Abstract
Background:
Stature lengthening in skeletal dysplasia is a contentious issue. Specific guidelines regarding the age and sequence of surgery, methods and extent of lengthening at each stage are not uniform around the world. Despite the need for multiple surgeries, with their attendant complications, parents demanding stature lengthening are not rare, due to the social bias and psychological effects experienced by these patients. This study describes the outcome and complications of extensive stature lengthening performed at our center.
Materials and Methods:
Eight achondroplasic and one hypochondroplasic patient underwent bilateral transverse lengthening for tibiae, humeri and femora. Tibia lengthening was carried out using a ring fixator and bifocal corticotomy, while a monolateral pediatric limb reconstruction system with unifocal corticotomy was used for the femur and humerus. Lengthening of each bone segment, height gain, healing index and complications were assessed. Subgroup analysis was carried out to assess the effect of age and bone segment on the healing index.
Results:
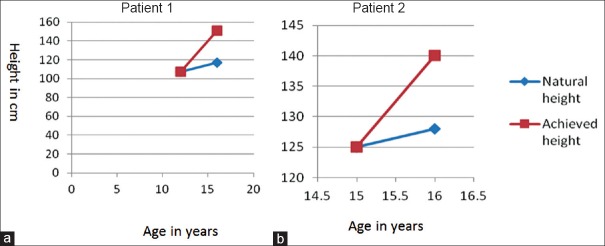
Nine patients aged five to 25 years (mean age 10.2 years) underwent limb lengthening procedures for 18 tibiae, 10 femora and 8 humeri. Four patients underwent bilateral lengthening of all three segments. The mean length gain for the tibia, femur and humerus was 15.4 cm (100.7%), 9.9 cm (52.8%) and 9.6 cm (77.9%), respectively. Healing index was 25.7, 25.6 and 20.6 days/cm, respectively, for the tibia, femur and humerus. An average of 33.3% height gain was attained. Lengthening of both tibia and femur added to projected height achieved as the 3rd percentile of standard height in three out of four patients. In all, 33 complications were encountered (0.9 complications per segment). Healing index was not affected by age or bone segment.
Conclusion:
Extensive limb lengthening (more than 50% over initial length) carries significant risk and should be undertaken only after due consideration.
Keywords: Ilizarov, limb reconstruction, short stature, skeletal dysplasia, stature lengthening
MeSh terms: Achondroplasia, bone lengthening, ilizarov technique, complications
INTRODUCTION
Short stature is defined as height less than the third percentile for chronological age.1 Achondroplasia is the most common skeletal dysplasia causing disproportionately reduced stature with rhizomelic short limbs.1,2 Societal prejudices extend to short stature and may cause psychological disturbance, mostly in early adolescence but also in childhood.3,4,5 In addition, it has been shown that achondroplastic children are more dependent on their parents.4 Extensive limb lengthening has to be considered in order to increase height at maturity in affected individuals6 and more significantly to restore normal body proportions.6,7,8 On average, this requires 25–30 cm lengthening of the lower limbs.8,9
The literature suggests that lengthening is achieved at great cost.10 It has mostly been performed in the older age group, usually adolescents, when the child's assent is possible, but the ability to adapt and change body image is limited.5,10,11,12,13,14,15 There are several accounts of limb lengthening for short stature in children, most reporting a significant complication rate.3,5,6,8,10,11,12,13,16,17,18,19,20,21 Pin site infections, poor regenerate, delayed consolidation, nonunion at the regenerate, joint contracture, joint deformity, subluxation, articular cartilage damage, stiffness and neurological and vascular compromise were some of the complications encountered in these series.3,16,18,20,22,23 Many of these complications are related to tissue compliance.6,16,22
In achondroplasia, endochondral ossification at bone ends is deficient but periosteal bone formation occurs normally.1 Skin, muscles and neurovascular structures develop normally or in excess.1,17 In this study, we have explored the use of long limb lengthening in achondroplasia and hypochondroplasia and analyzed the complications related to massive single stage lengthening in children treated by us. We have observed that though such children require bilateral lengthening close to 100% of their initial bone length, paradoxically, there are less complications and the regenerate takes less time to consolidate when compared to lengthening done for other nontraumatic indications such as congenital limb deficiencies and infections.
MATERIALS AND METHODS
This retrospective study was approved by our Institutional Review Board and follows the latest revision of the declaration of Helsinki. Nine patients (eight achondroplasia and one hypochondroplasia) who underwent stature lengthening in our unit between the years 2001 and 2013 were identified from inpatient records. Following informed written consent, all had undergone surgery for the same under the supervision of a single consultant orthopedic surgeon. Clinical details and radiographs were obtained from stored clinical records, computerized Hospital Information Processing Service and picture archiving and communication system. The presenting complaints, their duration, age and height at presentation, age at surgery for each segment, gender, bone involved, side of involvement and previous treatment (if any) were recorded. Complications and events affecting the outcome were extracted. Serial radiographs were assessed and the following noted: (a) Lengthening device, (b) Segment lengthened, (c) Duration of lengthening and time to removal of frame and (d) Amount of lengthening achieved per surgery.
Radiographs at presentation and the last followup were retrospectively compared for: (a) Extent of healing and (b) correction or worsening of the deformity following surgery. At each followup, the children were clinically examined for pain, deformity, range of movements of knee and ankle and limb length discrepancy and their radiographs analyzed for deformity and angular correction.
Except for a single child whose humeri were lengthened in succession, all patients underwent simultaneous bilateral transverse lengthening of affected bones. In patients, who underwent multiple segment lengthening, the tibiae, humeri and femora were lengthened in that order except for one child who underwent femur lengthening second on request and another for whom the sequence was femur followed by tibia.
For tibia lengthening, a ring fixator with 3 rings construct was used and bifocal corticotomy at the diaphyseo-metaphyseal junction was done. One centimeter of the fibula was excised from the mid-diaphysis. Corticotomy was performed subperiosteally, with multiple drill holes through an anterior approach and completed with an osteotome. The proximal ring was applied parallel to the knee joint, distal ring parallel to the ankle joint and the middle ring perpendicular to the diaphysis. The periosteum was closed with care afterward. All patients underwent foot frame application after initial distraction at variable times, usually one month [Figure 1]. Proximal tibiofibular wires were added at the time of foot frame application once fibula came down to the appropriate level.
Figure 1.

Radiographs (a-f) depict the lengthening started at age 5 and completed at age 10. (a) Three ring Ilizarov frame with bifocal corticotomy of tibia. (b) Frame is extended to the feet, and the proximal tibiofibular wire is added after fibula has descended to the appropriate level. (c) Tibia awaiting consolidation. (d) Humerus lengthening of 8 cm is carried out. (e) Finally, lengthening of the femur was carried out. (f) After 9 cm of lengthening at the femur and 20 cm of lengthening in the tibia. Note the medial ankle epiphysiodesis bilaterally to correct ankle valgus at age 11 years
For femur and humerus lengthening, a monolateral pediatric limb reconstruction system (Orthofix, Verona, Italy) was used, with mid-diaphyseal corticotomy for the humerus and distal diaphyseo-metaphyseal junction corticotomy for the femur. The iliotibial band was divided prophylactically while doing corticotomy of the femur to prevent the valgus and flexion deformity at the knee.9 The radial nerve was exposed and identified before distal pin placement in the humerus.
Distraction was started after the 5th postoperative day either in ward or in outpatient setting, using four 0.25 mm turns at each corticotomy site per day in order to achieve a daily increment of 1 mm. The mean duration of admission was about 5 days for each surgery. Planned lengthening was 15 cm for the tibia, 8 cm for the femur and 10 cm for the humerus. All joints were carefully observed clinically and radiologically for any signs of subluxation or deformity. The regular range of motion physiotherapy was carried out for the adjacent joints especially the knee. The regenerate was allowed to consolidate. The decision to remove the external fixator was taken after three cortices were seen in the regenerate in antero-posterior and lateral X-rays. All bony segments were protected for 4–6 weeks by patella tendon bearing casts for the legs and functional casts for the femur and humerus.
The healing index was expressed as the days of external fixator application per centimeter of lengthening of each bone.10,24 Bone lengthening was calculated by dividing the total length gained by the initial length of the bone segment and expressed as a percentage. The percentage of height gain was also calculated similarly. Paley tables were used to predict final height at skeletal maturity.25 The predicted height was added to the length achieved in the limb to assess final predicted height in those children who had not achieved maturity.
Complications and pin tract infections were classified as per Donnan et al.26
RESULTS
Nine patients (seven girls and two boys) underwent lengthening of 36 long bone segments (18 tibiae, 10 femora and 8 humeri). The mean age at the time of first surgery was 10.2 years (range 5–25 years; standard deviation [SD] 6.6). Eight children and one adult underwent bilateral tibia lengthening; five children had bilateral femur and four children had bilateral humerus lengthening. Four children underwent lengthening of all three long bone segments, that is, tibia, femur and humerus.
A total of 48 surgical interventions were performed for 36 segments in nine patients (5.3 per child) which included primary surgeries for bone lengthening, implant exits under anesthesia as day-care procedures and interventions for management of complications.
The mean followup was 58.5 months (range 1–11.5 years). Five out of nine patients continue to be followed up. Three of these children have finished all three segments lengthening.
Tibia lengthening
Nine patients underwent lengthening for 18 tibiae. The mean preoperative tibia length was 15.8 cm (range 12.5–23 cm; SD 3.3) which was lengthened to a postoperative average of 31.3 cm (range 25.5–40 cm; SD 5.5) thereby achieving a mean tibia length gain of 15.4 cm (range 7–22 cm; SD 3.8). The average percentage of lengthening achieved from initial tibial length was 100.7% (range 67.3–153%; SD 29.5) [Table 1]. The mean healing index for the tibia was 25.7 days/cm of lengthened bone (range 13.45–40.33 days/cm; SD 8.3).
Table 1.
Patient wise details of length achieved for each segment and final height achieved
The mean lengthening achieved at the proximal tibial corticotomy site was 7.6 cm (range 4–11.2 cm; SD 1.9), with a mean healing index of 49.8 days/cm (range 28.03–86.4 days/cm; SD 15.9). The average lengthening at the distal tibial corticotomy site was 7.7 cm (range 3.4–11.3 cm; SD 2.8), with a mean healing index of 49.7 days/cm (range 26.5–76.5 days/cm; SD 14.3). The difference in the healing indices was not significant by the unpaired t-test (P = 0.8).
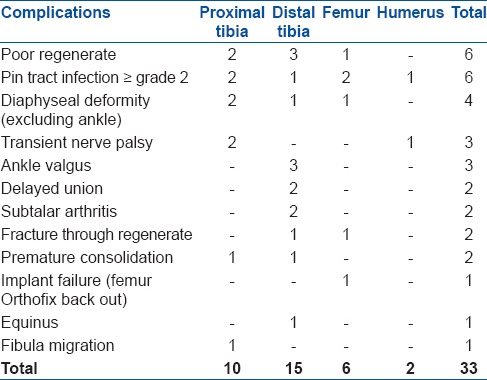
A total of 25 complications were encountered [Table 2], 10 attributed to the proximal lengthening site and 15 to the distal site. The difference in the number of complications between the two tibial sites failed to reach statistical significance (P = 0.08) using Fisher's t-test.
Table 2.
Distribution of complications encountered during lengthening procedure
Femur lengthening
Five children underwent a total of 10 femoral lengthening at a mean age of 8.7 years (range 5–14 years; SD 2.5). The mean preoperative length was 19.09 cm (range 14.7–26 cm; SD 4.3) and average final postoperative length 28.9 cm (range 23.8–38 cm; SD 5.3). The mean lengthening achieved was 9.9 cm (range 8–12 cm; SD 1.4) amounting to 52.8% (range 38.6–63.5%; SD 9.6) of the original length [Table 1]. The mean healing index was 25.6 days/cm (range 18.1–31.6 days/cm; SD 5.4). Six complications were encountered during lengthening [Table 2].
Humerus lengthening
Eight humeri were lengthened in 4 children at a mean age of 8.8 years (range 7–13 years; SD 2.8). The mean initial length was 12.3 cm (range 10.8–13 cm; SD 0.9) and the average postoperative length was 21.9 cm (range 19.1–24 cm; SD 0.94). The mean achieved length gain was 9.6 cm (range 8.2–11 cm; SD 0.9) which, in percentage terms, was 77.9% (range 69.2–84.6%; SD 6.4) [Table 1]. The mean healing index was 20.6 days/cm (range 16.2–6.5 days/cm; SD 5.06). Humerus lengthening was relatively uneventful, with only 2 complications.
Height gain
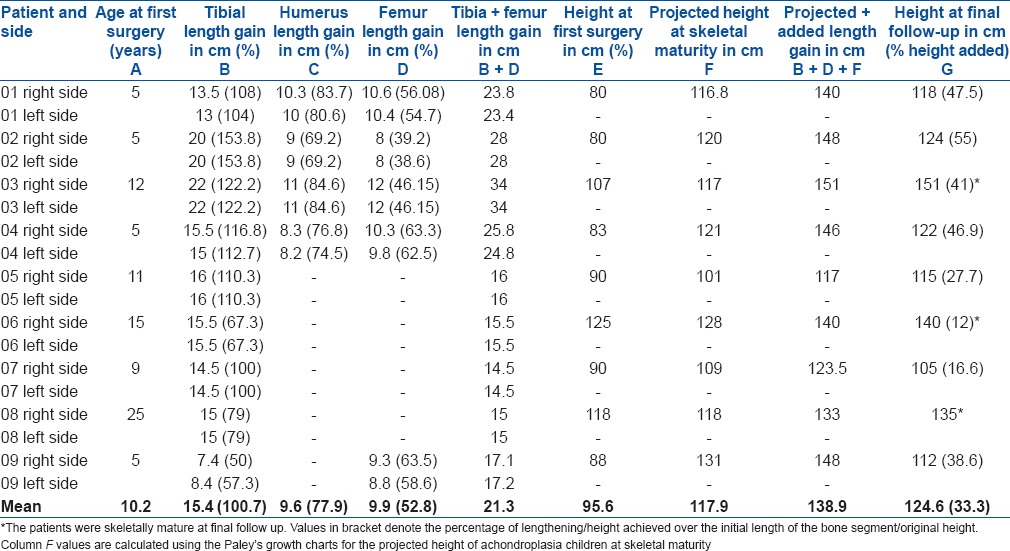
The mean height added over the initial stature was 33.3% (range 11.3–55%; SD 15.1) [Table 1]. Postoperative height in all children exceeded the predicted height calculated by Paley's charts, except for two children who each underwent only femur and tibia lengthening [Figure 2].
Figure 2.
The heights achieved with (a) both tibial and femoral and (b) tibial lengthening are compared. In (a) by lengthening of 22 cm in tibia and 12 cm in femur between ages of 11 and 16 a final height of 151 cm (between 10th and 25th percentile) was achieved. In (b) by tibial lengthening of 15.5 cm, a final height of 140 cm <3rd percentile of Indian standard was achieved
Range of motion at joints
Complete data for range of movements of joints was available for eighteen segments in six children. Hip range of motion was unchanged in all patients except one child while undergoing femur lengthening who had bilateral 20° flexion deformity of hip and another two children had 30° flexion deformity at the knee initially. All three recovered full extension with physiotherapy at the completion of treatment the respective bony segment. All our patients underwent application of ring foot frame in the neutral position after initial distraction. After completion of lengthening of the tibia, one patient eventually had 20° equinus which was treated with tendo achilles lengthening. Two children had bilateral absent dorsiflexion but walked plantigrade and three others had dorsiflexion limited to 20°. All four patients, in whom humerus lengthening was carried out, had preoperative bilateral elbow flexion deformity of 30–45°. This improved to 20° fixed elbow flexion deformity in two children. Further flexion was normal. Shoulder range of motion remained unchanged throughout the process of lengthening.
Complications
There were a total of 33 complications for 36 segments (0.9 per segment) [Table 2]. According to the Donnan system of classification of complications in limb lengthening, 17 were Grade II and 10 fell into Grade III. Poor regenerate and delayed union were managed with bone marrow injection and bone grafting in four cases each. Transient palsies were seen in two patients; one had radial and the other had bilateral common peroneal nerves affected. These recovered spontaneously in a few days. None of patients underwent prophylactic release of common peroneal nerve. One proximal tibia valgus and bilateral ankle valgus were managed with growth modulation using eight plate and medial malleolus screw epiphysiodesis, respectively. Delayed equinus in one child was managed with tendo achilles lengthening. Of the two regenerate fractures, one (in the femur) was managed with continuation of an above knee cast while the other, in the tibia, required revision of fixation using a monolateral external fixator (Orthofix). Two premature consolidations needed revision corticotomy.
Donnan Grade 1 pin tract infections were commonly seen, especially in the tibia. Four Grade 2 infections were managed with oral antibiotics, one Grade 3 infection with intravenous antibiotics and one Grade 4 with pin exchange.
Subgroup analysis – age versus healing index
The mean healing index for all 3 segments, for children who were <10 years old, was 22.5 days/cm (n = 20, SD 4.9) while the same was 26.6 days/cm (n = 14, SD 9.7) for those aged 10 or more. No statistical significance was found between these two groups with the unpaired t-test (P = 0.1).
Subgroup analysis – bony segment versus healing index
No statistically significant difference was found when the healing indices of the tibia (25.7 days/cm), humerus (20.6 days/cm) and femur (25.6 days/cm) were compared using the one-way ANOVA test.
Subgroup analysis – complications
Of the 33 complications, 25 were related to tibia lengthening (1.3 per segment) while femur and humerus lengthening had 6 (0.6 per segment) and 2 (0.2 per segment) complications, respectively. Complications related to lower limb lengthening (proximal tibia, distal tibia, femur) were significantly more than those for lengthening of the humerus (P = 0.01).
DISCUSSION
Children with short limbed skeletal dysplasia face difficulties in their daily activities such as comfortable sitting and optimal use of public transport and furniture in schools and workplaces.10 This is more so in developing countries, where disabled friendly facilities are lacking and buildings, furniture, transport and other public infrastructure are designed for normal physiological proportions.
Common dysplasias treated with limb lengthening are achondroplasia and hypochondroplasia, both have similar pathoanatomy but differing severity and are caused by fibroblast growth factor receptor-3 mutation.1 Many reports of limb lengthening include both syndromes in their patient population and advocate common recommendations.10,13,18,27 The surgeon is expected to have a clear understanding of the pathology, disproportion requiring correction and the ability to avoid and deal with complications, despite a steep learning curve.23 Although an established procedure in a few centers in the world, there are no published reports on this form of treatment from India and Southeast Asia and the present study is the first from our region.3,9,10 This small series of only 9 such children, recovered from a period of over 11 years in a tertiary center, indicates how rarely the requirements for such a difficult task are met.
Different strategies in achondroplasia include simultaneous bilateral, transverse, longitudinal and crossed lengthening of tibia and femur.8,9,10,28,29 The transverse lengthening is preferred by us as it leaves the decision regarding lengthening of other segments in the hands of patients. A transverse approach allows lengthening to be stopped at any point during treatment. Besides giving the patient a choice, transverse lengthening, also has the advantage of being symmetrical with both knees at the same level at any time point.
To obtain patient assent, many centers have delayed lengthening till 12 years of age.8,10,11,12,14,30 Completing treatment before puberty does not affect social maturity and educational milestones.8,9 In addition, younger children are easier to transport and manage because of their smaller size and weight. In our series half of those above ten years of age abandoned subsequent lengthening because it affected their academic schedule. In another child shift of residence to the hospital's city was required to continue schooling. In 80% of those, whose lengthening was started before ten years of age, all segment lengthening could be completed. This data suggests that older children have difficulty with long treatment duration.
According to Herzenberg and Paley, starting lengthening before ten years of age has an additional advantage of allowing staggering of the process into two episodes of shorter lengthening instead of a single extensive procedure, thereby reducing the complications further.28 This recommendation was not followed in our patients.
The velocity of distraction and consolidation of the regenerate depend on the age of the patient and the bone segment, and the healing index has traditionally been used to assess these aspects.10 Others have found the average healing index for achondroplastic children to range from 26.06 to 48 days/cm for various bone segments.16,18 In this study, despite length gain of up to 153.8% of initial bone segment length, the healing index averaged 23.65 days/cm for the tibia. Initiation of lengthening at an early age and bifocal tibial corticotomy allowed more than 100% lengthening without a significant increase in the number of complications. A noteworthy proportion of the latter are deformities around the ankle and distal corticotomy site.
Disproportionate short upper limbs significantly affect activity of daily living, more so, after following appreciable lengthening of lower segments.10,31 Therefore, it is important to consider bilateral humerus lengthening for functional reasons. Healing index and total fixator time are noticeably lower for the humerus when compared to the lower limb segments.17,31 Complications like radial nerve palsy are generally transient and best avoided using a monolateral fixator and identifying the radial nerve before putting the pins.17 We found humerus lengthening to be the easiest and least troublesome for children who were able to continue with schooling and social activities while on a bilateral humerus frame.
We preferred to sandwich humerus lengthening between that of the tibia and femur. This sequence has the advantage of providing time for function and bone remodeling in the lower limb segment lengthened. In addition, upper limb lengthening allows for the greater reach of the taller child [Figure 3].
Figure 3.

Clinical photographs before and after lengthening of the 11-year-old boy show the change in body proportion after lengthening and its effect on activities of daily living. (a) At 5 years, upper to lower segment ratio of 3.3 exaggerated by the presence of genu varum and hands reach the greater trochanters. (b) At age 11, after femoral and tibial lengthening, the ratio is 1.05, and the lengthened arms reach mid-thigh. (c) Child can sit on a normal chair with feet touching the ground and (d) He is able to board a school bus ed
One of the major issues in stature lengthening for achondroplasia is a disproportion between the upper and lower body segments.2,7 For children of average stature, the ratio of upper to lower body segments is 1.4 at birth, a figure that decreases to 1.0 by 10 years of age.7 For children with achondroplasia, the 50th percentile of this ratio is 2.0, which reduces to only 1.7 at skeletal maturity.7 While increasing stature, correction of this disproportion also requires consideration. Aldegheri and Dall’Oca despite adding an average of 20.5 cm to the lower limb length could not restore normal body proportions.10 In our study, eventual body proportion has not yet been calculated in all subjects, as not all have attained skeletal maturity.
Desired stature correction depends on ethnicity and local standards for stature. The overall goal should be to achieve a final height above the 3rd percentile. Standard 3rd percentile height is 148.3 cm for Indian girls and 161 cm for boys.32 In our study, predicted heights (by Paley's chart and length added by surgeries) for five children who completed both long segments of the lower limbs were 140, 151 and 146 cm for 3 girls and 148 cm each for two boys. These figures are close to the 3rd percentile height for our population [Table 1, Figures 2 and 3].
Extensive lengthening defined as more than 50% lengthening of any bone segment has many complications. Using Donnan's classification to grade our complications, because of its applicability to monolateral fixators, our complication rate of 0.9 per segment for an average of 21.3 cm length (range 14.5–34 cm; SD 7) was comparable to other similar studies [Table 1]. Kim et al. had 123 complications for 88 long bone segments in 22 achondroplastic children who underwent 10.21 cm femur and 9.13 cm tibia lengthening.3 Aldegheri and Dall’Oca noted a complication rate of 43.5% for lower limb lengthening with average length gain of 16.7 cm.10 Vaidya et al. had 46 complications for 47 tibia lengthened with an average gain of 6.8 cm.16 Lie et al. found a complication rate of 0.6 per bone segment which is very low compared to other series.18 However, their mean length gain of only 5.2 cm per segment in 8 patients is insufficient to have developed significant complications, which are normally associated with lengthening of greater than 6 cm.18
Most of our complications were in the distal tibial segments and related to poor regenerate, delayed union and re-fracture. Based on this, we now feel that after the initial stage, lengthening of the distal tibia should be slowed to avoid complications.
Hip instability and knee contractures are common complication in limb deficiencies.16,21,22,27,28 In achondroplasia, however, the soft tissue is normal and acetabular roof flat therefore except at the terminal part of lengthening, the soft tissue tension does not give rise to these complications.1,6,9,16,33,34 Some angular deformities around the knee can be avoided by intraoperative measures such as transfixing the proximal tibiofibular joint, gastroc-soleus recession and severance of the iliotibial band.8,9,28 Noonan et al. have reported significantly lower rate of joint-related complications in limb lengthening in achondroplasia compared to other causes of limb length discrepancies (0.008 vs. 0.02 complications per cm of limb lengthening, P = 0.04).33 Venkatesh et al. found no hip subluxation in their achondroplasia patients.6 In our analysis, there were no instances of hip and knee joint subluxation or dislocation supporting the previous observations on lengthening in achondroplasia.
The risk of reduction in the range of movement of joints in our patients was similar to the previous reports.6,16 Knee and hips regained full range of movement while ankles did show restricted dorsiflexion with one child needing intervention for equinus deformity. Vaidya et al. have reported equinus deformity in all patients undergoing >40% tibial lengthening.16 Venkatesh et al. considered the knee contractures were related to lateral pin placement and greater magnitude of lengthening.6 This however, was not an issue in our study as a circular ring fixator was used.
An unusual complication in our study was a distal migration of the fibula due to the early consolidation of the fibula osteotomy with no effect on the course of treatment or peroneal nerve dysfunction. Galardi et al. have found a clear relationship between the amount of tibial lengthening and subclinical common peroneal nerve neurophysiological abnormality.35 This is in contrast to Polo et al. who found no correlation in a similar situtation.36 Prophylactic common peroneal nerve release has been described though not carried out in our patients.16,37 Transient nerve palsy involving common peroneal and radial nerve was seen in the immediate postoperative period in 2 cases, both recovered fully. The transient radial nerve palsy occurred despite the exposure of the bone for distal pin placement. Four out of eight patients had transient common peroneal palsy in a study by Lie et al.18
We suggest that stature lengthening in achondroplasia should be initiated around five to six years following extensive psychosocial counseling of parents and child. Either femur or tibial lengthening can be embarked upon, based on the surgeon and parents’ choice. Bilateral humeral lengthening is advisable next, as this does not necessarily immobilize the child or restrict activities and at the same time allows the lower limbs to recover and remodel before the next lengthening. Transverse bilateral tibial/femoral lengthening should be done at the end. We prefer ring fixator and bifocal corticotomy for the tibia and monolateral fixators for the femur and humerus. The rate of distraction of the distal corticotomy should be reduced to half after an initial tibial lengthening of 3–5 cm to avoid complications. The addition of a foot frame after an initial lengthening of 3 cm and ensuring fixation of the tibiofibular joint, are useful in preventing ankle deformity.
In summary, limb lengthening in achondroplasia is a major undertaking associated with significant complications and should be embarked on only after due consideration. Performing all lower limb lengthening procedures by 10 years of age avoids interfering with schooling in the adolescent years.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Authors acknowledge the help provided by Dr. Noel M Walter (Professor of Pathology, Christian Medical College, Vellore) for reviewing the manuscript.
REFERENCES
- 1.Herring JA. In: Tachdjian's Pediatric Orthopaedics. 4th ed. Herring JA, editor. Philadelphia, PA: Saunders Elsevier; 2008. pp. 1677–700. [Google Scholar]
- 2.Savarirayan R, Rimoin DL. The skeletal dysplasias. Best Pract Res Clin Endocrinol Metab. 2002;16:547–60. doi: 10.1053/beem.2002.0210. [DOI] [PubMed] [Google Scholar]
- 3.Kim SJ, Balce GC, Agashe MV, Song SH, Song HR. Is bilateral lower limb lengthening appropriate for achondroplasia. Midterm analysis of the complications and quality of life? Clin Orthop Relat Res. 2012;470:616–21. doi: 10.1007/s11999-011-1983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ireland PJ, McGill J, Zankl A, Ware RS, Pacey V, Ault J, et al. Functional performance in young Australian children with achondroplasia. Dev Med Child Neurol. 2011;53:944–50. doi: 10.1111/j.1469-8749.2011.04050.x. [DOI] [PubMed] [Google Scholar]
- 5.Catagni MA, Lovisetti L, Guerreschi F, Combi A, Ottaviani G. Cosmetic bilateral leg lengthening: Experience of 54 cases. J Bone Joint Surg Br. 2005;87:1402–5. doi: 10.1302/0301-620X.87B10.16468. [DOI] [PubMed] [Google Scholar]
- 6.Venkatesh KP, Modi HN, Devmurari K, Yoon JY, Anupama BR, Song HR. Femoral lengthening in achondroplasia: Magnitude of lengthening in relation to patterns of callus, stiffness of adjacent joints and fracture. J Bone Joint Surg Br. 2009;91:1612–7. doi: 10.1302/0301-620X.91B12.22418. [DOI] [PubMed] [Google Scholar]
- 7.Hoover-Fong JE, Schulze KJ, McGready J, Barnes H, Scott CI. Age-appropriate body mass index in children with achondroplasia: Interpretation in relation to indexes of height. Am J Clin Nutr. 2008;88:364–71. doi: 10.1093/ajcn/88.2.364. [DOI] [PubMed] [Google Scholar]
- 8.Saleh M, Burton M. Leg lengthening: Patient selection and management in achondroplasia. Orthop Clin North Am. 1991;22:589–99. [PubMed] [Google Scholar]
- 9.Herzenberg HE, Paley D. Methods and strategies in limb lengthening and realignment for skeletal dysplasia. Limb Lengthening-for Whom, How and When? In: Laron Z, Mastragostino S, Romano C, editors. Tel Aviv: Freund Publishing Ltd; 1995. pp. 181–99. [Google Scholar]
- 10.Aldegheri R, Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001;10:238–47. [PubMed] [Google Scholar]
- 11.Stanitski CL. Limb lengthening for stature. J Pediatr Orthop. 2004;24:593–4. doi: 10.1097/00004694-200409000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Gross RH. Limb lengthening for stature: Another view. J Pediatr Orthop. 2005;25:128–9. doi: 10.1097/00004694-200501000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Aldegheri R. Distraction osteogenesis for lengthening of the tibia in patients who have limb-length discrepancy or short stature. J Bone Joint Surg Am. 1999;81:624–34. doi: 10.2106/00004623-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Aldegheri R, Trivella G, Renzi-Brivio L, Tessari G, Agostini S, Lavini F. Lengthening of the lower limbs in achondroplastic patients. A comparative study of four techniques. J Bone Joint Surg Br. 1988;70:69–73. doi: 10.1302/0301-620X.70B1.3339063. [DOI] [PubMed] [Google Scholar]
- 15.Ganel A, Horoszowski H. Limb lengthening in children with achondroplasia. Differences based on gender. Clin Orthop Relat Res. 1996;332:179–83. doi: 10.1097/00003086-199611000-00024. [DOI] [PubMed] [Google Scholar]
- 16.Vaidya SV, Song HR, Lee SH, Suh SW, Keny SM, Telang SS. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: An analysis of results and complications. J Pediatr Orthop. 2006;26:788–93. doi: 10.1097/01.bpo.0000242429.83866.97. [DOI] [PubMed] [Google Scholar]
- 17.Kim SJ, Agashe MV, Song SH, Choi HJ, Lee H, Song HR. Comparison between upper and lower limb lengthening in patients with achondroplasia: A retrospective study. J Bone Joint Surg Br. 2012;94:128–33. doi: 10.1302/0301-620X.94B1.27567. [DOI] [PubMed] [Google Scholar]
- 18.Lie CW, Chow W. Limb lengthening in short-stature patients using monolateral and circular external fixators. Hong Kong Med J. 2009;15:280–4. [PubMed] [Google Scholar]
- 19.Vargas Barreto B, Caton J, Merabet Z, Panisset JC, Pracros JP. Complications of Ilizarov leg lengthening: A comparative study between patients with leg length discrepancy and short stature. Int Orthop. 2007;31:587–91. doi: 10.1007/s00264-006-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watts J. China's cosmetic surgery craze. Leg-lengthening operations to fight height predjudice can leave patients crippled. Lancet. 2004;363:958. doi: 10.1016/s0140-6736(04)15832-7. [DOI] [PubMed] [Google Scholar]
- 21.Schiedel F, Rödl R. Lower limb lengthening in patients with disproportionate short stature with achondroplasia: A systematic review of the last 20 years. Disabil Rehabil. 2012;34:982–7. doi: 10.3109/09638288.2011.631677. [DOI] [PubMed] [Google Scholar]
- 22.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 23.Dahl MT, Gulli B, Berg T. Complications of limb lengthening. A learning curve. Clin Orthop Relat Res. 1994;301:10–8. [PubMed] [Google Scholar]
- 24.De Bastiani G, Aldegheri R, Renzi Brivio L, Trivella G. Chondrodiatasis-controlled symmetrical distraction of the epiphyseal plate. Limb lengthening in children. J Bone Joint Surg Br. 1986;68:550–6. doi: 10.1302/0301-620X.68B4.3733829. [DOI] [PubMed] [Google Scholar]
- 25.Paley D, Matz AL, Kurland DB, Lamm BM, Herzenberg JE. Multiplier method for prediction of adult height in patients with achondroplasia. J Pediatr Orthop. 2005;25:539–42. doi: 10.1097/01.bpo.0000161095.15845.7d. [DOI] [PubMed] [Google Scholar]
- 26.Donnan LT, Saleh M, Rigby AS. Acute correction of lower limb deformity and simultaneous lengthening with a monolateral fixator. J Bone Joint Surg Br. 2003;85:254–60. doi: 10.1302/0301-620x.85b2.12645. [DOI] [PubMed] [Google Scholar]
- 27.Kim SJ, Pierce W, Sabharwal S. The etiology of short stature affects the clinical outcome of lower limb lengthening using external fixation. A systematic review of 18 trials involving 547 patients. Acta Orthop. 2014;85:181–6. doi: 10.3109/17453674.2014.899856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Herzenberg JE, Paley D. In: Stature lengthening in skeletal dysplasia. Limb Lengthening and Reconstruction Surgery. Rozbruch RS, Ilizarov S, editors. New York: Informa Healthcare; 2007. pp. 575–96. [Google Scholar]
- 29.Kocaoglu M, Bilen FE, Dikmen G, Balci HI, Eralp L. Simultaneous bilateral lengthening of femora and tibiae in achondroplastic patients. Acta Orthop Traumatol Turc. 2014;48:157–63. doi: 10.3944/AOTT.2014.3274. [DOI] [PubMed] [Google Scholar]
- 30.Lavini F, Renzi-Brivio L, de Bastiani G. Psychologic, vascular, and physiologic aspects of lower limb lengthening in achondroplastics. Clin Orthop Relat Res. 1990;250:138–42. [PubMed] [Google Scholar]
- 31.Kiss S, Pap K, Vízkelety T, Terebessy T, Balla M, Szoke G. The humerus is the best place for bone lengthening. Int Orthop. 2008;32:385–8. doi: 10.1007/s00264-007-0327-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal DK, Agarwal KN, Upadhyay SK, Mittal R, Prakash R, Rai S. Physical and sexual growth pattern of affluent Indian children from 5 to 18 years of age. Indian Pediatr. 1992;29:1203–82. [PubMed] [Google Scholar]
- 33.Noonan KJ, Leyes M, Forriol F, Cañadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998;80:793–806. doi: 10.2106/00004623-199806000-00003. [DOI] [PubMed] [Google Scholar]
- 34.De Pellegrin M, Moharamzadeh D. Ultrasound hip evaluation in achondroplasia. J Pediatr Orthop. 2008;28:427–31. doi: 10.1097/BPO.0b013e3181653b87. [DOI] [PubMed] [Google Scholar]
- 35.Galardi G, Comi G, Lozza L, Marchettini P, Novarina M, Facchini R, et al. Peripheral nerve damage during limb lengthening. Neurophysiology in five cases of bilateral tibial lengthening. J Bone Joint Surg Br. 1990;72:121–4. doi: 10.1302/0301-620X.72B1.2298769. [DOI] [PubMed] [Google Scholar]
- 36.Polo A, Aldegheri R, Zambito A, Trivella G, Manganotti P, De Grandis D, et al. Lower-limb lengthening in short stature. An electrophysiological and clinical assessment of peripheral nerve function. J Bone Joint Surg Br. 1997;79:1014–8. doi: 10.1302/0301-620x.79b6.7912. [DOI] [PubMed] [Google Scholar]
- 37.Nogueira MP, Paley D. Prophylactic and therapeutic peroneal nerve decompression for deformity correction and lengthening. Oper Tech Orthop. 2011;21:180–3. [Google Scholar]