ABSTRACT
A physician's recommendation for human papillomavirus (HPV) vaccine is a key predictor of vaccine uptake; however, little is known about how physicians communicate about HPV vaccine with male patients. We sought to describe physicians' HPV vaccine communication practices with males who are of vaccine-eligible age (9-26 years). We surveyed representative samples of pediatric and family medicine physicians in Florida, and assessed whether physicians present HPV vaccine as optional or routine, and as a vaccine that prevents cancer. We also assessed the type of visit during which physicians discuss HPV vaccine with adolescent males and whether other healthcare providers in the practice discuss HPV vaccine or make the initial recommendation. We received 367 completed surveys (50.7% response rate). Few physicians (29.9%) reported they typically present HPV vaccine as routine to males ages 11-12 years, who constitute the target group for routine vaccination. When discussing HPV vaccination, many physicians reported somewhat or strongly emphasizing cancer prevention (80.0%). Physicians most often discussed HPV vaccine when they saw patients for well-child visits (93.0%) and least often at acute care visits (15.3%). Over half reported that at least one other healthcare professional in their practice discusses (56.1%) or makes the initial recommendation for (54.9%) HPV vaccination. Many physicians in our sample are presenting HPV vaccine as optional rather than routine and are missing opportunities to communicate with males about the vaccine. Our findings identify areas for future interventions to improve physicians' HPV vaccine communication and, ultimately, increase the use of this cancer-preventing vaccine.
KEYWORDS: Florida, health communication, human papillomavirus vaccines, males, physicians, primary care, survey methods
Introduction
In 2011, the Advisory Committee on Immunization Practices (ACIP) recommended routine vaccination with quadrivalent human papillomavirus (HPV) vaccine for males ages 11-12 years in the United States (US).1 ACIP also recommends catch-up vaccination for unvaccinated or partially vaccinated males ages 13-21 years and vaccination up to age 26 for special populations, including immunocompromised males and men who have sex with men. Despite these recommendations, HPV vaccine coverage is low. In 2014, about 42% of males ages 13-17 in the US had received ≥1 dose of the three-dose vaccine series, and only 22% had completed the series.2 Coverage in Florida is similarly low, which is concerning given that Florida is among the most populated US states, and has among the highest rates of HPV-associated anal cancer in males.3 Underuse of HPV vaccines leaves males vulnerable to unnecessary and life-threatening HPV-attributable anogenital cancers.4
Many vaccine-eligible adolescents do not receive HPV vaccines during visits with healthcare providers during which another vaccine was administered.5 If these missed opportunities for HPV vaccination were eliminated, coverage with ≥1 dose of HPV vaccine could be as high as 91.3% by age 13 for girls born in the year 2000.5 Some research suggests there are similar missed opportunities to vaccinate boys against HPV during preventive care visits.6 To minimize these missed opportunities, it is critical that providers take advantage of every healthcare encounter to assess HPV vaccination status7 and recommend vaccination.
Leaders in public health and medical communities provide suggestions regarding the content and context of HPV vaccine recommendation.4,8 With respect to content, the President's Cancel Panel recommends that physicians frame HPV vaccine as a cancer-preventing vaccine, emphasize vaccine safety and efficacy, and underscore the importance of vaccinating at age 11 or 12 years.4 With respect to context, it is clear that opportunities for vaccination extend beyond routine preventive care visits7,8 and recommendations can be either supported or delivered by other healthcare team members (e.g., nurses, medical assistants) to introduce, recommend, and/or reinforce HPV vaccination to patients and parents.9,10
Research conducted on the content and context of physician communication about HPV vaccine mostly has examined these components with female patients only,11,12 without distinguishing patient sex,13,14 or prior to vaccine licensure for males.15,16 We are aware of only two previous studies conducted with physicians that examined content of their communication with males after vaccine licensure.17,18 Given that HPV vaccine coverage for males lags behind females and for other adolescent immunizations,2 understanding these aspects of vaccine communication, particularly in a state with low HPV vaccine uptake,2 is essential for supporting physicians' HPV vaccine recommendations for males. To address this need, we assessed the content and context of HPV vaccine communication with male patients and their parents among a statewide sample of pediatricians and family medicine physicians in Florida.
Results
We randomly selected 770 pediatric and family medicine physicians based on their proportional representation in the Florida physician primary care workforce. After receiving institutional review board approval, we began a six-wave mailing approach beginning with pre-notice postcards mailed in May 2014 and ending with a final reminder to non-responders in August 2014. We received 367 completed surveys; after accounting for undeliverable surveys (n = 36) and ineligible respondents (n = 10), the overall response rate was 50.7%. For our current analyses, we excluded 12 participants who reported they did not see male patients ages 9-26, for an analytic sample size of 355.
Sample characteristics
The sample was about equally comprised of female (50.1%) and male (48.2%) physicians (Table 1). Participants' average age was 48.7 years (standard deviation [SD] = 9.0), about 65.6% were White and 73.0% were non-Hispanic. Half (49.0%) specialized in family medicine and 49.9% had been practicing for 16 or more years.
Table 1.
Demographic and practice characteristics of physicians who participated in the survey (N = 355).
|
Physician characteristics |
n (%) |
|---|---|
| Gender | |
| Female | 178 (50.1) |
| Male | 171 (48.2) |
| Missing | 6 (1.7) |
| Age | |
| 30-39 | 64 (18.0) |
| 40-49 | 124 (34.9) |
| ≥50 | 161 (45.4) |
| Missing | 6 (1.7) |
| Race | |
| White/Caucasian | 233 (65.6) |
| Black/African-American | 22 (6.2) |
| Asian | 38 (10.7) |
| Other | 51 (14.4) |
| Missing | 11 (3.1) |
| Ethnicity | |
| Hispanic | 86 (24.2) |
| Non-Hispanic | 259 (73.0) |
| Missing | 10 (2.8) |
| Years practicing | |
| ≤10 | 100 (28.2) |
| 11-15 | 64 (18.0) |
| ≥16 | 177 (49.9) |
| Missing | 14 (3.9) |
| Clinical specialty | |
| Pediatrics | 155 (43.7) |
| Family Medicine | 174 (49.0) |
| Othera | 20 (5.6) |
| Missing | 6 (1.7) |
| Practice characteristics | |
| Number of physicians | |
| 1 | 100 (28.2) |
| 2 | 174 (49.0) |
| 6-15 | 46 (13.0) |
| ≥16 | 29 (8.2) |
| Missing | 6 (1.7) |
| Practice situation | |
| Single specialty | 233 (65.6) |
| Multi-specialty | 91 (25.6) |
| Other | 25 (7.0) |
| Missing | 6 (1.7) |
| Practice type | |
| Private practice office | 229 (64.5) |
| Other | 112 (31.5) |
| Missing | 14 (3.9) |
| Practice location | |
| Urban | 129 (36.3) |
| Suburban | 180 (50.7) |
| Rural/Other | 33 (9.3) |
| Missing | 13 (3.7) |
| Race of patients | |
| White, non-Hispanic | 143 (40.3) |
| Minority group(s) | 121 (34.1) |
| No definable majority | 67 (18.9) |
| Missing | 24 (6.8) |
| Medicaid patients | |
| Medicaid only | 6 (1.7) |
| Medicaid and others | 215 (60.6) |
| No Medicaid | 97 (27.3) |
| Missing | 37 (10.4) |
| Typical daily patient volume | |
| <15 | 41 (11.5) |
| 15-19 | 96 (27.0) |
| 20-29 | 155 (43.7) |
| ≥30 | 56 (15.8) |
| Missing | 7 (2.0) |
| VFC provider | |
| Yes | 162 (45.6) |
| No | 156 (43.9) |
| Do not know | 35 (9.9) |
| Missing | 2 (0.6) |
Notes. Abbreviation: VFC, Vaccines for Children program
Other clinical specialty includes Urgent Care, Acute Care, Internal Medicine, Hospice, Geriatrics, General Physician, Primary Care, Emergency Room.
Regarding practice characteristics, the highest proportion (49.0%) of physicians reported their practice had two physicians. About two-thirds (65.6%) described their practice as single specialty, 64.5% worked in private practice, and 50.7% reported their practice was in a suburban location. Fewer than half (40.3%) reported seeing mostly White, non-Hispanic patients, and about 60.6% saw patients who used either Medicaid or another form of payment. Nearly half (45.6%) of surveyed physicians were a Vaccines for Children (VFC) provider.
The anonymous nature of the survey precludes examining the degree to which survey responders and non-responders were similar on demographic and practice characteristics. However, we were able to compare responding physicians to the population of physicians in Florida meeting our study eligibility criteria on characteristics including age, sex, and clinical specialty. We found no statistically significant difference in age for responding physicians (M = 48.7, SD = 9.0) compared to the larger population of Florida physicians (M = 48.8, SD = 10.0), t(410.67) = 0.28, p = .78. A similar proportion of females responded to our survey (51.3%) compared to the population of Florida physicians (46.7%), χ2(1, N = 6,907) = 2.82, p = .09. Survey responders were similar to Florida physicians regarding pediatric specialty (43.3% responders vs. 37.2% in Florida) and family medicine specialty (50.3% responders vs. 56.8% in Florida), χ2(2, N = 6,915) = 6.10, p = .05.
Content of HPV vaccine communication
Optional versus routine HPV vaccination
Physicians reported presenting HPV vaccination as routine most often (35.3%) to males ages 13-17, followed by males ages 18-21 (30.9%) (Fig. 1). Few physicians presented HPV vaccine as routine to males in the early vaccination group (ages 9-10; 9.1%) and for males in the age group for whom HPV vaccine is recommended only for special populations (ages 22-26; 22.8%). Less than one-third (29.9%) reported they typically present HPV vaccine as routine for 11-12 year old males; an additional 20.9% reported they do not discuss HPV vaccine with this age group. For all age groups, more physicians reported they presented HPV vaccine as an optional, rather than routine, vaccine.
Figure 1.
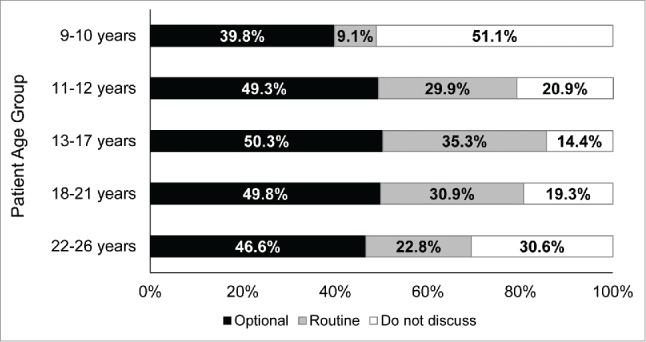
Physicians' presentation of HPV vaccine as optional or routine for males, by patient age group. Note. The number of patients seen differs by patient age group: 9–10 years, n = 264; 11–12 years, n = 278; 13–17 years, n = 292; 18–21 years, n = 301; 22–26 years, n = 206.
HPV vaccine relative to other adolescent immunizations
Among physicians who did not indicate they do not see 11- to 12-year-old males, more than half (57.3%) recommended HPV vaccine less strongly and 41.2% recommended HPV vaccine as strongly as tetanus, diphtheria, and pertussis (Tdap) vaccine (data not shown). Relative to meningococcal vaccine, about half (50.9%) recommended HPV vaccine less strongly, whereas 46.2% recommended HPV vaccine as strongly. Few physicians recommended HPV vaccine more strongly than Tdap (1.5%) and meningococcal vaccine (2.9%).
Emphasis during discussion
When discussing HPV vaccination with male patients and their parents, many physicians reported somewhat or strongly emphasizing cancer prevention (80.0%), sexually transmitted infection (STI) prevention (77.8%), the importance of vaccinating prior to the onset of sexual activity (77.2%), vaccine safety (68.5%), and vaccine efficacy (64.5%) (Table 2). Over half (57.8%) somewhat or strongly emphasized all five aspects in their discussions, whereas 13.8% did not emphasize any of the aspects (data not shown). About three-quarters (76.1%) stressed both STI and cancer prevention in their discussions, whereas few emphasized STI (1.4%) or cancer (3.9%) prevention without emphasizing the other. Physicians who somewhat or strongly emphasized cancer prevention tended to emphasize cervical cancer prevention in female sexual partners (76.9%); fewer emphasized prevention of anal cancer (49.8%) and possible prevention of penile cancer (56.0%) in the patient himself (Table 2).
Table 2.
Content of physicians' discussion about HPV vaccine with male patients and their parents.
| |
Strongly emphasize |
Somewhat emphasize |
Discuss only if questioned |
Do not discuss |
Don't know/not sure |
|---|---|---|---|---|---|
| Content area | n (%) | n (%) | n (%) | n (%) | n (%) |
| Sexually transmitted infection prevention | |||||
| Prevention of genital warts in the patient himself | 194 (54.6) | 76 (21.4) | 40 (11.3) | 31 (8.7) | 4 (1.1) |
| Prevention of genital warts in sexual partners | 146 (41.1) | 95 (26.8) | 64 (18.0) | 37 (10.4) | 2 (0.6) |
| Cancer prevention | |||||
| Prevention of cervical cancer in female sexual partners | 201 (56.6) | 72 (20.3) | 37 (10.4) | 32 (9.0) | 2 (0.6) |
| Prevention of anal cancer in the patient himself | 114 (32.1) | 63 (17.7) | 80 (22.5) | 85 (23.9) | 4 (1.1) |
| Possible prevention of penile cancer | 113 (31.8) | 86 (24.2) | 56 (15.8) | 85 (23.9) | 3 (0.8) |
| Safety of the vaccine in males | 158 (44.5) | 85 (23.9) | 66 (18.6) | 31 (8.7) | 5 (1.4) |
| Efficacy of the vaccine in males | 141 (39.7) | 88 (24.8) | 73 (20.6) | 31 (8.7) | 9 (2.5) |
| Importance of vaccination prior to the onset of sexual activity (for patients who have not initiated sexual activity) | 215 (60.6) | 59 (16.6) | 35 (9.9) | 33 (9.3) | 4 (1.1) |
Note. Percentages account for missing data. Missing data for each item ranged from 9 to 13 participants.
We further explored whether physicians strongly emphasized cancer and STI prevention in their discussions. Regarding cancer prevention generally, 22.5% of physicians strongly emphasized prevention of cervical cancer in female sexual partners, prevention of anal cancer in the patient himself, and possible prevention of penile cancer (data not shown). For STI prevention, 39.2% of physicians strongly emphasized prevention of genital warts in both the patient himself and in sexual partners. For the patient himself, about one-third of physicians strongly emphasized prevention of anal (32.1%) or penile (31.8%) cancer and just over half (54.6%) strongly emphasized prevention of genital warts (Table 2).
Context of HPV vaccine communication
Opportunities for communication
Similar numbers of physicians conveyed that they saw adolescent males who presented for school or college physicals (70.1%), acute care visits (68.2%), well-child visits (68.2%), and sports physicals (66.2%); fewer saw male patients for camp physicals (53.2%) and when the patient is in for other vaccines (42.5%) (Fig. 2). Among those who saw male patients for a particular type of visit, physicians most often also discussed HPV vaccine at well-child visits (93.0%), followed by when the patient is in for other vaccines (82.1%), school or college physicals (81.1%), sports physicals (56.2%), camp physicals (54.5%), and acute care visits (15.3%) (data not shown).
Figure 2.
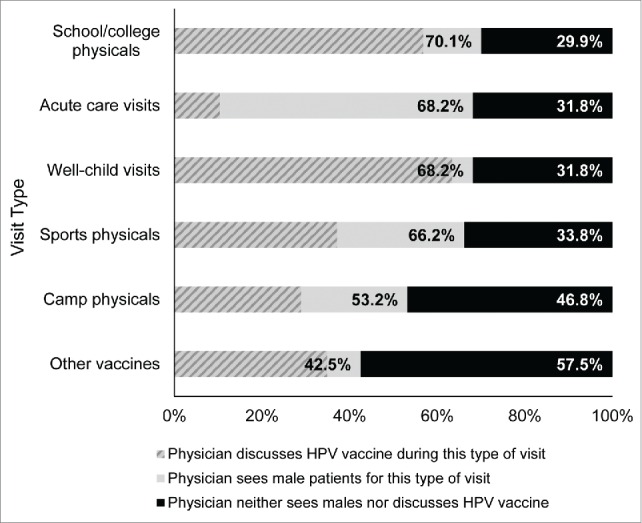
Types of visits at which physicians see male patients and discuss HPV vaccine. Note. 15 participants did not respond to the question regarding the type of visit where adolescent males are seen. Percentages account for these missing data.
Other healthcare professionals
Regarding other healthcare professionals' involvement in HPV vaccine discussion and recommendation, over half of physicians indicated that at least one other healthcare professional in their practice discusses (56.1%) or makes the initial recommendation for (54.9%) HPV vaccination. Physicians most often reported that a nurse practitioner (30.7%) in their practice discusses HPV vaccination with patients, followed by a medical assistant (24.2%), physician assistant (15.8%), and nurse (14.9%). Similar percentages of physicians reported that these healthcare professionals make the initial recommendation for HPV vaccination: nurse practitioner (29.9%), medical assistant (25.1%), physician assistant (16.6%), and nurse (16.6%).
Discussion
This study describes the content and context of physicians' communication about HPV vaccine with male patients and their parents. We found that many primary care physicians in our sample reported HPV vaccine communication practices that are inconsistent with national guidelines1 and evidence-based recommendations.4,8 The Centers for Disease Control and Prevention suggests that physicians recommend HPV vaccine the same way as other adolescent vaccines by stating that the child needs shots and then listing the ACIP-recommended vaccines for his or her age.19 Although ACIP recommends routine vaccination for males ages 11-12,1 only 29.9% present HPV vaccine as a routine at this age, which is a likely contributor to low vaccination rates. Although a higher proportion of physicians reported presenting HPV vaccine as routine for older ages, far fewer older adolescents present for preventive care.20 Consequently, a large proportion of these patients may never receive a routine recommendation, even if it is the physicians' intent to recommend more strongly at an older age.
In our study, over half of physicians reported recommending HPV vaccine less strongly than Tdap and meningococcal vaccines. Our findings echo other research conducted with a national sample of pediatricians and family physicians.14 This research found significantly higher proportions of physicians endorse Tdap (95%) and meningococcal (87%) vaccines compared to HPV vaccine (73%). Moreover, physicians in that study reported that they perceived parents' endorsement of Tdap (74%) and meningococcal (62%) vaccines as much higher than for HPV vaccine (13%). Thus, physicians may recommend Tdap and meningococcal vaccines more strongly than HPV vaccine because of their perceived support, and lower resistance, from parents. Physicians also may be more inclined to recommend Tdap and meningococcal vaccines more strongly than HPV vaccine because meningococcal meningitis, diphtheria, and pertussis are easily transmitted through casual contact,21-23 whereas HPV is transmitted sexually.
Although not transmitted through casual contact, HPV infection is common and persistent infection can lead to cancer;24 as such, evidence-based approaches to vaccine communication suggest emphasizing that HPV vaccine prevents cancer.4 In our study, about 80% of physicians somewhat or strongly emphasized some aspect of the vaccine's cancer prevention benefits, but far fewer (22.5%) strongly emphasized cancer prevention for multiple cancers. Moreover, more physicians highlighted HPV vaccine's cancer prevention benefits for female sexual partners than for the male patient himself, with only about one-third of physicians reporting they strongly emphasize that HPV vaccine can prevent anal cancer and possibly prevent penile cancer. This behavior may reflect a limited understanding of HPV-related disease in and the vaccine's cancer prevention benefits for males.25 Alternatively, one study found that physicians may be aware of these benefits, but are uncomfortable discussing anal and penile cancers with male patients and their parents.17 Some physicians in the study who acknowledged the cancer prevention benefits for males perceived this benefit as unimportant because of the low incidence of these cancers and, as a result, do not discuss these cancers when offering HPV vaccine to males. In our study, more physicians emphasized prevention of genital warts than cancer as a direct benefit of vaccination. What remains unclear is which message physicians used to lead their communication and the depth to which they discuss these messages, and whether these are important factors in parents' subsequent agreement to vaccinate their child. Also, it is important to recognize that potential variation in physicians' interpretation of what it means to somewhat or strongly emphasize cancer or STI prevention limits our understanding of gradations in these discussions. At the same time, available recommendations for vaccine communication advise physicians in rather general terms, such as framing HPV vaccine as a vaccine that prevents cancer.4 Additional evidence is needed on what constitutes a strong emphasis to support best clinical practices and establish a benchmark for measuring those practices.
Nearly all physicians took advantage of well-child visits to discuss HPV vaccine, but are missing other opportunities to communicate with males about the vaccine, particularly sick visits. This finding is consistent with previous research indicating that fewer than half of physicians discuss adolescent vaccines at sick visits; however, when they do, physicians more often discuss Tdap and meningococcal vaccine than HPV vaccine.14 Physicians who reported not discussing adolescent vaccines during sick visits most often cited that vaccination is better suited for a well visit. Physicians' disinclination to discuss HPV vaccine outside of well-child visits is particularly worrisome because boys' compliance with well-child visit recommendations declines after age 1226 and teenage boys usually visit a healthcare provider as a result of acute illness or injury.27 Thus, not taking advantage of every clinical encounter to discuss HPV vaccine perpetuates the current problem of missing opportunities for vaccination and undermining HPV-related cancer prevention efforts.
Over half of physicians in our study indicated that other healthcare providers in their practice setting discuss and recommend HPV vaccine. Given documented barriers related to physicians' time to discuss HPV vaccination,28,29 non-physician healthcare providers can be instrumental in facilitating vaccine uptake. These professionals may have more frequent and extended contact with patients,30 allowing greater opportunity to discuss and recommend HPV vaccination. We are aware of few studies that have targeted this group directly as a means to reduce missed clinical opportunities for HPV vaccination. One intervention study found that a structured presentation was effective in increasing physicians' and non-physician healthcare workers' knowledge about HPV vaccine.31 Although these results are promising, we recognize that changes in knowledge do not necessarily translate to changes in clinical practice behaviors. Additional research is needed on non-physician healthcare providers' role in and needs for effectively communicating about HPV vaccination.
To our knowledge, our study is among the first to focus on both the content and context of physicians' HPV vaccine communication specifically with male adolescent patients and their parents. Study strengths include a statewide sample of primary care providers in Florida and an examination of multiple components of physicians' communication.
Although assessing physicians' perspectives is a study strength, the self-reported survey data we collected also are a limitation given that physicians may have reported socially desirable behaviors or their responses may have been subject to recall bias. Second, our survey response rate was 50.7%; thus, our findings may be subject to nonresponse bias, thereby limiting the generalizability of our results. Third, the cross-sectional study design precludes our ability to examine whether physician communication about HPV vaccine results in subsequent vaccine uptake. Fourth, the survey design did not allow us to differentiate communication content and context based on the adolescent's age. Because some research shows that physicians' communication is influenced by patient age,17 future research should further examine this relationship. Also, the survey did not assess physicians' discussion of oropharyngeal cancer prevention. Although HPV vaccine is not indicated for prevention of oropharyngeal cancers,32 about 72% of oropharyngeal cancers are probably caused by HPV.33 Thus, some physicians may emphasize possible prevention of oropharyngeal cancers in their discussions. Finally, our survey did not include quantitative anchors to help standardize the distinction between strongly emphasize and somewhat emphasize responses; thus, physicians' interpretation of these response options may vary.
Taken together, our findings identify areas for future interventions to improve physicians' HPV vaccine communication and, ultimately, increase the use of this cancer-preventing vaccine. These areas include helping physicians present HPV vaccine as a routine part of the adolescent vaccination platform at ages 11-12 when males are still presenting routinely for well-child care, and as a vaccine that prevents cancer; to take advantage of all clinical encounters, particularly acute visits; and to maximize the use of support offered by non-physician healthcare professionals in communicating about HPV vaccination with patients. Without such interventions to support physicians' communication, HPV vaccine may remain underused by males, leaving them susceptible to unnecessary and preventable cancers.
Methods
Recruitment
We obtained a full mailing list of Florida-based pediatricians and family medicine physicians from an American Medical Association (AMA) Physician Masterfile licensee. Exclusion criteria were: 1) trainee status (i.e., residents and fellows), 2) locum tenens, 3) non-patient care reported as their major professional activity, 4) age 65 years or older, given that the AMA Masterfile has shown a significant lag in posting physician retirements,34 and 5) post office box listed as an address, which would preclude our ability to reach physicians using our FedEx mailing strategy. We randomly selected physicians from pediatric and family medicine specialties based on their proportional representation in the Florida physician primary care workforce (n = 770). After receiving institutional review board approval, we mailed pre-notice postcards in May 2014. We mailed the first wave of surveys via FedEx in June 2014 and sent reminders to non-responders through August 2014. The first survey packet included an up-front $25 cash incentive to participate.
Instrument
Our anonymous survey assessed multiple components of the content of physicians' communication about HPV vaccine and the context in which it occurs. Survey items pertaining to content and context were based in part on a previous survey on physician recommendation for HPV vaccination of males.35 To be clear, we asked physicians to respond to all items with regard to their male patients. We assessed the content of physicians' discussions about HPV vaccine for three domains. First, the survey asked physicians, “How do you usually present the HPV vaccine to your male patients/parents of male patients, in the following age groups [9-10, 11-12, 13-17, 18-21, 22-26]?” Response options included HPV vaccine is optional, HPV vaccine is routine, I do not discuss HPV vaccine with this age group, and I do not see male patients in this age group. Second, because ACIP guidelines recommend routine HPV vaccination for 11-12 year old males,36 we asked physicians two questions regarding the strength with which they recommend HPV vaccine relative to other ACIP-recommended vaccines on the 11-12 year old immunization platform. The survey asked, “For 11-12-year-old males, I recommend the HPV vaccine [less strongly than MCV4/Tdap, as strongly as MCV4/Tdap, more strongly than MCV4/Tdap].” MCV4 refers to meningococcal conjugate vaccine and Tdap refers to tetanus, diphtheria, and pertussis vaccine. Physicians also could indicate they do not see 11- to 12-year-old males.
Third, we assessed the content of physicians' discussions by asking, “When discussing HPV vaccination with male patients and their parents, how much emphasis do you place on the following aspects of the vaccine?” Content areas included prevention of genital warts in the patient himself, prevention of genital warts in sexual partners, prevention of cervical cancer in female sexual partners, prevention of anal cancer in the patient himself, possible prevention of penile cancer, vaccine safety in males, vaccine efficacy in males, and importance of vaccination prior to the onset of sexual activity (for patients who have not initiated sexual activity). Response options included strongly emphasize, somewhat emphasize, discuss only if questioned, do not discuss, and don't know/not sure. We reviewed these items individually, as well as examined emphasis on prevention of STIs and cancer on a broader scale. The two items pertaining to genital warts were collapsed to reflect discussion about STI prevention such that a somewhat emphasize or strongly emphasize response to at least one item constituted a discussion about STI prevention. The three items pertaining to cancer were similarly collapsed to reflect discussion about cancer prevention.
Context of physicians' HPV vaccine communication was assessed by asking two separate questions about the types of visits where physicians (1) see and (2) discuss HPV vaccination with adolescent males. The survey asked, “During what type of visit do you usually [see adolescent males, discuss HPV vaccination with adolescent males]?” Visit types included acute care visits, well-child visits, when the patient is in for other vaccines, school or college physicals, sports physicals, camp physicals, or other. We used these two items to create a variable that allowed us to examine whether physicians discuss HPV vaccine during the type(s) of visit(s) at which they see adolescent males. We also assessed context by asking two questions about other healthcare professionals' involvement in HPV vaccine recommendation and discussion: “In addition to you, do any of the following other healthcare professionals in your practice setting [make the initial recommendation for, discuss] HPV vaccination?” Response options included medical assistant, nurse (RN or BSN), nurse practitioner, physician assistant, other, or none of the above.
Physician characteristics measured included sex, age, race, ethnicity, number of years in practice, and clinical specialty. Practice characteristics included the number of physicians in the practice, practice situation (single specialty, multispecialty, other), practice type (private, other), practice location (urban, suburban, rural, other), race/ethnic category of the majority of patients seen, whether the practice serves patients who use Medicaid (Medicaid patients only, Medicaid and privately insured patients, no Medicaid patients), typical daily patient load, and whether the physician is a VFC provider.
Data analysis
We calculated frequencies and percentages for all variables using the SAS® 9.3 statistical software package (SAS Institute Inc., Cary, North Carolina).
Abbreviations
- ACIP
Advisory Committee on Immunization Practices
- AMA
American Medical Association
- HPV
human papillomavirus
- MCV4
meningococcal conjugate vaccine
- STI
sexually transmitted infection
- Tdap
tetanus, diphtheria, pertussis
- VFC
Vaccines for Children program
- US
United States
Disclosure of potential conflicts of interest
A.R.G. has received grant funding from Merck and is a consultant for Merck. The remaining authors report no conflicts.
Funding
This research was supported by a grant from the Bankhead-Coley Cancer Research Program (4BB10). Dr. Teri Malo is supported by the UNC Lineberger Cancer Control Education Program (R25CA057726). This work also has been supported in part by the Biostatistics Core Facility at the H. Lee Moffitt Cancer Center & Research Institute, an NCI designated Comprehensive Cancer Center (P30-CA076292).
References
- [1].Centers for Disease Control and Prevention . Recommendations on the use of quadrivalent human papillomavirus vaccine in males–Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep 2011; 60:1705-8; PMID:22189893 [PubMed] [Google Scholar]
- [2].Reagan-Steiner S, Yankey D, Jeyarajah J, Elam-Evans LD, Singleton JA, Curtis CR, MacNeil J, Markowitz LE, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2014. MMWR Morb Mortal Wkly Rep 2015; 64:784-92; PMID:26225476; http://dx.doi.org/ 10.15585/mmwr.mm6429a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Centers for Disease Control and Prevention HPV-associated anal cancer rates by state [Internet]. 2014. [cited 2015 Sept 11]. Available from: http://www.cdc.gov/cancer/hpv/statistics/state/anal.htm [Google Scholar]
- [4].Accelerating HPV Vaccine Uptake : Urgency for Action to Prevent Cancer. A Report to the President of the United States from the President's Cancer Panel. Bethesda, MD, 2014. [Google Scholar]
- [5].Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, Curtis RC, Markowitz L. Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure vaccine safety monitoring, 2006-2014 - United States. MMWR Morb Mortal Wkly Rep 2014; 63:620-4; PMID:25055185 [PMC free article] [PubMed] [Google Scholar]
- [6].Gilkey MB, Moss JL, McRee AL, Brewer NT. Do correlates of HPV vaccine initiation differ between adolescent boys and girls? Vaccine 2012; 30:5928-34; PMID:22841973; http://dx.doi.org/ 10.1016/j.vaccine.2012.07.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention . Human papillomavirus vaccination coverage among adolescent girls, 2007-2012, and postlicensure vaccine safety monitoring, 2006-2013 - United States. MMWR Morb Mortal Wkly Rep 2013; 62:591-5; PMID:23884346 [PMC free article] [PubMed] [Google Scholar]
- [8].National Foundation for Infectious Diseases Call to Action: HPV Vaccination as a Public Health Priority [Internet]. 2014 [cited 2015 Sept 21]. Available from: http://www.adolescentvaccination.org/professional-resources/hpv-resource-center/hpv-call-to-action.pdf [Google Scholar]
- [9].Gonik B. Strategies for fostering HPV vaccine acceptance. Infect Dis Obstet Gynecol 2006; 2006 Suppl:36797; PMID:16967911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].McKeever AE, Bloch JR, Marrell M. Human papillomavirus vaccination uptake and completion as a preventive health measure among female adolescents. Nurs Outlook 2015; 63:341-8; PMID:25982773; http://dx.doi.org/ 10.1016/j.outlook.2014.08.011 [DOI] [PubMed] [Google Scholar]
- [11].Goff SL, Mazor KM, Gagne SJ, Corey KC, Blake DR. Vaccine counseling: a content analysis of patient-physician discussions regarding human papilloma virus vaccine. Vaccine 2011; 29:7343-9; PMID:21839136; http://dx.doi.org/ 10.1016/j.vaccine.2011.07.082 [DOI] [PubMed] [Google Scholar]
- [12].Hughes CC, Jones AL, Feemster KA, Fiks AG. HPV vaccine decision making in pediatric primary care: a semi-structured interview study. BMC Pediatr 2011; 11:74; PMID:21878128; http://dx.doi.org/ 10.1186/1471-2431-11-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT. Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomarkers Prev 2015; 24:1673-9; PMID:26494764; http://dx.doi.org/ 10.1158/1055-9965.EPI-15-0326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gilkey MB, Moss JL, Coyne-Beasley T, Hall ME, Shah PD, Brewer NT. Physician communication about adolescent vaccination: how is human papillomavirus vaccine different? Prev Med 2015; 77:181-5; PMID:26051197; http://dx.doi.org/ 10.1016/j.ypmed.2015.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Babbel C, Markowitz LE, Dunne EF, Stokley S, Dickinson LM, et al.. A national survey of pediatrician knowledge and attitudes regarding human papillomavirus vaccination. Pediatrics 2006; 118:2280-9; PMID:17142510; http://dx.doi.org/ 10.1542/peds.2006-1946 [DOI] [PubMed] [Google Scholar]
- [16].Jensen ME, Hartenbach E, McElroy JA, Faerber A, Havighurst T, Kim KM, Bailey HH. Measuring the attitudes of health care professionals in Dane County toward adolescent immunization with HPV vaccine. WMJ 2009; 108:203-5; PMID:19753828 [PMC free article] [PubMed] [Google Scholar]
- [17].Alexander AB, Best C, Stupiansky N, Zimet GD. A model of health care provider decision making about HPV vaccination in adolescent males. Vaccine 2015; 33:4081-6; PMID:26143612; http://dx.doi.org/ 10.1016/j.vaccine.2015.06.085 [DOI] [PubMed] [Google Scholar]
- [18].McRee AL, Gilkey MB, Dempsey AF. HPV vaccine hesitancy: findings from a statewide survey of health care providers. J Pediatr Health Care 2014; 28:541-9; PMID:25017939; http://dx.doi.org/ 10.1016/j.pedhc.2014.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Centers for Disease Control and Prevention Tips and time-savers for talking with parents about HPV vaccine [Internet]. 2013 [cited 2015 Jul 23]. Available from: http://www.cdc.gov/vaccines/who/teens/for-hcp-tipsheet-hpv.html [Google Scholar]
- [20].Marcell AV, Klein JD, Fischer I, Allan MJ, Kokotailo PK. Male adolescent use of health care services: where are the boys? J Adolesc Health 2002; 30:35-43; PMID:11755799; http://dx.doi.org/ 10.1016/S1054-139X(01)00319-6 [DOI] [PubMed] [Google Scholar]
- [21].Perkins RB, Lin M, Silliman RA, Clark JA, Hanchate A. Why are US girls getting meningococcal but not human papilloma virus vaccines? Comparison of factors associated with human papilloma virus and meningococcal vaccination among adolescent girls 2008 to 2012. Womens Health Issues 2015; 25:97-104; PMID:25747517; http://dx.doi.org/ 10.1016/j.whi.2014.12.005 [DOI] [PubMed] [Google Scholar]
- [22].Centers for Disease Control and Prevention. Diphtheria: causes and transmission. [Internet]. 2015. [cited 2015 Nov 30]. Available from: http://www.cdc.gov/diphtheria/about/causes-transmission.html [Google Scholar]
- [23].Centers for Disease Control and Prevention Pertussis (whooping cough): causes and transmission. [Internet]. 2015 [cited 2015 Nov 30]. Available from: http://www.cdc.gov/pertussis/about/causes-transmission.html [Google Scholar]
- [24].National Cancer Institute HPV and Cancer [Internet]. 2015 [cited 2015 Sept 22]. Available from: http://www.cancer.gov/about-cancer/causes-prevention/risk/infectious-agents/hpv-fact-sheet [Google Scholar]
- [25].Perkins RB, Clark JA. Providers' attitudes toward human papillomavirus vaccination in young men: challenges for implementation of 2011 recommendations. Am J Mens Health 2012; 6:320-3; PMID:22398992; http://dx.doi.org/ 10.1177/1557988312438911 [DOI] [PubMed] [Google Scholar]
- [26].Selden TM. Compliance with well-child visit recommendations: evidence from the Medical Expenditure Panel Survey, 2000-2002. Pediatrics 2006; 118:e1766-78; PMID:17142499; http://dx.doi.org/ 10.1542/peds.2006-0286 [DOI] [PubMed] [Google Scholar]
- [27].Westwood M, Pinzon J. Adolescent male health. Paediatr Child Health 2008; 13:31-6; PMID:19119350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Vadaparampil ST, Malo TL, Kahn JA, Salmon DA, Lee JH, Quinn GP, Roetzheim RG, Bruder KL, Proveaux TM, Zhao X, et al.. Physicians' human papillomavirus vaccine recommendations, 2009 and 2011. Am J Prev Med 2014; 46:80-4; PMID:24355675; http://dx.doi.org/ 10.1016/j.amepre.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Daley MF, Crane LA, Markowitz LE, Black SR, Beaty BL, Barrow J, Babbel C, Gottlieb SL, Liddon N, Stokley S, et al.. Human papillomavirus vaccination practices: a survey of US physicians 18 months after licensure. Pediatrics 2010; 126:425-33; PMID:20679306; http://dx.doi.org/ 10.1542/peds.2009-3500 [DOI] [PubMed] [Google Scholar]
- [30].DeLucia PR, Ott TE, Palmieri PA. Performance in nursing. Rev Hum Factors Ergonomics 2009; 5:1-40; http://dx.doi.org/ 10.1518/155723409X448008 [DOI] [Google Scholar]
- [31].Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A brief educational intervention increases providers' human papillomavirus vaccine knowledge. Hum Vaccin Immunother 2015; 11:1331-6; PMID:25945895; http://dx.doi.org/ 10.1080/21645515.2015.1022691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].US. Food and Drug Administration Gardasil (human papillomavirus quadrivalent [types 6, 11, 16 and 18]): Highlights of prescribing information [Internet]. 2010 [cited 2015 Oct 1]. Available from: http://www.fda.gov/downloads/biologicsbloodvaccines/vaccines/approvedproducts/ucm111263.pdf [Google Scholar]
- [33].Centers for Disease Control and Prevention How many cancers are linked with HPV each year? [Internet]. 2014 [cited 2015 Oct 1]. Available from: http://www.cdc.gov/cancer/hpv/statistics/cases.htm [Google Scholar]
- [34].Kletke PR. Physician workforce data: when the best is not good enough. Health Serv Res 2004; 39:1251-5; PMID:15333107; http://dx.doi.org/ 10.1111/j.1475-6773.2004.00288.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Allison MA, Dunne EF, Markowitz LE, O'Leary ST, Crane LA, Hurley LP, Stokley S, Babbel CI, Brtnikova M, Beaty BL, et al.. HPV vaccination of boys in primary care practices. Acad Pediatr 2013; 13:466-74; PMID:24011749; http://dx.doi.org/ 10.1016/j.acap.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, Bocchini JA, Unger ER. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2014; 63:1-30; PMID:25167164 [PubMed] [Google Scholar]


