocaine | Nonmedical Prescription Drugs |
Other Drugs | Multiple Drugs | |
| (n=2,241) | (n=234) | (n=483) | (n=302) | (n=590) | ||
|
|
||||||
| Interpersonal | Model 1 | 1.98 (1.74-2.26)* | 3.88 (2.8 1-5.37)* | 2.66 (1.84-3.83)* | 2.29 (1.57-3.34)* | 2.81 (2.12-3.71)* |
| Model 2 | 1.78 (1.54-2.07)* | 2.64 (1.75-3.98)* | 2.20 (1.49-3.27)* | 1.70 (1.12-2.57)* | 2.31 (1.69-3.15)* | |
| Accidental | Model 1 | 1.22 (1.03-1.44)* | 2.34 (1.49-3.67)* | 1.40 (0.86-2.28) | 1.59 (1.08-2.34)* | 1.35 (0.98-1.86) |
| Model 2 | 1.12 (0.94-1.33) | 2.13 (1.34-3.38)* | 1.22 (0.75-2.01) | 1.40 (0.96-2.03) | 1.20 (0.88-1.65) | |
| Witnessing | Model 1 | 1.29 (1.07-1.55)* | 1.20 (0.83-1.72) | 1.18 (0.85-1.64) | 1.58 (1.07-2.33)* | 1.25 (0.95-1.65) |
| Model 2 | 1.17 (0.99-1.38) | 0.92 (0.58-1.46) | 1.09 (0.78-1.52) | 1.45 (0.97-2.17) | 1.11 (0.83-1.47) | |
| Other | Model 1 | 1.65 (1.31-2.09)* | 1.45 (0.71-2.96) | 2.19 (1.49-3.22)* | 1.88 (1.15-3.05)* | 1.79 (1.19-2.69)* |
| Model 2 | 1.48 (1.14-1.93)* | 1.14 (0.56-2.31) | 1.84 (1.21-2.80)* | 1.58 (0.95-2.65) | 1.46 (0.93-2.28) | |
| Any PTE | Model 1 | 1.50 (1.33-1.69)* | 2.78 (1.95-3.97)* | 1.80 (1.29-2.51)* | 1.90 (1.37-2.63)* | 1.74 (1.37-2.20)* |
| Model 2 | 1.34 (1.20-1.50)* | 2.17 (1.48-3.17)* | 1.50 (1.07-2.10)* | 1.58 (1.12-2.23)* | 1.45 (1.14-1.84)* | |
| One PTE | Model 1 | 1.32 (1.19-1.48)* | 2.13 (1.26-3.58)* | 1.50 (1.02-2.20)* | 1.56 (1.03-2.36)* | 1.38 (1.02-1.87)* |
| Model 2 | 1.22 (1.11-1.35)* | 1.98 (1.21-3.25)* | 1.34 (0.91-1.98) | 1.42 (0.95-2.14) | 1.25 (0.94-1.68) | |
| Two PTEs | Model 1 | 1.65 (1.37-1.99)* | 4.23 (2.73-6.55)* | 1.90 (1.20-3.01)* | 2.11 (1.32-3.39)* | 2.25 (1.57-3.21)* |
| Model 2 | 1.41 (1.15-1.72)* | 2.61 (1.44-4.73)* | 1.38 (0.81-2.33) | 1.49 (0.82-2.73) | 1.62 (1.04-2.52)* | |
|
Three or More
PTEs |
Model 1 | 2.17 (1.72-2.74)* | 3.58 (1.88-6.81)* | 3.14 (1.95-5.06)* | 3.26 (2.05-5.19)* | 2.69 (1.82-3.97)* |
| Model 2 | 1.89 (1.47-2.43)* | 2.24 (1.18-4.22)* | 2.50 (1.53-4.09)* | 2.51 (1.54-4.10)* | 2.14 (1.41-3.23)* | |
Model 1 logistic regression results adjusted for age, sex, race/ethnicity, and parent income; Model 2 logistic regression results adjusted for age, sex, race/ethnicity, parent income, and parent substance use problems.
For specific event types and “Any PTE” models, the reference group is participants who reported no PTEs of that type. For number of PTEs, the reference group is participants who reported no PTEs, and the number of PTEs are included as a single categorical variable in each model.
p<.05
In baseline models, exposure to traumatic accidents was associated with higher risk for lifetime marijuana, cocaine, and other drug use. After controlling for parent substance misuse, effect sizes were attenuated, and only cocaine use remained statistically significant. Witnessing a traumatic event or hearing about the PTEs of loved ones was associated with higher risk for marijuana and other drug use in baseline models. However, none of these associations remained significant after controlling for parent substance misuse. Unspecified PTEs were associated with higher risk for all types of drug use save cocaine in baseline models. After controlling for parent substance misuse, other PTEs were associated with higher risk for marijuana use (RR=1.48, CI: 1.14-1.93) and cocaine use (RR=1.84, CI: 1.21-2.80).
Sensitivity analyses assessed whether these associations persisted when simultaneously estimating all four PTE classes in the same regression models. We found that effect sizes were slightly attenuated in all models, but no tests of statistical significance of PTE exposure classes were changed in any instance (results not shown). Therefore, independent of exposure to other types of PTEs, all reported associations remained statistically significant for unique PTE exposures.
Number of Traumatic Events and Drug Use
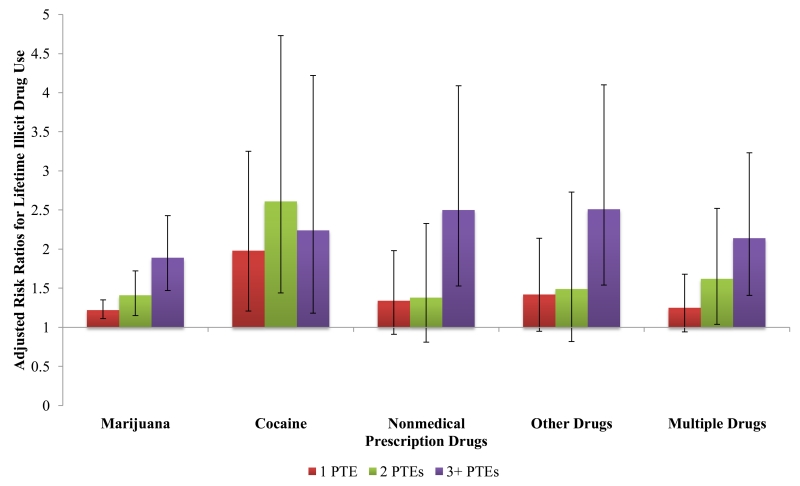
Controlling for demographic covariates, exposure to any PTE before the age of 11 was associated with higher risk for lifetime use of marijuana (RR=1.50, CI: 1.33-1.69), cocaine (RR=2.78, CI: 1.95-3.97), nonmedical prescription drugs (RR=1.80, CI: 1.29-2.51), other drugs (RR=1.90, CI: 1.37-2.63), and multiple drugs (RR=1.74, CI: 1.37-2.20) (Table 2). Controlling for parent substance misuse attenuated these effect estimates; however, all remained statistically significant. There was evidence of a positive monotonic relationship for number of PTEs experienced and risk of marijuana, other drug, and polydrug use (Figure 1). Controlling for demographic covariates and parent substance misuse, any, one, two, and three or more childhood PTEs reported were all statistically associated with higher risk for marijuana and cocaine use.
Figure 1.
Adjusted risk ratios and 95% CIs for lifetime illicit drug use associated with number of potentially traumatic experiences before age 11 among adolescents in the National Comorbidity Survey–Adolescent Supplement (N=9,956). Note: For each model, the reference group is adolescents exposed to no potentially traumatic events (PTEs) prior to age 11. All models adjusted for age, sex, race/ethnicity, parent income, and parent substance use problems.
Moderation by Parent Substance Misuse and Adolescent Psychiatric Disorders
Our results indicated that parental substance misuse largely failed to moderate the association between PTEs and adolescent drug use. Significant interactions were only observed for two drug use types. Adolescents reporting parent substance misuse were at higher risk for lifetime marijuana use associated with other PTEs (RR=1.63, CI: 1.28-2.07), compared to adolescents reporting no parent substance misuse (RR=1.38, CI: 1.00-1.90; pinteraction=.046). Adolescents reporting parent substance misuse were also at higher risk for use of other drugs associated with interpersonal PTEs (pinteraction=.02), any PTE (pinteraction=.02), and number of PTEs (pinteraction=.001), compared to adolescents not reporting parent substance misuse.
Similarly, adolescent distress disorders and behavioral disorders mostly did not moderate the associations between PTEs and drug use. The single exception was for interpersonal violence PTEs and nonmedical prescription drug use, where adolescents without a history of behavior disorder were at higher risk for prescription drug use (RR=3.00, CI: 1.92-4.70) compared to adolescents with a history of behavior disorder (RR=1.45, CI: 0.95-2.22; pinteraction=.0008).
DISCUSSION
In this population-representative sample of US adolescents, exposure to any PTE in childhood was associated with higher risk for lifetime use of all illicit drugs assessed. We found evidence for a dose-response relationship between number of PTEs experienced and marijuana, other drug, and polydrug use. Interpersonal violence experienced in childhood was consistently associated with lifetime use of all illicit drugs assessed, even after controlling for the confounding effect of parent substance misuse, which attenuated the effect sizes of many of the associations assessed. To our knowledge, this is the first population-based study to report that traumatic events other than childhood maltreatment are associated with higher risk for marijuana, cocaine, and nonmedical prescription drug use among adolescents.
Consistent with prior research using both the NCS-A and the adult sample of the National Comorbidity Survey (NCS-R), childhood maltreatment and interpersonal violence are strongly associated with multiple psychiatric and behavioral outcomes.10,11,44,46 Combined with results from previous studies on diverse health outcomes, our findings here confirm that these forms of physical and sexual violence exhibit multifinality in that they are associated with elevated risk for multiple adverse outcomes, including health behaviors, not only diagnosed disorders.44,46,48 Health behaviors such as adolescent drug use may be modifiable risk factors that can be targeted to prevent future adverse health outcomes.55 Efforts to prevent the particularly devastating forms of trauma such as physical, sexual, and domestic violence should be at the forefront. Researchers should continue to explore risk factors for the perpetration of this violence in order to inform policy and social welfare initiatives with an evidence-based primary prevention approach.
Although our measure of interpersonal violence comprised many of the indicators that are usually included in studies of childhood maltreatment (i.e., physical and sexual assault, domestic violence), our results also indicate that other forms of trauma are also associated with illicit drug use in adolescents when interpersonal violence exposure was controlled for in statistical models. Adolescents who experienced accidental PTEs were at elevated risk specifically for cocaine use. Prior work has shown that the association between unintentional or accidental events and adverse outcomes are generally less robust.56,57 However, particularly in an adolescent sample, perhaps these accidents and illnesses pose more real threat of death than other events, thus making the “dose” of traumatic stress stronger in this category.56-60 Future research should try to replicate these findings to determine whether this specificity of association persists in other populations, and if so, by what mechanism it may act. Specifically, researchers and clinicians should explore the nature of these events and their consequences, and try to determine whether the specific association with cocaine use has any relationship to the type of medical treatment received following these accidents or illnesses.
Events not disclosed to the survey team by participants were associated with higher risk for marijuana and non-medical prescription drug use, in line with past work showing that other/private events are associated with onset of psychiatric disorders and persistence of PTSD.44 This should be noted by researchers conducting future life events surveys, if study participants are less likely to report certain types of traumatic events. Healthcare workers and caregivers should also be aware of increased risk for drug use arising from undisclosed traumatic events.
The strongest effect sizes were for interpersonal violence and risk of cocaine and nonmedical prescription drug use, and for traumatic accidents and cocaine use. Future studies should explore whether these associations are driven by socio-environmental factors related to access to different drug types or whether there is something about the psychoactive effects of cocaine and some prescription drugs that is specifically sought by adolescents coping with traumatic memories.
The substantial confounding by parent substance misuse that we observed also deserves more attention in future studies. The associations between interpersonal violence and drug use outcomes were confounded by parent substance misuse, indicating a domestic environment with multiple forms of inter-related traumas for some children. Future studies should examine the mechanisms by which parental substance use and exposure to traumatic events are associated with adolescent substance use, for example through an influence on social norms and expectancies, modeling behavior, access to illicit substances, or by providing opportunity via low parental involvement or neglect.3,6,33-38 These explorations were beyond the scope of the current study, but future research can inform priorities for intervention in harmful home environments for children and adolescents. By and large, parent substance misuse did not affect the associations between PTEs and drug use. Exceptions included other PTEs and marijuana use, and interpersonal PTEs and other drug use. This could be related to access to drugs in the home or neighborhood, as marijuana and certain types of other drugs may be more easily obtained by adolescents. Alternatively, this statistical interaction could represent a constellation of adversity related to family dysfunction, as discussed in prior studies.10,46 Future work should utilize latent variable techniques to further explore these complex associations and pathways.
Given the breadth of exposures and outcomes assessed in the current study, it was beyond the scope of this article to assess the multiple possible mechanisms by which PTEs are associated with adolescent substance use. Future studies, ideally using longitudinal data, should continue to explore these patterns by conducting formal tests of mediation, assessing indirect effects of PTEs through distress and behavior disorders on substance use among both boys and girls. Additional avenues for future work include examination of the ways in which social norms, peer groups, sociodemographic factors, and drug availability affect these associations, and whether any protective factors exist that could be used to design interventions and educational campaigns for adolescents.
A number of limitations should be considered in interpreting these results. First, all associations reported here should be interpreted with caution, due to the cross-sectional nature of the data. However, our results are consistent with numerous prior studies3,7,8,10 reporting associations between childhood trauma and drug use outcomes. Furthermore, the potential for reverse causation is minimized because we only included PTEs experienced before the age of 11 and drug use after the age of 10.
A second concern is the retrospective reporting of both PTEs and lifetime drug use. While the potential for recall bias is reduced in younger participants with shorter lags between timing of event and reporting of event,20-22 we still cannot rule out the possibility of under-reporting of drug use due to social desirability bias and under-reporting of PTEs due to forgetting or trauma-related non-acceptance. These biases could result in either over-estimation or underestimation of results reported here. However, the prevalence of drug use reported in the NCS-A is consistent with or higher than that reported in other surveys,50,61,62 and the prevalence of any exposure to PTEs is only slightly lower than that of adult samples,44,63 suggesting that under-reporting may not be of great concern in this study.
Third, as noted above, confounding of the association between PTEs and drug use could be due to parental substance misuse, which we adjust for in final models. However, parental substance misuse could also be a direct outcome of a PTE, if the event was experienced by both the parent and the child (e.g. death of a loved one, car accidents). Including this variable in statistical models may therefore induce bias in these estimates. As we are unable to tease out the temporality of these variables in the NCS-A dataset, we present models both unadjusted and adjusted for parental substance misuse, for comparison. We also conducted interaction tests to assess moderation by parental substance misuse, and mostly found no significant differences, as noted above. Future studies should utilize longitudinal data to further explore these associations.
Fourth, another limitation is common to all studies using the PTSD Criterion A1 list of PTEs. This list of event types does not adequately capture the “dose” of the traumatic experience, the severity of the event, or the context in which the event was experienced.64 This makes it difficult to determine whether familial and sexual violence experiences are more strongly associated with deleterious outcomes because they are chronic experiences of trauma occurring within a child’s home, or because the events themselves are more “toxic”.59 Complementary research should continue to assess these more qualitative aspects of traumatic stress.
This study adds to the large body of research documenting the potentially toxic effects of psychological trauma to a wide range of behavioral and health outcomes beyond PTSD. These findings add to the childhood adversity literature by demonstrating: (1) that PTEs experienced in childhood are associated with drug use in adolescence – a potentially modifiable health behavior – and therefore a target for intervention and treatment in youth and (2) that adolescents with a trauma history are a high-risk group for illicit drug use and may benefit from prevention efforts that specifically address traumatic memories and coping strategies for dealing with stressful life events. Future work should explore whether adolescents with a trauma history are more likely to develop chronic or harmful drug use than their non-traumatized peers. In combination with other signs and indicators, early drug use can act as a marker for adolescents who may need additional support or intervention. For clinicians, our results combined with other studies imply that drug treatment programs may need to more directly address childhood trauma in their therapeutic approach. Early interventions targeting coping with trauma during this critical period of adolescence could have broad benefits to health and wellbeing of adults.
Acknowledgments
This work is supported in part by National Institutes of Health grants T32DA031099 (Carliner, PI: Hasin), MH102403 (Dunn), AA021511 (Keyes), R01DA037866 (Martins), R01HD060072 (Martins), MH106482 (McLaughlin), and MH103291 (McLaughlin).
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Preliminary results for this study were presented as an oral presentation at the College on Problems of Drug Dependence’s 77th Annual Meeting, Phoenix, AZ, June 13-18, 2015.
Disclosure: Drs. Carliner, Keyes, McLaughlin, Meyers, Dunn, and Martins report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Dr Hannah Carliner, Columbia University, New York.
Dr Katherine M. Keyes, Columbia University, New York.
Dr. Katie A. McLaughlin, University of Washington, Seattle.
Dr. Jacquelyn L. Meyers, State University of New York (SUNY) Downstate Medical Center, Brooklyn, New York.
Dr. Erin C. Dunn, Massachusetts General Hospital, Boston.
Dr Silvia S. Martins, Columbia University, New York.
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2013 national survey on drug use and health: Summary of national findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. [Google Scholar]
- 2.Faden VB. Trends in initiation of alcohol use in the United States 1975 to 2003. Alcohol Clin Exp Res. 2006;30:1011–1022. doi: 10.1111/j.1530-0277.2006.00115.x. [DOI] [PubMed] [Google Scholar]
- 3.Rothman EF, Edwards EM, Heeren T, Hingson RW. Adverse childhood experiences predict earlier age of drinking onset: results from a representative US sample of current or former drinkers. Pediatrics. 2008;122:e298–304. doi: 10.1542/peds.2007-3412. [DOI] [PubMed] [Google Scholar]
- 4.Bounoua N, Ali B, Lim A, et al. Early initiation of alcohol and illicit drug use: Associations with psychopathology among inpatient substance users. Drug Alcohol Depend. 2015;146:e227. [Google Scholar]
- 5.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 6.Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 7.Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood Abuse, Neglect, and Household Dysfunction and the Risk of Illicit Drug Use: The Adverse Childhood Experiences Study. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- 8.Dube SR, Miller JW, Brown DW, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:444, e441–444, e410. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Elliott JC, Stohl M, Wall MM, et al. The risk for persistent adult alcohol and nicotine dependence: the role of childhood maltreatment. Addiction. 2014;109:842–850. doi: 10.1111/add.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green JG, McLaughlin KA, Berglund PA, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allem J-P, Soto DW, Baezconde-Garbanati L, Unger JB. Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addict Behav. 2015;50:199–204. doi: 10.1016/j.addbeh.2015.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamburger ME, Leeb RT, Swahn MH. Childhood maltreatment and early alcohol use among high-risk adolescents. J Stud Alcohol Drugs. 2008;69:291–295. doi: 10.15288/jsad.2008.69.291. [DOI] [PubMed] [Google Scholar]
- 14.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 16.Norris FH, Murphy AD, Baker CK, Perilla JL, Rodriguez FG, Rodriguez Jde J. Epidemiology of trauma and posttraumatic stress disorder in Mexico. J Abnorm Psychol. 2003;112:646–656. doi: 10.1037/0021-843X.112.4.646. [DOI] [PubMed] [Google Scholar]
- 17.Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J Clin Psychiatry. 2000;61(Suppl 7):22–32. [PubMed] [Google Scholar]
- 18.Brunello N, Davidson JR, Deahl M, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology. 2001;43(3):150–162. doi: 10.1159/000054884. [DOI] [PubMed] [Google Scholar]
- 19.Hien D, Cohen L, Campbell A. Is traumatic stress a vulnerability factor for women with substance use disorders? Clinical Psychology Review. 2005;25(6):813–823. doi: 10.1016/j.cpr.2005.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dobson A, Smith N, Panchana N. Some problems with life event lists and health outcomes. International journal of behavioral medicine. 2005;12(3):199–205. doi: 10.1207/s15327558ijbm1203_9. [DOI] [PubMed] [Google Scholar]
- 21.Parra GR, O’Neill SE, Sher KJ. Reliability of self-reported age of substance involvement onset. Psychol Addict Behav. 2003;17:211–218. doi: 10.1037/0893-164X.17.3.211. [DOI] [PubMed] [Google Scholar]
- 22.Della Femina D, Yeager CA, Lewis DO. Child abuse: Adolescent records vs. adult recall. Child abuse & neglect. 1990;14(2):227–231. doi: 10.1016/0145-2134(90)90033-p. [DOI] [PubMed] [Google Scholar]
- 23.Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Education Research. 2001;16(4):457–469. doi: 10.1093/her/16.4.457. [DOI] [PubMed] [Google Scholar]
- 24.Rigg KK, Ibañez GE. Motivations for non-medical prescription drug use: A mixed methods analysis. Journal of Substance Abuse Treatment. 2010;39(3):236–247. doi: 10.1016/j.jsat.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flouri E, Kallis C. Adverse Life Events and Psychopathology and Prosocial Behavior in Late Adolescence: Testing the Timing, Specificity, Accumulation, Gradient, and Moderation of Contextual Risk. J Am Acad Child Adolesc Psychiatry. 2007;46:1651–9. doi: 10.1097/chi.0b013e318156a81a. [DOI] [PubMed] [Google Scholar]
- 26.Gibb BE, Chelminski I, Zimmerman M. Childhood emotional, physical, and sexual abuse, and diagnoses of depressive and anxiety disorders in adult psychiatric outpatients. Depress Anxiety. 2007;24:256–263. doi: 10.1002/da.20238. [DOI] [PubMed] [Google Scholar]
- 27.Hammen C, Brennan PA, Shih JH. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. J Am Acad Child Adolesc Psychiatry. 2004;43:994–1002. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- 28.Ouimette PE, Brown PJ. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. American Psychological Association; Washington, DC: 2003. [Google Scholar]
- 29.Conway KP, Swendsen J, Husky MM, He J-P, Merikangas KR. Association of Lifetime Mental Disorders and Subsequent Alcohol and Illicit Drug use: Results from the National Comorbidity Survey–Adolescent Supplement. J Am Acad Child Adolesc Psychiatry. 2016;55:280–8. doi: 10.1016/j.jaac.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 30.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Psychiatric Comorbidity of Full and Partial Posttraumatic Stress Disorder among Older Adults in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Am J Geriatric Psychiatry. 2012;20:380–390. doi: 10.1097/JGP.0b013e31820d92e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chatterji P, Markowitz S. The impact of maternal alcohol and illicit drug use on children’s behavior problems: evidence from the children of the national longitudinal survey of youth. Journal of Health Economics. 2001;20(5):703–731. doi: 10.1016/s0167-6296(01)00090-x. [DOI] [PubMed] [Google Scholar]
- 32.Walsh C, MacMillan HL, Jamieson E. The relationship between parental substance abuse and child maltreatment: findings from the Ontario Health Supplement. Child Abuse Negl. 2003;27:1409–1425. doi: 10.1016/j.chiabu.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 33.Kandel DB, Wu P. The contributions of mothers and fathers to the intergenerational transmission of cigarette smoking in adolescence. J Res Adolesc. 1995;5:225–252. [Google Scholar]
- 34.Wickrama KAS, Rand DC, Wallace LE, Elder GH., Jr The Intergenerational Transmission of Health-Risk Behaviors: Adolescent Lifestyles and Gender Moderating Effects. Journal of Health and Social Behavior. 1999;40(3):258–272. [PubMed] [Google Scholar]
- 35.Biederman J, Faraone SV, Monuteaux MC, Feighner JA. Patterns of Alcohol and Drug Use in Adolescents Can Be Predicted by Parental Substance Use Disorders. Pediatrics. 2000;106(4):792–797. doi: 10.1542/peds.106.4.792. [DOI] [PubMed] [Google Scholar]
- 36.Merikangas KR, Stolar M, Stevens DE, et al. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998 Nov;55(11):973–979. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- 37.Latvala A, Tuulio-Henriksson A, Perälä J, et al. Prevalence and correlates of alcohol and other substance use disorders in young adulthood: a population-based study. BMC psychiatry. 2009;9(1):73. doi: 10.1186/1471-244X-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chassin L, Pillow DR, Curran PJ, Molina BS, Barrera M., Jr Relation of parental alcoholism to early adolescent substance use: a test of three mediating mechanisms. Journal of abnormal psychology. 1993;102(1):3. doi: 10.1037//0021-843x.102.1.3. [DOI] [PubMed] [Google Scholar]
- 39.Wilson N, Battistich V, Syme SL, Boyce WT. Does elementary school alcohol, tobacco, and marijuana use increase middle school risk? J Adolesc Health. 2002;30:442–447. doi: 10.1016/s1054-139x(01)00416-5. [DOI] [PubMed] [Google Scholar]
- 40.Guo JIE, Hill KG, Hawkins JD, Catalano RF, Abbott RD. A Developmental Analysis of Sociodemographic, Family, and Peer Effects on Adolescent Illicit Drug Initiation. J Am Acad Child Adolesc Psychiatry. 2002;41:838–845. doi: 10.1097/00004583-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 41.Martin CA, Kelly TH, Rayens MK, et al. Sensation Seeking, Puberty, and Nicotine, Alcohol, and Marijuana Use in Adolescence. J Am Acad Child Adolesc Psychiatry. 2002;41:1495–1502. doi: 10.1097/00004583-200212000-00022. [DOI] [PubMed] [Google Scholar]
- 42.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18:69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kessler RC, Avenevoli S, Costello EJ, et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry. 2009;48:380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McLaughlin KA, Koenen KC, Hill ED, et al. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52:815–830. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48:367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McMahon SD, Grant KE, Compas BE, Thurm AE, Ey S. Stress and psychopathology in children and adolescents: is there evidence of specificity? J Child Psychol Psychiatry. 2003;44:107–133. doi: 10.1111/1469-7610.00105. [DOI] [PubMed] [Google Scholar]
- 49.Vachon DD, Krueger RF, Rogosch FA, Cicchetti D. ASsessment of the harmful psychiatric and behavioral effects of different forms of child maltreatment. JAMA Psychiatry. 2015:1135–1142. doi: 10.1001/jamapsychiatry.2015.1792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Swendsen J, Burstein M, Case B, et al. Use and abuse of alcohol and illicit drugs in US adolescents: Results of the National Comorbidity Survey-Adolescent Supplement. Arch Gen Psychiatry. 2012;69:390–398. doi: 10.1001/archgenpsychiatry.2011.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kessler RC, Avenevoli S, McLaughlin KA, et al. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Psychological Medicine. 2012;42(9):1997–2010. doi: 10.1017/S0033291712000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating Model-Adjusted Risks, Risk Differences, and Risk Ratios From Complex Survey Data. Am J Epidemiol. 2010;171:618–23. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 53.Research Triangle Institute . SUDAAN Language Manual. 1 and 2. Research Triangle Institute; Research Triangle Park, NC: 2012. Release 11. [Google Scholar]
- 54.Merikangas KR, He J-p, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication?Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–990. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Substance Abuse and Mental Health Services Administration (SAMHSA) SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. [Google Scholar]
- 56.Bowman ML, Yehuda R. Risk Factors and the Adversity-Stress Model. In: Rosen GM, editor. Posttraumatic Stress Disorder: Issues and Controversies. John Wiley and Sons, Ltd; Hoboken, NJ: 2004. [Google Scholar]
- 57.Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. J Trauma Stress. 2009;22:227–35. doi: 10.1002/jts.20406. [DOI] [PubMed] [Google Scholar]
- 58.Kira IA. Taxonomy of Trauma and Trauma Assessment. Traumatology. 2001;7:73–86. [Google Scholar]
- 59.Kira IA, Lewandowski L, Templin T, Ramaswamy V, Ozkan B, Mohanesh J. Measuring Cumulative Trauma Dose, Types, and Profiles Using a Development-Based Taxonomy of Traumas. Traumatology. 2008;14(2):62–87. [Google Scholar]
- 60.Keenan EK. Seeing the forest and the trees: using dynamic systems theory to understand “stress and coping” and “trauma and resilience”. J Hum Behav Soc Environ. 2010;20:1038–60. [Google Scholar]
- 61.Fryar CD, Merino MC, Hirsch R, Porter KS. Smoking, Alcohol Use, and Illicit Drug Use Reported by Adolescents Aged 12–17 years: United States, 1999-2004. US Dept of Health and Human Services; Washington, DC: 2009. [PubMed] [Google Scholar]
- 62.Johnston L, O’Malley P, Bachman J, Schulenberg J. Marijuana use is rising; ecstasy use is beginning to rise; and alcohol use is declining among US teens. University of Michigan News Service; Ann Arbor, MI: 2010. [Google Scholar]
- 63.Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R) J Behav Med. 2008;31:341–349. doi: 10.1007/s10865-008-9158-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychol Bull. 2006;132:477. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]