Abstract
Objective
To evaluate the association between exposure to childhood adversity and insomnia, with an emphasis on the role of adversity type, timing, and accumulation (i.e. the number of specific types of adversities the child reported being exposed to).
Methods
Our analytic sample comprised 9,582 adolescents from the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), a nationally-representative population-based sample. We examined the association between 18 different types of retrospectively-reported adversities (capturing interpersonal violence, accidents and injuries, social network or witnessing events, other adverse events) and risk of self-reported past-year insomnia. We also examined whether the age at first exposure to adversity was associated with risk for insomnia, and whether exposure to a greater number of different types of adversities (i.e. accumulation) conferred an elevated risk for insomnia. Additionally, we performed a sensitivity analysis excluding adolescents with a past-year diagnosis of major depression, dysthymia, post-traumatic stress disorder, or generalized anxiety disorder.
Results
Almost one third of adolescents reported insomnia, with a higher prevalence among girls and those from racial/ethnic minority groups. Adolescents exposed to at least one childhood adversity of any type (59.41%) were more likely than their non-exposed peers to experience insomnia (across adversities, prevalence ratios ranged from 1.31 to 1.89). Risk of insomnia differed based on the age at first exposure to adversity as well as the type of adversity. Adolescents exposed to a greater number of different types of adversities had a higher risk of insomnia compared to those experiencing fewer adversities. These results were similar, by and large, to those obtained after excluding adolescents with at least one of the four past-year psychiatric disorders.
Conclusions
Exposure to adversity confers an elevated risk for insomnia. This association varied by type, timing, and accumulation of exposure and did not appear to be driven by psychiatric disorders. Given the well-documented physical and mental health consequences of insomnia, such findings add further support to the need for practitioners to screen children for exposure to childhood adversity and insomnia symptoms.
Keywords: Childhood Adversity, Insomnia, Sensitive Periods
Introduction
Upwards of 48% of children in the United States experience one or more types of childhood adversity, such as abuse or neglect, parental death, and witnessing violence1,2. Exposure to childhood adversity is now recognized as one of the major determinants of health across the lifespan3. Indeed, numerous studies have shown, in both youth and adults, that childhood adversity exposure is associated with a doubling in the risk for mental health problems4–6, increased risk for physical health risk factors and disease outcomes7,8 and appears to elevate risk for premature mortality9,10.
Relatively little is known about the association between childhood adversity and sleep problems, especially insomnia or insomnia symptoms, which is the most reported type of sleep disturbance among adolescence11–13, a major correlate of health problems14, and among the top concerns raised by parents to health professionals15. To date, most studies of adversity and sleep have examined childhood maltreatment, namely exposure to abuse or neglect16,17. These studies have generally observed at least a 20% greater risk of insomnia, insomnia symptoms, or other sleep problem among adolescents and adults exposed to maltreatment during childhood16–24. However, only a handful of these studies have been conducted in population-based samples, especially of youth. Even fewer have examined other childhood adversities beyond maltreatment, such as witnessing violence, which is more common than child maltreatment25. However, the handful of studies focusing on a broader array of adversities (see for example24,26) tend to show a significant dose-response relationship whereby each additional exposure to a unique adverse event confers a greater risk for poor sleep quality in adulthood. In addition, it remains unclear whether all childhood adversities are equally damaging across all stages of development or whether there are “sensitive periods” when the negative effects of adversity are particularly heightened27–30. Identification of these sensitive periods is needed to determine the high-risk stages of development when efforts by practitioners would be most helpful to ensure healthy child development and build the foundation for adult health31.
The goal of this study was to examine, in a large population-based sample of adolescents, the association between childhood adversity and insomnia. First, we examined whether children exposed to different types of adversity were more likely than their unexposed peers to experience insomnia. Second, we examined whether the age at first exposure to adversity was associated with risk for insomnia, consistent with the notion of sensitive periods. Finally, to replicate previous findings, we also evaluated whether there was a dose-response relationship between the number of different types of adversities reported (i.e. accumulation) and insomnia. This accumulation score, which is derived by summing across the unique type of adversities reported, is consistent with the “ACE score” (e.g., adversity childhood experiences”) calculated by the Adversity Childhood Experiences Study9, a well-known study of the health consequences of childhood maltreatment among members of the Kaiser Permanente Health Maintenance Organization. Additionally, we performed a sensitivity analysis to examine whether these results were the same after excluding adolescents experiencing a past-year diagnosis of major depression, dysthymia, post-traumatic stress disorder, or generalized anxiety disorder, as these psychiatric disorders are known correlates of insomnia32–36. We hypothesized that exposure to adversity of any type and accumulation of adversity would be associated with insomnia symptoms. However, given the lack of prior research, we did not have any a priori hypotheses concerning the effects of age at onset to adversity and insomnia.
Methods
Sample
Data came from the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), the first nationally representative study to provide estimates of the prevalence and correlates of mental and other health problems among English-speaking U.S. adolescents. Description of the sampling has been noted elsewhere37. Briefly, NCS-A investigators conducted face-to-face interviews with 10,148 adolescents ages 13 through 18 between February 2001 and January 2004 from the continental US. Adolescents were sampled through a dual-frame sample comprised of adolescents from households in the National Comorbidity Survey Replication (NCS-R)38 (household subsample n=904) and adolescents from a representative sample of schools in the adult sample areas of the NCS-R (school subsample n=9,244 adolescents in 320 schools). The overall response rate was 75.6% (74.7% school-based sample and 85.9% household sample)37. The Human Subjects Committees of Harvard Medical School and the University of Michigan approved NCS-A study recruitment and informed consent procedures. Parent-written informed consent and adolescent-written informed assent were obtained prior to interview completion. In this study, we analyzed data from adolescents with valid sampling weights and complete data on all variables (n=9,582; 94.42% of the total sample) (Table 2). Participants in our analytic sample (n=9582) did not differ from those who were excluded (n=566) with respect to most demographic characteristics, including age, race, gender, poverty level and urbanicity. However, the excluded sample comprised less youth from families with college and graduate education (27.0% versus 35.8%; p=0.004).
Table 2.
Distribution of covariates in the total sample and by those reporting insomnia and exposure to any childhood adversity
| Total Sample | With Insomnia | χ2 | p-value | Exposed to any childhood adversity | χ2 | p-value | ||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N=9,582 | N=2065 (21.6%) | N=5693 (59.4%) | ||||||
| Age | 13 | 1,564 (15.1) | 287 (18.5) | 6.85 | 0.23 | 776 (49.0) | 73.53 | <0.001 |
| 14 | 2,091 (20.8) | 413 (21.7) | 1,109 (53.6) | |||||
| 15 | 1,797 (20.8) | 418 (24.0) | 1,061 (57.5) | |||||
| 16 | 1,903 (20.9) | 438 (23.0) | 1,206 (61.7) | |||||
| 17 | 1,662 (17.0) | 391 (22.4) | 1,139 (68.8) | |||||
| 18 | 565 (5.5) | 118 (17.8) | 403 (69.1) | |||||
|
| ||||||||
| Sex | Male | 4,707 (51.3) | 835 (17.9) | 33.73 | <.001 | 2,774 (57.9) | 0.46 | 0.50 |
| Female | 4,875 (48.7) | 1,230 (25.9) | 2,919 (59.3) | |||||
|
| ||||||||
| Race | White | 5,357 (65.9) | 1,077 (20.8) | 10.61 | 0.01 | 2,983 (54.9) | 72.93 | <0.001 |
| Black | 1,849 (15.0) | 458 (26.0) | 1,269 (70.7) | |||||
| Hispanic | 1,803 (14.2) | 396 (21.1) | 1,102 (63.2) | |||||
| Other | 573 (4.9) | 134 (26.5) | 339 (59.2) | |||||
|
| ||||||||
| Parental Education | <HS | 1554 (15.3) | 359 (20.7) | 2.12 | 0.55 | 943 (58.2) | 45.34 | <.0001 |
| HS | 2913 (29.7) | 670 (22.8) | 1801 (62.8) | |||||
| Some college | 1890 (19.2) | 402 (22.9) | 1203 (64.1) | |||||
| College & Graduate | 3225 (35.8) | 634 (20.9) | 1746 (52.2) | |||||
|
| ||||||||
| Poverty | Low income | 1,603 (14.6) | 356 (21.2) | 1.25 | 0.74 | 1,021 (64.4) | 11.90 | 0.008 |
| Low-middle income | 1,911 (19.2) | 425 (21.9) | 1,166 (60.9) | |||||
| High-middle income | 2,943 (31.9) | 622 (22.6) | 1,718 (57.1) | |||||
| High income | 3,125 (34.3) | 662 (21.3) | 1,788 (56.6) | |||||
|
| ||||||||
| Region | Northeast | 1,775 (18.0) | 415 (23.3) | 6.97 | 0.07 | 987 (54.4) | 20.39 | <0.001 |
| Midwest | 2,612 (23.1) | 571 (21.2) | 1,535 (58.4) | |||||
| South | 3,276 (36.2) | 622 (19.9) | 1,947 (57.2) | |||||
| West | 1,919 (22.7) | 457 (24.2) | 1,224 (64.8) | |||||
|
| ||||||||
| Urban | Metro | 4264 (47.3) | 963 (22.8) | 5.45 | 0.06 | 2598 (61.1) | 8.96 | 0.0113 |
| Other urban | 3137 (37.9) | 694 (21.9) | 1854 (57.0) | |||||
| Rural | 2181 (14.8) | 408 (18.2) | 1241 (55.4) | |||||
Cell entries are the number and percent. The percent entries under Total Sample sum up to 100% while the percent entries by insomnia and exposure to any adversity are proportions within each level of covariates. Exposed to any childhood adversity was defined as experiencing at least one of the following adversities: parent violence, other violence, rape, kidnapping, other sexual assault, car accident, disaster, illness, chemical exposure, other accident, witnessing fights at home, witnessing death, other person died unexpectedly, other persona experienced unexpected threat, war/terror, refugee, other trauma, or non-disclosed trauma. Rao-Scott chi-square values indicate whether the distribution of demographic covariates was significantly different by those with insomnia or reporting childhood adversity.
Measures
Exposure to childhood adversity
Adolescents reported through structured interviews whether they had experienced 18 potentially traumatic events and if so, the age at first experience. These events are commonly included in measures of childhood adversity39 and were included in the NCS-A as part of the Composite International Diagnostic Interview (CIDI) to assess presence or absence of post-traumatic stress disorder. We grouped these events into four types (i.e. interpersonal violence, accidents and injuries, social network or witnessing events, other), consistent with prior empirical studies based on the NCS-A40 and other datasets41. We then generated three predictor variables from this data: presence or absence of each childhood adversity (18 events), presence or absence of each childhood adversity type (4 types), and age at first exposure to each adversity or adversity type. Age at first exposure was characterized into three unique developmental timing windows, similar to prior studies30,42,43: (1) early childhood (between ages 0–5); (2) middle childhood (ages 6–10); and (3) adolescence (ages 11–18). By using these age groupings, we were able to maintain consistency with prior studies. Of note, we observed that adolescents were very good reporters of their age at onset to specific events. For instance, the correlation between parent- and child-reported age at onset to child major depressive disorder was very high (r=0.81).
The first group of adversities included acts of interpersonal violence: (1) Parent Violence: “Badly beaten up by your parents or the people who raised you”; (2) Other Violence: “Badly beaten up by anyone else”; (3) Rape: “…someone either having sexual intercourse with you or penetrating your body with a finger or object when you did not want them to, either by threatening you or by using force”; (4) Kidnapped: “Kidnapped or held captive”; and (5) Other sexual assault: “Other than rape, ever sexually assaulted or molested”.
The second group of adversities involved accidents and injuries: (7) Car accident: “Involved in a very serious or life-threatening car accident”; (8) Disaster: “Involved in a major disaster, like a devastating flood, hurricane, fire, bomb explosion, tornado, or earthquake”; (9) Illness: “Have a very serious or life threatening illness”; (10) Chemical: “Exposed to a poisonous chemical or substance that could cause you serious harm”; and (11) Other accident: “Have any other very serious or life threatening accident”.
The third group involved social network or witnessing events: (13) Witnessed fights at home: “Witness serious physical fights at home, like when your father beat up your mother”; (14) Witness death: “Seen someone badly injured or killed or unexpectedly seen a dead body”; (15) Other person died unexpectedly: “Someone very close to you die unexpectedly, for example, they were killed in an accident, murdered, committed suicide, or had a fatal heart attack at a young age”; (16) Other person unexpected threat: “Anyone very close to you ever have a very stressful or life-threatening experience, like being kidnapped, tortured, or raped”; (17) War Terror: “Live in a place where there was war or ongoing terror”; and (16) Refugee: “A refugee, that is, did you ever flee from your home to a foreign country or place to escape danger or persecution).
The fourth group included other adversities: (18) Other trauma: “Experience any other extremely upsetting or life threatening event that I haven’t asked you about”; (19) Non-disclosed event: “Sometimes people have experiences they don’t want to talk about in interviews. I won’t ask you to describe anything like this, but, without telling me what it was, did you ever have an extremely upsetting or life-threatening event that you didn’t tell me about because you didn’t want to talk about it”.
Insomnia
Consistent with previous studies of adolescents11,44 and the International classification of sleep disorders 2 (ICSD-II) 45,46 insomnia definition for adults, insomnia was defined as the presence of daytime sleepiness in addition to at least one of the following other self-reported sleep problems, occurring for two weeks or longer in the past year: (1) have problems getting to sleep, when nearly every night it took you a long time to fall asleep; (2) have problems staying asleep, when you woke up nearly every night and took a long time to get back to sleep; (3) have problems waking too early, when you woke up nearly every morning much earlier than you wanted to. Response options to each sleep problem were binary (0=no; 1=yes). These 4 items were strongly correlated with each other (tetrachoric correlations ranged from 0.51 to 0.75). Daytime sleepiness was defined by the child as “feeling sleepy” during the day.
Covariates
All models adjusted for the following covariates: sex, age (continuous), highest level of parent education (less than high school; high school; some college; college graduate), poverty index ratio, which was derived based on family size and the ratio of family income to the family’s poverty threshold (≤1.5=low income; 1.6–3=low-middle income; <3-≤6= high-middle income; and >6=high income), race/ethnicity (Non-Hispanic White; Non-Hispanic Black; Hispanic; other), region of the country (Northeast, Midwest, South, West), and urbanicity, (Major Metropolitan Area, other urbanized area, rural area).
Analysis
We first conducted basic univariate and bivariate analyses to examine the prevalence of insomnia symptoms and the demographic correlates of both insomnia and exposure to childhood adversity. We then used generalized estimating equations (GEE) to estimate the risk of insomnia by childhood adversity, focusing on exposure to each event and subtype (0=unexposed; 1=exposed). These multivariate analyses yielded prevalence ratios (PR), which are preferred over odds ratios when the outcome is common (e.g., has a prevalence of about 30%) 47–49. To investigate potential differences in the prevalence of insomnia by timing of exposure to childhood adversity, we estimated prevalence ratios corresponding to age at onset of each adversity subtype. We also examined whether accumulation of adverse events (i.e. a count indicating the number of specific types of adversities the child reported being exposed to) was associated with a differential risk for insomnia. Finally, given the known association between mental disorders and sleep problems50,35,36, we conducted sensitivity analyses to examine the association between exposure to childhood adversity and insomnia after excluding adolescents meeting DSM-IV51 criteria for a past-year diagnosis of major depression, dysthymia, post-traumatic stress disorder, or generalized anxiety disorder as assessed by the CIDI. These disorders were included based upon their association to sleep problems in previous literature and our finding that they were highly correlated with insomnia in our sample (0.45, 0.44, 0.44, and 0.39, respectively). These analyses were intended to evaluate whether our results were explained by recent experiences of a psychiatric disorder.
All analyses were conducted using the survey regression procedures available in SAS Version 9.4 to account for the complex survey design. We used sampling weights to account for the differential probability of selection of respondents within households (for the household subsample), differential non-response, and adjust for differences between the sample and the US population on selected socio-demographic characteristics, making this sample nationally representative of the US population on the variables included in this analysis. A false discovery rate (FDR) correction was used to adjust our alpha level for the multiple testing of 23 different childhood adversities.
Results
Insomnia symptoms were common in this sample. Nearly 38% reported daytime sleepiness, while 22% reported taking a long time to fall asleep and 17% reported waking up too early (Table 1). Insomnia was more common among girls compared to boys (57.8% vs. 42.2%; p<0.0001) and among adolescents from racial/ethnic minority groups compared to Whites (Table 2). No differences were observed in the prevalence of insomnia by age, poverty-level, parental education level, or urbanicity (Table 2).
Table 1.
Prevalence of insomnia symptoms and insomnia among adolescents in National Comorbidity Survey Replication Adolescent Supplement (NCS-A) (N = 9582)
| Symptoms (2 weeks or longer in the past year) | Yes | No | Percent (%) |
|---|---|---|---|
| Took a long time to fall asleep | 2,133 | 7,448 | 22.26 |
| Took long time to get back to sleep | 1,288 | 8,294 | 13.44 |
| Woke up too early | 1,615 | 7,966 | 16.86 |
| Daytime sleepiness | 3,601 | 5,981 | 37.58 |
|
| |||
| Insomnia | 2065 | 7,517 | 21.55 |
Insomnia was defined as having at least one of the three primary sleep problems (long time to fall asleep, get back to sleep, or wake too early) with daytime sleepiness for two weeks or longer in the past year. Note: The first and third rows do not sum to 9582 due to one respondent with missing data.
A total of 59.41% of adolescents reported at least one childhood adversity (mean=1.17; standard deviation (SD) =1.43; range=0–11). Adolescents exposed to at least one childhood adversity were more likely to be older, Black and Hispanic, and to reside in families with low socioeconomic status and who lived in metro areas (Table 2).
Adversity exposure and risk of insomnia
Overall, adolescents exposed to childhood adversity were more likely than their non-exposed peers to experience insomnia (Table 3). Those exposed to at least one type of adversity had 1.93 times the risk of insomnia relative to those who were unexposed (PR=1.93; CI=1.68, 2.21). The effects of adversity also appeared to differ by type. Relative to other types of childhood adversity, exposure to interpersonal violence conferred the largest risk for insomnia symptoms. Exposure to rape conferred the largest risk relative to all other adversities (PR=1.90, CI=1.57, 2.30).
Table 3.
Risk of insomnia by exposure to childhood adversity
| Childhood Adversity | Prevalence (%) | Prevalence Ratio (CI) | FDR p-value* |
|---|---|---|---|
| Exposure to any type | 5693 (59.41) | 1.93 (1.68, 2.21)* | 4.20E-19 |
| Interpersonal violence | |||
| Parent violence | 159 (1.66) | 1.51 (1.05, 2.14)* | 3.10E-02 |
| Other violence | 460 (4.80) | 1.63 (1.27, 2.11)* | 2.19E-04 |
| Rape | 250 (2.61) | 1.90 (1.57, 2.30)* | 1.82E-10 |
| Kidnapped | 58 (0.61) | 0.87 (0.51, 1.48) | 6.02E-01 |
| Other sexual assault | 331 (3.45) | 1.89 (1.53, 2.32)* | 5.63E-09 |
| Any of above | 1000 (10.44) | 1.80 (1.52, 2.14)* | 5.19E-11 |
| Accidents and injuries | |||
| Car accident | 741 (7.73) | 1.35 (1.09, 1.67)* | 8.40E-03 |
| Disaster | 1088 (11.35) | 1.31 (1.08, 1.60)* | 8.40E-03 |
| Illness | 606 (6.32) | 1.42 (1.19, 1.69)* | 1.33E-04 |
| Chemical | 236 (2.46) | 1.65 (1.31, 2.07)* | 3.60E-05 |
| Other accident | 731 (7.63) | 1.56 (1.33, 1.83)* | 9.72E-08 |
| Any of above | 2727 (28.46) | 1.59 (1.40, 1.81)* | 2.49E-12 |
| Social network or witness events | |||
| Witness fights at home | 705 (7.36) | 1.53 (1.20, 1.95)* | 7.74E-04 |
| Witness death | 1178 (12.29) | 1.49 (1.30, 1.69)* | 8.08E-09 |
| Other person died unexpectedly | 2841 (29.65) | 1.46 (1.28, 1.67)* | 4.99E-08 |
| Other person unexpected threat | 868 (9.06) | 1.59 (1.40, 1.81)* | 6.84E-12 |
| War terror | 214 (2.23) | 1.11 (0.78, 1.58) | 6.02E-01 |
| Refugee | 45 (0.47) | 0.80 (0.36, 1.77) | 6.02E-01 |
| Any of above | 3735 (38.98) | 1.65 (1.45, 1.87)* | 2.73E-13 |
| Other events | |||
| Other trauma | 268 (2.80) | 1.40 (1.11, 1.75)* | 4.96E-03 |
| Non-disclosed event | 490 (5.11) | 1.83 (1.56, 2.14)* | 5.69E-13 |
| Any of above | 726 (7.58) | 1.67 (1.44, 1.94)* | 7.66E-11 |
Cell entries are the prevalence of each childhood adversity and results of the generalized estimating equations (GEE) models examining the risk of insomnia for each exposure to childhood adversity, after adjusting for covariates. The prevalence column lists the number and in parentheses, the percent. The prevalence ratio column lists the prevalence ratio and in parentheses, the 95% confidence interval. A false discovery rate (FDR) correction was applied to adjust our alpha level for the multiple testing of 19 different exposures (including exposure to any adversity). Statistical significance after imposing the FDR correction is denoted with an asterisk. P-values are expressed in scientific notation (e.g., p=3.05E-02 = p=0.0305).
Timing of exposure to adversity and risk of insomnia
Although adolescents exposed to adversity at any age had a higher risk of insomnia relative to their non-exposed peers, by and large, the risk of insomnia did not differ by age at first exposure to adversity (Table 4). This is shown by the finding that the prevalence ratios (comparing those first exposed in one developmental period to those who were never exposed) were generally not statistically different from one another. That is, the only significant differences we observed were based on timing of first exposure to interpersonal violence. Here, we found that those exposed to adversity in early childhood or adolescence had a significantly greater risk of insomnia relative to those exposed during middle childhood. All other types of adversities showed no significant difference in the prevalence ratio when comparing those exposed for the first time at different ages. Results for each type of adversity are shown in Supplemental Table 1.
Table 4.
Risk of insomnia by timing of exposure to childhood adversity
| Childhood Adversity | Prevalence (%) | Prevalence Ratio (CI) | FDR p-value |
|---|---|---|---|
| Exposure to any type | |||
| Early childhood | 1438 (15.01) | 1.95 (1.59, 2.39)* | 1.36E-09 |
| Middle childhood | 1764 (18.41) | 2.02 (1.77, 2.32)* | 0.00E+00 |
| Adolescence | 2491 (26.00) | 1.86 (1.58, 2.19)* | 1.65E-12 |
| Interpersonal violence † ‡ | |||
| Early childhood | 167 (1.74) | 2.01 (1.55, 2.62)* | 9.16E-07 |
| Middle childhood | 291 (3.04) | 1.38 (0.99, 1.92) | 9.81E-02 |
| Adolescence | 542 (5.66) | 2.00 (1.71, 2.35)* | 0.00E+00 |
| Accidents and injuries | |||
| Early childhood | 784 (8.18) | 1.44 (1.21, 1.71)* | 1.61E-04 |
| Middle childhood | 850 (8.87) | 1.67 (1.43, 1.94)* | 2.91E-10 |
| Adolescence | 1092 (11.40) | 1.65 (1.37, 2.00)* | 8.04E-07 |
| Social network or witness events | |||
| Early childhood | 597 (6.23) | 1.56 (1.20, 2.02)* | 2.20E-03 |
| Middle childhood | 1172 (12.23) | 1.67 (1.37, 2.02)* | 9.16E-07 |
| Adolescence | 2470 (25.78) | 1.67 (1.47, 1.90)* | 7.28E-14 |
| Other events | |||
| Early childhood | 74 (0.77) | 1.57 (1.01, 2.44) | 7.97E-02 |
| Middle childhood | 154 (1.61) | 1.10 (0.73, 1.66) | 7.22E-01 |
| Adolescence | 498 (5.20) | 1.89 (1.59, 2.25)* | 6.52E-12 |
Cell entries are the results of the generalized estimating equations (GEE) models examining the risk of insomnia for each exposure to childhood adversity, after adjusting for covariates. The reference group for each row is adolescents who were unexposed. A false discovery rate (FDR) correction was applied to adjust our alpha level for the multiple testing of 19 different exposures (including exposure to any adversity). Statistical significance after imposing the FDR correction is denoted with an asterisk.
refers to a significant difference (p<0.05) between early versus middle childhood.
refers to a significant difference (p<0.05) between middle childhood and adolescence.
Accumulation of exposure to adversity and risk of insomnia
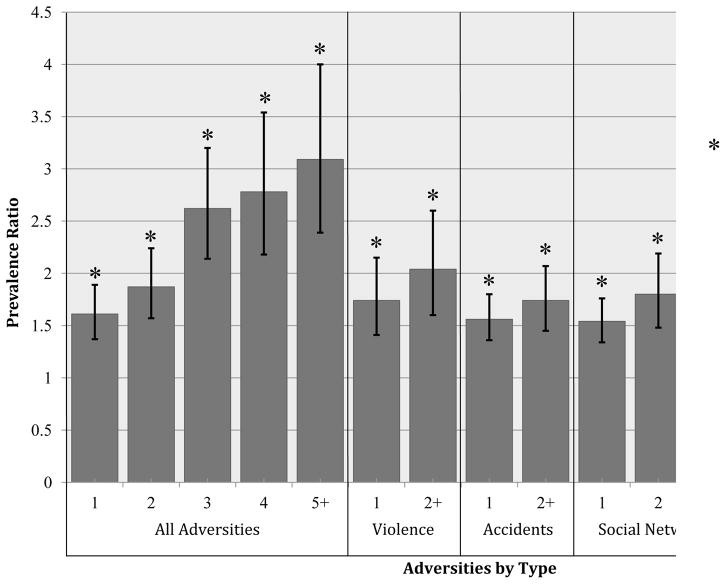
There was a dose-response relationship between the number of specific types of adversities reported by the child and risk for insomnia, such that each additional exposure to a different type of adversity was associated with an elevated risk for insomnia as compared to those unexposed to adversity (Figure 1; Supplemental Table 2). Specifically, youth exposed to 5 or more different types of adversities had more than 3 times the risk of those who were unexposed to experience insomnia (PR=3.09, CI=2.39, 4.00); this risk was more than doubled from those exposed to only one type of adversity (PR=1.61; 1.37, 1.89).
Figure 1. Risk of insomnia by count of the number of exposures to childhood adversity.
This figure presents the results of the generalized estimating equation (GEE) model examining the risk of insomnia based on the count of the number of total adversities experienced as well as count of each subtype, after adjusting for covariates. The reference group refers to adolescents who experienced zero adversities. A false discovery rate (FDR) correction was applied to adjust our alpha level for the multiple testing of 19 different exposures (including exposure to any adversity). Statistical significance after imposing the FDR correction is denoted with an asterisk. Specific p-values for these associations are denoted in Supplemental Table 6.
Sensitivity Analysis
A total of 15% of the sample (n=1430) experienced a major depressive episode (n=829), dysthymia (n=201), PTSD (n=244), or had generalized anxiety disorder (n=156) in the past year. We re-conducted our analyses after excluding these 1430 adolescents from the analytic sample. As shown (Supplemental Tables 3–6), the overall prevalence of insomnia (18.1% versus 21.55%) and exposure to at least one childhood adversity (56.6% versus 59.41%) was similar in the sample excluding these adolescents compared to the larger analytic sample. Overall, the effect estimates for these associations were similar to the results including the adolescents with depression, dysthymia, PTSD, or generalized anxiety disorder, though some coefficients displayed slight increases and decreases in an inconsistent fashion.
Discussion
In this study, we used data from a large, nationally-representative sample of adolescents to examine the relationship between multiple types of childhood adversity and insomnia. In addition to examining whether there was an overall association between exposure to adversity and insomnia, we were also interested in whether there were “sensitive periods” when the effect of exposure to childhood adversity was most pronounced27–29. We also sought to determine whether accumulation of exposure to adversity (meaning the number of types of adversity an adolescent reported) predicted risk for insomnia. This study builds upon previous literature stating the importance of sleep in adolescence and the potential negative mental and physical effects of insomnia14. We aimed to expand previous knowledge about the association between childhood adversity and insomnia by examining multiple different types of adversities, as prior studies have focused on a limited set of exposures. This study also advances the existing literature on childhood adversity and sleep disorders by examining the relationships between multiple childhood adversities and insomnia specifically during adolescence. By using an adolescent sample, we minimized potential bias due to retrospective recall (relative to studies conducted in adults), as most studies examining these associations have used self-reported data.
Three findings emerged from this study. First, we found that youth exposed to adversity were more likely to have insomnia compared to their non-exposed peers. However, the prevalence of insomnia differed as a function of type of adversity. For example, and as with previous studies, those exposed to interpersonal violence (e.g. parent violence or rape) in childhood or adolescence showed the highest risk of sleep disturbance16,20,21. Similar to previous studies on trauma and risk of insomnia18, we also found that those exposed to accidents or injuries in childhood or adolescence were more likely to develop insomnia in adolescence. Additionally, we found a significant association between exposure to “other events” in adolescence and insomnia. We hypothesize that due to the recency of the exposure; there may be a stronger effect of these events on sleep. In addition, “other events” captures all other adversities besides those that were able to be classified; these events may encompass other risk factors, which should be disentangled.
Second, we observed a differential risk for insomnia based on the age at first exposure specifically for interpersonal violence events. Specifically, those exposed to interpersonal violence during early childhood (between 0–5 years of age) or adolescence (between 11–18 years of age) had a larger risk of insomnia relative to respondents who were never exposed and more specifically relative to those who were exposed during middle childhood. To our knowledge, this was the first study to examine developmental timing differences in the effect of adversity on sleep.
Third, there was a clear dose-response relationship between exposure to multiple types of adversity and risk for insomnia. This finding parallels previous population-based studies, which also have found exposure to a greater number of childhood adversities conferred a larger risk for insomnia in adults24,26.
Our finding that there were differences based on the type, timing, and accumulation of exposure – in both the larger sample and the smaller sample of adolescents without a history of past-year psychiatric disorders – underscore the need for future studies to consider specific features of childhood adversity exposure beyond simply characterizing individuals as “exposed” or “non-exposed.” Additionally, although the focus of the current study was on the long-term effects of adversity on sleep, future studies should more closely examine the immediate effects of adversity on sleep.
Converging lines of research on trauma, stress and sleep neurobiology and psychophysiology provide insight on possible mechanisms that underlie associations between childhood adversities and risk of insomnia in adolescence52. Substantial evidence shows that exposure to trauma evokes an intense stress/fear response that initiates hyperarousal in specific brain areas (e.g., amygdala, prefrontal cortex, reticular activating system) 52,53. In turn, this hyperarousal leads to exaggerated reactivity of the hypothalamic-pituitary adrenal axis and the sympathetic nervous system, which manifests in a generalized state of physiological and neurobiological hyperarousal that impedes sleep onset and continuity, and may ultimately contribute to chronic insomnia52,54,55.
Findings from this study must be evaluated in light of several limitations. First, adolescents retrospectively reported whether, and if so when, they were exposed to each adversity and whether they experienced insomnia symptoms. As a result of memory lapses or an unwillingness to disclose private matters, such retrospective reports may lead to over- or under-reporting. However, recent studies have found retrospective and prospective measures of child maltreatment, in particular, produce similar estimates of effect for health-related problems56. Second, this was a cross-sectional analysis, where exposure and outcome data were captured at the same time. Although a limitation, we maintained a prospective association between childhood adversity and insomnia symptoms, as youth retrospectively recalled their age at first onset to adversity and we focused on sleep problems measured in the past year. However, to replicate these findings, true prospective studies of adolescents will be needed; ideally, these studies should include measures of earlier sleep problems, which can aid in identifying sleep problems that are subsequent to (rather than prior to) adversity exposure. Third, we did not examine other indicators commonly included in studies of childhood adversity, such as parental mental illness, parental incarceration, and exposure to child neglect, or poverty. These constructs were either unmeasured in the current dataset or were measured without regard to developmental timing of exposure. For example, poverty was collected at only one specific time period and did not include information about timing of exposure to poverty. Studies examining the effects of multiple indicators of adversity on insomnia will be important for disentangling the role of specific types of adversity on sleep. Fourth, our study does not accurately test the biological mechanism(s) behind the association between insomnia and adversity; therefore we are only able to hypothesize a possible mechanism of how trauma may affect insomnia in adolescence. Lastly, there is a large amount of literature that defines insomnia in adulthood; however, the definition of insomnia in adolescence is less clear. There is both the ICSD-II46 definition and the DSM-IV46 definition of insomnia. Comparing the results of this study with those using a DSM-IV definition would be of interest. Finally, due to the small cell sizes we were unable to examine the joint effect of timing and the number of adverse exposures. Studies examining these effects will further elucidate the way in which adverse events affect sleep.
Conclusion
Results of this analysis suggest that exposure to adversity confers an elevated risk for insomnia during adolescence. This association varied by primarily by type and accumulation of exposure and to some extent, by timing of exposure. Given the well-documented physical and mental health consequences of insomnia, such findings add further support to the need for practitioners to screen children for exposure to both childhood adversity and insomnia symptoms. Based on our findings, screening efforts should focus on not just whether the child was exposed to an adverse event, but also when in the course of development the adversity first occurred (especially for interpersonal violence events) and how many total adversities the child experienced. By querying these domains, physicians may be able to better treat and possibly prevent insomnia symptoms and ultimately reduce the long-term health ailments associated with insomnia.
Supplementary Material
Highlights.
Three significant findings emerge from this study.
We found that youth exposed to adversity are more likely to have insomnia during adolescence and the prevalence of insomnia differs by type of adversity.
For certain types of adversities, the risk for insomnia differed based on age at first exposure. This finding is consistent with the notion of “sensitive periods” in development.
There was a clear dose-response relationship between number of childhood adversities reported and risk for insomnia.
Acknowledgments
The authors thank Jenna Kiely for her assistance in preparing this manuscript for publication.
Funding Source: Research reported in this publication was supported, in part, by the National Institute of Mental Health (NIMH) under award number (K01 MH102403 Dunn) and the Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD) under award number (R01 HD073352 Hale). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial Disclosure: All authors list no financial relationships relevant to this article to disclose.
Conflict of Interest: All authors list no conflicts of interest.
Abbreviations: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff (Millwood) 2014;33:2106–15. doi: 10.1377/hlthaff.2014.0914. [DOI] [PubMed] [Google Scholar]
- 2.Friedman EM, Montez JK, Sheehan CM, Guenewald TL, Seeman TE. Childhood Adversities and Adult Cardiometabolic Health: Does the Quantity, Timing, and Type of Adversity Matter? J Aging Health. 2015 doi: 10.1177/0898264315580122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shonkoff JP, Garner AS, et al. Committee on Psychosocial Aspects of C. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129:e232–46. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 4.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication II: Associations with persistence of DSM-IV disorders. Archives of General Psychiatry. 2010;67:124–32. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. JAMA Psychiatry. 2012;69:1151–60. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korkeila J, Vahtera J, Nabi H, et al. Childhood adversities, adulthood life events and depression. J Affect Disord. 2010;127:130–8. doi: 10.1016/j.jad.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 7.Nusslock R, Miller GE. Early-Life Adversity and Physical and Emotional Health Across the Lifespan: A Neuroimmune Network Hypothesis. Biol Psychiatry. 2015 doi: 10.1016/j.biopsych.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–97. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of chilhood abuse and household dysfunction in many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 10.Goodwin RD, Stein MB. Association between childhood trauma and physical disorders among adults in the United States. Psychol Med. 2004;34:509–20. doi: 10.1017/s003329170300134x. [DOI] [PubMed] [Google Scholar]
- 11.Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, Liao D, Bixler EO. Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med. 2014;15:91–5. doi: 10.1016/j.sleep.2013.08.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fricke-Oerkermann L, Pluck J, Schredl M, et al. Prevalence and course of sleep problems in childhood. Sleep. 2007;30:1371–7. doi: 10.1093/sleep/30.10.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Li AM, Kong AP, Lai KY, Tang NL, Wing YK. A community-based study of insomnia in Hong Kong Chinese children: Prevalence, risk factors and familial aggregation. Sleep Med. 2009;10:1040–6. doi: 10.1016/j.sleep.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3:S7–10. [PMC free article] [PubMed] [Google Scholar]
- 15.Mindell JA, Moline ML, Zendell SM, Brown LW, Fry JM. Pediatricians and sleep disorders: training and practice. Pediatrics. 1994;94:194–200. [PubMed] [Google Scholar]
- 16.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2006;31:469–80. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 17.Poon CY, Knight BG. Impact of childhood parental abuse and neglect on sleep problems in old age. J Gerontol B Psychol Sci Soc Sci. 2011;66:307–10. doi: 10.1093/geronb/gbr003. [DOI] [PubMed] [Google Scholar]
- 18.Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001;345:1825–32. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- 19.Chapman DP, Liu Y, Presley-Cantrell LR, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC Public Health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired sleep maintenance in abused children. J Am Acad Child Adolesc Psychiatry. 1997;36:1236–43. doi: 10.1097/00004583-199709000-00016. [DOI] [PubMed] [Google Scholar]
- 21.Sadeh A. Stress, Trauma, and Sleep in Children. Child Adolesc Psychiatr Clin N Am. 1996;5:685–700. [Google Scholar]
- 22.Bader K, Schafer V, Nissen L, Schenkel M. Heightened beta EEG activity during nonrapid eye movement sleep in primary insomnia patients with reports of childhood maltreatment. J Clin Neurophysiol. 2013;30:188–98. doi: 10.1097/WNP.0b013e3182767c4a. [DOI] [PubMed] [Google Scholar]
- 23.Bader K, Schafer V, Schenkel M, Nissen L, Kuhl HC, Schwander J. Increased nocturnal activity associated with adverse childhood experiences in patients with primary insomnia. J Nerv Ment Dis. 2007;195:588–95. doi: 10.1097/NMD.0b013e318093ed00. [DOI] [PubMed] [Google Scholar]
- 24.Chapman DP, Wheaton AG, Anda RF, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12:773–9. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Slopen N, Shonkoff JP, Albert MA, et al. Racial Disparities in Adverse Child and Family Experiences in the United States: Interactions with Family Immigration History and Income. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 26.Koskenvuo K, Hublin C, Partinen M, Paunio T, Koskenvuo M. Childhood adversities and quality of sleep in adulthood: A population-based study of 26,000 Finns. Sleep Med. 2010;11:17–22. doi: 10.1016/j.sleep.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Knudsen E. Sensitive periods in the development of the brain and behavior. Journal of Cognitive Neuroscience. 2004;16:1412–25. doi: 10.1162/0898929042304796. [DOI] [PubMed] [Google Scholar]
- 28.Bornstein MH. Sensitive periods in development: Structural characteristics and causal interpretations. Psychological Bulletin. 1989;105:179–97. doi: 10.1037/0033-2909.105.2.179. [DOI] [PubMed] [Google Scholar]
- 29.Kuh D, Ben-Shlomo Y, editors. A life course approach to chronic disease epidemiology. 2. Oxford: Oxford University Press; 2004. [PubMed] [Google Scholar]
- 30.Dunn EC, McLaughlin KA, Slopen N, Rosand J, Smoller JW. Developmental timing of child maltreatment and symptoms of depression and suicidality in young adulthood: Results from the National Longitudinal Study of Adolescent Health. Depression and Anxiety. 2013;30:955–64. doi: 10.1002/da.22102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities. Journal of the American Medical Association. 2009;301:2252–9. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 32.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9(Suppl 1):S3–9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 33.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40:700–8. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 34.Archibald HC, Long DM, Miller C, Tuddenham RD. Gross stress reaction in combat--a 15 year follow-up. Am J Psychiatry. 1962;119:317–22. doi: 10.1176/ajp.119.4.317. [DOI] [PubMed] [Google Scholar]
- 35.Taylor DJ. Insomnia and depression. Sleep. 2008;31:447–8. doi: 10.1093/sleep/31.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arriaga F, Paiva T. Clinical and EEG sleep changes in primary dysthymia and generalized anxiety: a comparison with normal controls. Neuropsychobiology. 1990;24:109–14. doi: 10.1159/000119471. [DOI] [PubMed] [Google Scholar]
- 37.Kessler RC, Avenevoli S, Costello EJ, et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:380–5. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kessler RC, Merikangas KR. The national comorbidity survey replication (NCS-R): background and aims. International Journal of Methods in Psychiatric Research. 2004;13:60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA pediatrics. 2013;167:70–5. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- 40.McLaughlin KA, Green JG, Alegria M, et al. Food insecurity and mental disorders in a national sample of U.S. adolescents. J Am Acad Child Adolesc Psychiatry. 2012;51:1293–303. doi: 10.1016/j.jaac.2012.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 42.Kaplow JB, Widom CS. Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology. 2007;116:176–87. doi: 10.1037/0021-843X.116.1.176. [DOI] [PubMed] [Google Scholar]
- 43.Andersen SL, Tomada A, Vincow ES, Valente E, Polcari A, Teicher MH. Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. Journal of Neuropsychiatry and Clinical Neurosciences. 2008;20:292–301. doi: 10.1176/appi.neuropsych.20.3.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walsh JK, Coulouvrat C, Hajak G, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS) Sleep. 2011;34:997–1011. doi: 10.5665/SLEEP.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- 46.Dohnt H, Gradisar M, Short MA. Insomnia and its symptoms in adolescents: comparing DSM-IV and ICSD-II diagnostic criteria. J Clin Sleep Med. 2012;8:295–9. doi: 10.5664/jcsm.1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- 48.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–5. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 49.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC medical research methodology. 2003;3:21. doi: 10.1186/1471-2288-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shanahan L, Copeland WE, Angold A, Bondy CL, Costello EJ. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014;53:550–8. doi: 10.1016/j.jaac.2013.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Arlington, VA: American Psychiatric Publishing; 2000. [Google Scholar]
- 52.Sinha SS. Trauma-induced insomnia: A novel model for trauma and sleep research. Sleep Med Rev. 2015 doi: 10.1016/j.smrv.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 53.Williams LM, Kemp AH, Felmingham K, et al. Trauma modulates amygdala and medial prefrontal responses to consciously attended fear. NeuroImage. 2006;29:347–57. doi: 10.1016/j.neuroimage.2005.03.047. [DOI] [PubMed] [Google Scholar]
- 54.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 55.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14:9–15. doi: 10.1016/j.smrv.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 56.Scott KM, McLaughlin KA, Smith DAR, Ellis PM. Childhood maltreatment and DSM-IV adult mental disorders: Comparison of prospective and retrospective findings. British Journal of Psychiatry. 2012;200:469–75. doi: 10.1192/bjp.bp.111.103267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.