Abstract
Lumbar epidural varices can also present with radiculopathy similar to acute intervertebral disc prolapse (IVDP). However as the magnetic resonance imaging (MRI) in these patients are usually normal without significant compressive lesions of the nerve roots, the diagnosis is commonly missed or delayed leading to persistent symptoms. We present a rare case of acute severe unilateral claudication with a normal MRI unresponsive to conservative management who was treated surgically. The nerve root on the symptomatic side was found to be compressed by large anterior epidural varices secondary to an abnormal cranial attachment of ligamentum flavum. Decompression of the root and coagulation of the varices resulted in complete pain relief. To conclude, lumbar epidural varices should be considered in the differential diagnosis of acute onset radiculopathy and claudication in the absence of significant MRI findings.
Keywords: Epidural varices, ligamentum flavum, lumbar disc prolapse
MeSh terms: Intermittent claudication, disc, herniated, varices, spine
INTRODUCTION
Lumbar radiculopathy due to root irritation by prolapsed intervertebral disc and hypertrophied ligamentum flavum (LF) is a well known entity. Varices of epidural venous plexus has also been rarely implicated as the cause of lumbar nerve root impingement in which magnetic resonance imaging (MRI) doesn’t show significant abnormality.1,2 Zimmerman et al. reported 0.07% incidence of epidural varices, whereas Hammer et al. reported it as 4.7%.3,4 Their clinical presentation closely resembles acute intervertebral disc prolapse (IVDP) with sudden onset low back ache (LBA) and radiculopathy. Apart from obstruction of inferior venacava (IVC), localized spinal cord compression secondary to disc or other lesions have been implicated to cause epidural varices.5
We report a rare case of neurogenic claudication due to lumbar nerve root impingement by anterior epidural varices secondary to localized compression caused by an abnormal cranial attachment of LF.
CASE REPORT
A 45-year-old hypertensive female presented with sudden onset severe right lower-limb claudication since 1-week with a claudication distance of 4–5 steps. She was on conservative management for LBA and radicular pain since 5 months, and the recent increase in severity of pain had restricted her mobility significantly. Clinical examination revealed spasm in the lumbar region with list and tenderness and straight leg raising was 30° on the right side and 70° on the left. Motor examination revealed grade 3/5 power in right L5 with a corresponding sensory deficit.
Plain radiographs [Figure 1] revealed spondylotic changes with sclerosis of the posteroinferior corner of L4 vertebral body. MRI [Figure 2] showed mild disc bulge at L5–S1 with no significant central or lateral canal stenosis. Sclerotic change was observed in the posteroinferior aspect of L4 vertebral body on the right side [Figure 2a]. A linear hypointense signal extending anteriorly from the LF on the right side until the posterolateral aspect of L4 body medial to the nerve root [Figure 2b] was visualized in the axial T2-weighted images. As MRI did not show any significant compression of roots, she was being managed conservatively in many hospitals, but her pain was persistent and severe.
Figure 1.
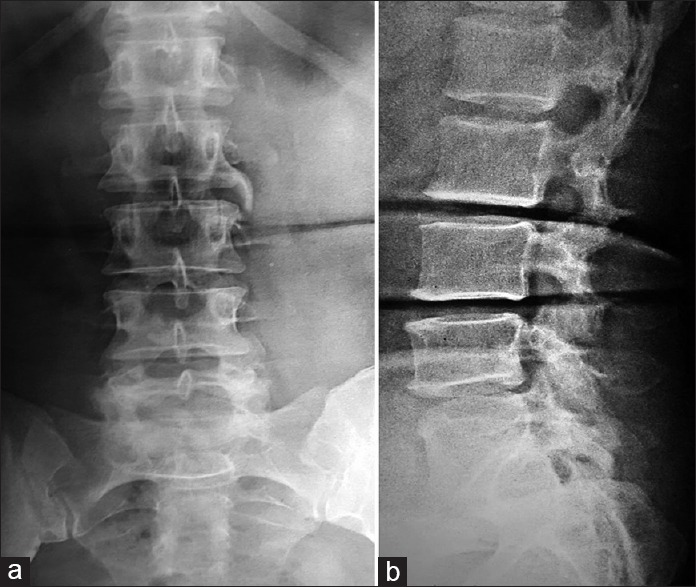
(a) Anteroposterior and (b) lateral plain radiographs of lumbosacral spine showing spondylotic changes with syndesmophytes at L3, L4 and L5
Figure 2.
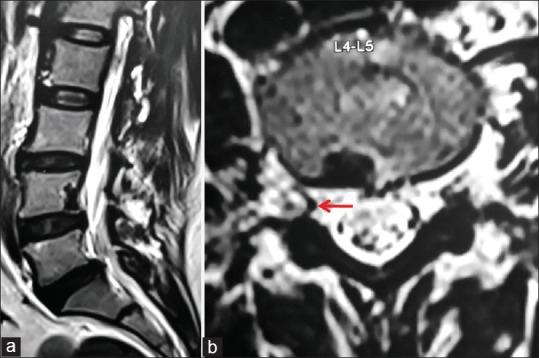
(a) Sagittal and (b) axial T2-weighted magnetic resonance images showing sclerotic changes at the posteroinferior corner of L4 vertebral body on the right side. The red arrow shows a hypointense signal extending anteriorly from the ligamentum flavum on the right side to get inserted into the posterolateral aspect of L4 body medial to the nerve root
As she was not responding to conservative management for a period of 5 months and her pain was very severe with inability to walk even a few steps, she was planned for decompression of right sided root as the MRI showed a band of ligamentum flavum compressing the nerve from the medial side at L4–L5 isolating it from the main dura and disc bulge at L5–S1. Under general anesthesia, L5–S1 central and lateral canal was explored and the right sided root was found to be free. At L4–L5, the LF on the right interlaminar region was not hypertrophied but instead of attaching to the lower border and anteroinferior surface of cranial vertebra, it's lateral part was coursing anteriorly under the lamina beyond the facet joint capsule and was attached to the posterolateral surface of L4 vertebral body just medial to the pedicle [Figure 3a] as visualized in the MRI. Partial medial facetectomy was done to view this part of LF, that was positioned between the exiting nerve root laterally and traversing nerve root medially. It was difficult to introduce the nerve root dissector under the LF to probe the right sided nerve roots due to severe foraminal stenosis. The LF that was attached to the vertebral body was then gradually excised to decompress the nerve roots and sent for histopathological examination (HPE). On retraction of right side nerve roots after decompression, grossly engorged anterior epidural veins were found to be situated directly anterior to these roots compressing it [Figure 3b]. The veins were coagulated, and nerve roots decompressed. The disc space was then visualized, and no evidence of disc bulge was found.
Figure 3.
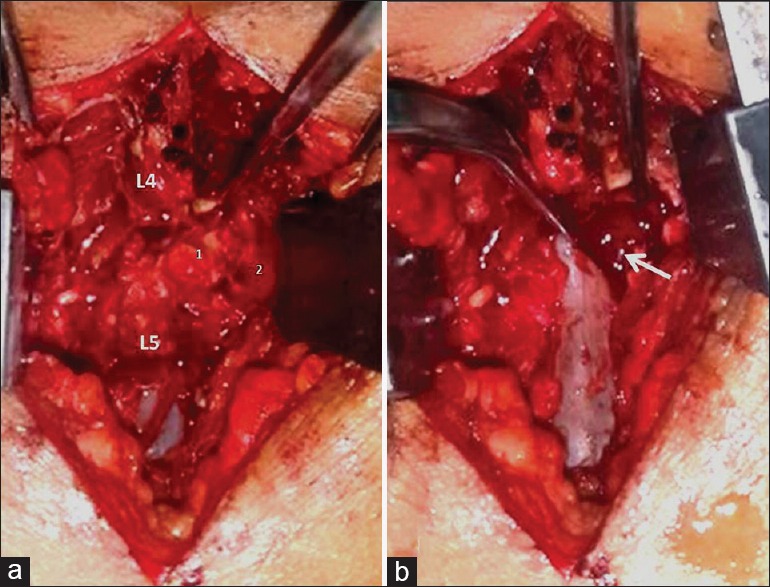
(a) Intraoperative photographs showing the ligamentum flavum (LF) (1) extending anteriorly beyond the facet joint (2) to get attached to the posterolateral aspect of L4 vertebral body. (b) Large epidural venous varices on retracting the dura after excision of LF (arrow)
The patient had complete relief of claudication postoperatively, and she was mobilized without any aid. She was discharged on the 3rd day, and the sutures were removed on the 10th day. Her radicular pain intensity on visual analog scale improved from 10/10 preoperatively to no pain (0/10) postoperatively. Biopsy report was consistent with normal LF with normal chondrocytes at the site of bony attachment to the vertebral body [Figure 4] without evidence of hypertrophy, fibrosis or chondroid metaplasia. She was reviewed at regular intervals and was asymptomatic at her final followup of 13 months postoperatively during which the motor power of right L5 improved to grade 4/5.
Figure 4.
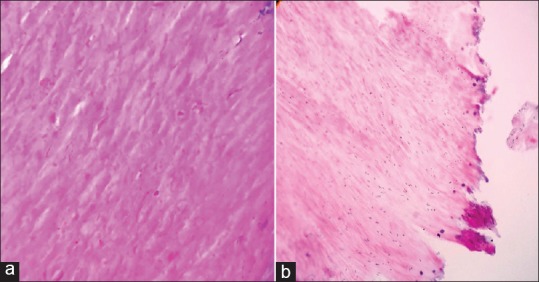
(a) Light microscopic (×100), hematoxylin and eosin stained sections of ligamentum flavum showing organized pattern of elastic fibers without evidence of hypertrophy. (b) Fibrocartilagenous tissue at the site of bony attachment with normal chondrocytes
DISCUSSION
The onset of pain due to lumbar epidural varices are sudden and intractable akin to acute disc prolapse. These patients generally get admitted to the emergency voluntarily due to the severe intensity of pain, which is resistant to conservative measures, including analgesics, steroids and physiotherapy.4 Trigeminal neuralgia secondary to irritation of the fifth nerve within skull has been reported by Petty et al. to be caused by vascular anomalies.6 Similarly, venous plexus surrounding the cord and nerve root is a very potent source of radicular pain as it directly compresses the root and dorsal ganglion.4 Epidural varices has also been rarely implicated as an etiological factor for claudication due to the epidural collateral circulation that occur secondary to IVC obstruction,1 which was not seen in our patient. Localized compression of anterior internal vertebral veins also results in rostral blood flow causing a secondary dilatation of valveless epidural venous sinuses.3 These anterior internal vertebral veins course vertically within the spinal canal in the posterolateral aspect of the vertebral body medial to the pedicle consistent with the vertically oriented group of veins as seen in our case.
Dabasia et al.7 emphasized the importance of lumbar epidural venous engorgement as a cause of neurogenic claudication in the absence of spinal stenosis in a case of follicular lymphoma due to compression of IVC by enlarged lymph nodes. Marshman et al.8 reported a rare case of symptomatic spinal extradural arteriovenous malformation (E-AVM) causing claudication and concluded that E-AVM exacerbates claudication by both compressive and venous hypertensive mechanisms when there is preexistent canal stenosis. Porter described a two-level stenosis concept of venous pooling in the cauda equina between two levels of low-pressure central canal occlusion for the pathogenesis of neurogenic claudication.9 Lumbar epidural pressure of 15–18 mmHg have been reported in flexion and 80–100 mmHg in extension.10 Walking increases the venous return from lower-limbs and this exercise-induced increase in pressure causes further engorgement of epidural veins raising the stenotic pressure significantly.11 This mechanism might also have been the cause of claudication in our patient as she was asymptomatic in the sitting posture and walking induced elevation of epidural venous pressure would have aggravated the pressure on the nerve root which was already compressed in the lateral recess by the abnormally attached slip of LF. The clinical differentiation of lumbar epidural varices from lumbar canal stenosis is difficult as the symptoms and signs of neurogenic claudication is similar in both entities. Marshman et al. reported the role of spinal angiography in the diagnosis of vascular causes of stenosis. As we attributed the lateral recess stenosis due to the abnormally attached LF as the cause of claudication in our patient, spinal angiography was not done preoperatively. However, the intraoperative identification of epidural varices as the compressive element in this patient highlights the importance of recognizing this entity preoperatively and performing spinal angiography in those presenting with classical claudication, but with a normal MRI.
The lateral border of LF generally fuses with the corresponding facet joint capsule and forms the roof of the intervertebral foramen. However, the LF in our case extended anteriorly beyond the joint capsule to get attached to the posterolateral surface of L4 vertebral body. The HPE of hypertrophied LF shows large areas of fibrosis with degradation of elastic fibers, intrasubstance calcification and chondroid metaplasia at the site of its bony attachment. In contrast, normal LF shows an orderly flowing pattern of elastic fibers, collagen fibers and the scattered spindle shaped fibrocytes while elastic fibrocartilaginous tissue is seen at its site of attachment to the bone with abundant collagenous component containing chondrocyte-like cells.7 The biopsy of the portion of LF that was removed from its attachment to the L4 body in this patient showed features consistent with normal morphology further proving that the LF hypertrophy was not the cause of claudication in our case. As LF hypertrophy was not observed in MRI, intraoperatively and in HPE, the claudication in this case was due to the compression of nerve root by epidural varices that probably would have been due to the compression of anterior internal vertebral veins by the abnormally attached LF.
Hence, lumbar epidural varices can also present with acute onset of radiculopathy similar to IVDP, especially aggravated after walking a few steps as seen in lumbar canal stenosis. However, the MRI can be normal which might delay its diagnosis and treatment resulting in the patient suffering from persistent symptoms.
CONCLUSION
Lumbar epidural varices should be considered in the differential diagnosis of acute onset radiculopathy and claudication in the absence of significant pathology in MRI in a patient with the clinical diagnosis of lumbar disc prolapse. In the absence of IVC obstruction, epidural varices can also be secondary to the localized compression of anterior internal vertebral veins by a prolapsed intervertebral disc or LF.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Kawai M, Udaka F, Nishioka K, Houshimaru M, Koyama T, Kameyama M. A case of idiopathic spinal epidural lipomatosis presented with radicular pain caused by compression with enlarged veins surrounding nerve roots. Acta Neurol Scand. 2002;105:322–5. doi: 10.1034/j.1600-0404.2002.1c194.x. [DOI] [PubMed] [Google Scholar]
- 2.Blättler W, Spiess H. Spinal claudication following ileocaval venous thrombosis. Schweiz Med Wochenschr. 1988;118:1209–12. [PubMed] [Google Scholar]
- 3.Zimmerman GA, Weingarten K, Lavyne MH. Symptomatic lumbar epidural varices. Report of two cases. J Neurosurg. 1994;80:914–8. doi: 10.3171/jns.1994.80.5.0914. [DOI] [PubMed] [Google Scholar]
- 4.Hammer A, Knight I, Agarwal A. Localized venous plexi in the spine simulating prolapse of an intervertebral disc: A report of six cases. Spine (Phila Pa 1976) 2003;28:E5–E12. doi: 10.1097/00007632-200301010-00025. [DOI] [PubMed] [Google Scholar]
- 5.Paksoy Y, Gormus N. Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine (Phila Pa 1976) 2004;29:2419–24. doi: 10.1097/01.brs.0000144354.36449.2f. [DOI] [PubMed] [Google Scholar]
- 6.Petty PG, Southby R, Siu K. Vascular compression: Cause of trigeminal neuralgia. Med J Aust. 1980;1:166–7. doi: 10.5694/j.1326-5377.1980.tb134736.x. [DOI] [PubMed] [Google Scholar]
- 7.Dabasia H, Rahim N, Marshall R. Neurogenic claudication without spinal stenosis arising as a result of lumbar epidural varices. J Bone Joint Surg Br. 2012;94:1292–4. doi: 10.1302/0301-620X.94B9.29322. [DOI] [PubMed] [Google Scholar]
- 8.Marshman LA, David KM, Chawda SJ. Lumbar extradural arteriovenous malformation: Case report and literature review. Spine J. 2007;7:374–9. doi: 10.1016/j.spinee.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 9.Porter RW. Spinal stenosis and neurogenic claudication. Spine (Phila Pa 1976) 1996;21:2046–52. doi: 10.1097/00007632-199609010-00024. [DOI] [PubMed] [Google Scholar]
- 10.Takahashi K, Miyazaki T, Takino T, Matsui T, Tomita K. Epidural pressure measurements. Relationship between epidural pressure and posture in patients with lumbar spinal stenosis. Spine (Phila Pa 1976) 1995;20:650–3. [PubMed] [Google Scholar]
- 11.Takahashi K, Kagechika K, Takino T, Matsui T, Miyazaki T, Shima I. Changes in epidural pressure during walking in patients with lumbar spinal stenosis. Spine (Phila Pa 1976) 1995;20:2746–9. doi: 10.1097/00007632-199512150-00017. [DOI] [PubMed] [Google Scholar]


