ABSTRACT
Low measles, mumps and rubella (MMR) immunization levels in European children highlight the importance of identifying determinants of parental vaccine uptake to implement policies for increasing vaccine compliance. The aim of this paper is to identify the main factors associated with partial and full MMR vaccination uptake in European parents, and combine the different studies to obtain overall quantitative measures. This activity is included within the ESCULAPIO project, funded by the Italian Ministry of Health. ORs and CIs were extracted, sources of heterogeneity explored and publication bias assessed. Forty-five papers were retrieved for the qualitative study, 26 of which were included in the meta-analysis. The following factors were associated with lower MMR vaccine uptake: misleading knowledge, beliefs and perceptions on vaccines (OR 0.57, CI 0.37-0.87); negative attitudes and behaviors toward vaccination (OR 0.71, CI 0.52-0.98); demographic characteristics, such as different ethnicity in Southern populations (OR 0.44, CI 0.31-0.61), higher child's age (OR 0.80, CI 0.76-0.85); low socio-economic status (OR 0.64, CI 0.51-0.80), especially low income (OR 0.39, CI 0.25-0.60) and education (OR 0.64, CI 0.48-0.84), high number of children (OR 0.54, CI 0.42-0.69), irregular marital status (OR 0.80, CI 0.66-0.96). The factors explaining heterogeneity were country location, administration modality, collection setting and responses reported on MMR alone or in combination. Findings from this study suggest policy makers to focus communication strategies on providing better knowledge, correct beliefs and perceptions on vaccines, and improving attitudes and behaviors in parents; and to target policies to people of ethnic minority from Southern Europe, low educated and deprived, with higher number of children and non-married marital status.
KEYWORDS: determinant, measles, mumps and rubella, parents, vaccine, uptake
Introduction
Measles, mumps and rubella (MMR) are serious diseases that can cause significant morbidity and lead to potentially fatal illness, disability and death.1 Despite the introduction of the trivalent MMR vaccine in the 1970s, measles is still circulating in several regions of Europe, mainly in the form of recurring spatially localized epidemics, with 4,284 cases reported during the recent 12-month period (June 2014 – May 2015) in 30 EU/EEA Member States,2 77% of which in unvaccinated subjects, and 15.5% in vaccinated with 1 dose. The low immunization levels found in Europe highlight the importance of identifying and understanding the factors that affect the uptake of recommended childhood immunizations,3 to address proper interventions and implement public health policies aimed at increasing vaccine compliance. Uptake could be improved by understanding and modifying the complex structures that are behind vaccination decisions.4 Different studies have been carried out to elicit parental concerns about MMR vaccinations. Recent reviews analyzed factors underlying parental decisions,4,5 demonstrating that vaccine-acceptors and vaccine-decliners do think differently on a number of factors, such as effectiveness or safety of the vaccine, trust in health professionals, media and government, need of better information.
Although many qualitative reviews exist in the literature, to our knowledge there is a lack of meta-analyses that could investigate parental MMR vaccine predictors by systematically combining results from different studies. The present paper aimed at identifying the main factors associated with partial and full MMR vaccination uptake in European parents, and performing a meta-analysis of the main classes of factors predicting parental MMR vaccine catch-up. This activity was included within the ESCULAPIO project, funded by the Italian National Centre for Disease Prevention and Control of the Ministry of Health (CCM), with the main objective of implementing targeted campaigns and planning effective strategies to increase vaccine coverage.
Results
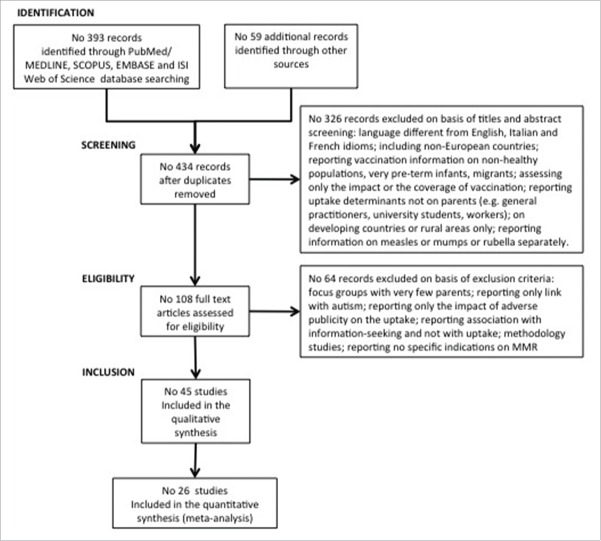
An initial number of 452 articles was retrieved; no. 434 records were obtained after excluding duplicates, and through the initial screening of titles and abstracts no. 108 full text articles were assessed for eligibility (Fig. 1). A total of 45 studies met all the inclusion criteria and were then included in the qualitative synthesis (Table 1);3,6-49 out of the 32 quantitative studies retrieved, no. 26 reported ORs and CIs and then were included in the meta-analysis.3,6,7,9-11,14-17,19,21,23-27,29,31,33,34,37,38,40,42,48
Figure 1.
Flow diagram of the systematic literature review process on the determinants of European parents' decision of vaccinating their children against measles, mumps and rubella.
Table 1.
Studies selected through the systematic review of the underlying determinants of European parents' decision on vaccinating their children against measles, mumps and rubella (MMR).
| Ref. Article | Publication year | Study year | Country | Sample size | Children's age | Data collection method | Administration modality | Administration setting | Vaccine | MMR specific yes/no | Vaccine schedule adherence | Qualitative / Quantitative study | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Lernout T6 | 2014 | 2012 | Belgium | 874 | 18–24 mo | questionnaire | IW | home (face-to-face) | MMR and DTP | yes | partial | quantitative (included in the meta-analysis) |
| 2 | Robert E7 | 2014 | 2012 | Belgium | 519 (in Wallonia); 538 (in Brussels) | 18–24 mo | interview | IW | home (face-to-face) | MMR in a schedulea | no | partial | quantitative (included in the meta-analysis) |
| 3 | Harmsen IA8 | 2013 | 2011 | The Netherlands | 60 | 0–4 y | focus groups: semistructured protocol with open-ended questions. Digital voice recorded and transcribed verbatim | IW | antroposophical child welfare centers | MMR in a scheduleb | no | NS | qualitative |
| 4 | Pavlopoulou ID9 | 2013 | 2010–2011 | Greece | 731 | 0–65 mo | interview | IW | home (telephone) | MMR in a schedulec | no | full and partial | quantitative (included in the meta-analysis) |
| 5 | Pearce A3 | 2013 | 2003–2007 | UK | 751 | 5 y | interview | IW | home (face-to-face) | MMR | yes | full and partial | quantitative (included in the meta-analysis) |
| 6 | van Lier A10 | 2013 | 2009 | The Netherlands | 180,456 | 0–14 mo | Country of birth were taken from Præventis (2 October 2009); proxy for SES from The Netherlands Institute for Social Research; proxy of religious objection to vaccination from municipal offices. | NA | official records | MMR in a scheduled | yes | full | quantitative (included in the meta-analysis) |
| 7 | Bouhamam N11 | 2012 | 2009–2010 | France | 375 | 9 mo - 7 y | questionnaire | IW | hospital (face-to-face) | MMR in a schedulee | yes | full | quantitative (included in the meta-analysis) |
| 8 | Brown K12 | 2012 | 2008/2009 | UK | 24 | 11 mo-3.5 y | interview | IW | home (face-to-face and telephone) | MMR | yes | full and partial | qualitative |
| 9 | Kriwy P13 | 2012 | 2001 | Germany | 464 | NS | interview | IW | home (face-to-face) | MMR | yes | full | quantitative |
| 10 | Mollema L14 | 2012 | 2006–2007 | The Netherlands | 1,744 | 0–10 y | questionnaire | SA | home | MMR in a schedulef | no | partial | quantitative (included in the meta-analysis) |
| 11 | Schönberger K15 | 2012 | 2002–2005 | Germany | 1,774 | < 4 y | interview | IW | home (telephone) | MMR | yes | full and partial | quantitative (included in the meta-analysis) |
| 12 | Brown K16 | 2011 | 2008–2010 | UK | 284 | 5–18 y | questionnaire | SA | home (postal) | MMR | yes | full | quantitative (included in the meta-analysis) |
| 13 | Brown K17 | 2011 | 2009 | UK | 373 | 5–18 y | questionnaire | SA | home (postal) | MMR | yes | full and partial | quantitative (included in the meta-analysis) |
| 14 | Coniglio MA18 | 2011 | 2008 | Italy | 1,218 | 3–5 y | questionnaire | SA | day-care center | MMR in a scheduleg | no | NS | quantitative |
| 15 | Sakou I-I19 | 2011 | 2009 | Greece | 1,005 | 14 y | questionnaire | IW | hospital (face-to-face) | MMR in a scheduleh | no | full | quantitative (included in the meta-analysis) |
| 16 | Babatsikou F20 | 2010 | NS | Greece | 304 | 0–12 y | questionnaire | SA | day-care centers and primary schools | MMR in a schedulei | no | NS | quantitative |
| 17 | Danis K21 | 2010 | 2006 | Greece | 2,950 | 6 y | questionnaire | SA | school | MMR in a schedulel | no | full | quantitative (included in the meta-analysis) |
| 18 | Gardner B22 | 2010 | 2008 | UK | 28 | < 6 y | Focus group discussions informed by a booklet and transcribed verbatim | NA | primary care trust | MMR | yes | NA | qualitative |
| 19 | Jessop LJ23 | 2010 | 2001–2004 | Ireland | 556 | 5 y | questionnaire | SA | hospital | MMR | yes | partial | quantitative (included in the meta-analysis) |
| 20 | Borràs E24 | 2009 | 2003–2004 | Spain | 630 | < 3 y | questionnaire | IW | home (telephone) | MMR in a schedulem | no | partial | quantitative (included in the meta-analysis) |
| 21 | Borràs E25 | 2009 | 2003–2005 | Spain | 630 | < 3 y | questionnaire | IW | home (telephone) | MMR in a schedulen | no | partial | quantitative (included in the meta-analysis) |
| 22 | Pearce A26 | 2008 | 2000–2002 | UK | 13,826 | 9 mo - 3 y | interview | IW | home (face-to-face) | MMR | yes | full and partial | quantitative (included in the meta-analysis) |
| 23 | Theeten H27 | 2009 | 2005 | Belgium | 792 | 7 y | questionnaire | IW | home (face-to-face) | MMR in a scheduleo | yes | full | quantitative (included in the meta-analysis) |
| 24 | Vandermeulen C28 | 2008 | 2005 | Belgium | 3,490 | <18 y | questionnaire | IW | home (face-to-face) | MMR | yes | full | qualitative |
| 25 | Mixer RE29 | 2007 | 2003 | UK | 6,444 quantitative study; 37 qualitative study | 18 mo - 3 y | For quantitative study: ethnicity data from Brent Primary Care Trust database. For qualitative study: focus groups and interviews transcribed verbatim. A questionnaire on socioeconomic status was filled in | For ethnicity: records. For qualitative study: IW | primary care trust (face-to-face and records) | MMR | yes | partial | quantitative (included in the meta-analysis) and qualitative |
| 26 | Smith A30 | 2007 | 1996–2006 | UK | 1,004 | < 36 mo | interview | IW | home (face-to-face) | MMR | yes | NA | qualitative |
| 27 | Theeten H31 | 2007 | 2005 | Belgium | 1,349 | 18–24 mo | interview and questionnaire | IW | home (face-to-face) | MMR in a schedulep | yes | partial | quantitative (included in the meta-analysis) |
| 28 | Casiday R32 | 2006 | 2004 | UK | 87 | < 4 y | questionnaire | SA | home (postal) | MMR | yes | NS | quantitative |
| 29 | Cassell JA33 | 2006 | 2004 | UK | 413 | 15–24 mo | questionnaire | SA | home (postal) | MMR | yes | full | quantitative (included in the meta-analysis) |
| 30 | Paulussen TG34 | 2006 | 1999 | The Netherlands | 491 | 0–4 y and 9–10 y | questionnaire (computer-based) | SA | home | MMR in a scheduleq | no | full | quantitative (included in the meta-analysis) |
| 31 | Wright J35 | 2006 | 1993–2004 | UK | 303 | < 2 y | official records | NA | NA | MMR | yes | NS | quantitative |
| 32 | Dannetun E36 | 2005 | 2003 | Sweden | 203 | < 4 y | questionnaire | SA | home (telephone) | MMR | yes | NS | qualitative |
| 33 | Gellatly J37 | 2005 | 2003–2004 | UK | 105 | 1–56 mo | questionnaire | IW | nursery (face-to-face) | MMR | yes | full | quantitative (included in the meta-analysis) |
| 34 | Hak E38 | 2005 | 1999 | The Netherlands | 150 | 3 mo - 5 y | focus group interview and questionnaire | SA | day-care center | MMR in a scheduler | no | full | quantitative (included in the meta-analysis) |
| 35 | Alfredsson R39 | 2004 | 1999 | Sweden | 250 | < 4 y | questionnaire | SA | home (postal) | MMR | yes | NS | qualitative |
| 36 | Flynn M40 | 2004 | 1997–1998 | UK | 511 | 2 y | questionnaire | SA | home (postal) | MMR | yes | NS | quantitative (included in the meta-analysis) |
| 37 | McMurray R41 | 2004 | 2002–2003 | UK | 69 | 4–5 y | interview | IW | home (face-to-face) | MMR | yes | NS | qualitative |
| 38 | Petrovic M42 | 2003 | 1997 | UK | NA | NA | questionnaire | SA | home (postal) | MMR | yes | full | quantitative (included in the meta-analysis) |
| 39 | Smailbegovic MS43 | 2003 | 2000–2001 | UK | 76 | 0–18 mo | questionnaire | SA | home | MMR in a schedules | yes | NS | qualitative |
| 40 | Alonso JAN44 | 2002 | 2000 | Spain | NS | NS | questionnaire | SA | home (postal) | MMR in a schedulet | no | NS | qualitative |
| 41 | Ramsay ME45 | 2002 | 2001 | UK | 1,013 | <3 y | interview | IW | home (face-to-face) | MMR | yes | NS | qualitative |
| 42 | Evans M46 | 2001 | NS | UK | 48 | 14 mo-3 y | focus groups with interviews | NA | community hall | MMR | yes | NS | qualitative |
| 43 | Swennen B47 | 2001 | 1999 | Belgium | 1,005 (Flanders), 835 (Wallonia) | 18–24 mo | interview | IW | NS | MMR in a scheduleu | no | NS | qualitative |
| 44 | Impicciatore P48 | 2000 | 1997 | Italy | 1,035 | <6 y | questionnaire | IW | shopping centers and parks (face-to-face) | MMR | yes | full | quantitative (included in the meta-analysis) |
| 45 | Pareek M49 | 2000 | NS | UK | 300 | <36 mo | questionnaire | SA | home (postal) | MMR | yes | full | quantitative |
4 doses hexavalent, 3 doses pneumococcal, 1 dose MMR,1 dose MenC.
MMR, DTP/DTaP, OPV/IPV, Hib, HBV
MMR, DTaP-IPV, Hib, Men C
polio, DTP, MMR, Hib, MenC, HBV, HPV
2 doses MMR, diphtheria, tetanus, poliomyelitis, Hib, pertussis, tuberculosis, pneumococcal, HBV
polio, DTP, MMR, Hib, MenC, HBV, pneumococcal, HPV
IPV, DT, HBV, MMR, pertussis, varicella, pneumococcal, Hib
The adolescent booster dose (6th dose) Td or Tdap, 5 or more doses polio, 3 or more doses HBV, 2 doses HAV, 2 doses MMR, 1 dose MenC
5 doses DTP, 5 doses polio, 2 doses MMR, 3 doses HBV; MMR available at that time, if they had received 1 dose, at the age of >12 months, and the booster at the age> 10 y; 4 doses Hib if the first dose was administered at the age of 0–6 months and the 4th at the age of > 12 months; alternatively for Hib, 3 doses if vaccination began at the age of 7–11 months and the 3rd dose was administered at the age of > 12 months, or 2 doses if the first dose was administered at the age of 12–14 months or 1 dose if Hib vaccination was administered at the age of > 15 months.
5 doses DTP, 5 doses polio, 2 doses MMR, 3 doses HBV, full vaccination for Hib
4 DTPa/w doses, 4 Hib doses, 4 OPV doses, 3 MenC doses and 1 MMR dose
4 DTP, 4 OPV, 1 MMR, and the necessary doses of Hib and MenC
OPV, DTP, HBV, MMR, MenC and booster DT-IPV
4 doses IPV, DTP and Hib, 3 doses HBV and 1 dose MMR and MenC
4 injections of a combined vaccine for diphtheria, tetanus, pertussis and poliomyelitis (DPeTPo), 2 injections with a combined vaccine for diphtheria, tetanus and poliomyelitis (DT-Po), 4 injections with a conjugated vaccine for Hib, 2 injections with a combined MMR vaccine (MuMeR).
DPTP, Hib, MMR, MenC, diphtheria, tetanus and polio, a-cellular pertussis
BCG, pertussis, polio, Hib, MenC, MMR
DTP, OPV, Hib, MMR
polio, DTP, Hib, HBV, MMR
Abbreviations
DTP:diphtheria-tetanus-pertussis; DTaP or Tdap: diphtheria-tetanus-acellular pertussis; DT or Td: diphtheriatetanus
MenC: Meningococcus C
OPV/IPV: Oral polio vaccine/Inactivated polio vaccine
Hib: Haemophilus influenzae type b
HBV: hepatitis B
HPV: human papillomavirus
HAV: hepatitis A
BCG: Bacillus Calmette-Guerin
The characteristics of the retrieved studies are reported in Table 2, and Fig. 2 shows the frequency of factors reported in the retrieved articles.
Table 2.
Characteristics of the retrieved 45 articles on the determinants of European parental decision of vaccinating their children against measles, mumps and rubella (MMR).
| Study characteristics | No. | % |
|---|---|---|
| Data collection method | ||
| • Questionnaires | 28 | 62 |
| • Interviews | 12 | 27 |
| • Focus groupsa | 5 | 11 |
| • Official records | 3 | 7 |
| Administration modalityb | ||
| • Interviewer-administered | 23 | 51 |
| • Self-administered | 18 | 40 |
| Data collection setting | ||
| • Home | 29 | 64 |
| • Hospital/nursery/primary care trust | 6 | 13 |
| • Day-care centers/Schools | 4 | 9 |
| • Otherc | 3 | 7 |
| Geographical location | ||
| • Northern Europed | 22 | 49 |
| • Western Europee | 14 | 31 |
| • Southern Europef | 9 | 20 |
| Questionnaires reporting on | ||
| • MMR vaccine alone | 31 | 69 |
| • MMR plus other vaccines included in the local schedule | 14 | 31 |
| MMR vaccine schedule adherence | ||
| • All recommended doses | 15 | 33 |
| • 1 dose | 8 | 18 |
| • Both | 6 | 13 |
| Children's age at the moment of the study | ||
| • ≤ 5 y | 30 | 67 |
| • > 5 y | 3 | 7 |
| • Mixed age | 9 | 20 |
using semi-structured protocol with open-ended questions, questionnaires or interviews, or discussions, recorded and transcribed
delivered by post, by telephone or by hand, or face-to-face interviews
anthroposophical child welfare centers, community halls, shopping centers and parks
19 studies in UK, 2 in Sweden, 1 in Ireland
6 studies in Belgium, 5 in The Netherlands, 2 in Germany, 1 in France
4 studies in Greece, 3 in Spain, 2 in Italy
Figure 2.
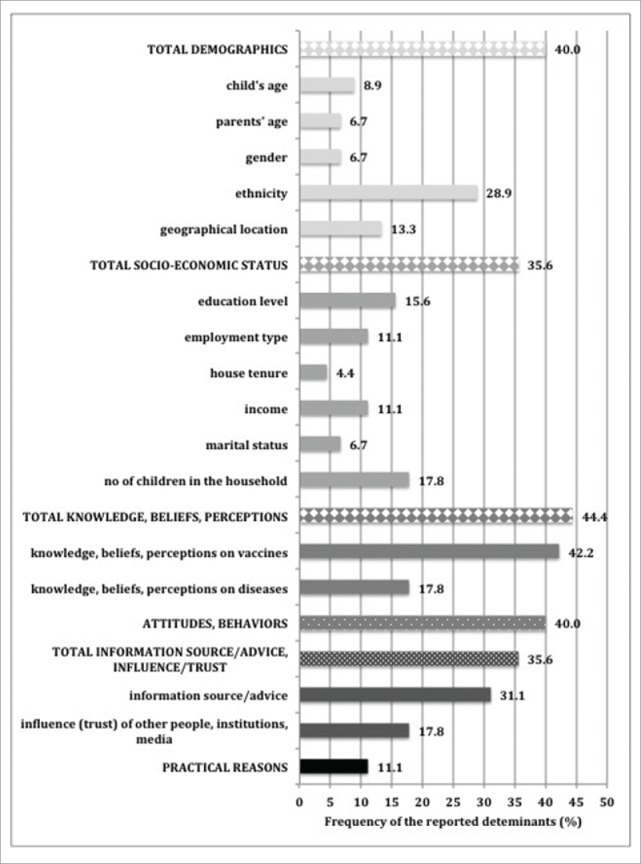
Determinants of European parents' decision on the vaccination of their children against measles, mumps and rubella, reported in the retrieved 45 articles.
Quantitative analysis
Knowledge, beliefs, perceptions on vaccines and diseases (KBPvd)
Nine studies reported 22 population samples having both good and misleading KBPvd.3,14-16,24,34,37,38,40 The analysis showed no clear effect for the overall population of parents. Since high heterogeneity was present between the studies, a random effect model was used for the subgroup analysis. After eliminating the outliers, i.e. 1 sample from Brown et al.,16 2 populations from Hak et al.38 1 from Paulussen et al.,34 and 1 from Schönberger et al.,15 and performing the subgroup analysis, a clear and significant effect was revealed for the group of the KBPv (OR 0.57, CI 0.37 to 0.87) compared to the group on diseases, which tended, instead, to have better knowledge, beliefs, perceptions and then to be more likely to vaccinate (OR 1.62, CI 1.32–1.99) (Fig. 3). In this last group a low between study heterogeneity was revealed (I2 38.5% p = 0.181). Lower KBPvd were also observed for parents filling self-administered questionnaires (OR 0.34, CI 0.13–0.86) and parents from Western countries (OR 0.60, CI 0.38–0.93).
Figure 3.
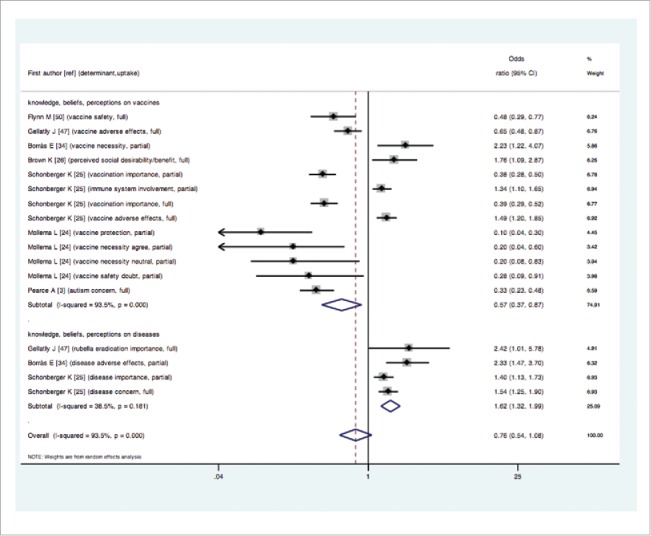
Forest plot of the overall effect (showed as exponentiated Odds Ratios and Confidence Intervals) of parental knowledge, beliefs and perceptions (KBP) on measles, mumps and rubella vaccine uptake, examined by KBP on vaccines and on diseases.
Attitudes/behaviors
Positive or negative attitudes/behaviors toward vaccinations were reported in 11 studies showing 20 population samples.6,17,23,25-27,31,33,34,40,48 After eliminating outliers,34,40 overall negative attitudes and behaviors toward vaccination were found out, that took to decreasing vaccination choices (fixed effect OR 0.79, CI 0.73–0.86; random effect OR 0.71, CI 0.52–0.98). The effect was due to interviewer-administered (IW) questionnaires (OR 0.61, CI 0.40–0.94), in particular IW face-to-face (OR 0.54, CI 0.35–0.83), and Western European countries (OR 0.40, CI 0.25–0.66).
Demographics
Ethnicity, child's age, and gender were the demographic considered factors
With regard to ethnicity, the overall effect was a slightly decreased likelihood of vaccinating their children from parents of ethnic minorities than the majority in the fixed effect model (OR 0.89, CI 0.86–0.93), but this effect disappeared in the random effect (OR 1.03, CI 0.79–1.34). In Northern countries, a higher vaccination uptake was revealed (OR 1.74, CI 1.25–2.42), compared to the parents from Southern countries (OR 0.44, CI 0.31–0.61), while in Western European parents there was no significant effect (Fig. 4).
Figure 4.
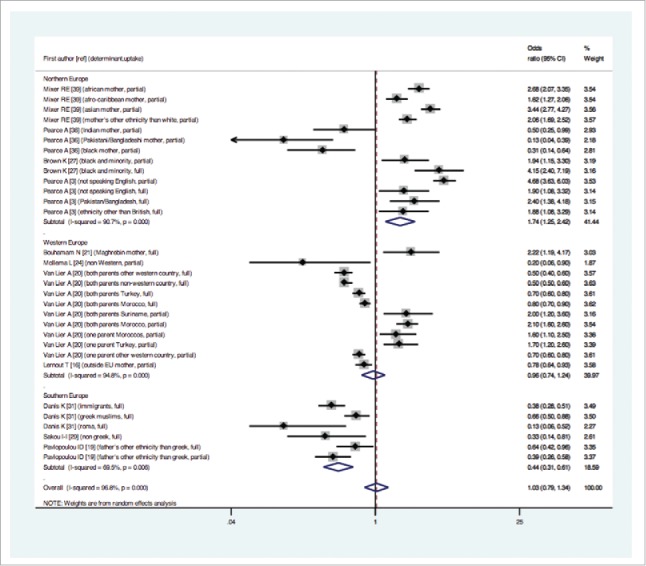
Forest plot of the overall effect (showed as exponentiated Odds Ratios and Confidence Intervals) of parental ethnic minority on measles, mumps and rubella vaccine uptake, examined by study geographical location.
When analyzing responses to MMR vaccine and MMR plus other vaccines in local schedules, parents who provided non-specific responses were less prone to vaccinate and the heterogeneity was lower (OR 0.42, CI 0.30 to 0.58; I2 66.7% p = 0.006) compared to those who provided specific answers on MMR vaccine (OR 1.26, CI 1.07–1.44).
Child's age was in the direction that the higher the age the lower the vaccination uptake (OR 0.80, CI 0.76–0.85 both fixed and random). Female gender tended to be vaccinated less (OR 0.57, CI 0.56–0.58 fixed effect); in the random effect model no significant effect was observed.
Socio-economic status (SES)
Twenty-four samples of parents from 9 papers3,7,11,21,23,25-27,38 reported an association between vaccine uptake and SES. The overall effect indicated that the lower the SES, the lower the vaccination uptake both in the fixed and random effect models (OR 0.82, CI 0.77–0.87 and OR 0.64, CI 0.51–0.80, respectively).
Income and education level were the responsible of the observed effect, with less than double and a half likelihood of vaccinating for parents with lower incomes (OR 0.39, CI 0.25–0.60) and lower likelihood for parents with lower education level (OR 0.64, CI 0.48–0.84) (Fig. 5). A stronger effect, moreover, was showed for Western European countries (OR 0.33, CI 0.24–0.45), which showed also homogeneity between studies (I2 0.0%, p = 0.889).
Figure 5.
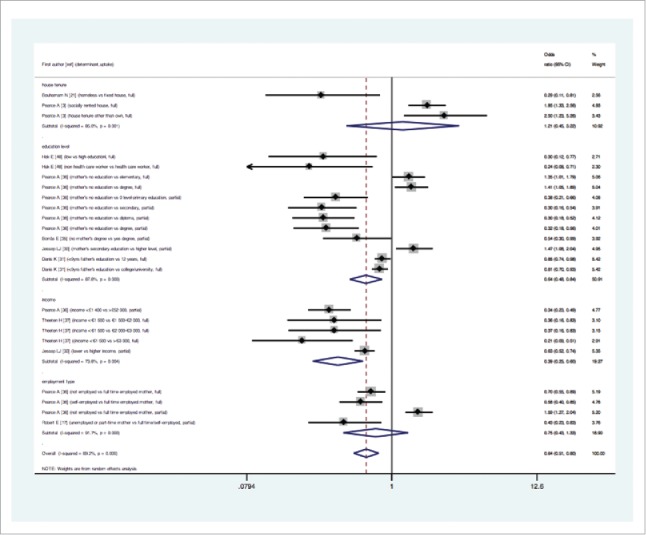
Forest plot of the overall effect (showed as exponentiated Odds Ratios and Confidence Intervals) of parental socio-economic status on measles, mumps and rubella vaccine uptake, examined by specific socio-economic determinants.
Employment and house tenure did not show significant effect. With regard to the income, studies were homogeneous for the home setting, IW face-to-face (I2 0.0% p = 0.890) and Western Europe (I2 0.0% p = 0.730). The non-married status (i.e., single, divorced, co-habiting, homosexual partnership) was a barrier to vaccination (OR 0.80, CI 0.66–0.96; I2 64,6% p = 0.059 random effect model). The higher was the no. of children in the household, the lower was the uptake (fixed effect OR 0.70, CI 0.66–0.75; random effect OR 0.54, CI 0.42–0.69).
Information source/advice
Eleven population samples from 6 studies reported ORs and CIs of information sources/advice.7,15,17,37,42,48 The information source is often lacking or insufficient, as well as the advice from GP or other health practitioners, this leading to an overall lower vaccination uptake (OR 0.75, CI 0.67–0.84 fixed effect model); in the random effect model no clear effect was showed.
In the subgroup analysis, the administration method revealed opposite directions: parents answers to IW by telephone demonstrated a less likelihood of vaccinating (OR 0.53, CI 0.43–0.64), and studies were moderately heterogeneous (I2 54,7% p = 0.085); parents responding to an IW by face-to-face were 3 times more prone to vaccinate (OR 3.12, CI 2.24–4.34) and studies were quite homogeneous (I2 30.9%, p = 0.227); self-administered (SA) postal had not a clear direction (Fig. 6).
Figure 6.
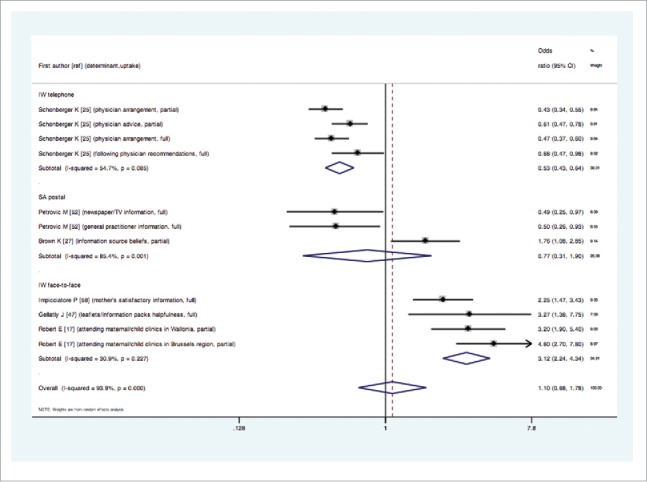
Forest plot of the overall effect (showed as exponentiated Odds Ratios and Confidence Intervals) of parental information source/advice opinions on measles, mumps and rubella vaccine uptake, examined by administration modality.
Influence or trust of other people, institutions, media
Four articles with 6 population samples16,38,43 reported that natural practitioners/naturopaths did not influence decisions of parents to vaccinate their children, and they had faith in media and in the medical profession, so that the total effect was a general positive influence from other people or institutions and media, in the fixed effect model (OR 1.94, CI 1.53–2.46), while the random effect model did not show a clear direction. The subgroup analysis did not reveal any particular effect, also because of the low number of the studies.
Discussion
This review and meta-analysis summarize evidence on the factors underlying parental decisions about single and combined MMR vaccines uptake for their children in Europe.
To our knowledge, this is the first meta-analysis study regarding the MMR vaccination uptake in European populations of parents. Although this poses some limits to the possibility of comparing our results with data from other authors, it provides new insights in the overall parental decision on vaccinating their children from a quantitative point of view.
The qualitative analysis showed that most parents are not totally directed to one clear attitude toward vaccination, and this, in line with Brown et al.,4 highlights the multifaceted nature of their choice. However, robust indications emerge from the quantitative analysis, evidencing specific variables underlying parental decision to vaccinate their children.
Results from the meta-analysis revealed opposite effects for overall KBPv compared to those regarding diseases. The first were misleading and drove parents to a lower vaccination uptake, while the second appeared more positive and correct; this could be related to the very wide claim that because some diseases are becoming less prevalent, people's perceptions and knowledge about their dangers are being altered, and hence their vaccine uptake rates are affected. These results are partially in line with reviews stating that public debate over the MMR vaccine safety in several countries persists, and this underpins most hesitant attitudes.1,50
Some characteristics emerged negatively associated with parents' choices, such as the KBPvd reported in SA questionnaires or referred to Western European countries.
Similar considerations have to be done also for the attitudes and behaviors, which were frequently reported uptake determinants. When investigating the overall population, negative attitudes and behaviors were prevalent, decreasing to the half the vaccination uptake of parents. From the subgroup analysis, the same negative effect was found in IW face-to-face questionnaires and Western countries. Attitudes and behaviors are often likely consequences of misleading information; thus our results suggest, in line with other studies,4,50 that interventions should be focused on better communication strategies that could provide parents with clear messages specifically on vaccines, in order to build right KBP and create correct attitudes and behaviors. These messages should be addressed mainly to vaccine efficacy, safety, bad side effects/consequences, health protection, necessity; and focusing on the importance of the compliance with the second dose of the MMR vaccine. Still some concern exists with regard to the link between vaccine and autism, thus messages to parents should clearly expose the last scientific literature denial on such a link and the possible mechanisms underlying the real upset of the autism.51
Demographics are important and frequently reported factors influencing parental choices, and the quantitative specific results on the ethnicity suggest that communication strategies should be targeted on parents of ethnic minority, living particularly in Southern countries of Europe. This result is difficult to explain; probably people of minor ethnicity in UK (the only Northern country represented in the articles about demographics) are more integrated and then more informed about vaccination benefits.
Our analysis suggests that communication strategies should be addressed also to lower SES families, in particular to those families with low income and low education level. Parents having high incomes have more than twice likelihood of vaccinating their kids, and those with high education levels have one and a half likelihood. Higher education is a determinant for positive vaccination uptake particularly for partial vaccine adherence, home environment, IW questionnaires/interviews and non-specific MMR vaccine intentions. Parents coming from Western countries are 3 times more prone to vaccinate, with homogeneity confirming the consistency of the studies. Moreover, having a numerous family and a non-married status are barriers for vaccination, this suggesting that interventions should be targeted to these types of families. These results are in line with other studies.4,31,52
An overall lack of information source or advice is revealed in the quantitative analysis when using a fixed effect model, taking parents to a general decision of non-vaccinating their own children, but this is not confirmed in the random effect models. Both the literature and market research data confirmed that advice from healthcare professionals is the main and most influential source of vaccination information for most people.5,50 Even though professionals report difficulties in building trustful relationships with patients,50 in our meta-analysis parents complain about the physician or GP not giving advice for vaccination. They also criticize scarce television and newspapers information. This suggests that GP and the other health practitioners should be adequately informed in order to better transfer knowledge to parents. Full information packs about vaccinations should be distributed, and mass media information should be fortified. On the other hand, when answers are provided via face-to-face interviews and within an environment different from home, the overall effect is opposite, with parents more disposed to vaccinate their children of 3 times and 2 and a half times respectively. It may be hypothesized that the presence of an interviewer and an environment different from own home could take parents to answer positively toward vaccination choices, even though this cannot be verified.
The concept of information trust and advice is linked with the influence exercised by other people, institutions and media. Even though the analysis through the fixed effect model revealed an overall positive influence of other people, institutions and media, and an overall lacking or insufficient information source and advice from GP or other health practitioners, a robust effect could not be demonstrated when using the random effect model.
Among the considered variables, the quality of the articles was fair or good, this showing that studies were reliable, and no evidence was showed that the findings differed systematically for fair or good quality studies. Similarly, vaccine schedule adherence, children's age at the moment of the study and data collection method (interview, questionnaire, official database) did not influence the results of the meta-analysis. The following factors, instead, were found mostly explaining the heterogeneity between studies: specificity of the response on vaccines, country location, administration modality, and setting.
As showed by the UNICEF and WHO,53 evidence suggests that uptake varies by vaccine, therefore parents may not make decisions about the entire vaccine schedule, but rather about individual vaccines. Our meta-analysis confirms that in some cases parents make different decisions with regard to responses on MMR vaccine alone or MMR plus other vaccines included in the local schedule. E.g. parents of ethnic minority are disposed to vaccinate for MMR diseases and are not for other vaccines included in a schedule; conversely, parents with high education levels look like more inclined to vaccinate when they answer on the combination vaccines rather than on the specific MMR one. Anyway, a common consistent direction was not revealed through our meta-analysis when parental responses were about combination vaccines rather than specific MMR vaccine; this is not in line with results from Brown et al 4, who stated that there were consistent and significant relationships between negative perceptions of combination vaccines (e.g. belief in safety/preferability of separate vaccines and fear of immune overload) and lower vaccine uptake, and qualitative evidence that these issues were more influential in MMR decisions than in decisions about other combination vaccines.
With regard to country location, parents from Western areas have generally misleading KBPv and more negative attitudes/behaviors, and then are less prone to vaccinate their children, compared to parents from Northern countries, that are more prone to vaccinate. The IW administration modality is mostly negatively influencing vaccine uptake, even though in some cases also positive influence is showed, as well as home environment.
Limitations
Different limitations can be found in the present study
The symmetry of the funnel plots was examined to search for possible publication bias or even heterogeneity. Asymmetry was found for studies reporting ethnicity, SES and information source/advice (Table 3).
Table 3.
Analysis for funnel plot asymmetry of studies reporting the different variables, estimated by Egger's regression test.
| No. studies | coefficient | 90% CI | p-value | |
|---|---|---|---|---|
| Knowledge, beliefs, perceptions (right vs misleading) | 19 | −2.21 | −5.560 – 1.178 | 0.272 |
| Attitudes/behaviors (positive vs negative) | 18 | −0.83 | −3.508 – 1.843 | 0.595 |
| Ethnicity (different vs local) | 31 | 3.24 | 0.339 – 6.138 | 0.068 |
| Socio-economic status (high vs low) | 24 | 2.55 | 0.825 – 4.268 | 0.019 |
| Information source/advice (sufficient vs insufficient) | 11 | 6.64 | 2.140 – 11.137 | 0.024 |
The ethnicity and SES were also analyzed through a contour plot where the missing studies were in a bottom left and bottom right area of significance, so publication bias was unlikely to be the underlying cause of asymmetry; in the information source/advice contour plot, instead, missing studies were in the area of not significance, thus a publication bias may be hypothesized on missing studies (supplemental file S1). Since studies are missing on the actual parents' opinions on information source and advices about vaccinations and related diseases, this could be a factor to be considered in the strategies to plan to increase vaccine compliance. Immunization guidance for health professionals could focus more on improving parents' satisfaction with vaccination consultations, and fostering trusting relationships with parents in the context of immunization.4,52
This study suffers from a limitation due to the arbitrary classification of the analyzed factors.
The authors have decided to combine and analyze some variables that can be incorporated into 1 main class of determinants (e.g., the main “knowledge, beliefs and perceptions” class includes parents' responses on these 3 aspects), this leading to decrease the methodological rigour of the meta-analysis. Moreover, there is often confusion between terms such as attitudes, perceptions or beliefs, also due to the lack of a standard tool for assessment of immunization decision-making. Nevertheless, the authors were supported by the idea that for the development of effective health communication campaigns it is important to recognize underlying beliefs. Theoretical models use these classes of determinants54 that lead to change people's intentions and engage them in health behaviors.
A different coding of the variables underlying parental decision was also present in the analyzed studies, that may have led to under evaluate some less reported determinant, and then to an incomplete framework of the situation.
All this suggests the need of developing a standardized tool to better investigate the decision-making process across parents and other populations as well, and to compare studies at the international level.
A potential overestimation of the actual uptake could have occurred, since examined studies generally used subjective measures of vaccine uptake that cause recall bias,55 so that e.g. past attitudes/behaviors can be confused with the current ones. Objective data from primary care records are needed, to produce a more reliable measure of uptake.4 In our meta-analysis, data from official databases were reported only for what concerns demographics, and, as previously mentioned, no difference was noticed in the subgroup analysis with the questionnaires or interviews.
A possible limit of the present study could also be the different vaccine policy and strategy of the European countries, and the different vaccine introduction time within each country, all factors that could have influenced parents in their vaccination choices. Finally, data in this analysis were available only for some European countries (e.g., publications from the Eastern area were missing).
Conclusions and policy implications
Overall misleading knowledge, beliefs and perceptions on vaccines, general negative attitudes and behaviors toward vaccination, some demographic characteristics such as minor ethnicity, low socio-economic status (especially low income and education, high number of children and non-married status) are strong predictors of lower MMR vaccination uptake in European parents for their children. These findings could be used to suggest that policies aimed at increasing MMR vaccine uptake in Europe should be focused on providing better knowledge, creating correct beliefs and perceptions on vaccines, improving attitudes and behaviors in European parents. Thus, interventions should be focused on better communication strategies that could provide parents with clear messages specifically on vaccine efficacy, safety, bad side effects/consequences, health protection, necessity, and that could highlight the importance of the compliance with the second dose of the MMR vaccine. Moreover, communication strategies should be addressed mainly to people of ethnic minorities living in Southern Europe, and to low educated and deprived families, with higher number of children and non-married marital status. Health practitioners on their side could be adequately informed in order to better transfer knowledge to parents.
This paper could suggest carrying on similar studies in Eastern European countries, to obtain a complete framework of the European situation about the determinants of the decision of parents of vaccinating their children against MMR.
Material and methods
Systematic literature review
A systematic literature review (SLR) was carried out on the factors associated with MMR vaccine uptake by parents, considering key terms used in combination and referred to vaccine/immunization, uptake/coverage, determinant/factor, and measles, mumps and rubella, with medical Subject Headings (MeSH) and MeSH Major Topics included in the syntax. The online databases PubMed/MEDLINE, SCOPUS, EMBASE, ISI Web of Science were considered, as well as the gray literature and a manual search from the references of the articles retrieved.
Original articles published between 2000 and 2014 were retrieved, with restriction criteria applied to the European region and to the English language. Qualitative and quantitative studies describing the determinants underlying vaccination uptake in parents were included in the review. Studies were required to focus on routine childhood vaccinations against MMR. Information was collected from parents' answers both to questions specific on MMR vaccine and questions regarding all the vaccine schedule including the MMR vaccine.
The following exclusion criteria were initially applied: articles published in a language different from the English idiom, including non-European countries or rural areas only, reporting vaccination information on sick populations, very pre-term infants and migrants; as well as assessing only the impact or the coverage of vaccination, reporting uptake determinants not on parents (e.g., general practitioners, university students, workers, etc). Focus groups with less than 10 parents were arbitrarily excluded from the full text analysis, and other exclusion criteria were applied such as not reporting direct linking with uptake (e.g. linking with adverse publicity or with information-seeking), methodology studies or papers reporting no specific indications on MMR. Studies were then selected for the qualitative and quantitative analysis.
Variables extraction was conducted on the basis of previously identified potential classes of determinants, adapted from previous SLR.4,50 These classes included: knowledge, beliefs and perceptions both on vaccines and diseases (KBPvd); attitudes/behaviors; demographics, including ethnicity, mother's age, child' age, gender, geographic location; socio-economic status (SES), including education level, employment, house tenure, income, marital status, no. of children in the household; information source/advice; influence/trust of other people, institutions, media; practical reasons. The literature search and the systematic review were conducted by 2 independent investigators, that, in case of any incongruity, came up to an agreement after further discussion.
Meta-analysis
After selecting the articles reporting Odds Ratios (ORs) and 95% Confidence Intervals (CIs) as measures of association of the underlying determinants with the vaccine uptake, a meta-analysis was conducted on the extracted measures in order to assess the overall effect. The dependent variable was the “vaccine uptake” and the considered determinants were the independent variables. When the outcome variable of the examined study was the non-uptake, the inverse of the ORs were calculated and included in the analysis. Adjusted ORs were considered where available, with unadjusted ORs used if not reported, and the logarithms were used for the meta-analysis, with exponentiated effect sizes and confidence intervals displayed in the forest plots.
Pooled estimates were calculated using both fixed effects and DerSimonian and Laird 56 random effects models, weighting individual study results by the inverse of their variances. Forest plots were used to visually assess the pooled estimates and corresponding 95% CI across studies. A test of heterogeneity was performed using a chi-square test57 at significance level of p < 0.05 and reported with the I2 statistic, in which cut-offs of 25%, 50% and 75% indicated low, moderate and high heterogeneity, respectively.58
When the test showed significant heterogeneity, the sources of heterogeneity were explored through subgroup and sensitivity analyses. The following variables were considered for the subgroup analysis: questionnaires reporting on MMR vaccine alone MMR plus other vaccines included in the local schedule, MMR vaccine schedule adherence (all recommended doses, 1 dose, both), geographical location (Northern, Western, Southern Europe), children's age at the moment of the study (<5 y, >5 y, mixed age), data collection method (interview, questionnaire, official database), administration modality (interviewer-administered face-to-face, interviewer-administered telephone, self-administered postal, self-administered hand, records), administration setting (home, hospital/nursery/primary care trust, day-care centers/schools, other). When more than 1 modality was present, variables were dichotomized for the sake of analysis. Sensitivity analyses were conducted to examine the contribution of each individual study by evaluating the impact of the outlier studies, eliminating each study from the meta-analysis and comparing the point estimates including and excluding the study.
To assess the potential of publication bias, a graphical plot of estimates of the logarithm of the effect versus its standard error for each study was employed and the Egger test was performed.59,60 To overcome the limit of the Egger test due to the presence of small studies, evidence of asymmetry has been set on p < 0.1 and intercepts have been presented with 90% CI.60 In order to aid visual interpretation, contour lines were included corresponding to perceived milestones of statistical significance (P = 0.01, 0.05, 0.1, etc.).61,62 Results were also displayed in a Galbraith plot, where the standard normal deviate of intervention effect estimate is plotted against its precision.
The methodological quality of quantitative studies included in the meta-analysis was assessed using revised versions of previously validated checklists for quantitative cross-sectional and retrospective studies62 as recommended by the Cochrane Collaboration.63
All data were analyzed by using the statistical package of STATA/MP 12.1 (StataCorp LP, College Station, TX, USA), with the “metan” command used for meta-analysis “metafunnel,” “metabias” and “confunnel” for publication bias assessment.64
Abbreviations
- GP
general practitioners
- IW
interviewer-administered
- KBPvd
knowledge, beliefs and perceptions on vaccines and diseases
- MMR
Mumps, measles and rubella
- SA
self-administered
- SES
socio-economic status
Supplementary Material
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Authors' contributions
GT, CC, VM and MC designed the search strategy; GT searched for articles, extracted data, performed statistical analysis and prepared the first draft of the paper; GN and AC contributed in the statistical analysis and interpretation of results; FV double checked results and their interpretation. All authors contributed to subsequent drafts and agreed on the final paper. All members of ESCULAPIO agreed on the design of the study.
Funding
This work was carried on within the project ESCULAPIO (CUP B33G13001190001), funded by the Italian Centre for Disease Prevention and Control (CCM) of the Ministry of Health. The funding had no role in the manuscript preparation and submission.
References
- [1].Demicheli V, Rivetti A, Debalini MG, Di Pietrantonj C. Vaccines for measles, mumps and rubella in children. Evidence-Based Child Heal 2013; 8:2076-38; http://dx.doi.org/ 10.1002/ebch.1948 [DOI] [Google Scholar]
- [2].European Centre for Disease Prevention and Control Measles and rubella monitoring, July 2015 – Reporting on July 2014 – June 2015 surveillance data and epidemic intelligence data to the end of July 2015. Stockholm: ECDC; 2015. [Google Scholar]
- [3].Pearce A, Mindlin M, Cortina-Borja M, Bedford H. Characteristics of 5-year-olds who catch-up with MMR: findings from the UK Millennium Cohort Study. BMJ Open [Internet] 2013; 3:1-9. PMID:23864213; http://dx.doi.org/ 10.1136/bmjopen-2013-003152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, Vincent CA, Fraser G, Sevdalis N. Factors underlying parental decisions about combination childhood vaccinations including MMR: A systematic review. Vaccine 2010; 28:4235-48; PMID:20438879; http://dx.doi.org/ 10.1016/j.vaccine.2010.04.052 [DOI] [PubMed] [Google Scholar]
- [5].Nagaraj A. Does qualitative synthesis of anecdotal evidence with that from scientific research help in understanding public health issues: A review of low MMR uptake. Eur J Public Health 2006; 16:85-8; PMID:16446303; http://dx.doi.org/ 10.1093/eurpub/cki058 [DOI] [PubMed] [Google Scholar]
- [6].Lernout T, Theeten H, Hens N, Braeckman T, Roelants M, Hoppenbrouwers K, Van Damme P. Timeliness of infant vaccination and factors related with delay in Flanders, Belgium. Vaccine 2014; 32:284-9; PMID:24252698; http://dx.doi.org/ 10.1016/j.vaccine.2013.10.084 [DOI] [PubMed] [Google Scholar]
- [7].Robert E, Dramaix M, Swennen B. Vaccination Coverage for Infants: Cross-Sectional Studies in Two Regions of Belgium. Biomed Res Int 2014:107, Article ID 838907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Harmsen IA, Mollema L, Ruiter RA, Paulussen TG, De Melker HE, Kok G. Why parents refuse childhood vaccination: a qualitative study using online focus groups. BMC Public Health 2013;13:1183. DOI: 10.1186/1471-2458-13-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Pavlopoulou ID, Michail KA, Samoli E, Tsiftis G, Tsoumakas K. Immunization coverage and predictive factors for complete and age-appropriate vaccination among preschoolers in Athens, Greece: a cross- sectional study. BMC Public Health [Internet] 2013; 13:1 Available from: http://www.biomedcentral.com/1471-2458/13/908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Van Lier A, Van De Kassteele J, De Hoogh P, Drijfhout I, De Melker H. Vaccine uptake determinants in the Netherlands. Eur J Public Health 2014; 24:304-9; PMID:23531526; http://dx.doi.org/ 10.1093/eurpub/ckt042 [DOI] [PubMed] [Google Scholar]
- [11].Bouhamam N, Laporte R, Boutin A, Uters M, Bremond V, Noel G, Rodier P, Minodier P. N. Précarité, couverture sociale et couverture vaccinale : enquête chez les enfants consultant aux urgences pédiatriques. Arch Pediatr 2012;19: 242-7. PMID:22226013 [DOI] [PubMed] [Google Scholar]
- [12].Brown KF, Long SJ, Ramsay M, Hudson MJ, Green J, Vincent CA, Kroll JS, Fraser G, Sevdalis N. UK parents' decision-making about measles-mumps-rubella (MMR) vaccine 10 years after the MMR-autism controversy: A qualitative analysis. Vaccine 2012; 30:1855-64; PMID:22230590; http://dx.doi.org/ 10.1016/j.vaccine.2011.12.127 [DOI] [PubMed] [Google Scholar]
- [13].Kriwy P. Similarity of parents and physicians in the decision to vaccinate children against measles, mumps and rubella. Int J Public Health 2012; 57(2):333-40. [DOI] [PubMed] [Google Scholar]
- [14].Mollema L, Wijers N, Hahné SJ, van der Klis FR, Boshuizen HC, de Melker HE. Participation in and attitude towards the national immunization program in the Netherlands: data from population-based questionnaires. BMC Public Health 2012; 12:57; PMID:222643; http://dx.doi.org/ 10.1186/1471-2458-12-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Schönberger K, Ludwig MS, Wildner M, Kalies H. Timely MMR vaccination in infancy: Influence of attitudes and medical advice on the willingness to vaccinate. Klin Padiatr 2012; 224:437-42; PMID:22821294; http://dx.doi.org/ 10.1055/s-0032-1321731 [DOI] [PubMed] [Google Scholar]
- [16].Brown K, Fraser G, Ramsay M, Shanley R, Cowley N, van Wijgerden J, Toff P, Falconer M, Hudson M, Green J, et al.. Attitudinal and demographic predictors of measles-mumps-rubella vaccine (MMR) uptake during the UK catch-up campaign 2008–09: Cross-sectional survey. PLoS One 2011; 6:e19381; PMID:21602931; http://dx.doi.org/ 10.1371/journal.pone.0019381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Brown KF, Shanley R, Cowley NAL, van Wijgerden J, Toff P, Falconer M, Ramsay M, Hudson MJ, Green J, Vincent CA, et al.. Attitudinal and demographic predictors of measles, mumps and rubella (MMR) vaccine acceptance: Development and validation of an evidence-based measurement instrument. Vaccine 2011; 26:1700-9; PMID:21185850; http://dx.doi.org/ 10.1016/j.vaccine.2010.12.030 [DOI] [PubMed] [Google Scholar]
- [18].Coniglio MA, Platania M, Privitera D, Giammanco G, Pignato S. Parents' attitudes and behaviours towards recommended vaccinations in Sicily, Italy. BMC Public Health 2011; 11:305; PMID:21569424; http://dx.doi.org/ 10.1186/1471-2458-11-305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sakou I-I, Tsitsika AK, Papaevangelou V, Tzavela EC, Greydanus DE, Tsolia MN. Vaccination coverage among adolescents and risk factors associated with incomplete immunization. Eur J Pediatr 2011; 170:1419-26; PMID:21465121; http://dx.doi.org/ 10.1007/s00431-011-1456-z [DOI] [PubMed] [Google Scholar]
- [20].Babatsikou F, Vorou R, Vardaki Z, Galani S, Ktenas E, Koutis C. Childhood vaccination uptake and factors affecting this in athens, Greece. Heal Sci J 2010; 4(4):237-44. [Google Scholar]
- [21].Danis K, Georgakopoulou T, Stavrou T, Laggas D, Panagiotopoulos T. Predictors Of Childhood Vaccination Uptake: A Cross-sectional Study In Greece. Procedia in Vaccinology 2010; 2(1):84-9. [Google Scholar]
- [22].Gardner B, Davies A, McAteer J, Michie S. Beliefs underlying UK parents' views towards MMR promotion interventions: a qualitative study. Psychol Health Med 2010; 15:220-30; PMID:20391239; http://dx.doi.org/ 10.1080/13548501003623963 [DOI] [PubMed] [Google Scholar]
- [23].Jessop LJ, Murrin C, Lotya J, Clarke AT, O'Mahony D, Fallon UB, Johnson H, Bury G, Kelleher CC, Murphy AW. Socio-demographic 625 and health-related predictors of uptake of first MMR immunisation in the Lifeways Cohort Study. Vaccine 2010; 28(38):6338-43. [DOI] [PubMed] [Google Scholar]
- [24].Borras E, Domınguez A, Fuentes M, Batalla J, Cardenosa N, Plasencia A. Parental knowledge of paediatric vaccination. BMC Public Health 2009; 9:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Borràs E, Domínguez A, Oviedo M, Batalla J, Salleras L. The influence of public or private paediatric health care on vaccination coverages in children in Catalonia (Spain). Eur J Public Health 2009; [DOI] [PubMed] [Google Scholar]
- [26].Reading R. The Millennium Cohort Study Child Health Group Factors associated with uptake of measles, mumps, and rubella vaccine (MMR) and use of single antigen vaccines in a contemporary UK cohort: prospective cohort study. Child Care Health Dev 2008; 34(4):545-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Theeten H, Vandermeulen C, Roelants M, Hoppenbrouwers K, Depoorter AM, Van Damme P. Coverage of recommended vaccines in children at 7–8 years of age in Flanders, Belgium. Acta Paediatr Int J Paediatr 2009; 98:1307-12 PMID:19432835; http://dx.doi.org/ 10.1111/j.1651-2227.2009.01331.x [DOI] [PubMed] [Google Scholar]
- [28].Vandermeulen C, Roelants M, Theeten H, Van Damme P, Hoppenbrouwers K. Vaccination coverage and sociodemographic determinants of measles-mumps-rubella vaccination in three different age groups. Eur J Pediatr 2008; 167:1161-8; PMID:18204860; http://dx.doi.org/ 10.1007/s00431-007-0652-3 [DOI] [PubMed] [Google Scholar]
- [29].Mixer RE, Jamrozik K, Newsom D. Ethnicity as a correlate of the uptake of the first dose of mumps, measles and rubella vaccine. J Epidemiol Community Health 2007; 61:797-801; PMID:17699534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Smith A, Yarwood J, Salisbury DM. Tracking mothers' attitudes to MMR immunisation 1996–2006. Vaccine 2007; 25:3996-4002; PMID:17395344 [DOI] [PubMed] [Google Scholar]
- [31].Theeten H, Hens N, Vandermeulen C, Depoorter AM, Roelants M, Aerts M, Hoppenbrouwers K, Van Damme P. Infant vaccination coverage in 2005 and predictive factors for complete or valid vaccination in Flanders, Belgium: an EPI-survey. Vaccine 2007; 25:4940-8; PMID:17524528 [DOI] [PubMed] [Google Scholar]
- [32].Casiday R, Cresswell T, Wilson D, Panter-Brick C. A survey of UK parental attitudes to the MMR vaccine and trust in medical authority. Vaccine 2006; 24:177-84; PMID:16157422 [DOI] [PubMed] [Google Scholar]
- [33].Cassell JA, Leach M, Poltorak MS, Mercer CH, Iversen A, Fairhead JR. Is the cultural context of MMR rejection a key to an effective public health discourse? Public Health 2006; 220:783-94; PMID:16828492 [DOI] [PubMed] [Google Scholar]
- [34].Paulussen TGW, Hoekstra F, Lanting CI, Buijs GB, Hirasing RA. Determinants of Dutch parents' decisions to vaccinate their child. Vaccine 2006; 24:644-51; PMID:16157423 [DOI] [PubMed] [Google Scholar]
- [35].Wright JA, Polack C. Understanding variation in measles-mumps-rubella immunization coverage - A population-based study. Eur J Public Health 2006; 16:137-42; PMID:16207728 [DOI] [PubMed] [Google Scholar]
- [36].Dannetun E, Tegnell A, Hermansson G, Giesecke J. Parents' reported reasons for avoiding MMR vaccination. A telephone survey. Scand J Prim Health Care 2005; 23:149-53; PMID:16162466 [DOI] [PubMed] [Google Scholar]
- [37].Gellatly J, McVittie C, Tiliopoulos N. Predicting parents' decisions on MMR immunisation: A mixed method investigation. Fam Pract 2005; 22:658-62; PMID:16024553 [DOI] [PubMed] [Google Scholar]
- [38].Hak E, Schönbeck Y, De Melker H, Van Essen GA, Sanders EAM.. Negative attitude of highly educated parents and health care workers towards future vaccinations in the Dutch childhood vaccination program. Vaccine 2005; 23:3103-7; PMID:15837208 [DOI] [PubMed] [Google Scholar]
- [39].Alfredsson R, Svensson E, Trollfors B, Borres MP. Why do parents hesitate to vaccinate their children against measles, mumps and rubella? Acta Paediatr 2004; 93:1232-7; PMID:15384890 [PubMed] [Google Scholar]
- [40].Flynn M, Ogden J. Predicting uptake of MMR vaccination: A prospective questionnaire study. Br J Gen Pract 2004; 54:526-30; PMID:15239915 [PMC free article] [PubMed] [Google Scholar]
- [41].McMurray R, Cheater FM, Weighall A, Nelson C, Schweiger M, Mukherjee S. Managing controversy through consultation: A qualitative study of communication and trust around MMR vaccination decisions. Br J Gen Pract 2004; 54:520-5; PMID:15239914 [PMC free article] [PubMed] [Google Scholar]
- [42].Petrovic M, Roberts RJ, Ramsay M, Charlett A. Parents' attitude towards the second dose of measles, mumps and rubella vaccine: a case-control study. Commun Dis Public Health 2003; 6:325-9; PMID:15067860 [PubMed] [Google Scholar]
- [43].Smailbegovic MS, Laing GJ, Bedford H. Why do parents decide against immunization? The effect of health beliefs and health professionals. Child Care Health Dev 2003; 29:303-11; PMID:12823336 [DOI] [PubMed] [Google Scholar]
- [44].Navarro Alonso JA, Bernal González PJ, Niguez Carbonell JC. Analysis of factors influencing vaccine uptake: perspective from Spain. Vaccine 2001; 20:S13-5; PMID:11587802 [DOI] [PubMed] [Google Scholar]
- [45].Ramsay ME, Yarwood J, Lewis D, Campbell H, White JM. Parental confidence in measles, mumps and rubella vaccine: Evidence from vaccine coverage and attitudinal surveys. Br J Gen Pract 2002; 52:912-6; PMID:12434960 [PMC free article] [PubMed] [Google Scholar]
- [46].Evans M, Stoddart H, Condon L, Freeman E, Grizzell M, Mullen R. Parents' perspectives on the MMR immunisation: A focus group study. Br J Gen Pract 2001; 51:904-10; PMID:1176120 [PMC free article] [PubMed] [Google Scholar]
- [47].Swennen B, Van Damme P, Vellinga A, Coppieters Y, Depoorter AM. Analysis of factors influencing vaccine uptake: perspectives from Belgium. Vaccine 2001; 20(Suppl 1):S5-7; discussion S1; PMID:11587800; http://dx.doi.org/ 10.1016/S0264-410X(01)00307-3 [DOI] [PubMed] [Google Scholar]
- [48].Impicciatore P, Bosetti C, Schiavio S, Pandolfini C, Bonati M. Mothers as active partners in the prevention of childhood diseases: maternal factors related to immunization status of preschool children in Italy. Prev Med (Baltim) 2000; 31:49-55; PMID:10896843 [DOI] [PubMed] [Google Scholar]
- [49].Pareek M, Pattison HM. The two-dose measles, mumps, and rubella (MMR) immunisation schedule: Factors affecting maternal intention to vaccinate. Br J Gen Pract 2000; 50:969-71; PMID:11224968 [PMC free article] [PubMed] [Google Scholar]
- [50].Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: A critical review. Soc. Sci. Med. 2014; 112:1-11; PMID:24788111 [DOI] [PubMed] [Google Scholar]
- [51].Taylor LE, Swerdfeger AL, Eslick GD. Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine 2014; 32:3623-9; PMID:24814559; http://dx.doi.org/ 10.1016/j.vaccine.2014.04.085 [DOI] [PubMed] [Google Scholar]
- [52].Ganczak M, Dmytrzyk-Daniłów G, Karakiewicz B, Korzeń M, Szych Z. Determinants influencing self-paid vaccination coverage, in 0–5 years old Polish children. Vaccine 2013; 31:5687-92; PMID:24120549; http://dx.doi.org/ 10.1016/j.vaccine.2013.09.056 [DOI] [PubMed] [Google Scholar]
- [53].UNICEF/WHO. Immunization summary: a statistical reference containing data through 2010. (2012 ed.). The United Nations Children's Fund (UNICEF), January 2012. [Google Scholar]
- [54].Fishbein M, Yzer M. Using Theory to Design Effective Health Behavior Interventions. Commun Theory [Internet] 2003; :164-83. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=9674241352091541817\nfile:///Users/cameronnorman/Library/Application Support/Papers2/Articles/2003/Fishbein/2003 Fishbein.pdf\npapers2://publication/uuid/0630; http://dx.doi.org/ 10.1111/j.1468-2885.2003.tb00287.x [DOI] [Google Scholar]
- [55].Suarez L, Simpson DM, Smith DR. Errors and correlates in parental recall of child immunizations: effects on vaccination coverage estimates. Pediatrics 1997; 99:E3; PMID:9113960; http://dx.doi.org/ 10.1542/peds.99.5.e3 [DOI] [PubMed] [Google Scholar]
- [56].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177-88; PMID:3802833; http://dx.doi.org/ 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- [57].Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res 1993; 2:121-45; PMID:8261254; http://dx.doi.org/ 10.1177/096228029300200202 [DOI] [PubMed] [Google Scholar]
- [58].Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ Br Med J 2003; 327:557-60; PMID:1295812; http://dx.doi.org/ 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Sterne JAC, Egger M. Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. J Clin Epidemiol 2001; 54:1046-55; PMID:11576817; http://dx.doi.org/ 10.1016/S0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- [60].Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629-34; PMID:9310563; http://dx.doi.org/ 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 2008; 61:991-6; PMID:18538991; http://dx.doi.org/ 10.1016/j.jclinepi.2007.11.010 [DOI] [PubMed] [Google Scholar]
- [62].Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. 2012. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- [63].Reeves C B, Deeks J J, Higgins P.,T. J, Wells A G. Cochrane Handbook: Special Topics: Ch 13: Including non-randomized studies [Internet]. In: Higgins P.,T. J, Green S, editors. Cochrane Handbook for: Systematic Reviews of Interventions. Wiley-Blackwell; 2011. page 389-432. Available from: J:/WMCSU/WORK PROGRAMME/PROJECTS TRAINING/2_EXTERNAL EDUCATION & TRAINING/COURSES - Planned Training/UoB_EVIDENCE REVIEW Training/COURSES RUN. [Google Scholar]
- [64].Palmer TM, Sterne JAC, editors. Meta-Analysis in Stata: An Updated Collection from the Stata Journal. 2nd ed. Stata Press; 2015, 534 p. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.