ABSTRACT
Purpose: We describe HPV vaccine attitudes among students of different education levels. Methods: High school, college, and graduate-level health care professional students were surveyed regarding HPV vaccine knowledge, attitudes, and receipt. Relationships between categorical variables were analyzed using chi-square tests of independence and z-tests for proportions. Means for quantitative variables were compared using t-tests and one-way analysis of variance. Results: 57% and 42% of the 889 students reported starting and completing HPV vaccine series, respectively, with no statistical difference by education level. 61% of students who reported receiving a provider recommendation had completed the series, compared to 6% of those who did not receive recommendation (p<0.001). The belief that HPV vaccine prevents cancer was strongly associated with vaccine completion (p=0.003). Conclusion: HPV vaccine coverage rates remain suboptimal. Future interventions should focus on improving provider recommendation and patient belief that HPV vaccine prevents cancer.
KEYWORDS: adolescent immunizations, human papillomavirus, HPV, vaccine attitudes, vaccine completion
Introduction
In the US, there are approximately 14 million new cases of human papillomavirus (HPV) infection each year, with up to half of these infections occurring in 15 to 24 year olds. Nationwide, 33,000 genitourinary and oropharyngeal cancers and 6,000 cancer-related deaths have been attributed to HPV annually.1 First licensed in the US in 2006, HPV vaccine is now routinely recommended for females aged 11 through 26 years and for males aged 11 through 21 years. The most recently approved and recommended 9-valent HPV vaccine has the potential to prevent up to 85% of HPV-associated cancers. Yet, HPV vaccine series completion remains low with rates of 38% and 14% for females and males, respectively.2 In response to suboptimal vaccine uptake, the Centers for Disease Control and Prevention has identified improving HPV vaccination rates as one of their top priorities.3
Parental, patient, and provider vaccine hesitancy are all obstacles to HPV vaccine completion. Parents and providers with low perception of adolescent disease risk and those who believe that vaccinating adolescents condones sexual activity or encourages ‘sexual debut’ are less likely to immunize against HPV.4-7 On the other hand, providers and parents who believe that HPV vaccine is effective in cancer prevention are more likely to administer HPV vaccine to the adolescent.8-11 There are few studies to date, however, looking at HPV vaccine knowledge, beliefs and receipt among adolescents and young adults over a range of education levels. In this study, we aim to describe HPV vaccine attitudes and factors associated with HPV vaccine completion among students at 3 education levels: high school, college, and graduate students in health care programs.
Results
A total of 889 completed questionnaires were included in this study from 415 (47%) high school, 252 (28%) college, and 222 (25%) health care professional students (Table 1). The student ages ranged from 14 through 26 years; 400/872 (46%) were male. The majority of the students were white and from a suburban community. 285/401 (71%) high school students, 119/244 (49%) college students, and 16/214 (7%) health care professional students stated their primary care provider is a pediatrician. 7/401 (2%) high school students, 24/244 (10%) college students, and 20/214 (9%) health care professional students state that they do not have a primary care provider. High school and college students (481/601, 80%) were more likely to have received a provider recommendation for HPV vaccine than health care professional students (108/202, 53%, p <0.001).
Table 2.
Questionnaire administered to enrolled adolescents.
| Has your doctor recommended HPV vaccine? Yes No Do not have a doctor | |||||
| HPV vaccine protects against genital warts. True False | |||||
| HPV vaccine protects against genital cancer. True False | |||||
| HPV vaccine protects against head and neck cancer. True False | |||||
| Have you received HPV vaccine? Yes No | |||||
| How many doses of HPV vaccine have you received? 0 1 2 3 4 5 | |||||
| If you have not received all doses, what is the reason for not finishing the HPV vaccine series? | |||||
| What is the main reason you accept/decline HPV vaccine? | |||||
| What source of HPV information do you trust most? Family/Friends Doctor News Media Social Media | |||||
| Select one response for each statement |
Strongly agree |
Agree |
Do not know |
Disagree |
Strongly disagree |
| HPV vaccine is important for the health of girls/women | |||||
| HPV vaccine is important for the health of boys/men | |||||
| I do not plan to receive HPV vaccine | |||||
| I plan to complete the HPV vaccine series | |||||
| I have already completed the HPV vaccine series | |||||
| HPV vaccine is safe | |||||
| HPV vaccine is effective in preventing genital cancers | |||||
| HPV vaccine is effective at preventing head/neck cancers | |||||
| I have friends who have received HPV vaccine | |||||
| I am concerned about short-term side effects | |||||
| I am concerned HPV vaccine has long-term health risks | |||||
| HPV vaccine is unnecessary | |||||
| HPV vaccine costs more than I can afford | |||||
| Receiving HPV vaccine will change my sexual behaviors | |||||
| It is hard to find time to get all doses of HPV vaccine | |||||
| It is hard to find a place to get all doses of HPV vaccine | |||||
| I would get HPV vaccine if my doctor recommended it | |||||
| I have enough information to make a decision about receiving HPV vaccine. | |||||
Table 1.
Demographics of the surveyed population.
| Total n (%) | High school n (%) | College n (%) | Health care profession n (%) | |
|---|---|---|---|---|
| Enrolled | 889 | 415 (47) | 252 (28) | 222 (25) |
| Gender answered | 872 (98) | 412 (99) | 245 (97) | 215 (97) |
| Male | 400 (46) | 197 (48) | 98 (40) | 105 (49) |
| Female | 472 (54) | 215 (52) | 147 (60) | 110 (51) |
| Age range (years) | 14–26 | 14–19 | 17–24 | 21–26 |
| Mean (median) age (years) | 19 (18) | 16 (16) | 20 (19) | 23 (23) |
| Community answered | 874 (98) | 407 (98) | 249 (99) | 218 (98) |
| Rural | 122 (14) | 28 (7) | 29 (12) | 65 (30) |
| Suburban | 645 (74) | 370 (91) | 160 (64) | 115 (53) |
| Urban | 107 (12) | 9 (2) | 60 (24) | 38 (17) |
| Ethnicity answered | 883 (99) | 415 (100) | 250 (99) | 218 (98) |
| White | 718 (81) | 382 (92) | 168 (67) | 168 (77) |
| African American | 34 (4) | 9 (2) | 16 (6) | 9 (4) |
| Hispanic | 21 (2) | 8 (2) | 12 (5) | 1 (<1) |
| Asian | 80 (9) | 4 (1) | 42 (17) | 34 (16) |
| Othera | 30 (3) | 12 (3) | 12 (5) | 6 (3) |
| Primary care provider answeredb | 859 (98) | 401 (97) | 244 (97) | 214 (96) |
| Pediatrics | 420 (48) | 285 (71) | 119 (49) | 16 (7) |
| Family practice | 309 (35) | 107 (27) | 84 (34) | 118 (55) |
| Internal Medicine | 63 (7) | 0 (0) | 8 (3) | 55 (26) |
| Obstetrician/gynecology | 16 (2) | 2 (<1) | 9 (4) | 5 (2) |
| No primary care provider | 51 (6) | 7 (2) | 24 (10) | 20 (9) |
| Provider recommended HPV vaccine/number answered | 589/803 (73) | 300/384 (78) | 181/217 (83) | 108/202 (53) |
Other ethnicity responses included Caribbean, European, Middle Eastern, and mixed
Some students identified more than one primary care provider
Of the 889 students, it was correctly reported that HPV vaccine protects against genital warts by 541 (61%), genital cancer by 653 (73%), and head and neck cancer by 276 (31%). Health care professional students were more likely than the collective group of high school and college students to correctly report that HPV vaccine protects against genital warts (179/222 (81%) vs 362/667 (54%), p < 0.0001), genital cancer (218/222 (98%) vs 435/667 (65%), p < 0.0001), and head and neck cancer (153/222 (69%) vs 123/667 (18%), p < 0.0001).
Of the students who answered the question regarding HPV vaccine receipt, the combined group of high school and college students (374/628, 60%) were more likely than the health care professional students (110/219, 50%) to have received any doses of HPV vaccine (p = 0.016). In total, 351 (42%) of the 829 students who had provided the number of doses of HPV vaccine received had completed the vaccine series. Of the 380 high school students who reported the number of HPV vaccine doses received, 232 (61%) and 167 (44%) started and completed vaccine se-ries, respectively. Similarly, 137/231 (59%) and 94/231 (41%) college students started and completed vaccine series, respectively and 107/218 (49%) and 90/218 (41%) health care professional students started and completed vaccine series, respectively. There was no difference in HPV vaccine completion by education level (p = 0.74). Health care professional students (109/216 (50%)) were more likely than the combined group of high school and college students (253/611, 41%) to have not received any doses of HPV vaccine (p = 0.021), but also were more likely to have completed the vaccine series once started (87/107, 81% vs 254/358, 71%,p = 0.03).
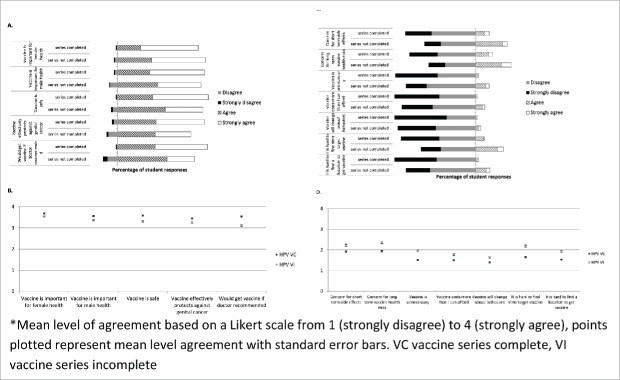
The most common reason provided for accepting HPV vaccine by high school students was promotion of health, by college students was doctor recommendation and prevention of sexually transmitted infection, and by health care professional students was cancer prevention. On the other hand, the most common reason provided for not receiving HPV vaccine by students of all education levels was lack of doctor recommendation (68/196, 35%) (Fig. 1).
Figure 1.
Reasons for accepting [A] and declining [B] HPV vaccine given by 226 high school students (HS), 133 college (C) students, and 97 health care professional (HCP) students.
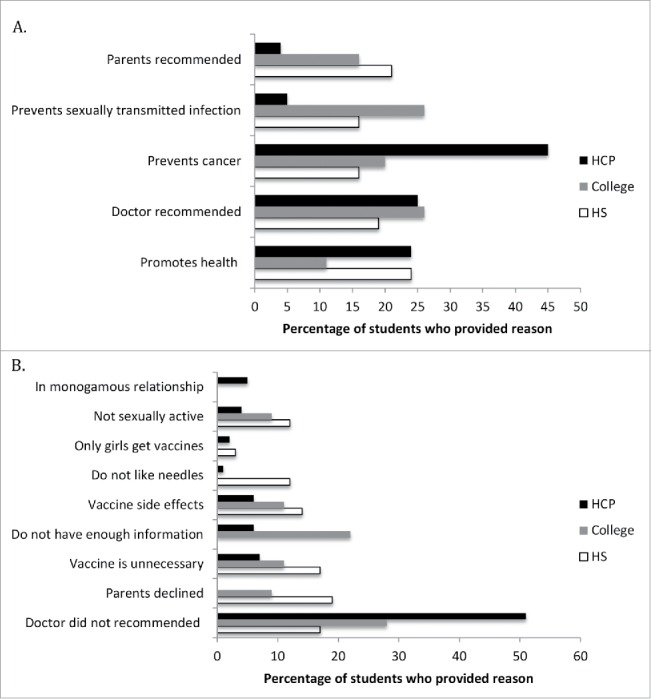
Health care professional students had a higher mean level of agreement when compared to the high school and college students for the belief that HPV vaccine is important for female health (3.76 vs 3.55, p<0.0001) and that HPV vaccine is safe (3.55 vs 3.40, p = 0.02). Similarly, health care professional students had a lower mean level of agreement when compared to the high school and college students for expressing concern with short term vaccine side effects (1.80 vs 2.22, p<0.0001), concern with long term vaccine health risks (1.91 vs 2.30, p<0.0001), and the belief that HPV vaccine receipt would change sexual behaviors (1.37 vs 1.59, p<0.0001). (Fig. 2)
Figure 2.
Responses to survey questions [A] and mean level of agreement* [B] regarding HPV vaccine attitudes among high school and college (HS/C) and health care professional (HCP) students.
Factors associated with HPV vaccine series completion include primary care provider specialty, any provider recommendation for vaccine receipt, and source of HPV vaccine information. Higher vaccine completion rates were seen among students with a primary provider pediatrician (187/378, 49%) when compared to students cared for by family practitioners (116/301, 39%) or had no provider (7/45, 16%) (p < 0.05) (Table 1). Similarly, vaccine completion rates were higher among students cared for by obstetrician/gynecologists (14/19, 74%) than those cared for by internists (33/73, 45%), family practitioners (116/301, 39%) or had no provider (7/45, 16%) (p<0.05) (Table 1). Sixty one percent (357/583) of the students who reported receiving a specific provider vaccine recommendation had completed the vaccine series, compared to only 6 percent (12/216) of those who did not receive provider vaccine recommendation (p<0.001). Students who reported that their HPV vaccine information source was the doctor had a higher vaccine completion rate when compared to students whose information source was family and friends (p=0.009). Additionally, females (204/440, 46%) were more likely than males (128/372, 34%) to have completed the HPV vaccine series (p = 0.001). Correctly identifying that HPV vaccine prevents genital cancers was associated with vaccine completion (277/622, 45% vs 50/170, 29% (p<0.01), but not with correctly identifying that HPV vaccine prevents genital warts (p = 0.095) or head and neck cancer (p = 0.573).
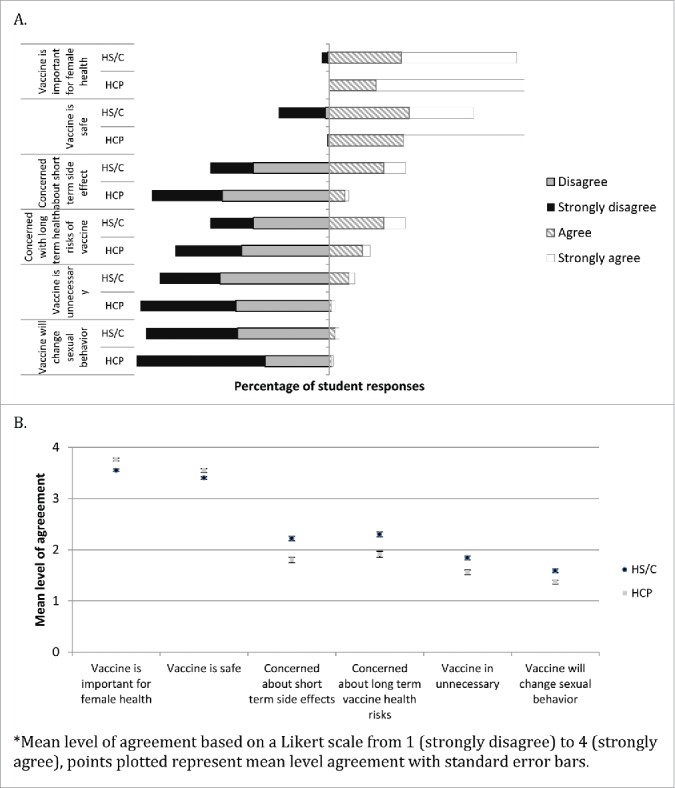
Attitudes that were positively associated with HPV vaccine completion include the beliefs that HPV vaccine is important for the health of females (p = 0.003), is important for the health of males (p<0.0001), is safe (p<0.0001), and is effective in preventing genital cancer (p = 0.003) (Fig. 3). Attitudes negatively associated with HPV vaccine completion were stating concern for the short-term vaccine side effects (p<0.0001) or long-term vaccine health risks (p<0.0001) or believing that HPV vaccine is unnecessary (p<0.0001). Students who admitted difficulty in finding the time or place to get HPV vaccine were also less likely to have completed the vaccine series (p<0.0001 in each case) (Fig. 3).
Figure 3.
HPV vaccine attitudes and mean level of agreement* for factors positively (A and B) and negative (C and D) associated with HPV vaccine series completion.
Discussion
To our knowledge, this is one of the first studies to describe HPV vaccine attitudes and factors associated with HPV vaccine completion, by students at different educational levels. Despite the Advisory Committee on Immunization Practices (ACIP) recommendation for routine administration of HPV vaccine to females since 2006 and males since 2011, vaccine coverage remains suboptimal. In our study, 42% of surveyed students (34% males, 46% females) between the ages of 14 and 26 years reported completing the HPV vaccine series. While our cohort reported vaccine series completion rates somewhat higher than the national reported rates of 22% and 40% for males and females, respectively, rates remain suboptimal 4–9 years after the initial recommendation. Further determination of factors associated with vaccine completion at different educational stages may reveal potential interventions for a sustained increase in HPV vaccine coverage rates.
We found that parental decision making was a major contributor to HPV vaccine acceptance and refusal for the enrolled high school students, supporting current efforts to target provider-parent communication to improve HPV vaccine uptake in the young adolescent population. Addressing parental concerns regarding HPV vaccine safety and benefits and providing a strong vaccine recommendation have been associated with increased parental vaccine acceptance and adolescent vaccine uptake (Clark).
Published studies describing provider and/or parental HPV vaccine attitudes are important and well documented, but the patient's perspective regarding HPV vaccine provides different and unique insights into strategies that may prove more successful in improving vaccine uptake. While parents make the final vaccine decision for students under the age of 18 years, many are influenced by their adolescent's attitudes, particularly with increasing adolescent age.8,12 Understanding adolescent beliefs and factors positively and negatively associated with vaccine uptake and completion can lead to the development of interventions that focus on reducing patient vaccine hesitancy and increasing adolescent vaccination. It may be important to re-visit the HPV vaccine decision with adolescents who are not immunized prior to age 18 years due to parental hesitancy as their views and decisions may not align with those of their parents.
During our study, we found that cancer prevention was a common theme to vaccine acceptance and completion. We also found, as expected, that HPV risk denial, belief that vaccine is unnecessary, belief that only females need vaccine, or the belief that the student is not at risk because he/she is not sexually active or is in a monogamous relationship, contributed to vaccine refusal. Similar findings have been described among health care providers, as providers who believe HPV vaccine prevents cancer are more likely to strongly recommend vaccine while providers who associate HPV vaccine with sexual activity are less likely to recommend vaccine to their patients.8-11,13-15 Based on these findings, interventions that promote de-associating HPV vaccine from sexual activity, and focus instead on HPV vaccine effectiveness in preventing cancer appear likely to improve HPV vaccination coverage rates.
We found that adolescents who obtain vaccine information from their provider and those who had received a specific provider based vaccine recommendation were more likely to have completed the HPV vaccine series, supporting the previously described impact that providers have in patient and parent vaccine decision making.16-19 More specifically, nearly all students stated they would receive HPV vaccine if recommended by their provider. In this work, surveyed high school and college students were more likely to have received a provider vaccine recommendation when compared to the health care professional students, suggesting that more providers are routinely recommending HPV vaccine to the younger adolescents. Furthermore, we found that surveyed adolescents whose providers were pediatricians or obstetricians/gynecologists were more likely to be HPV vaccine series complete when compared to those whose providers were family practitioners or internists, highlighting another potential provider obstacle to student immunization completion. While, pediatricians are generally known to be more adherent to ACIP vaccine recommendations than family practitioners, few studies assess vaccine attitudes and practices of internal medicine physicians.14,20-23 One study found that even though 93% of surveyed obstetrician-gynecologists and family practitioners routinely recommended HPV vaccine to females, they most commonly did so for adolescents between the ages of 13 and 26 years, despite the ACIP recommendation that vaccine is administrated starting at age 11 or 12 year.24 Barriers to stocking and administering vaccines in internal medicine and family practice offices have also been described, including difficulties with reimbursement, high cost of purchasing vaccines and maintaining inventory, the potential for financial loss if vaccines expire before use, patient refusal, and the notion that patients can ‘get vaccines elsewhere’.25, 26 Specifically, Freed found that more than one-third of family practice and internal medicine offices did not stock HPV vaccine.26
Knowledge that HPV vaccine prevents genital warts, genital cancers, and head and neck cancers alone was not enough to result in completion of vaccine series among the students we surveyed. Health care professional students were more likely to have knowledge regarding HPV vaccine, but were less likely to have provider recommendation for vaccine when compared to the high school and college students. The lack of difference in vaccine completion rates between the students of the various education levels suggests that improving disease and vaccine knowledge alone is unlikely to impact current vaccination rates substantially. Instead, interventions which involve a combination of improving a specific provider-based recommendation as well as adolescent knowledge regarding HPV disease and the benefits of HPV vaccine together appears to have the highest potential of increasing HPV vaccination rates in this population.
There are several limitations to this study. First the majority of our students were white and from suburban communities, and therefore our data cannot be generalized to the entire student population. Second, the results of this study are dependent on recall of vaccine receipt and whether or not a specific recommendation was made by the provider. Last, while we recognize the limitations of survey methodology, this study allowed us to describe vaccine attitudes and factors associated with HPV vaccine completion among 889 students at different education levels and determine areas for future interventions to improve vaccine coverage rates in this population.
In conclusion, our data brings to attention several points regarding HPV vaccination among students. First, determining HPV vaccine attitudes of provider groups appears crucial. Most publish data focuses on pediatric and gynecologic providers, but family practitioners and internal medicine physicians will also be presented with students who have yet to be immunized. Studying vaccine attitudes among these groups is an important step in understanding and removing obstacles to HPV vaccine administration in those practices. Second, while some providers and parents may believe that the students can wait to receive HPV vaccine, the likelihood of vaccination decreases as patients transition to non-pediatric providers. This is especially problematic for adolescents who do not find another provider after leaving the pediatric office. In fact, ∼10% of the students we surveyed in college and health care professional school stated that they did not have a health care provider. For these reasons, it is important to capture adolescents, as recommended by the ACIP, at the 11- or 12-year old visit when they are in the office receiving other routinely recommended adolescent vaccines.
Methods
The study team developed a one page, self-administered questionnaire regarding HPV vaccine knowledge, attitudes, and receipt (Table 2). The survey was pilot tested with a convenience sample to ensure clarity of questions and ease of administration. The paper questionnaire was explained and distributed to students of public high school, college, and graduate-level health care professional schools (including medical and physician assistant school) in New York State by peers at the same education level. The students were asked to anonymously complete the questionnaire and return it to the peer study team member. There were no incentives offered for participation.
Students were excluded from the study if they were older than 26 years of age, since they would no longer be eligible for HPV vaccination. Demographic information, including gender, current education level (high school, college, health care profession), home community (rural, suburban, urban), ethnicity, and primary care provider (pediatrician, family practitioner, internist, obstetrician/gynecologist, no provider) were collected. Questions regarding HPV vaccine knowledge, attitudes, and receipt were asked. This study was deemed exempt from review by the SUNY Upstate Medical University institutional review board.
Student attitudes regarding HPV vaccine were assessed by the use of a Likert scale questionnaire, with an agreement level of 1 representing strongly disagree, 2 disagree, 3 agree, and 4 strongly agree. In all cases, the mean levels of agreement for the high school and college students were closer to each other than to the health care professional students, therefore the high school and college students were combined into one group for the statistical analyses.
Statistical analysis
Descriptive statistics were used to quantify salient demographic and other characteristics of the sample. Association between vaccine completion and categorical factors such as education level and physician recommendation were tested using Pearson's chi-square tests of independence or Fisher's exact tests, as indicated. Differences in percentages between groups were also compared using z-tests for independent proportions. Ordinal Likert-scale measures of attitudes and beliefs were compared across educational levels and between other factors such as primary care physician specialty using t-tests and one-way analysis of variance.
All statistical testing was conducted using a priori α=.05, and 2-tailed p-values are reported. When applicable, Sidak-adjustment or other post-hoc comparison methods were used to maintain family-wise error rates at .05. All statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 22.0. (IBM Corp., Armonk, NY).
Abbreviations
- HPV
Human papillomavirus
- ACIP
Advisory Committee on Immunization Practices
Disclosure of potential conflicts of interest
MS has research funding from GlaxoSmithKline. JBD has funding for clinical vaccine trials from GlaxoSmithKline and Merck.
References
- [1].CDC Human papillomavirus vaccination: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2014; 63:1-30. [PubMed] [Google Scholar]
- [2].CDC . Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014 – United States. MMWR 2014; 63:620-4; PMID:25055185 [PMC free article] [PubMed] [Google Scholar]
- [3].CDC Human Papillomavirus and Cancer. Available at www.cdc.gov/cancer/hpv. Accessed July1, 2015. [Google Scholar]
- [4].Thomas TL, Strickland O, Diclemente R, Higgins M. An opportunity for cancer prevention during preadolescence and adolescence: stopping human papillomavirus (HPV)-related cancer through HPV vaccination. J Adolesc Health 2013; 52:S60-8; PMID:23298993; http://dx.doi.org/ 10.1016/j.jadohealth.2012.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Rand CM, Schaffer SJ, Humiston SG, Albertin CS, Shone LP, Heintz EV, Blumkin AK, Stokley S, Szilagyi PG. Patient-provider communication and human papillomavirus vaccine acceptance. Clin Pediatr 2011; 50:106-13; http://dx.doi.org/ 10.1177/0009922810379907 [DOI] [PubMed] [Google Scholar]
- [6].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents. A systematic review of the literature. JAMA Pediatr 2014; 168:76-82; PMID:24276343; http://dx.doi.org/ 10.1001/jamapediatrics.2013.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Perkins RB, Clark JA. Providers' perceptions of parental concerns about HPV vaccination. J Health Care Poor Underserved 2013; 24:828-39; PMID:23728048; http://dx.doi.org/ 10.1353/hpu.2013.0080 [DOI] [PubMed] [Google Scholar]
- [8].Griffioen AM, Glynn S, Mullins TK, Zimet GD, Rosenthal SL, Fortenberry JD, Kahn JA. Perspectives on decision making about human papillomavirus vaccination among 11- to 12- year old girls and their mothers. Clin Pediatr 2012; 51:560-8; http://dx.doi.org/ 10.1177/0009922812443732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jeudin P, Liveright E, del Carmen MG, Perkins RB. Race, ethnicity, and income factors impacting human papillomavirus vaccination rates. Clin Ther 2014; 36:24-37; PMID:24417783; http://dx.doi.org/ 10.1016/j.clinthera.2013.11.001 [DOI] [PubMed] [Google Scholar]
- [10].Brawner BM, Baker JL, Voytek CD, Leader A, Cashman RR, Silverman R, Peter N, Buchner BJ, Barnes CA, Jemmott LS, et al.. The development of a culturally relevant theoretically driven HPV prevention intervention for urban adolescent females and their parents/guardians. Health Promot Pract 2013; 14:624-36; PMID:23099659; http://dx.doi.org/ 10.1177/1524839912462389 [DOI] [PubMed] [Google Scholar]
- [11].Kennedy S, Osgood R, Rosenbloom L, Feinglass J, Simon M. Knowledge of human papillomavirus among publicly and privately insured women. J Midwifery Women's Health 2011; 56:481-7; http://dx.doi.org/ 10.1111/j.1542-2011.2011.00040.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Clark SJ, Cowan AE, Fillipp SL, Fisher AM, Stokley S. Parent perception of provider interactions influences HPV vaccination status of adolescent females. Clinical Pediatrics 2015; http://dx.doi.org/ 10.1016/j.pedn.2015.12.013 [DOI] [PubMed] [Google Scholar]
- [13].Gowda C, Schaffer SE, Dombrkowski KJ, Dempsey AF. Understanding attitudes toward adolescent vaccination and the decision-making dynamic among adolescents, parents, and providers. BMC Public Health 2012; 12:509; PMID:22768870; http://dx.doi.org/ 10.1186/1471-2458-12-509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bynum SA, Staras SAS, Malo TL, Giuliano AR, Shenkman E, Vadaparampil ST. Factors associated with Medicaid providers' recommendation for the HPV vaccine to low-income adolescent girls. J Adolesc Health 2014; 54:190-6; PMID:24064282; http://dx.doi.org/ 10.1016/j.jadohealth.2013.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Daley MF, Crane LA, Markowitz LE, Black SR, Beaty BL, Barrow J, Babbel C, Gottlieb SL, Liddon N, Stokley S, et al.. Human papillomavirus vaccination practices: a survey of US physicians 18 months after licensure. Pediatrics 2010; 126:425-33; PMID:20679306; http://dx.doi.org/ 10.1542/peds.2009-3500 [DOI] [PubMed] [Google Scholar]
- [16].Perkins RB, Clark JA, Apte G, Vercruysse JL, Sumner JJ, Wall-Haas CL, Rosenquist AW, Pierre-Joseph N. Missed opportunities for HPV vaccination in adolescent girls: a qualitative study. Pediatrics 2014; 134:e666-74; PMID:25136036; http://dx.doi.org/ 10.1542/peds.2014-0442 [DOI] [PubMed] [Google Scholar]
- [17].Suryadevara M, Bonville CA, Cibula DA, Valente M, Handel A, Domachowse JR, Domachowske JB. Pertussis vaccine for adults: Knowledge, attitudes, and vaccine receipt among adults with children in the household. Vaccine 2014; 32:7000-4; PMID:25454869; http://dx.doi.org/ 10.1016/j.vaccine.2014.10.018 [DOI] [PubMed] [Google Scholar]
- [18].Gargano LM, Herbert NL, Painter JE, Sales JM, Morfaw C, Rask K, Murray D, DiClemente RJ, Hughes JM. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Hum Vaccin Immunother 2013; 9:2627-33; PMID:23883781; http://dx.doi.org/ 10.4161/hv.25823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rickert VI, Rehm SJ, Aalsma MC, Zimet GD. The role of parental attitudes and provider discussions in uptake of adolescent vaccines. Vaccine 2015; 33:642-7; PMID:25529293; http://dx.doi.org/ 10.1016/j.vaccine.2014.12.016 [DOI] [PubMed] [Google Scholar]
- [20].Rosenthal SL, Weiss TW, Zimet GD, Ma L, Good MB, Vichnin MD. Predictors of HPV vaccine uptake among women aged 19–26: Importance of a physician's recommendation. Vaccine 2011; 29:890-5; PMID:20056186; http://dx.doi.org/ 10.1016/j.vaccine.2009.12.063 [DOI] [PubMed] [Google Scholar]
- [21].Vadaparampil ST, Malo TL, Kahn JA, Salmon DA, Lee JH, Quinn GP, Roetzheim RG, Bruder KL, Proveaux TM, Zhao X, et al.. Physicians' human papillomavirus vaccine recommendations, 2009 and 2011. Am J Prev Med 2014; 46:80-84; PMID:24355675; http://dx.doi.org/ 10.1016/j.amepre.2013.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Allison MA, Cohn AC, Stokley S, Crane LA, O'Leary ST, Hurley LP, Babbel CI, Dong F, Gahm C, Temte JL, et al.. Timing of adolescent meningococcal conjugate vaccination attitudes and practices of pediatricians and family medicine physicians. Am J Prev Med 2011; 41:581-7; PMID:22099234; http://dx.doi.org/ 10.1016/j.amepre.2011.08.007 [DOI] [PubMed] [Google Scholar]
- [23].Schaffer SJ, Humiston SG, Shone LP, Averhoff FM, Szilagyi PG. Adolescent immunization practices: a national survey of US physicians. Arch Pediatr Adolesc Med 2001; 155:566-71; PMID:11343499; http://dx.doi.org/ 10.1001/archpedi.155.5.566 [DOI] [PubMed] [Google Scholar]
- [24].Oster NV, McPhillips-Tangum CA, Averhoff F, Howell K. Barriers to adolescent immunization: A survey of family physicians and pediatricians. J Am Board Fam Pract 2005; 18:13-9; PMID:15709059; http://dx.doi.org/ 10.3122/jabfm.18.1.13 [DOI] [PubMed] [Google Scholar]
- [25].Roland KB, Benard VB, Greek A, Hawkins NA, Saraiya M. Primary care providers human papillomavirus vaccine recommendations for the medically underserved: A pilot study in US Federally Qualified Health Centers. Vaccine 2014; 32:5432-5; PMID:25131744; http://dx.doi.org/ 10.1016/j.vaccine.2014.07.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hurley LP, Bridges CB, Harpaz R, Allison MA, O'Leary ST, Crane LA, Brtnikova M, Stokley S, Beaty BL, Jimenez-Zambrano A, et al.. US physicians' perspective of adult vaccine delivery. Ann Intern Med 2014; 160:161-170; PMID:24658693; http://dx.doi.org/ 10.7326/M13-2332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Freed GL, Clark SJ, Cowan AE, Coleman MS. Primary care physician perspectives on providing adult vaccines. Vaccine 2011; 29:1850-4; PMID:21216314; http://dx.doi.org/ 10.1016/j.vaccine.2010.12.097 [DOI] [PubMed] [Google Scholar]