abstract
Objective: To describe why adolescent females who initiated HPV vaccination completed or did not complete the series.
Methods: Semi-structured interviews were conducted with parents/guardians of 11–17 year old female adolescents and their pediatric primary care providers in one inner-city public clinic and three private practices to ascertain why girls who initiated HPV vaccination did or did not complete the series. Qualitative analysis was used to identify perceived barriers and facilitators of completion.
Results: 65 parents/guardians participated: 37 whose daughters received 1 or 2 HPV vaccine doses and 28 whose daughters completed the series. 89% (n = 33) of parents who did not complete the series intended to do so, but were not reminded by the clinic or encountered logistical barriers. Four (11%) decided to stop the vaccine series. 33 providers participated: 24 physicians, 3 nurse practitioners, and 6 registered nurses. Half (n = 14, 52%) of the providers said they told parents when the next doses were due but relied on parents to schedule appointments, 11 (41%) scheduled the second dose when the first dose was given, and 2 (7%) tried to immunize patients when they returned for other appointments. None of the four practices had a reminder/recall system in place to ensure series completion. Of note, neither parents nor providers stated that the need for three doses was a barrier to series completion.
Conclusions: Most failure to complete the HPV vaccine series occurred because providers expected parents to make appointments while parents expected to be reminded. Increased use of reminder/recall systems and team-based care with clear communication of expectations regarding appointment scheduling could increase completion rates.
KEYWORDS: HPV vaccination, vaccine series completion, qualitative research, parents' attitudes, physician attitudes
Introduction
Currently available HPV vaccines can prevent the majority of cervical, vaginal, vulvar and anal dysplasias and genital warts.1-3 Since the licensures of these vaccines, vaccine-type HPV prevalence has decreased by over 50%, and rates of cervical cancer precursors have declined.4,5 However, vaccine administration is complicated, as it consists of three doses given six months apart. Vaccination rates for girls have risen slowly since 2011.6 The overall rates of initiating and completing the HPV vaccine series among US girls are only 60% and 40% respectively.7 Protection against cervical dysplasia and genital warts is inferior with incomplete dosing,7,8 and the long-term effectiveness of incomplete vaccination is undetermined,9-11 therefore the low rate of completion among those who start the series is of particular concern. Low income and minority girls have lower rates of series completion compared with white and affluent girls, though completion rates are poor among adolescents of all races.13-19 Disparate patterns of HPV vaccine receipt could exacerbate existing cervical cancer health disparities, as poor and minority women are at the highest risk for cervical cancer.12-14 Reasons for incomplete vaccination are not well understood.15,16 Therefore we conducted a qualitative study in both safety net and private practice settings to explore barriers and facilitators of HPV vaccine series completion, as perceived by parents/guardians of girls who initiated and either completed or did not complete the three-dose series, and their pediatric providers.
Results
Parents/guardians motivations for vaccination
65 parents/guardians participated: 37 whose daughters received 1 or 2 doses of HPV vaccine (Incomplete Group) and 28 whose daughters completed 3 doses (Complete Group) (Table 1). Parents whose daughters did not complete the series were more often younger, self-identified as Black or Latino, foreign-born, had lower educational attainment and annual household income, and used public insurance than those whose daughters completed the series.
Table 1.
Demographic characteristics of parents/guardians.
| Variable Mean (range) or N (%) | Complete | Incomplete | P value* |
|---|---|---|---|
| Total | 28 | 37 | |
| Age of parent/guardian | 49.2 (32-65) | 41.7 (27-54) | <0.001 |
| Race | |||
| White | 19 (68) | 5 (14) | |
| Black | 4 (14) | 20 (54) | <0.001 |
| Hispanic | 4 (14) | 6 (16) | |
| Other | 1 (4) | 6 (16) | |
| Interviewee is | |||
| Mother | 23 (82) | 35 (95) | |
| Father | 3 (11) | 1 (3) | 0.34 |
| Guardian | 2 (7) | 1 (3) | |
| Interviewee is | |||
| Male | 3 (11) | 1 (3) | 0.31 |
| Female | 25 (89) | 36 (97) | |
| Marital status | |||
| Married | 18 (64) | 14 (38) | |
| Single | 3 (11) | 12 (32) | 0.11 |
| Divorced/Widowed/Separated | 6 (21) | 8 (22) | |
| Non-marriage partners | 1 (4) | 3 (8) | |
| Country of origin | |||
| US | 26 (93) | 24 (65) | 0.008 |
| Other | 2 (7) | 13 (35) | |
| Religious affiliation | |||
| No | 12 (43) | 18 (49) | 0.64 |
| Yes | 16 (57) | 19 (51) | |
| Education | |||
| Less than high school | 2 (7) | 6 (16) | |
| High school graduate | 6 (21) | 15 (41) | 0.009 |
| Some college | 7 (25) | 8 (22) | |
| College graduate | 8 (29) | 6 (16) | |
| Post-college | 5 (18) | 2 (5) | |
| Household income | |||
| <$20000 | 4 (15) | 15 (42) | |
| $21-40000 | 6 (22) | 7 (19) | <0.001 |
| $41-60000 | 4 (15) | 7 (19) | |
| $61-100000 | 2 (7) | 4 (11) | |
| >$100000 | 11 (41) | 3 (8) | |
| Insurance | |||
| Public | 12 (43) | 25 (68) | 0.046 |
| Private | 16 (57) | 12 (32) |
Demographic differences notwithstanding, parents in both groups expressed similar reasons for initiating the HPV vaccine series (Fig. 1). More than two-thirds of parents/guardians in both groups stated they felt that the benefits of HPV vaccination outweighed the risks. Over one third of parents felt that parents were responsible for protecting their children with HPV vaccination, and more than 30% stated that their trusting relationships with their providers were their primary reasons for vaccinating. Small numbers of parents in both groups felt their daughters needed the vaccine because all adolescents are likely to have sexual intercourse at some point. Some differences emerged regarding belief in vaccine effectiveness, however. Nearly half of parents who completed the series (13 of 28) cited the effectiveness of the vaccine in preventing cancer, compared with 16% (6 of 37) parents of girls who did not complete the series.
Figure 1.
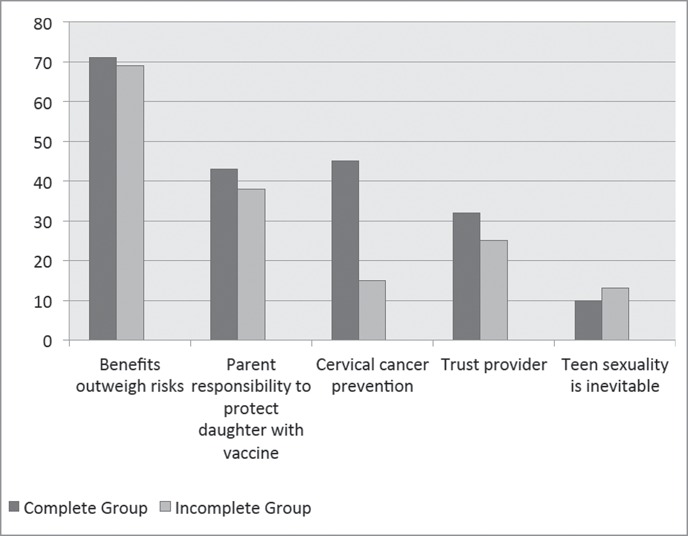
Motivating reasons for vaccinating in Complete and Incomplete groups. Parents/guardians provided reasons why they initiated the vaccine series for their daughters. Parents could express multiple reasons, which are represented in the percentages above.
Parents/guardians reasons for not completing the HPV vaccine series
Nearly all (33 of 37) of participants whose daughters did not complete the series had intended to complete all three doses. Participants' reasons for not completing the vaccine series fell into three broad categories: 1) expectation that their provider's office would remind them of future shots (expect reminder), 2) inconvenience or access barriers (inconvenience), and 3) changing their minds after the first shot (conscious decision) (Fig. 2, Table 2). Of note, parents did not state that the need for three doses was a barrier to series completion.
Figure 2.
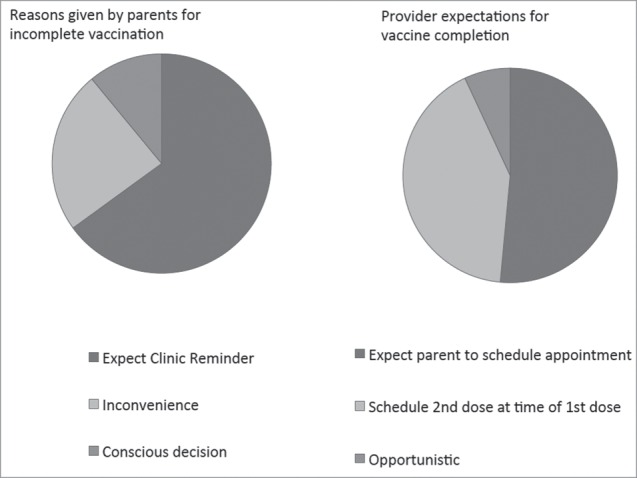
Comparison of reasons parents cited for incomplete vaccination and provider expectations for vaccine series completion Legend. Most parents expected clinic reminders for subsequent doses, while most providers expected parents to schedule follow-up doses themselves.
Table 2.
Summary of barriers described by parents/guardians and providers.
|
Parents expect clinic reminder (reported by 65% of parents; n = 24) “Because parents today they are very busy working, keeping the schedule, send the kids to school, keep the kids in school, it's too much stress for parents today. Then you know to keep in track all of the appointments and everything, it's very difficult so if the staff at least can remind them when they go to visit the doctor that what vaccine they missing so that way they keep a track of the kids vaccinations and that way they can help the kids to prevent this.”–Hispanic mother of 17 year-old, private practice, Complete Group “I didn't know it was 3 shots. Maybe if they don't do it on the visits, they don't call you back and say this is what happened then you know you don't really know” – Black mother of 12 year-old, public clinic, Incomplete Group “I would have probably brought her if I had gotten something just to remind me” –Caucasian mother of 11 year-old, private practice, Incomplete Group “It's in the system. They have all the records. So if it is important they will give it to her.” (54 year old mother of 14 year old, public clinic, Incomplete Group) |
|
Parents find returning for shot inconvenient (reported by 24% of parents; n = 9) “I think it's just one of those things. You get busy and then you put it off and the next thing you know, you never went back to have a follow-up. I'm guilty of it so I can see that happening. It's unfortunate that it can't be done in one shot.” –Caucasian mother of 14 year-old, private practice, Complete Group “A lot of people are, you know, it's not that they don't want to do things, it's just that we're busy, we forget, don't realize the importance” –Caucasian mother of 15 year-old, private practice, Complete Group “I forgot that she had the second appointment. Typically, normally she is a healthy child and she has always been up to date on immunizations.” –Black mother of 11 year-old, public practice, Incomplete Group |
|
Providers expect parents to make appointments (reported by 52% of providers; n = 14) “We're dependent on parents and families remembering to come and get a painful shot… I have virtually no belief that we're very effective.” –Pediatrician, public clinic |
|
Providers feel that busy schedules interfere with series completion (reported by 37% of providers; n = 10) “The big no show rate and then a lot of teenagers don't think they need to come in because there are no real required shots after 11 and then they feel kind of invincible.” –Pediatrician, private practice |
|
Providers feel that few parents make a conscious decision to stop seriesa “I've had maybe a half a dozen that I can think of off the top of my head that have had one HPV and the parents refuse to continue the series and they've had no adverse reaction to it, none.” –Nurse practitioner, private practice |
Percentage not reported, as providers were asked generally why adolescents did not complete the series, not specifically whether they felt parents consciously decided to stop the series, so the denominator could not be calculated.
Expect clinic reminder
Most girls (65%, n = 24) did not obtain all three shots because the parents/guardians expected that the clinic would contact them regarding scheduling any additional doses. Specific difficulties included in this category included: a lack of clinic reminders (n = 5, 21%), subsequent appointments not being scheduled at the time of visit (n = 5, 21%), and missed opportunities where the adolescent had an appointment but was not vaccinated (n = 4, 17%) or where a parent/guardian forgot or missed an appointment and the appointment was not rescheduled (n = 3, 17%). These parents/guardians felt that ensuring vaccine series completion is the responsibility of the provider or the clinic, not the patient: “It's a physician's job to discuss these things with parents. And you know, if it's not being done, then that's on them,” (33 year old mother of 14 year old, public clinic, Incomplete Group).
Inconvenience
Nine parent/guardians (24%) mentioned access barriers or inconvenience as the primary reason for failing to complete the vaccine series (Fig. 2, Table 2). Barriers included in this category included parents/guardians' and adolescents' busy schedules (n = 5, 56%), other health problems that took precedence over completing HPV vaccine series (n = 3, 33%), and long commutes to the clinic (n = 1, 11%).
Conscious decision
Conscious decisions to halt the series were reported by only four participants (11%). Interestingly, no parent/guardian stopped the series due to a side effect or adverse event. The first parent was highly motivated to vaccinate: “Because I know that there'll be some point in time she'll be sexually active, so I'd rather [be] on board with it early to prevent what could or couldn't happen. That's why I choose to do it early.” However she had a negative experience with the person who gave the injection, and discontinued the series for this reason. The second mother stopped the vaccine series after the first shot due to negative media: “I don't remember what I started hearing, but it was just you know all the talk, I don't know.” However, she later said she would support the HPV vaccine after receiving more education and when she perceived it as one of the “normal shots.” The third parent also decided to halt the vaccine series after her 16 year old daughter was given the first dose also due to concerns about side effects: “All I know is that they are putting a virus in her body, and to me a virus is not good. We are trying to keep the virus out of her body so I don't understand why they would put a virus in her body to combat a virus that's gonna come later on.” The last of the four parents who decided to stop the series did so because both the parents felt that vaccination was only needed after sexual debut.
Knowledge and timing of vaccine dose schedule
More parents whose daughters completed the series were aware of the timing of the three dose vaccination schedule (n = 13, 46%)a than parents whose daughters did not complete the series (n = 4, 11%; p = 0.0017). In fact, only 57% (n = 21) parents in the Incomplete group were aware that three doses were required, and 7 participants (29%) incorrectly thought that they had already completed the vaccine series. However, overall knowledge about the timing of vaccine doses was poor in both groups, with 54% (n = 15) of parents in the Complete group and 89% (n = 33) in the Incomplete group being unsure or inaccurately reporting the vaccination schedule. Though only two parents (n = 7%) in the Complete group reported difficulty in obtaining all doses, only 43% (n = 12) in the Complete group reported finishing the series on time; 32% (n = 9) reported completing the series late, and 25% (n = 7) did not recall when the doses were given.
Providers' expectations for completion of the HPV vaccine series
Among the physicians (n = 24) and nurse practitioners (n = 3) that prescribe HPV vaccination for patients, plans for series completion included telling parents when the next doses were due but relying on parents to schedule appointments (52%), scheduling the second dose when the first dose was given (41%), and trying to immunize patients when they returned for other appointments (7%). Neither the inner-city public clinic nor the private practices had organized reminder or recall systems at the time of the study. Most patients scheduled nurse-only visits for second and third doses, and nursing schedules went out only 8–10 weeks, posing considerable logistical challenges for third dose scheduling. In the absence of standardized systems, individual providers used different approaches even within the same practices. Figure 2 compares parents' reasons for series non-completion with provider expectations for vaccine completion.
Expectation that parents will schedule appointment
A provider at the inner-city public clinic described his typical experience with follow-up: “We leave it to the parents, we tell them they have to come back in two months to get a second dose and they don't have to see the doctor but we can't really make a nurse visit. So parents have to call typically to get that visit and a large number of kids don't get their second dose on schedule. So it's pretty frequent that I would see a kid a year later [for the second dose].” He also described the limitations in implementation of electronic medical records, “even though we've had an EMR for 12 years, we don't have an easy-to-use reminder/recall system for patients.” This sentiment was echoed in the private practices: “We have a lot that forget their second one and they come in for their checkup next year.”
Scheduling the second dose at the time of the first vaccination
Providers described more success when the second dose was scheduled at when the first dose was given: “I find that being proactive about it and saying, ‘We're going to make you an appointment for you,’ or ‘We're going to call you to make this appointment,’ tends to be more effective [than telling them to make an appointment] for them actually completing the series in the time that it should be completed.” (Pediatrician, public clinic) Some intentionally scheduled additional follow-up appointments for other medical problems at the time when the second shot was due. Yet scheduling alone was imperfect: “So we schedule the second one at the time of the first. We don't schedule the third one because enough people don't show up for the second one that then you'd have this bogus third appointment scheduled which couldn't be done and it does clog up the nurse's schedule.” (Pediatrician, private practice) Nurses at the private practices who did see patients for second dose appointments discussed difficulties scheduling the third appointment because their schedules only went out two months.
Opportunistic vaccination
Providers described a lack of systems in place to ensure vaccine series completion: “We let the patients know, “You need to come back in two months for this vaccine you can book an appointment at the front desk.” From there. I don't know if they go on a list and they get called or if it's something that just gets dropped, I have no idea.” (Pediatrician, private practice) These providers relied on giving patients the next vaccine when they returned for a subsequent visit, but realized that competing priorities made this challenging: “when you're not busy occasionally [you review the immunization record] but I'd say in reality, most of us don't do that and we're busy.” (Pediatrician, private practice). Another provider added: “some of these HPV's are on the one year plan. You know, they get number two a year later, number three a year later.” (Pediatrician, private practice).
Providers' impressions of reasons why patients do not complete the HPV vaccine series
Similar to parents/guardians, providers also stated that most failures to complete were due to a lack of systems, not a conscious decision to stop the series: “I think I've only had like one patient ever [stop the series]. They just get busy. They forget. They don't schedule it.” (Pediatrician, private practice) Providers stated that completing the series was harder for older adolescents because they less often presented for care, and had more competing demands on their time: “The later teens, if for some reason they've pushed it off [are less likely to complete the series]. They're just busier with sports and school work and what not. Which is unfortunate because they are probably the ones who really need it to be done.” (Pediatrician, private practice) Of note, no providers stated that the need for three doses was a barrier to series completion. Clinic systems that providers stated could facilitate vaccine series completion included standing orders for second and third doses, walk-in appointments, and reminder cards with the due dates of each subsequent dose. Some practices had partially implemented some of these ideas.
Discussion
Most parents and guardians intended that their daughters complete the HPV vaccine series. However, 65% of parents/guardians expected to be reminded of any needed doses, while 52% of providers relied on parents to schedule subsequent shots. This finding is consistent with prior literature indicating that providers infrequently discuss series completion with their patients when recommending vaccination.17,18 No practice had a functional reminder/recall system that would provide a safety net for gaps in communication. Because medical practices frequently reach out to patients with appointment reminders and other information, many parents/guardians were expecting to be reminded of the timing of subsequent doses. Thus, reminder and recall systems may be effective for improving completion of the HPV vaccine series. Interventions with proven efficacy include phone calls, educational brochures, letters, and text messages.19-24 Many states support centralized immunization information systems or registries also provide useful tools for reminder and recall systems, and have also been shown to increase vaccination rates.25 Even practices with electronic medical record systems or access to state registries often find the implementation of reminder and recall systems very difficult. Another cost-effective option in states with highly functional immunization registries may be centralized reminder and recall systems where patients receive reminders directly from the state registry independent of individual medical practices.26 Many states support centralized immunization information systems or registries also provide useful tools for reminder and recall systems, and have also been shown to increase vaccination rates.25
The second reason most frequently cited by parents for not completing the series was inconvenience, specifically difficulty finding time in their busy schedules to make clinic appointments to complete the series. Providers agreed that busy schedules were a barrier, especially among older teens. Adolescents older than age 14 have fewer medical visits than younger adolescents, with an especially strong age-related decline in the number of preventive visits at which the need for immunizations is routinely reviewed.27 Alternative sites for vaccine delivery, such as schools and pharmacies, could be explored as means to increase completion of the three dose series. When considering alternative sites, however, care must be taken to ensure that all patients have access to the site regardless of their insurance status, and that systems are in place to ensure documentation and communication between primary care office and alternative sites to avoid over- or under-vaccinating patients.
Healthcare access is often cited as a reason for non-adherence to a variety of medical recommendations. However, study participants did not cite access as barrier to completing the vaccine series, specifically denying financial costs of the vaccine, transportation to the clinic, and the ability to cancel and reschedule medical appointments. This study took place in Massachusetts however, where universal healthcare has been in place since 2006, which may have overcome some access-related barriers. In states where access to primary care, including vaccination, is more limited, financial barriers may be more problematic. Studies in other areas have found significant relationships between out-of-pocket vaccine costs and rates of HPV vaccination.28-31
Only four of the 37 parents interviewed who did not complete the series made the conscious decision to stop the vaccination series. Reasons cited included a negative experience with a staff person, misconceptions regarding vaccine side effects, and lack of understanding of the reasons for vaccinating in advance of sexual debut. Of note, neither parents/guardians nor providers mentioned personal experiences with side effects as reasons why parents stopped the vaccine series. Many of the concerns voiced by parents could potentially be addressed by discussions with their providers. When providers treat questions and hesitation by parents as opportunities for education, vaccine hesitant parents are more likely to vaccinate.32-36 If hesitant parents are given the opportunity to voice their concerns and opinions, and the provider can address them systematically, the parents may be more likely to respond positively.33
Of note, no parent stated that the reason for non-completion of the series was the need for three doses, nor did any provider feel that reducing the number of doses would improve completion. Consideration is currently being given to reducing the vaccine schedule from three to two doses, and one of the reasons is to improve completion of the series. However, data from this study do not support that reducing the number of needed doses from three to two would improve completion rates, as neither parents nor providers felt that the need for three doses was a barrier to series completion.
Limitations
This analysis reports on a subset of previously described interviews.37 The strengths of this study include the use of interview data from both providers and parents, allowing for triangulation, the inclusion of interviewees from diverse racial/ethnic, socioeconomic, and linguistic backgrounds, and the use of multiple coders to conduct thematic content analysis. Failure to complete the three-dose series is an important public health problem because the effectiveness of incomplete dosing has not been established. This is the first study to our knowledge that has examined in depth the reasons for non-completion of the HPV vaccine series from the point of view of both parents and providers. We identified a previously-unidentified but remediable problem: patients expect clinic reminders when subsequent doses are due, but many healthcare systems are not providing this service. The institution of clinic-based or centralized reminder-recall systems thus may have the potential to substantially improve completion of the three dose series.
The limitations of this qualitative study include a small, non-random sample of parents/guardians from a single geographic area, and the inability to include interviews with teens. Another important limitation is the inability to identify race- and income-specific barriers to HPV vaccine series completion. Nationally, low-income and minority adolescents are less likely to complete the HPV vaccine series than white and affluent adolescents. In an effort to examine differences between these groups, we purposefully recruited equivalent numbers of parents whose daughters did and did not complete the series at both private practices and public clinics. This study design, which did not allow us to assess the magnitude of differences in completion rates between patients of different races or income levels, was chosen to allow us to identify distinct barriers among different racial and income groups. However, we found instead that similar reasons were cited by parents of all races and income levels who did not complete the series. Possible explanations of observed race and income disparities may include differences in healthcare systems with which the patients are interacting, or other unmeasured differences among the parents themselves, such as greater reliance on external reminders or more proactive advanced scheduling among parents of different races or income levels.
Conclusions
Most cases of non-completion of the HPV vaccine series are unintentional, usually resulting from parents expecting reminders from healthcare systems and providers expecting parents to schedule appointments. Therefore reminder and recall systems have great potential to improve completion rates, especially if implemented within a context of communication with patients and a team based approach. Other potential solutions include improved preventive care management of all patients within the medical home, better anticipatory guidance and/or consistent use of after visit summaries, and standardization of services provided by the staff giving the vaccine. Inconvenience, the second most common reason for not completing the series, could be addressed by improving access with better schedule management, walk-in hours, extended hours, and other interventions to strengthen the medical home.
Methods
Setting
Data for this study were collected in 2012–2013 at one inner-city public clinic serving low-income and minority patients and 3 sites (2 suburban, 1 urban) serving primarily white and relatively affluent patients. The inner-city public clinic cares for a diverse adolescent population including 48% Black, 26% Latino, 20% White and 6% other races. The private practice populations included 72% White, 12% Black, 5% Latino and 11% adolescents of other races. Eighty-four percent of patients at private practices had private insurance, compared with 25% at the inner-city public clinic. This study represents a subset of interviews previously analyzed to examine barriers to and facilitators of initiation of HPV vaccine series initiation.37
Participants
Parents/guardians whose daughters were between the ages of 11–17 years and had received at least one dose of HPV vaccine were eligible to participate. Parents/guardians were recruited when they accompanied their daughters to the clinic for preventive care or other problem-related visits. Trained research assistants reviewed practice schedules to determine eligible patients and recruited parents in the waiting areas either before or after scheduled visits. Because Black and Latino girls are less likely to complete the vaccine series, we oversampled parents/guardians who self-identified as Black and Latino. The subjects who identified themselves as African-American, Afro-Caribbean, Haitian, and African were classified as Black. The parent/guardian interviews were conducted in English, Haitian-Creole or Spanish. All the interviews were audio-recorded and then transcribed verbatim. Native speakers transcribed the Haitian-Creole and Spanish interviews, which were then translated to English and then back translated to validate accuracy. Parents/guardians received $20 gift cards for participation. We recruited physicians, nurse practitioners, and registered nurses who provided primary care including HPV vaccination at the inner-city public clinic and private practices. At each clinical site, a physician involved in the study recruited additional providers. The providers were not compensated. The Institutional Review Boards of Boston University Medical Campus and Harvard Vanguard Medical Associates approved this study.
Interviews were designed to elicit reasons why girls who started the HPV vaccine series did or did not complete all three shots from the point of view of both parents/guardians and providers. Review of the medical record was conducted for all subjects to confirm the number of shots received. Parent/guardian interviews elicited demographic information, vaccination status, perceptions related to parent-provider communication, and reasons for completing or failing to complete the HPV vaccine series. Provider interviews elicited practices that facilitated or hindered series completion. All interviews were coded by three to six researchers, and discrepancies were discussed to achieve consensus. Consistent with the methods of qualitative analysis, we used the data to generate codes that were revised following every coding meeting and recurring themes were identified. When multiple reasons for series non-completion were mentioned, transcripts were reviewed again by two researchers to determine the primary reasons for failure to complete the series. Parent/guardian answers were compared across race/ethnicity, socioeconomic status, and practice settings (inner-city public clinic or private practice), to determine differences in primary reasons for completing or not completing vaccination. Provider responses were assessed to determine common themes that facilitated or hindered completion.
Abbreviations
- HPV
Human Papillomavirus
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
This work is supported by American Cancer Society Mentored Research Scholar Grant (MRSG-09-151-01), and Centers for Disease Control and Prevention Cooperative Agreement (1UO1IP000636). After this study was completed, Dr. Pierre-Joseph received the following award: Integrating HPV vaccination Promotion Initiative with Cervical Cancer Screening and Preventive Initiatives in Primary Care, Award#: 53261, unrestricted educational grant from Merck & Co.
Note
The question to elicit parental knowledge of dose timing was open-ended, eliciting a variety of responses. Responses were considered correct if parents noted that three doses were needed within a six month time period.
Funding
This work is supported by American Cancer Society Mentored Research Scholar Grant (MRSG-09-151-01), and Centers for Disease Control and Prevention Cooperative Agreement (1UO1IP000636). No commercial support was obtained.
References
- [1].ACIP Quadrivalent Human Papillomavirus Vaccine Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Moral Wkly Rep 2007:56 http://origin.glb.cdc.gov.ezproxy.bu.edu/MMWR/preview/mmwrhtml/rr5602a1.htm. Accessed September15, 2014 [PubMed] [Google Scholar]
- [2].ACIP . FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2010; 59:626-9; PMID:2050859s3 [PubMed] [Google Scholar]
- [3].Joura EA, Giuliano AR, Iversen OE, Bouchard C, Mao C, Mehlsen J, Moreira ED Jr, Ngan Y, Petersen LK, Lazcano-Ponce E, et al.. A 9-valent HPV vaccine against infection and intraepithelial neoplasia in women. N Engl J Med 2015; 372(8):711-23; PMID:25693011; http://dx.doi.org/ 10.1056/NEJMoa1405044 [DOI] [PubMed] [Google Scholar]
- [4].Markowitz LE, Hariri S, Lin C, Dunne EF, Steinau M, McQuillan G, Unger ER. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. J Infect Dis 2013; 208(3):385-93; PMID:23785124; http://dx.doi.org/ 10.1093/infdis/jit192 [DOI] [PubMed] [Google Scholar]
- [5].Niccolai LM, Julian PJ, Meek JI, McBride V, Hadler JL, Sosa LE. Declining rates of high-grade cervical lesions in young women in Connecticut, 2008–2011. Cancer Epidemiol Biomarkers Prev 2013; 22(8):1446-50; PMID:23704476; http://dx.doi.org/ 10.1158/1055-9965.EPI-13-0272 [DOI] [PubMed] [Google Scholar]
- [6].Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, Curtis RC, Markowitz L. Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006–2014 - United States. MMWR Morb Mortal Wkly Rep 2014; 63(29):620-4. http://www.ncbi.nlm.nih.gov/pubmed/25055185; PMID:25055185 [PMC free article] [PubMed] [Google Scholar]
- [7].Gertig DM, Brotherton JML, Budd AC, Drennan K, Chappell G, Saville AM. Impact of a population-based HPV vaccination program on cervical abnormalities: a data linkage study. BMC Med 2013; 11:227; PMID:24148310; http://dx.doi.org/ 10.1186/1741-7015-11-227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Herweijer E, Leval A, Ploner A, Eloranta S,Simard JF, Dillner J, Netterlid E, Sparén P, Arnheim-Dahlström L. Association of varying number of doses of quadrivalent human papillomavirus vaccine with incidence of condyloma. JAMA 2014; 311(6):597-603; PMID:24519299; http://dx.doi.org/ 10.1001/jama.2014.95 [DOI] [PubMed] [Google Scholar]
- [9].Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, et al.. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 2009; 374(9686):301-14; PMID:19586656; http://dx.doi.org/ 10.1016/S0140-6736(09)61248-4 [DOI] [PubMed] [Google Scholar]
- [10].Group F. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N Engl J Med 2007; 356(19):1915-27; PMID:17494925; http://dx.doi.org/ 10.1056/NEJMoa061741 [DOI] [PubMed] [Google Scholar]
- [11].Pomfret TC, Gagnon JM, Gilchrist AT. Quadrivalent human papillomavirus (HPV) vaccine: a review of safety, efficacy, and pharmacoeconomics. J Clin Pharm Ther 2011; 36(1):1-9; PMID:21198715; http://dx.doi.org/ 10.1111/j.1365-2710.2009.01150.x [DOI] [PubMed] [Google Scholar]
- [12].SEER Stat Fact Sheets: Cervix Uteri Cancer. http://seer.cancer.gov/statfacts/html/cervix.html. Published 2013 [Google Scholar]
- [13].Cook RL, Zhang J, Mullins J, Kauf T, Brumback B, Steingraber H, Mallison C. Factors Associated With Initiation and Completion of Human papillomavirus vaccine series among young women enrolled in medicaid. J Adolesc Heal 2010; 47(6):596-9; http://dx.doi.org/ 10.1016/j.jadohealth.2010.09.015 [DOI] [PubMed] [Google Scholar]
- [14].Widdice LE, Bernstein DI, Leonard AC, Marsolo KA, Kahn JA. Adherence to the HPV vaccine dosing intervals and factors associated with completion of 3 doses. Pediatrics 2011; 127(1):77-84; PMID:21149425; http://dx.doi.org/ 10.1542/peds.2010-0812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kester LM, Zimet GD, Fortenberry JD, Kahn JA, Shew ML. A national study of HPV vaccination of adolescent girls: rates, predictors, and reasons for non-vaccination. Matern Child Health J 2013; 17(5):879-85; PMID:22729660; http://dx.doi.org/ 10.1007/s10995-012-1066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kouyoumdjian FG, Bailowitz A. Completion of the human papillomavirus vaccine series in females attending an urban immunization clinic. Pediatr Infect Dis J 2011; 30(8):718-9; PMID:21343841; http://dx.doi.org/ 10.1097/INF.0b013e3182121426 [DOI] [PubMed] [Google Scholar]
- [17].Alexander AB, Stupiansky NW, Ott MA, Herbenick D, Reece M, Zimet GD. Parent-son decision-making about human papillomavirus vaccination: a qualitative analysis. BMC Pediatr 2012; 12(1):192; PMID:23241217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Alexander AB, Best C, Stupiansky N, Zimet GD. A model of health care provider decision making about HPV vaccination in adolescent males. Vaccine 2015; 33(33):4081-6; PMID:26143612 [DOI] [PubMed] [Google Scholar]
- [19].Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA. Effect of Patient Reminder / Recall Interventions on Immunization Rates A Review. J Am Med Assoc 2014; 284(14):1820-7 [DOI] [PubMed] [Google Scholar]
- [20].Cassidy B, Braxter B, Charron-Prochownik D, Schlenk EA. A quality improvement initiative to increase HPV vaccine rates using an educational and reminder strategy with parents of preteen girls. J Pediatr Health Care 2014; 28(2):155-64; PMID:23522561 [DOI] [PubMed] [Google Scholar]
- [21].Chao C, Preciado M, Slezak J, Xu L. A randomized intervention of reminder letter for human papillomavirus vaccine series completion. J Adolesc Health 2015; 56(1):85-90; PMID:25438965 [DOI] [PubMed] [Google Scholar]
- [22].Kharbanda EO, Stockwell MS, Fox HW, Andres R, Lara M, Rickert VI. Text message reminders to promote human papillomavirus vaccination. Vaccine 2011; 29(14):2537-41; PMID:21300094 [DOI] [PubMed] [Google Scholar]
- [23].Matheson EC, Derouin A, Gagliano M, Thompson JA, Blood-Siegfried J. Increasing HPV Vaccination Series Completion Rates via Text Message Reminders. J Pediatr Health Care 2014; 28(4):e35-9; PMID:24200295 [DOI] [PubMed] [Google Scholar]
- [24].Stockwell MS, Kharbanda EO, Martinez RA, Lara M, Vawdrey D, Natarajan K, Rickert VI. Text4Health: impact of text message reminder-recalls for pediatric and adolescent immunizations. Am J Public Health 2012; 102(2):e15-21; PMID:22390457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Groom H, Hopkins DP, Pabst LJ, Murphy Morgan J, Patel M, Calonge N, Coyle R, Dombkowski K, Groom AV, et al.. Immunization Information Systems to Increase Vaccination Rates: A Community Guide Systematic Review. J Public Health Manag Pract 2014; 97227:1-22 [DOI] [PubMed] [Google Scholar]
- [26].Kempe A, Saville AW, Dickinson LM, Beaty B, Eisert S, Gurfinkel D, Brewer S, Shull H, Herrero D, Herlihy R. Collaborative centralized reminder/recall notification to increase immunization rates among young children: a comparative effectiveness trial. JAMA Pediatr 2015; 169(4):365-73; PMID:25706340 [DOI] [PubMed] [Google Scholar]
- [27].Rand CM, Shone LP, Albertin C, Auinger P, Klein JD, Szilagyi PG. National health care visit patterns of adolescents: implications for delivery of new adolescent vaccines. Arch Pediatr Adolesc Med 2007; 161:252-9; PMID:17339506 [DOI] [PubMed] [Google Scholar]
- [28].Conroy K, Rosenthal SL, Zimet GD, Jin Y, Bernstein DI, Glynn S, Kahn JA. Human Papillomavirus Vaccine Uptake, Predictors of Vaccination, and Self-Reported Barriers to Vaccination. J Women's Heal 2009; 18(10):1679-86 [DOI] [PubMed] [Google Scholar]
- [29].Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health 2014; 14(1):700; PMID:25004868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pourat N, Jones JM. Role of Insurance, Income, and Affordability in Human Papillomavirus Vaccination. Am J Manag Care 2012; 18(6):320-30; PMID:22775000 [PubMed] [Google Scholar]
- [31].Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: a systematic review. Prev Med (Baltim) 2014; 58:22-32 [DOI] [PubMed] [Google Scholar]
- [32].Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics 2008; 122(4):718-25; PMID:18829793; http://dx.doi.org/ 10.1542/peds.2007-0538 [DOI] [PubMed] [Google Scholar]
- [33].Opel DJ, Heritage J, Taylor JA, Mangione-Smith R, Salas HS, Devere V, Zhou C, Robinson JD. The architecture of provider-parent vaccine discussions at health supervision visits. Pediatrics 2013; 132(6):1037-46; PMID:24190677; http://dx.doi.org/ 10.1542/peds.2013-2037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Fredrickson DD, Davis TC, Arnold CL, Kennen EM, Hurniston SG, Cross JT, Bocchini JA Jr. Childhood Immunization Refusal: Provider and Parent Perceptions. Fam Med 2004; 36(6):431-9; PMID:15181556 [PubMed] [Google Scholar]
- [35].Healy CM, Pickering LK. How to communicate with vaccine-hesitant parents. Pediatrics 2011; 127 Suppl (May 2011):S127-33; PMID:21502238; http://dx.doi.org/ 10.1542/peds.2010-1722S [DOI] [PubMed] [Google Scholar]
- [36].Smith PJ, Kennedy AM, Wooten K, Gust DA, Pickering LK. Association between health care providers' influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics 2006; 118(5):e1287-92; PMID:17079529; http://dx.doi.org/ 10.1542/peds.2006-0923 [DOI] [PubMed] [Google Scholar]
- [37].Perkins RB, Clark JA, Apte G, Vercruysse JL, Sumner JJ, Wall-Haas CL, Rosenquist AW, Pierre-Joseph N. Missed opportunities for HPV vaccination in adolescent girls: a qualitative study. Pediatrics 2014; 134(3):e666-74; PMID:25136036; http://dx.doi.org/ 10.1542/peds.2014-0442 [DOI] [PubMed] [Google Scholar]


