Abstract
Objective
Research on the manifestations and health correlates of eating disorder symptoms among males is lacking. This study identified patterns of appearance concerns and eating disorder behaviors from adolescence through young adulthood and their health correlates.
Method
Participants were 7,067 males from the prospective Growing Up Today Study. Surveys from 1999–2007 (spanning ages 13–26 years) provided repeated measures data on: muscularity and leanness concerns; eating disorder behaviors (purging, overeating, binge eating, use of muscle-building products); and health correlates (obesity, non-marijuana drug use, binge drinking, and depressive symptoms).
Results
Latent class analyses of observations at ages 13–15, 16–18, 19–22, and 23–26 identified one large Asymptomatic class and four symptomatic patterns: Body Image Disturbance (high appearance concerns, low eating disorder behaviors; 1.0%–6.0% per age period); Binge Eating/Purging (binge eating and purging, use of muscle-building products, low appearance concerns; 0.1%–2.5%); Mostly Asymptomatic (low levels of muscularity concern, product use, and overeating; 3.5%–5.0%); and Muscularity Concerns (high muscularity concerns and use of products; 0.6%–1.0%). The Body Image Disturbance class was associated with high estimated prevalence of depressive symptoms. Males in the Binge Eating/Purging and Muscularity Concerns classes had high prevalence of binge drinking and drug use. Despite exhibiting modestly greater appearance concerns and eating disorder behaviors than the Asymptomatic class, being in the Mostly Asymptomatic class was prospectively associated with adverse health outcomes.
Conclusion
Results underscore the importance of measuring concerns about leanness, muscularity, and use of muscle-building products when assessing eating disorder presentations among males in research and clinical settings.
Keywords: eating disorder, body image, gender, adolescence, longitudinal analysis
INTRODUCTION
Eating disorders require substantial clinical resources to treat and are a tremendous burden to the health and development of those afflicted. Concerns with one’s appearance and eating disorder behaviors (e.g., binge eating) at subclinical levels can also increase risk for deleterious physical and mental health outcomes.1–5 Eating disorder diagnostic criteria are largely based on research and clinical work with females.6,7 The dearth of work on afflicted males may be due to the historic view that males are not at risk, the insensitivity of diagnostic frameworks in indexing the concerns and behaviors of males, insufficient numbers of male patients in clinical treatment settings, and the lack of population-based data on appearance concerns and eating disorder behaviors among males.8
Research using diagnostic interviews and questionnaires has found that males are less likely than females to report appearance concerns and body dissatisfaction, despite having similar levels of psychopathology, and that males may binge eat to similar or greater degrees than females, but with less concomitant negative emotionality.6,9–11 Recent changes to the DSM-5—such as recognizing binge eating disorder as a stand-alone diagnosis and reducing the behavioral thresholds for the bulimia nervosa diagnosis12—may allow for greater detection of eating disorders among males. However, males may also exhibit unique presentations of eating disorders tied to gendered ideals about appearance and performance (e.g., muscle dysmorphia).4,8,13 Beyond concerns regarding body weight and adiposity, males may be concerned about their muscle size and definition.14–17 Whereas the thin ideal is generally widely internalized among females, males who perceive themselves to be too thin or lacking muscles and those who perceive themselves as being overweight are vulnerable to body dissatisfaction and behaviors such as muscle-building product use (e.g., creatine, steroids).4,15 Whether muscularity-oriented disordered concerns and eating behaviors should be considered an eating disorder phenotype is the topic of ongoing research and clinical debate.18
Pattern-centered analyses (e.g., latent class analysis [LCA]),19 have been used to evaluate and refine eating disorder diagnostic criteria, generally in samples with few or no male participants.5,20–23 Few studies have used LCA to examine appearance concerns and eating disorder behaviors in males across time. One study of 15- to 20-year-old males in the Growing Up Today Study used LCA to examine patterns of appearance concerns and eating disorder behaviors among heterosexual, gay, bisexual, and mostly heterosexual males, detecting patterns focused on weight restriction and muscle-building.24 However, this study utilized low thresholds for defining cases (e.g., any past-year binge eating) and did not assess whether patterns were associated with health consequences. To help identify clinically relevant patterns of symptom presentation, analyses should incorporate more severe presentations of eating disorder cognitions and behaviors and examine their health correlates. The current study used LCA to identify co-occurring patterns of appearance concerns about muscularity and leanness and eating disorder behaviors among males from adolescence through young adulthood, and evaluated clinical relevance by comparing classes’ risks for obesity, substance use, and depressive symptoms.
METHOD
Participants and Procedure
Participants in the Growing Up Today Study (GUTS) are children of women in the Nurses’ Health Study II and were 9–14 years old at baseline in 1996. After obtaining parental consent, children were invited to enroll in GUTS, with return of the baseline questionnaire considered as assent (N=7,843 males). Participants completed questionnaires annually from 1996–2001 and biennially after 2001. The Brigham and Women’s Hospital institutional review board approved this study. Data for the current study were from the 1999–2007 questionnaires, spanning ages 13–26 years.
Measures
Latent class indicators
Concern about muscularity and concerns about leanness were assessed using items adapted from the McKnight Risk Factor Survey (MRFS),25 which uses a 5-point scale to measure the frequency that participants experienced a particular concern in the past year (1=Never to 5=Always). An item assessing muscularity concern was created for GUTS and examined desire for toned or defined muscles, with responses of 1–3 coded as low or no muscularity concern, and responses of 4–5 coded as high muscularity concern. Leanness concerns were assessed as the mean of three items: (1) thought about wanting to be thinner; (2) worried about having fat on your body; (3) felt fat. Mean leanness concerns scores that were 1–3 were coded as low or no leanness concerns, and mean scores that were 4–5 were coded as high leanness concerns.
For product use, participants indicated past-year frequency of using creatine, amino acids, dehydroepiandrosterone (DHEA), androstenedione, growth hormone, and anabolic/injectable steroids (not including steroids used for treating medical conditions). Use of any products was coded into three categories: never or less than monthly use, at least monthly use, and at least weekly use.
Purging was assessed as past-year frequency of vomiting or using laxatives to lose weight or keep from gaining weight (0=Never to 5=Daily). Responses were coded as never or less than monthly purging vs. at least monthly purging.
Participants answered two questions to identify overeating and binge eating (i.e., overeating with a loss of control). Participants were first asked about overeating: “Sometimes people will go on an ‘eating binge,’ where they eat an amount of food that most people, like their friends, would consider to be very large, in a short amount of time. In the past year, how often did you go on an eating binge?” Participants who engaged in overeating less than once a month were coded as 0 (referent) for the overeating and binge eating variables. Respondents who engaged in overeating at least monthly received the follow-up question: “Did you feel out of control, like you couldn’t stop eating even if you wanted to stop?” (Yes/No). Participants who responded “No” were coded as 1 (overeating at least monthly) for the overeating variable. Participants who responded “Yes” were coded as 1 (binge eating at least monthly) for the binge eating variable.
In the class enumeration phase, LCA models were adjusted for current weight status. Participants reported height and weight at each wave for calculation of body mass index (BMI; kg/m2). BMIs for observations before age 18 years were coded as overweight or obese using International Obesity Task Force cutoffs.26 BMIs for observations ages 18 and older were coded as overweight if BMI was ≥25 and <30 kg/m2, and obese if BMI was ≥30 kg/m2.
Health Correlates
Classes were compared on the health correlates of incident (i.e., new cases of) obesity and prevalent and incident frequent binge drinking, drug use, and high depressive symptoms. To assess frequent binge drinking, participants who indicated ever trying alcohol (beer, wine, or liquor) were asked, “During the past year, how many times did you drink 5 or more alcoholic drinks over a few hours?” A single drink was defined as 1 can/bottle of beer, 1 glass of wine, 1 shot of liquor, or 1 mixed drink. Frequent binge drinking was defined as ≥12 episodes of consuming 5+ alcoholic beverages over a few hours in the past year. Participants reported non-marijuana drug use by indicating whether they engaged in any past-year use of ecstasy, heroin, cocaine, crystal meth, speed, mushrooms, LSD, and drugs without a doctor’s prescription (e.g., Ritalin). Past-year drug use was defined as use of at least one of the drugs assessed. Marijuana was excluded from analyses due to the expected cross-sectional association between marijuana use and overeating.
In the 1999–2003 waves, past-year depressive symptoms were assessed using the mean of six items from the MRFS (e.g., “In the past year, how often did you feel ‘down in the dumps’ or depressed?”, 0=Never to 4=Always). In 2007, depressive symptoms were assessed using the mean of the 10-item version of the Centers for Epidemiological Studies Depression scale,27 which assessed how often participants experienced certain feelings in the past week (e.g., “I felt that everything I did was an effort,” 0=Rarely or none of the time, to 3=All of the time). High depressive symptoms were defined at each wave as mean score at or above the top quintile.
Analyses
Repeated measures observations were grouped into four age periods: 13–15, 16–18, 19–22, and 23–26 years old. Participants were included in every age period in which they had an observation of weight status and at least one of the latent class indicators. Methods to account for missing data and the class enumeration phase of analyses (which identified patterns of appearance concerns and eating disorder behaviors; see Table S1, available online) are described in Supplement 1 (available online). To examine associations between the identified classes and the health correlates, we used the 3-step approach in Mplus28,29 to calculate estimated number of cases of each of the health correlates per class. The 3-step procedure conducts pairwise Wald Chi-Square tests to detect significant differences between classes on each health correlate.29 Significance was set at alpha=.01 to reduce the probability of Type-I error due to the number of pair-wise tests.
RESULTS
The analytic sample consisted of 7,067 males (90.1% of baseline sample) who, across six survey waves, contributed 14,077 repeated measures observations at ages 13–15 years old; 8,994 observations at ages 16–18; 7,742 observations at ages 19–22; and 4,538 observations at ages 23–26. Table 1 displays descriptive statistics for the latent class indicators and health correlates.
Table 1.
Frequencies for Eating Disorder Latent Class Indicators From Ages 13–26 Years Among Males in the Growing Up Today Study (Participant n = 7,067)
| %(n) | ||||
|---|---|---|---|---|
| Observations From Ages 13–15 Years n = 14,077 |
Observations From Ages 16–18 Years n = 8,994 |
Observations From Ages 19–22 Years n = 7,742 |
Observations From Ages 23–26 Years n = 4,538 |
|
| Latent Variable Indicators | ||||
| Leanness Concern | 3.1% (439) | 2.2% (198) | 3.2% (247) | 0.8% (38) |
| Muscularity Concern | 4.2% (589) | 5.0% (446) | 6.7% (519) | 1.1% (52) |
| Weekly Product Use | 0.2% (35) | 2.3% (209) | 3.2% (244) | 2.3% (103) |
| Monthly Product Use | 0.1% (19) | 0.9% (79) | 1.1% (85) | 0.8% (37) |
| Purging | 0.4% (53) | 0.4% (33) | 0.5% (35) | 1.2% (46) |
| Binge Eating | 0.5% (70) | 0.8% (69) | 1.8% (142) | 1.6% (74) |
| Overeating | 1.2% (167) | 2.4% (217) | 5.0% (388) | 4.5% (203) |
| Health Correlates | ||||
| Incident Obesity | 1.5% (208) | 1.2% (107) | 1.9% (144) | 1.0% (47) |
| Frequent Binge Drinking | ||||
| Prevalence | 0.8% (106) | 10.4% (932) | 33.9% (2,623) | 38.0% (1726) |
| Incidence | 2.1% (295) | 11.1% (995) | 7.0% (544) | 1.5% (66) |
| Non-Marijuana Drug Use | ||||
| Prevalence | 1.3% (184) | 5.5% (498) | 11.1% (862) | 28.1% (1275) |
| Incidence | 0.9% (122) | 3.6% (320) | 6.9% (534) | 2.9% (132) |
| High Depressive Symptoms | ||||
| Prevalence | 4.5% (637) | 11.3% (1,012) | 11.5% (889) | 15.4% (697) |
| Incidence | 1.6% (228) | 3.1% (281) | 4.4% (339) | 1.7% (78) |
Note: Prevalent health correlate variables represent current health states and behaviors at a given age. Incident health correlate variables were used in prospective lagged analyses and represent all new cases reported at subsequent ages after censoring existing cases. At the first wave of assessment of a variable, all cases are considered incident.
Latent classes
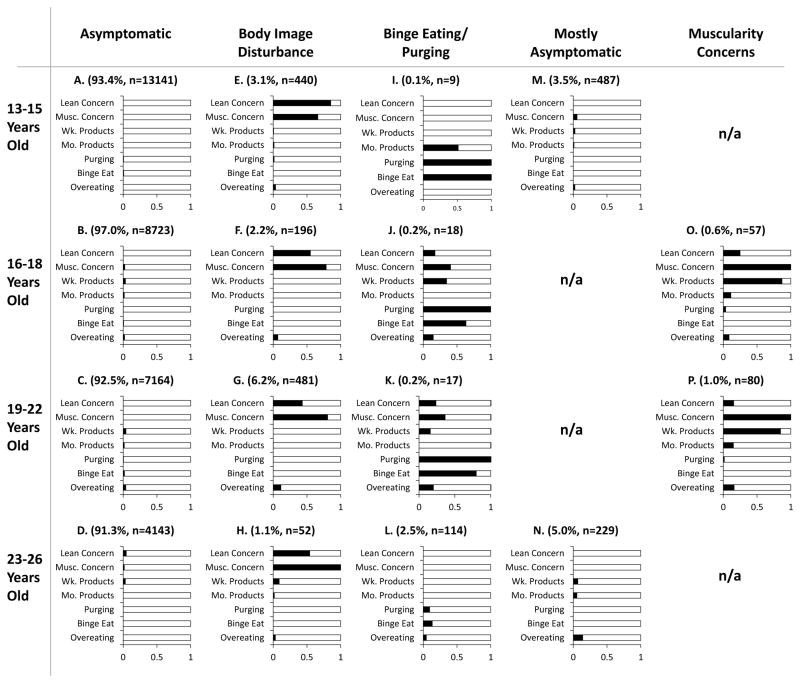
Figure 1 plots the identified classes by indicator probability. The largest class at each age period was an Asymptomatic class (91%–97% of observations per age period), which exhibited little or no appearance concerns or eating disorder behaviors. Four symptomatic classes emerged at each age period: two presenting at all four age periods (Body Image Disturbance and Binge Eating/Purging) and two presenting only during two age periods (Mostly Asymptomatic and Muscularity Concerns). Participants in the Body Image Disturbance class (Figure 1E–1H; 1.0%–6.0%) exhibited high prevalence of leanness and muscularity concerns, but low prevalence of eating disorder behaviors relative to the other classes. Participants in the Binge Eating/Purging class (Figure 1I–1L; 0.1%–2.5%) exhibited higher prevalence of binge eating and purging relative to the other classes, although the class varied in the presentation of symptoms across the age periods. Between ages 13–22 years old, participants in the Binge Eating/Purging class also reported higher levels of use of muscle-building products relative to the Asymptomatic class, and between ages 16–22 years old participants in the Binge Eating/Purging class exhibited higher levels of leanness and muscularity concerns relative to the Asymptomatic class.
Figure 1.
Grid displaying the proportion of male participants presenting each latent class indicator by age period (row) and latent class (column) in the Growing Up Today Study. Note: The (%,n) for each plot corresponds to the percentage and number of repeated measures observations within each age period.
Participants classified to the Mostly Asymptomatic class (ages 13–15 and 23–26 years old; 3.5%–5.0%) were distinguished from the Asymptomatic class by their slightly greater prevalence of muscle-building product use, overeating, and muscularity concern. Finally, participants in the Muscularity Concerns class (ages 16–18 and 19–22 years old; 0.6%–1.0%) were distinguished by their high prevalence of muscularity concern and weekly use of muscle-building products.
Health correlates
Table 2 displays the model-estimated cases per 100 observations for each of the health correlates by age period and class. Overall, at each age period there were fewer estimated cases for the health correlates in the asymptomatic class relative to the four symptomatic classes. At ages 13–15 years old, the Body Image Disturbance class was distinguished from all other classes by its greater estimated incidence of obesity (e.g., 7 times greater incidence than the Asymptomatic class) and from the Asymptomatic and Mostly Asymptomatic classes by its higher prevalence of high depressive symptoms (47.2 cases compared to 0 cases [Asymptomatic] and 26.8 cases [Mostly Asymptomatic]). Compared to the Asymptomatic class, which had approximately 0 estimated cases of incident frequent binge drinking, prevalent drug use, and prevalent high depressive symptoms, the Mostly Asymptomatic class had much greater binge drinking incidence (9.5 cases per 100), drug use prevalence (8.1 cases), and high depressive symptoms prevalence (26.7 cases).
Table 2.
Estimated Number of Cases Presenting Health Correlates per 100 Observations by Eating Disorder Latent Class and Age Period Among Males in the Growing Up Today Study
| Estimated Cases per 100 Observations (Standard Error [SE])
|
Significant Group Differences (p<.01) | Overall Wald Chi-Square Test | |||||
|---|---|---|---|---|---|---|---|
| Asymptomatic (A) | Body Image Disturbance (B) | Binge Eating/Purging (C) | Mostly Asymptomatic (D) | Muscularity Concerns (E) | |||
| Ages 13–15 Years | |||||||
| Incident Obesity | 1.5 (0.7) | 10.4 (2.4) | 0.0 (0.0) | 1.7 (0.9) | -- | ACD < B | 272.34, p < 0.001 |
| Frequent Binge Drinking | |||||||
| Prevalence | 0.6 (0.8) | 3.2 (1.3) | 51.8 (25.8) | 2.8 (1.3) | -- | 7.17, p = 0.07 | |
| Incidence | 0.2 (1.4) | 1.9 (0.9) | 0.0 (0.0) | 9.5 (2.0) | -- | ABC < D | 178.80, p < 0.001 |
| Non-Marijuana Drug Use | |||||||
| Prevalence | 0.0 (0.0) | 10.1 (2.4) | 50.9 (36.0) | 8.1 (0.8) | -- | A < BD | 174.14, p < 0.0001 |
| Incidence | 5.2 (2.0) | 9.1 (6.1) | 0.0 (0.0) | 6.4 (3.3) | -- | C < ABD | 779.70, p < 0.0001 |
| High Depressive Symptoms | |||||||
| Prevalence | 0.0 (0.0) | 47.2 (3.9) | 51.0 (36.1) | 26.8 (2.1) | -- | A < C < B | 401.82, p < 0.0001 |
| Incidence | 11.1 (2.8) | 15.4 (10.0) | 11.2 (2.8) | 17.1 (6.1) | -- | A < C | 1282.78, p < 0.0001 |
| Ages 16–18 Years | |||||||
| Incident Obesity | 1.6 (0.2) | 4.3 (2.5) | 0.0 (0.0) | -- | 5.6 (4.0) | C < A | 154.89, p < 0.0001 |
| Frequent Binge Drinking | |||||||
| Prevalence | 12.0 (0.4) | 10.8 (2.4) | 48.8 (14.5) | -- | 25.3 (6.5) | 10.94, p = 0.01 | |
| Incidence | 15.7 (0.5) | 25.8 (3.9) | 42.9 (22.0) | -- | 19.9 (7.6) | 7.85, p = 0.05 | |
| Non-Marijuana Drug Use | |||||||
| Prevalence | 9.4 (0.4) | 14.6 (2.8) | 50.7 (20.2) | -- | 43.0 (7.5) | AB < E | 26.45, p < 0.0001 |
| Incidence | 11.4(0.5) | 16.1 (5.4) | 39.4 (36.3) | -- | 56.4 (15.7) | 9.44, p = 0.02 | |
| High Depressive Symptoms | |||||||
| Prevalence | 18.5 (0.6) | 52.0 (3.8) | 24.1 (19.0) | -- | 20.5 (6.2) | AE < B | 63.96, p < 0.0001 |
| Incidence | 13.2 (0.4) | 17.7 (8.3) | 37.9 (33.5) | -- | 6.8 (8.5) | 1.38, p = 0.71 | |
| Ages 19–22 Years | |||||||
| Incident Obesity | 2.6 (0.2) | 6.0 (1.5) | 0.0 (0.0) | -- | 1.9 (1.9) | C < AB | 231.40, p < 0.0001 |
| Frequent Binge Drinking | |||||||
| Prevalence | 36.2 (0.6) | 45.0 (2.4) | 72.3 (13.0) | -- | 62.9 (5.7) | A < BC, A < E | 38.52, p < 0.0001 |
| Incidence | 15.5 (0.5) | 15.6 (2.6) | 86.2 (40.7) | -- | 21.8 (8.7) | 3.54, p = 0.32 | |
| Non-Marijuana Drug Use | |||||||
| Prevalence | 20.4 (0.5) | 19.2 (2.7) | 53.3 (17.6) | -- | 24.4 (7.1) | 3.98, p = 0.26 | |
| Incidence | 18.0 (0.6) | 22.7 (3.2) | 53.7 (23.0) | -- | 64.9 (9.1) | A < E, B < E | 28.99, p < 0.0001 |
| High Depressive Symptoms | |||||||
| Prevalence | 21.0 (0.6) | 37.6 (3.2) | 57.6 (16.4) | -- | 10.1 (5.0) | E < BC, A < B | 32.38, p < 0.0001 |
| Incidence | 13.9 (0.6) | 20.3 (3.6) | 0.0 (0.0) | -- | 20.0 (8.1) | C < AB | 1301.32, p < 0.0001 |
| Ages 23–26 Years | |||||||
| Incident Obesity | 2.9 (1.5) | 0.0 (0.0) | 11.8 (7.7) | 4.6 (3.0) | -- | B < ACD | 116.39, p < 0.0001 |
| Frequent Binge Drinking | |||||||
| Prevalence | 33.7 (2.7) | 50.2 (7.6) | 41.0 (4.8) | 54.1 (4.1) | -- | A < D | 11.83, p < 0.01 |
| Incidence | 6.3 (2.5) | 12.9 (8.8) | 14.3 (9.2) | 6.9 (9.8) | -- | 0.80, p = 0.85 | |
| Non-Marijuana Drug Use | |||||||
| Prevalence | 30.1 (2.4) | 7.0 (1.3) | 51.8 (5.5) | 45.9 (4.9) | -- | B < A < CD | 903.07, p < 0.0001 |
| Incidence | 4.9 (4.0) | 19.7 (9.0) | 33.3 (11.0) | 38.0 (14.7) | -- | 8.42, p = 0.03 | |
| High Depressive Symptoms | |||||||
| Prevalence | 9.1 (1.9) | 0.0 (0.0) | 47.0 (5.0) | 31.0 (4.4) | -- | B < A < D < C | 653.26, p < 0.0001 |
| Incidence | 7.6 (2.4) | 6.6 (6.9) | 23.1 (11.5) | 7.4 (6.1) | -- | 1.67, p = 0.64 | |
Note: Results were calculated using the 3-step procedure for distal categorical outcomes in Mplus.
At ages 16–18 years old, the Muscularity Concerns class had more than four times the estimated prevalence of drug use of the asymptomatic class. Relative to the asymptomatic class, the Body Image Disturbance class had nearly three times the prevalence of high depressive symptoms. At ages 19–22 years old, the Body Image Disturbance class had higher prevalence of binge drinking and high depressive symptoms than the asymptomatic class, although it was not significantly different from the Binge Eating/Purging class on these health correlates. The Muscularity Concerns class had approximately three times greater incidence of drug use than the asymptomatic and Body Image Disturbance classes.
At ages 23–26 years old, the Binge Eating/Purging class had greater estimated prevalence of non-marijuana drug use and high depressive symptoms than the Asymptomatic and Body Image Disturbance classes. The Mostly Asymptomatic class had greater prevalence of binge drinking, non-marijuana drug use, and high depressive symptoms relative to the Asymptomatic class. Surprisingly, the Body Image Disturbance class reported lower incidence of obesity, prevalence of non-marijuana drug use, and prevalence of high depressive symptoms than the Asymptomatic class. However, it is possible that this apparent reversal in the direction of health disparities may be due to the smaller size of the Body Image Disturbance class in the 23–26-year-old period relative to the preceding age periods.
DISCUSSION
This study identified patterns of eating disorder symptoms in adolescent and young adult males that diverge from existing diagnostic criteria and are of clinical relevance. By age 22, 6% of participants were classified to the Body Image Disturbance class, which exhibited high risk for depressive symptoms across adolescence. This study also identified a subset of males in mid- to late-adolescence characterized by high levels of muscularity concern and weekly product use. Like the Binge Eating/Purging class, the Muscularity Concerns class was prone to drug use and frequent binge drinking. Relative to the Asymptomatic class, the Muscularity Concerns class had over four times the estimated prevalence of drug use at ages 16–18 years old, over three times as many participants starting to use drugs at ages 19–22 years old, and twice as many participants binge drinking frequently at ages 19–22 years old. Surprisingly, the analyses also detected a large, Mostly Asymptomatic class in early adolescence and young adulthood. Despite exhibiting only modestly greater muscularity concern, muscle-building product use, and overeating than the Asymptomatic class, the Mostly Asymptomatic class exhibited much greater binge drinking, drug use, and high depressive symptoms. Although the classes that emerged differ from similar analyses on female samples, the findings are consistent with research in females indicating that subclinical symptomatic patterns of eating disorder symptoms are also associated with concurrent and incident depressive symptoms and substance use.5
The findings have implications for risk assessment and screening. Previous research using diagnostic interviews and self-report assessments has found that males who exhibit eating disorder behaviors are less likely to report appearance concerns than females who exhibit eating disorder behaviors.6,9,30 Consistent with prior research, males in the Binge Eating/Purging class had low levels of body image concern. However, Body Image Disturbance and Muscularity Concerns classes also emerged, thus challenging the perception that appearance concerns are less relevant among males compared to females. The presentation of appearance concerns may be an indicator of greater risk for psychopathology.31 In the current study, appearance concerns were associated with elevated substance use and depressive symptoms, even when such appearance concerns did not co-occur with eating disorder behaviors. The findings highlight the importance of including cognitive, weight- and muscularity-focused symptoms as components of eating disorder risk assessment in males.4,32
By examining patterns of diverse appearance concerns and eating disorder behaviors from early adolescence through young adulthood, this study provides information on symptom heterogeneity that age-limited analyses might obscure. For example, the Muscularity Concerns class emerged in mid- to late-adolescence only. Because muscularity is linked to the embodiment of masculinity in Western cultures,7 it is possible that muscularity concerns are highest during developmental periods in which males are particularly vulnerable to social pressures to appear strong and masculine, such as in mid-adolescence when differences in physical development are more apparent, and later adolescence when they are entering adult roles (e.g., college, the work force).8,24,33–35 Whereas the Body Image Disturbance class was consistent in its high levels of leanness and muscularity concerns across all age periods, the Binge Eating/Purging class fluctuated in its presentation of body image concerns and eating disorder behaviors across ages, with purging and binge eating being most prevalent from ages 13–22 years old, and leanness and muscularity concerns being most prevalent between ages 16–22 years old. Such fluctuations across age could reflect developmental changes in the structure and phenomenology of the class across time. The variation could also be due to the small number of participants classified to the Binge Eating/Purging class from ages 13–22 years old.
The analysis of health correlates provided information about the clinical relevance of the symptomatic classes, and yielded insights into the potential underpinnings of eating disorder symptom patterns. Males in the Muscularity Concerns class reported higher concurrent and incident drug use than the Asymptomatic class. This trend is consistent with findings that product use may be connected to an overall vulnerability to use substances.36 In late adolescence and early adulthood, the Binge Eating/Purging class had greater concurrent binge drinking, drug use, and depressive symptoms than the Asymptomatic class. Given this behavioral and mental health profile, it is possible that males in the Binge Eating/Purging class are generally prone to impulsivity, emotional dysregulation, or engagement in maladaptive coping.37
There are limitations to note. The cohort is predominantly white and of restricted socioeconomic diversity, potentially limiting the generalizability of results. Data were collected via participant self-report, generally with single-item measures, thus the variables examined may be limited in depth (e.g., not assessing all dimensions of muscularity concern, not including compensatory exercise) and subject to reporting biases (e.g., under- or over-reporting). Although the patterns detected were consistent with existing theoretical and empirical literature, the LCA fit statistics did not consistently favor a specific latent class solution at each age period. However, because fit statistics are relative measures, and substantive meaning is also a critical piece of model selection, previous research discourages using fit statistics alone to determine LCA model solutions.19,38,39 In addition, although this study evaluated the clinical relevance of the classes by examining their associations with diverse health outcomes, the classes identified in this study may not have utility for predicting health outcomes not examined in this study, or those occurring outside the age periods studied.
Regardless of gender, many individuals with an eating disorder do not seek treatment, and even among those receiving treatment, the majority do not meet the full criteria for eating disorders specified in the DSM.40,41 This study underscores the importance of asking about concerns about leanness, muscularity, and use of muscle-building products when assessing eating disorder presentations that may be unique in males. Additional research, perhaps deploying taxometric methods and integrating clinical assessments of participants, is required in order to replicate the findings of this study and to further establish the validity and clinical relevance of the symptomatic classes.
Supplementary Material
Clinical Guidance.
Patterns of eating disorder presentations among males may diverge from existing diagnostic criteria. Ascertainment of eating disorders in adolescent and young adult males should include an assessment of appearance concerns and eating disorder behaviors that focuses on leanness, weight control (e.g., purging), and drive for muscularity (e.g., muscle-building supplement use).
Appearance concerns in males may focus on leanness or drive for muscularity. Even in the absence of co-occurring eating disorder behaviors, such appearance concerns are associated with elevated substance use and depressive symptoms.
Clinicians should be aware that adolescent males who exhibit high levels of muscularity concern and regularly use muscle-building products, and males who binge eat and purge may be particularly prone to drug use and frequent binge drinking.
Acknowledgments
The Growing Up Today Study (GUTS) was funded by National Institutes of Health (NIH) grants HD045763, HD057368, DK46834, HL03533, and MH087786. Dr. Calzo was supported by K01DA034753 from the National Institute on Drug Abuse (NIDA). Drs. Field, Horton, Crosby, and Micali were supported by R01MH087786 from the National Institute of Mental Health (NIMH).
The authors would like to thank the GUTS team of investigators and staff, and the thousands of young people across the country participating in GUTS.
Footnotes
Supplemental material cited in this article is available online.
The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Drs. Horton, Crosby, Swanson, and Calzo served as the statistical experts for this research.
Disclosure: Drs. Calzo, Horton, Sonneville, Swanson, Crosby, Micali, Eddy, and Field report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stice E, Burton EM, Shaw H. Prospective relations between bulimic pathology, depression, and substance abuse: unpacking comorbidity in adolescent girls. J Consult Clin Psychol. 2004;72:62–71. doi: 10.1037/0022-006X.72.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Field AE, Austin SB, Taylor CB, et al. Relation Between Dieting and Weight Change Among Preadolescents and Adolescents. Pediatrics. 2003;112(4):900–906. doi: 10.1542/peds.112.4.900. [DOI] [PubMed] [Google Scholar]
- 3.Crow SJ, Eisenberg ME, Story M, Neumark-Sztainer D. Suicidal behavior in adolescents: relationship to weight status, weight control behaviors, and body dissatisfaction. Int J of Eat Disord. 2008;41:81–87. doi: 10.1002/eat.20466. [DOI] [PubMed] [Google Scholar]
- 4.Field AE, Sonneville KR, Crosby RD, et al. Prospective associations of concerns about physique and the development of obesity, binge drinking, and drug use among adolescent boys and young adult men. JAMA Pediatrics. 2014;168(1):34–39. doi: 10.1001/jamapediatrics.2013.2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swanson SA, Horton NJ, Crosby RD, et al. A latent class analysis to empirically describe eating disorders through developmental stages. Int J Eat Disord. 2014;47(7):762–772. doi: 10.1002/eat.22308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Darcy AM, Lin IH-J. Are We Asking the Right Questions? A Review of Assessment of Males With Eating Disorders. Eating Disorders. 2012;20(5):416–426. doi: 10.1080/10640266.2012.715521. [DOI] [PubMed] [Google Scholar]
- 7.Pope H, Phillips KA, Olivardia R. The Adonis Complex: The Secret Crisis of Male Body Obsession. New York: Free; 2000. [Google Scholar]
- 8.Ricciardelli L, McCabe M. Eating disorders in boys and men. In: Smolak L, Levine MP, editors. The Wiley Handbook of Eating Disorders. Wiley-Blackwell; 2015. pp. 492–506. [Google Scholar]
- 9.Darcy AM, Doyle AC, Lock J, Peebles R, Doyle P, Le Grange D. The eating disorders examination in adolescent males with anorexia nervosa: How does it compare to adolescent females? Int J Eat Disord. 2012;45(1):110–114. doi: 10.1002/eat.20896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ricciardelli LA, Williams RJ, Kiernan MJ. Bulimic symptoms in adolescent girls and boys. Int J Eat Disord. 1999;26(2):217–221. doi: 10.1002/(sici)1098-108x(199909)26:2<217::aid-eat12>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 11.Micali N, De Stavola B, Ploubidis G, Simonoff E, Treasure J, Field AE. Adolescent eating disorder behaviours and cognitions: gender-specific effects of child, maternal and family risk factors. British Journal of Psychiatry. 2015;207(4):320–327. doi: 10.1192/bjp.bp.114.152371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, D.C: American Psychiatric Publishing; 2013. [Google Scholar]
- 13.Murray SB, Rieger E, Touyz SW, De la Garza García LY. Muscle dysmorphia and the DSM-V conundrum: Where does it belong? A review paper. Int J Eat Disord. 2010;43:483–91. doi: 10.1002/eat.20828. [DOI] [PubMed] [Google Scholar]
- 14.Calzo JP, Corliss HL, Blood EA, Field AE, Austin SB. Development of muscularity and weight concerns in heterosexual and sexual minority males. Health Psychol. 2013;32:42–51. doi: 10.1037/a0028964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Calzo JP, Sonneville KR, Haines J, Blood EA, Field AE, Austin SB. The development of associations among body mass index, body dissatisfaction, and weight and shape concern in adolescent boys and girls. J Adolesc Health. 2012;51(5):517–523. doi: 10.1016/j.jadohealth.2012.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCreary DR, Sasse DK. An exploration of the drive for muscularity in adolescent boys and girls. Journal of American College Health. 2000;48:297–304. doi: 10.1080/07448480009596271. [DOI] [PubMed] [Google Scholar]
- 17.Cafri G, Thompson JK. Measuring Male Body Image: A Review of the Current Methodology. Psychology of Men & Masculinity. 2004;5(1):18–29. [Google Scholar]
- 18.Murray SB, Griffiths S, Mond J. Evolving eating disorder psychopathology: conceptualising muscularity-oriented disordered eating. British Journal of Psychiatry. doi: 10.1192/bjp.bp.115.168427. In press. [DOI] [PubMed] [Google Scholar]
- 19.Masyn KE. Latent class analysis and finite mixture modeling. In: Little TD, editor. The Oxford Handbook of Quantitative Methods in Psychology. Vol. 2. New York: Oxford University Press; 2013. pp. 551–611. [Google Scholar]
- 20.Keel PK, Fichter M, Quadflieg N, et al. Application of a latent class analysis to empirically define eating disorder phenotypes. Arch Gen Psychiatry. 2004;61:192–200. doi: 10.1001/archpsyc.61.2.192. [DOI] [PubMed] [Google Scholar]
- 21.Crow SJ, Swanson SA, Peterson CB, Crosby RD, Wonderlich SA, Mitchell JE. Latent class analysis of eating disorders: relationship to mortality. J Abnorm Psychol. 2012;121:225–31. doi: 10.1037/a0024455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eddy KT, Le Grange D, Crosby RD, et al. Diagnostic classification of eating disorders in children and adolescents: how does DSM-IV-TR compare to empirically-derived categories? J Am Acad Child Adolesc Psychiatry. 2010;49(3):277–287. doi: 10.1016/j.jaac.2009.10.012. quiz 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peterson CB, Crow SJ, Swanson SA, et al. Examining the stability of DSM-IV and empirically derived eating disorder classification: implications for DSM-5. J Consult Clin Psychol. 2011 Dec;79(6):777–783. doi: 10.1037/a0025941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calzo JP, Masyn KE, Corliss HL, Scherer EA, Field AE, Austin SB. Patterns of body image concerns and disordered weight- and shape-related behaviors in heterosexual and sexual minority adolescent males. Developmental Psychology. 2015;51(9):1216–1225. doi: 10.1037/dev0000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999;25:195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 26.Cole TJ, Lobstein T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012 Aug;7(4):284–294. doi: 10.1111/j.2047-6310.2012.00064.x. [DOI] [PubMed] [Google Scholar]
- 27.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 28.Asparouhov T, Muthen B. Auxiliary variables in mixture modeling: three-step approaches using Mplus. Structural Equation Modeling. 2014;21(3):329–341. [Google Scholar]
- 29.Lanza S, Tan X, Bray B. Latent class analysis with distal outcomes: a flexible model-based approach. Structural Equation Modeling. 2013;20:1–26. doi: 10.1080/10705511.2013.742377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams RJ, Ricciardelli LA. Negative perceptions about self-control and identification with gender-role stereotypes related to binge eating, problem drinking, and to comorbidity among adolescents. Journal of Adolescent Health. 2003;32(1):66–72. doi: 10.1016/s1054-139x(02)00454-8. [DOI] [PubMed] [Google Scholar]
- 31.Grilo CM, Crosby RD, Masheb RM, et al. Overvaluation of shape and weight in binge eating disorder, bulimia nervosa, and sub-threshold bulimia nervosa. Behav Res Ther. 2009;47(8):692–696. doi: 10.1016/j.brat.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eisenberg ME, Wall M, Neumark-Sztainer D. Muscle-enhancing Behaviors Among Adolescent Girls and Boys. Pediatrics. 2012 Dec;130(6):1019–1026. doi: 10.1542/peds.2012-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kimmel M. Guyland: The Perilous World Where Boys Become Men. New York: Harper Collins; 2008. [Google Scholar]
- 34.Hunt CJ, Gonsalkorale K, Murray SB. Threatened masculinity and muscularity: An experimental examination of multiple aspects of muscularity in men. Body Image. 2013;10:290–9. doi: 10.1016/j.bodyim.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 35.Engeln R, Sladek MR, Waldron H. Body talk among college men: content, correlates, and effects. Body Image. 2013 Jun;10(3):300–308. doi: 10.1016/j.bodyim.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Hildebrandt T, Yehuda R, Alfano L. What can allostasis tell us about anabolic- androgenic steroid addiction? Dev Psychopathol. 2011 Aug;23(3):907–919. doi: 10.1017/S0954579411000393. [DOI] [PubMed] [Google Scholar]
- 37.Micali N, Ploubidis G, De Stavola B, Simonoff E, Treasure J. Frequency and patterns of eating disorder symptoms in early adolescence. J Adolesc Health. 2014;54(5):574–581. doi: 10.1016/j.jadohealth.2013.10.200. [DOI] [PubMed] [Google Scholar]
- 38.Marsh H, Hau K, Grayson D. Goodness of fit evaluation in structural equation modeling. In: Maydeu-Olivares, McArdle J, editors. Contemporary Psychometrics. Mahway, NJ: Lawrence Erlbaum Associates, Inc; 2005. pp. 275–340. [Google Scholar]
- 39.Nylund K, Asparouhov T, Muthen B. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–569. [Google Scholar]
- 40.Le Grange D, Swanson SA, Crow SJ, Merikangas KR. Eating disorder not otherwise specified presentation in the US population. Int J Eat Disord. 2012 Jul;45(5):711–718. doi: 10.1002/eat.22006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and Correlates of Eating Disorders in Adolescents: Results From the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.