Abstract
Background
Heart failure (HF) is the leading cause for hospital readmission. Hospice care may help palliate HF symptoms but its association with 30-day all-cause readmission remains unknown.
Methods and Results
Of the 8032 Medicare beneficiaries hospitalized for HF in 106 Alabama hospitals (1998–2001), 182 (2%) received discharge hospice referrals. Of the 7850 patients not receiving hospice referrals, 1608 (20%) died within 6 months post-discharge (the hospice-eligible group). Propensity scores for hospice referral were estimated for each of the 1790 (182+1608) patients and were used to match 179 hospice-referral patients with 179 hospice-eligible patients who were balanced on 28 baseline characteristics (mean age, 79 years, 58% women, 18% African American). Overall, 22% (1742/8032) died in 6 months, of whom 8% (134/1742) received hospice referrals. Among the 358 matched patients, 30-day all-cause readmission occurred in 5% and 41% of hospice-referral and hospice-eligible patients, respectively (hazard ratio {HR} associated with hospice referral, 0.12; 95% confidence interval {CI}, 0.06–0.24). HRs (95% CIs) for 30-day all-cause readmission associated with hospice referral among the 126 patients who died and 232 patients who survived 30-day post-discharge were 0.03 (0.04–0.21) and 0.17 (0.08–0.36), respectively. Although 30-day mortality was higher in the hospice referral group (43% vs. 27%), it was similar at 90 days (64% vs. 67% among hospice-eligible patients).
Conclusions
A discharge hospice referral was associated with lower 30-day all-cause readmission among hospitalized HF patients. However, most HF patients who died within 6 months of hospital discharge did not receive a discharge hospice referral.
Keywords: Medicare beneficiaries, heart failure, discharge hospice referral, 30-day all-cause readmission
Heart failure (HF) is the leading cause for hospital readmissions in the United States. About one in four Medicare beneficiaries hospitalized for acute decompensated HF are readmitted within 30 days of hospital discharge.1 Hospital readmission accounts for over $17 billion annually of Medicare spending and readmission reduction is a major focus of the Affordable Care Act.1, 2 Under the law, hospitals with above-average readmission rates are subject to financial penalties and it has been projected that over the next 10 years U.S. hospitals may collectively lose over $7 billion in Medicare payments. Under pressure to reduce readmission rates many hospitals are adopting unproven transition of care strategies.3 There has also been increased interest in better understanding the effects of evidence-based HF therapy on 30-day all-cause readmission in patients with HF. We have demonstrated that digoxin may reduce the risk of 30-day all-cause hospital readmission in patients with HF and reduced ejection fraction (EF) without any adverse effect on mortality, but not in HF with preserved EF.4-6 We also observed similar beneficial association with angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, but not with beta-blockers and spironolactone.7-9 Thus, there is a need to identify high quality, HF-specific and evidence-based non-pharmacological strategies to reduce 30-day all-cause readmission in patients with HF.
Dyspnea is one of the cardinal symptoms of HF regardless of reduced or preserved EF.10 Worsening HF symptoms, such as dyspnea are often responsible for hospital admissions. Hospice and palliative care approaches to HF management including expert symptom control may be expected to improve HF symptoms and reduce hospitalization. However, the impact of discharge hospice referral on hospital readmissions in patients with HF remains unclear.11 In the current study, we examined the association of discharge hospice referral with 30-day all-cause readmission in Medicare beneficiaries hospitalized for decompensated HF.
Methods
Data Sources and Study Population
The Alabama Heart Failure Project is a registry of hospitalized HF patients based on a quality improvement project, the details of which have been presented elsewhere.12 Briefly, extensive data on baseline characteristics, past medical history, admission and discharge medications, in-hospital events, hospital care characteristics and laboratory values were collected on 8555 Medicare beneficiaries discharged from 106 Alabama hospitals with a principal discharge diagnosis of HF between July 1, 1998 and October 31, 2001.12 Medical records of patients with HF were identified using ICD-9 codes and were centrally abstracted and data were later linked to Medicare outcomes data.12 Of the 8555 Medicare beneficiaries with HF, 8049 were discharged alive. The Alabama Heart Failure Project data were approved for secondary analyses by the Institutional Review Board of the University of Alabama at Birmingham.
Exposure Variables
Extensive data on discharge disposition were collected by chart abstraction that included discharge referral for hospice care. Of the 8049 patients discharged alive, data on discharge hospice referral was available for 8032 patients, of which 182 (2%) were referred for hospice care and were included in the hospice-referral group (Figure 1). To assemble a cohort of hospice-eligible patients, we identified patients who died within 6 months post-discharge but did not receive discharge hospice referrals. Medicare hospice eligibility requires certification that a patient has a life expectancy of 6 months or less if the terminal illness runs its normal course. Of the 7850 patients who did not receive a discharge hospice referral, 1608 patients died within 6 months of hospital discharge and were considered to be hospice-eligible (Figure 1).
Figure 1.
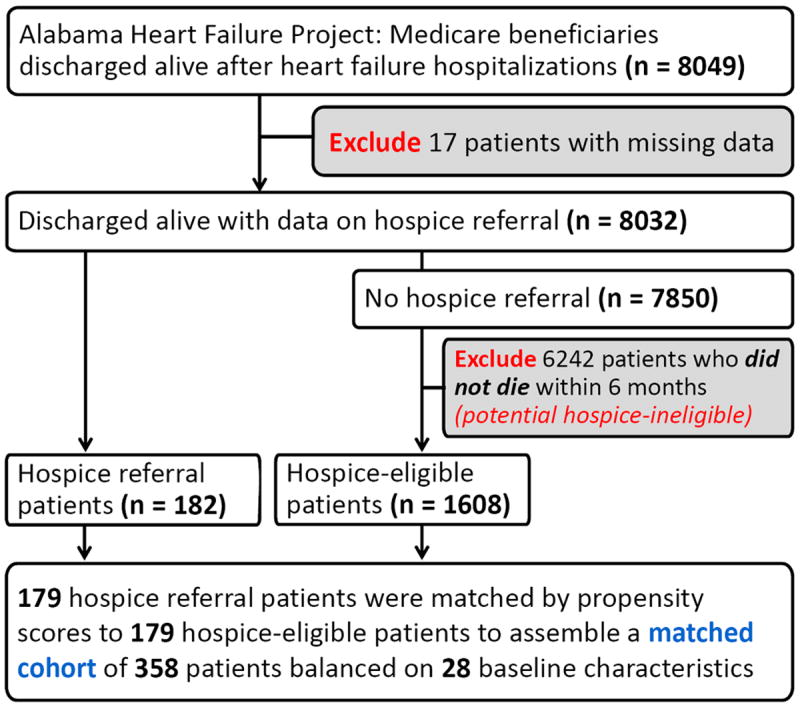
Flow chart displaying assembly of matched inception cohort of hospice-referral and hospice-eligible patients
Outcomes Data
The primary outcome of our study was all-cause readmission within 30 days of hospital discharge. Secondary outcomes included all-cause readmission within 3 and 6 months of hospital discharge, HF readmission, all-cause mortality and the composite end-point of all-cause mortality or all-cause readmission at 1, 3 and 6 months after hospital discharge. All outcomes data were obtained from Center for Medicare Services (CMS) Medicare utilization files, CMS Denominator files, CMS Medicare Provider Analysis and Review (Med PAR) files.12
Assembly of a Propensity-Matched Balanced Cohort
To reduce bias due to imbalances in baseline characteristics between hospice-referral and hospice-eligible patients, we used propensity scores to assemble a matched balanced cohort.13, 14 We used a non-parsimonious multivariable logistic regression model using 28 key baseline characteristics (Table 1) to estimate propensity scores or predicted probability for hospice referral for each of the 1790 patients.15-19 We then used a greedy matching protocol to match patients based on their propensity scores, thus assembling a cohort of 179 pairs of hospice-referral and hospice-eligible patients (Table 1 and Figure 2).
Table 1.
Baseline patient characteristics of older heart failure patients by hospice referral, before and after propensity score matching
| n (%) or mean (±SD) | Before propensity score matching (N=1790) | After propensity score matching (N=358) | ||||
|---|---|---|---|---|---|---|
| Hospice referral | Hospice referral | |||||
| No (n=1608) | Yes (n=182) | P value | No (n=179) | Yes (n=179) | P value | |
| Age (years) | 78 (±10) | 79 (±11) | 0.172 | 80 (±9) | 79 (±11) | 0.690 |
| Female | 866 (54) | 104 (57) | 0.399 | 105 (59) | 102 (57) | 0.828 |
| African American | 333 (21) | 33 (18) | 0.414 | 32 (17) | 33 (18) | 0.894 |
| Admission from nursing home | 227 (14) | 25 (14) | 0.889 | 27 (15) | 25 (14) | 0.880 |
| Left ventricular ejection fraction <45% | 636 (40) | 81 (45) | 0.196 | 78 (44) | 79 (44) | 1.000 |
| Past medical history | ||||||
| Prior heart failure | 1295 (81) | 156 (86) | 0.091 | 147 (82) | 153 (86) | 0.480 |
| Hypertension | 1041 (65) | 105 (58) | 0.060 | 105 (59) | 103 (58) | 0.914 |
| Coronary artery disease | 941 (59) | 118 (65) | 0.100 | 112 (63) | 115 (64) | 0.820 |
| Diabetes mellitus | 672 (42) | 83 (46) | 0.323 | 73 (41) | 80 (45) | 0.515 |
| Stroke | 404 (25) | 56 (31) | 0.099 | 59 (33) | 54 (30) | 0.630 |
| Chronic obstructive pulmonary disease | 625 (39) | 66 (36) | 0.494 | 62 (35) | 66 (37) | 0.752 |
| Dementia | 241 (15) | 33 (18) | 0.264 | 39 (22) | 33 (18) | 0.504 |
| Cancer | 70 (4) | 8 (4) | 0.979 | 12 (7) | 8 (5) | 0.503 |
| Atrial fibrillation | 500 (31) | 46 (25) | 0.106 | 43 (24) | 46 (26) | 0.810 |
| Clinical and laboratory findings | ||||||
| Pulse (beats per minute) | 89.6 (±22) | 90.5 (±23) | 0.637 | 88 (±22) | 90 (±23) | 0.370 |
| Systolic blood pressure (mmHg) | 139 (±31) | 136 (±30) | 0.211 | 134 (±30) | 136 (±30) | 0.629 |
| Pulmonary edema by chest x-ray | 1163 (72) | 145 (80) | 0.034 | 139 (78) | 142 (79) | 0.801 |
| Serum creatinine (mEq/L) | 1.81 (±1.33) | 1.83 (±1.10) | 0.834 | 1.80 (±1.21) | 1.83 (±1.11) | 0.802 |
| In hospital events | ||||||
| Pneumonia | 564 (35) | 67 (37) | 0.642 | 64 (36) | 67 (37) | 0.838 |
| Acute myocardial infarction | 74 (5) | 8 (4) | 0.900 | 12 (7) | 8 (5) | 0.503 |
| Pressure ulcer | 250 (16) | 58 (32) | <0.001 | 58 (32) | 55 (31) | 0.761 |
| Hospital and care characteristics | ||||||
| Rural hospital | 537 (33) | 45 (25) | 0.018 | 49 (27) | 45 (25) | 0.689 |
| Cardiology care | 767 (48) | 102 (56) | 0.033 | 104 (58) | 99 (55) | 0.675 |
| Intensive care | 84 (5) | 13 (7) | 0.278 | 14 (8) | 13 (7) | 1.000 |
| Discharge medications | ||||||
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers | 784 (49) | 77 (42) | 0.099 | 83 (46) | 77 (43) | 0.590 |
| Beta blockers | 294 (18) | 33 (18) | 0.960 | 37 (21) | 33 (18) | 0.683 |
| Loop diuretics | 1284 (80) | 140 (77) | 0.353 | 140 (78) | 138 (77) | 0.901 |
| Digoxin | 736 (46) | 89 (49) | 0.422 | 92 (51) | 88 (49) | 0.744 |
Figure 2.
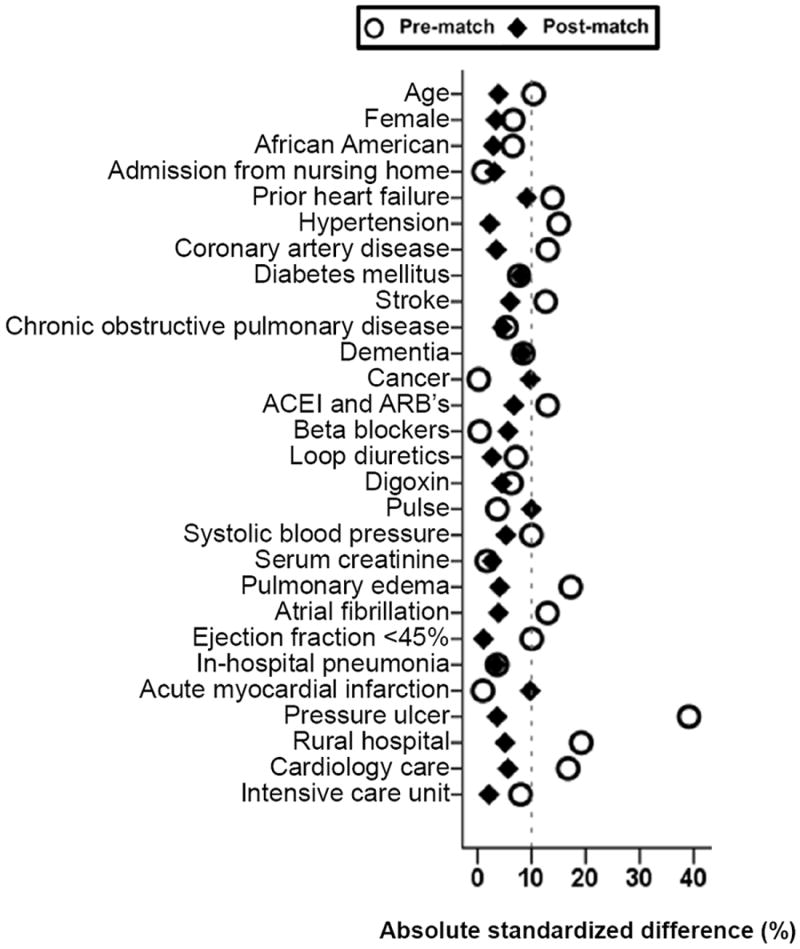
Love plot displaying absolute standardized differences comparing 28 baseline characteristics between hospice-referral and hospice-eligible heart failure patients, before and after propensity score matching. ACEI (angiotensin converting enzyme inhibitors); ARB (angiotensin receptor blockers)
Statistical Analyses
Between-group differences in baseline characteristics were compared using Pearson’s chi-square and Wilcoxon rank sum-test for pre-match, and McNemar test and paired sample t-test for post-match, as appropriate. Kaplan-Meier plots were used to compare adjusted primary outcome of 30-day all-cause readmission rates between propensity-matched hospice-referral and hospice-eligible patients. Bivariate Cox regression models were used to examine the association of hospice referral with the primary and other secondary outcomes among matched patients. A formal sensitivity analyses was conducted to quantify the degree of a hidden bias that would be required to explain away a significant primary association among matched patients.20 To examine if the association between hospice referral and 30-day all-cause readmission was influenced by a difference in 30-day mortality between the hospice referral and hospice-eligible groups, we separately examined that association among matched patients who died vs. survived during the 30-day post-discharge period.
To examine if the primary outcome was affected by 6-month mortality, we examined the primary outcome among a subset of hospice-referral patients who died 6-month post-discharge vs. hospice-eligible patients, who by study design, died during 6-month post-discharge. To examine the heterogeneity of association, we examined the association of hospice referral with 6-month all-cause readmission in several clinically important subgroups of matched patients. Finally, to complement the associations observed in the matched cohort (n=358), we repeated our analyses in the pre-match cohort (N=1790) using two traditional multivariable-adjusted Cox regression models: first, adjusting for the 28 variables used to calculate propensity scores as described above, and then, adjusting for the propensity score variable alone as a composite variable representing the 28 variables. All statistical analyses were two-tailed and p values <0.05 were considered significant. All data analyses were performed using SPSS-21 for Windows (SPSS, Incl., 2012, Chicago, IL).
Results
Baseline Characteristics
Patients (n=358) had a mean age of 79 years, 58% were female, and 18% were African American. Although pre-match baseline characteristics of HF patients receiving hospice referral and hospice-eligible HF patients not receiving hospice referral were generally similar, those in the hospice-referral group were likely to be sicker with higher prevalence of admission pulmonary edema and in-hospital pressure ulcer (Table 1 and Figure 2). Post-match absolute standardized differences for all 28 baseline characteristics were <10% suggesting that the balance achieved was substantial and any residual bias would be inconsequential (Figure 2).
Hospice Referral and 30-Day Post-Discharge Outcomes
Among the 8032 pre-match patients with data on hospice referral who were discharged alive, 21% (n=1685) were readmitted due to all causes within 30 days of hospital discharge. Among the 358 matched patients, 23% (n=82) had 30-day all-cause readmissions, which occurred in 5% (9/179) and 41% (73/179) of hospice-referral and hospice-eligible patients, respectively (hazard ratio {HR} associated with hospice referral, 0.12; 95% confidence interval {CI}, 0.06–0.24; Table 2 and Figure 3). There were a total of 58 matched pairs with clear outcomes – for 56 of these pairs, hospice-referral patients were readmitted later than hospice-eligible patients. In the absence of a hidden bias, a sign-score test for matched data with censoring provides strong evidence (p <0.0001) that hospice-eligible patients had more readmissions than hospice-referral patients. Among the 310 matched hospice-referral patients who died during the 6 months of follow-up, 30-day all-cause readmissions occurred in 4% (vs. 41% of the hospice-eligible patients; HR associated with hospice referral, 0.10; 95% CI, 0.04–0.25). Multivariable-adjusted and propensity score-adjusted HRs (95% CIs) for 30-day all-cause readmission among the 1790 pre-match patients were 0.13 (0.07–0.26) and 0.13 (0.07–0.26), respectively. Hospice referral was also associated with lower 30-day HF readmission (Table 2).
Table 2.
Association of hospice referral with post-discharge outcomes among propensity-score matched Medicare beneficiaries hospitalized for heart failure
| % (total events) | Hazard ratio* (95% confidence interval); p-value | ||
|---|---|---|---|
| Hospice referral | |||
| No (n=179) | Yes (n=179) | ||
| 30-day post-discharge | |||
| All-cause readmission | 41% (73) | 5% (9) | 0.12 (0.06–0.24); p<0.001 |
| Heart failure readmission | 17% (31) | 2% (4) | 0.14 (0.05–0.40); p<0.001 |
| All-cause mortality | 27% (49) | 43% (77) | 1.86 (1.30–2.67); p=0.001 |
| All-cause mortality or all-cause readmission | 55% (99) | 48% (85) | 0.83 (0.62–1.11); p=0.207 |
| 90-day post-discharge | |||
| All-cause readmission | 59% (105) | 13% (23) | 0.18 (0.12–0.29); p<0.001 |
| Heart failure readmission | 24% (42) | 6% (10) | 0.25 (0.13–0.51); p<0.001 |
| All-cause mortality | 67% (120) | 64% (114) | 1.14 (0.88–1.47); p=0.334 |
| All-cause mortality or all-cause readmission | 88% (158) | 72% (129) | 0.69 (0.55–0.88); p=0.002 |
| 6-month post-discharge | |||
| All-cause readmission | 64% (115) | 18% (32) | 0.18 (0.12–0.28); p<0.001 |
| Heart failure readmission | 27% (49) | 8% (15) | 0.26 (0.15–0.48); p<0.001 |
| All-cause mortality | 100% (179) | 73% (131) | 0.68 (0.54–0.86); p=0.001 |
| All-cause mortality or all-cause readmission | 100% (179) | 82% (147) | 0.59 (0.47–0.74); p<0.001 |
Hazard ratios comparing patients receiving hospice referral vs. hospice-eligible patients not receiving hospice referral
Figure 3.
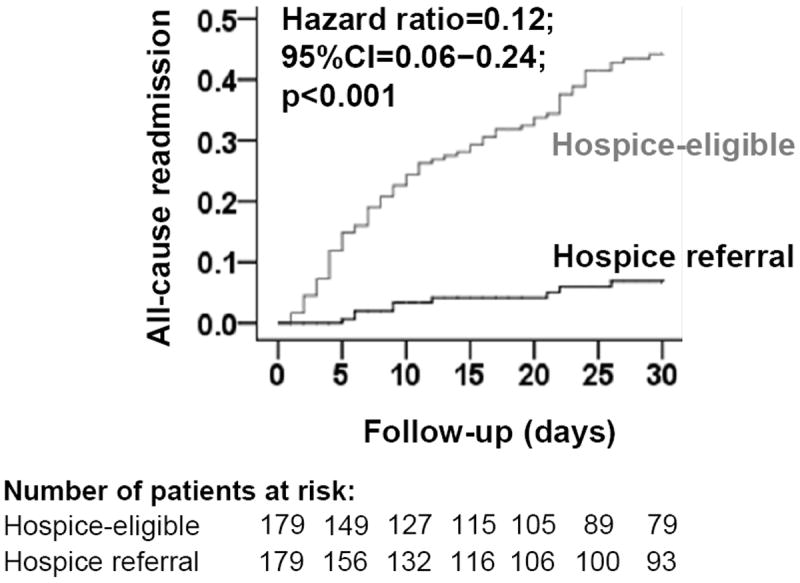
Kaplan Meier plot for 30-day all-cause readmission among propensity-matched hospice-referral and hospice-eligible heart failure patients. (CI=Confidence Interval)
Overall, 126 (35%) matched patients died during the first 30 days post-discharge, which was higher in the hospice-referral group (43% vs. 27% in the hospice-eligible group; HR, 1.86; 95% CI, 1.30–2.67; Table 2). As a result, hospice referral had no significant association with the composite end points of 30-day all-cause readmission or all-cause mortality (HR, 0.83; 95% CI, 0.62–1.11; Table 2). However, among the 232 matched patients who were alive during the first 30 days, 30-day all-cause readmission occurred in 8% and 39% of hospice-referral and hospice-eligible patients, respectively (HR, 0.17; 95% CI 0.08–0.36). Among the 126 matched patients who died during the first 30 days, 30-day all-cause readmission occurred in 1% and 47% of hospice-referral and hospice-eligible patients, respectively (HR, 0.03; 95% CI 0.04–0.21).
Hospice Referral and 3- and 6-Month Post-Discharge Outcomes
Among the 358 matched patients, 3-month all-cause readmission occurred in 13% and 59% of patients in the hospice-referral and hospice-eligible groups, respectively (HR, 0.18; 95% CI, 0.12–0.29; Table 2). Hospice referral was associated with lower 3-month HF readmission but had no association with 3-month all-cause mortality (Table 2). Among the 124 matched patients who survived the first 3 months after hospital discharge, 3-month all-cause readmission occurred in 23% and 64% of hospice-referral and hospice-eligible patients, respectively (HR 0.24; 95% CI 0.13–0.43). Among the 234 matched patients who died during the first 3 months after hospital discharge, 3-month all-cause readmission occurred in 7% and 56% of hospice-referral and hospice-eligible patients, respectively (HR 0.15; 95% CI 0.07–0.31).
Among the 358 matched patients, 6-month all-cause readmission occurred in 18% and 64% of hospice-referral and hospice-eligible patients, respectively (HR, 0.18; 95% CI, 0.12–0.28; Table 2). This association between hospice referral and 6-month all-cause readmission was homogenous across various clinically relevant subgroups of patients (Figure 4). As expected, 6-month all-cause mortality was 100% among hospice-eligible patients, but was 73% among hospice-referral patients.
Figure 4.
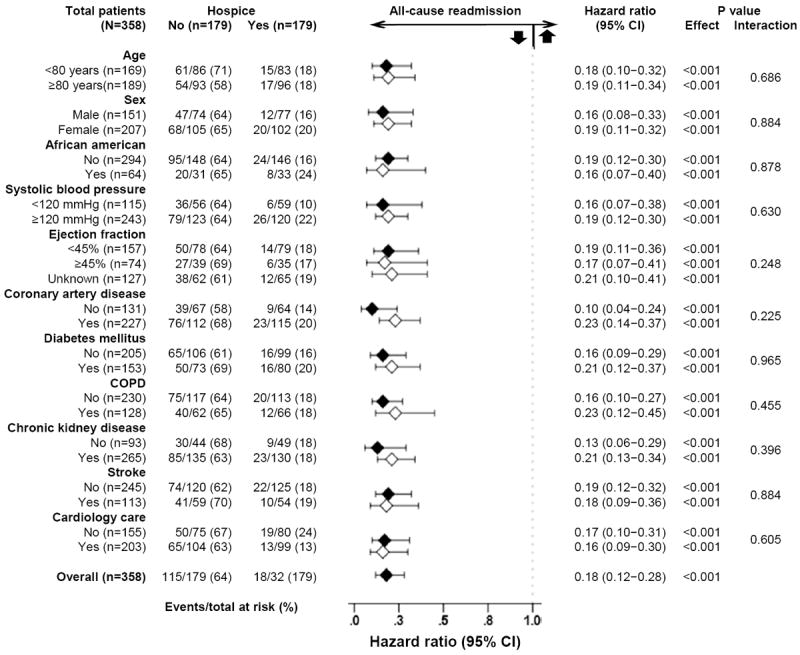
Hazard ratio and 95% confidence interval (CI) for 6-month all-cause readmission among subgroups of propensity matched hospice-referral and hospice-eligible heart failure patients. COPD (chronic obstructive pulmonary disease)
Discussion
Findings from the current study demonstrate that among Medicare beneficiaries discharged alive after hospitalization due to acute decompensated HF, when compared to a propensity-score matched group of hospice-eligible patients who died within six months of hospital discharge, the receipt of a discharge hospice referral was associated with a significantly lower 30-day all-cause hospital readmissions. Further, this beneficial association of hospice referral with readmission was observed throughout the entire six months post-discharge period and was unaffected by all-cause mortality. To the best of our knowledge, this is the first study to report a robust independent association of discharge hospice referral and lower 30-day hospital readmission in Medicare beneficiaries with HF regardless of EF.
There are several potential explanations for the lower readmission rates among patients in the hospice referral group in our study. HF is typically characterized by periods of stability, interrupted by episodes of acute exacerbation, and variable functional ability. However, with disease progression, the mode of death in HF changes from predominantly sudden death to predominantly pump failure death, which is often accompanied by worsening symptoms.21, 22 Yet, clinicians often are unable to predict outcomes in patients with HF, even toward the end of life.23, 24 HF patients and their families generally have minimal prognostic awareness due to lack of knowledge about the disease trajectory. However, enrollment into hospice involves explicit discussion of prognosis, coordination of care and difficult decision making, all of which may enhance their understanding and awareness of the limited prognosis and influence a shift in goals of care towards a less aggressive comfort care at home. However, worsening dyspnea, which is experienced by most HF patients toward the end of life, may still prompt some patients and families to seek care outside home.24 The substantially lower readmission rate in the hospice-referral group in our study suggests that the palliative care approach used by hospice teams may have been effective in alleviating HF symptoms, thus obviating needs for readmission. Hospice care also aims to address pain, anxiety and depression, all common in end stage HF.24, 25 Hospice patients are required to enter into a contractual agreement with hospice providers forgoing regular Medicare-covered benefits related to the treatment of the terminal illness and related conditions, which may cause some patients and families to avoid hospitalization.
Another potential explanation for the very low 30-day readmission rates is the very short survival after hospital discharge which may be a marker of late referral to hospice. Although all hospice patients were referred at the time of hospital discharge, some may have been very near death. National estimates suggest that hospice median length of stay is only 19 days overall and 17 days for HF patients, and that 35% of patients die or are discharged within 7 days of hospice admission.26, 27 However, the higher 30-day mortality in the hospice group is unlikely to fully explain the lower 30-day readmission rates as hospice care was also associated with lower readmission among those who were alive during the first 30 days post-discharge. Compared with hospice patients with cancer and HF, those with dementia are known to have longer hospice length of stay and fewer resource utilization, which may in turn result in lower hospitalizations.27 It is also possible that some HF patients were referred to hospice for non-HF related diagnoses such as advanced dementia. Although we did not have data on specific hospice-defining diagnosis, the impact of dementia-related differences in resource utilization maybe relatively low as there was no significant between-group difference in the baseline prevalence of dementia.
Over 40% of all patients in the hospice referral group (vs. <30% of non-hospice patients) in our study died during the first 30 days post-discharge. It is possible that hospice patients were sicker and prognostically different from the matched controls, at least during the first month post-discharge. It is also possible that treatment of these sicker patients may have contributed to this higher early mortality. While we had no data on the prevalence of opioid use post-discharge, it is possible that some of the hospice patients received opioids which are known to alleviate dyspnea, pain and anxiety in end-stage HF patients.28-30 Additionally, opioids use has been shown to be associated with higher mortality.31, 32 Thus, opioid use may in part explain the higher early mortality in the hospice-referral group, although selection bias cannot be ruled out. Intravenous inotropes, also recommended for short-term symptom management in end-stage HF, are also known to increase mortality.33, 34 The 25% of the hospice-referral patients who were alive at 6-month may be different clinically (less sick and/or better responders) from the matched controls.35 However, the results of our sensitivity analysis suggest that the exclusion of those 25% of the survivors did not alter the primary association. By 90 days post-discharge, mortality rates were similar between the groups and as a result, hospice referral was also associated with a significantly lower risk of the combined end point of 90-day all-cause readmission or 90-day all-cause mortality.
Findings from the current study are of substantial public health importance. HF is the leading cause for 30-day all-cause readmission. Although the focus on 30-day in the Affordable Care Act has been criticized as short-sighted,36 a 25% 30-day readmission rate is unacceptably high. In our study, 41% of the hospice-eligible patients who died within 6 months post-discharge were readmitted within 30 days of discharge, which was nearly double the rate of 21% for overall HF patients in our study. Yet, this rate was 5% among the hospice-referral patients. Findings from our study also suggest that about 10% of the 1790 patients who died in the 6 months after discharge received hospice referral. A recent study observed a similar low rate for the receipt of palliative care services among contemporary HF patients.37 Future studies need to develop and test tools to identify hospice-eligible patients for potential hospice care, and to define evidence-based strategies to prevent readmission.
Several limitations of our study need to be acknowledged. As in any non-randomized study, findings of our study may potentially be confounded by imbalances in unmeasured covariates. However, findings from our sensitivity analysis suggest that hospice referral associated lower all-cause readmission was rather insensitive to a potential unmeasured confounder. For an unmeasured covariate to explain away this association it would need to increase the odds of 30-day all-cause readmission by nearly seven-fold. However, for such an imaginary unmeasured binary covariate to become a confounder, it would also need to be a near perfect predictor of 30-day all-cause readmission and could not be strongly correlated to any of the 28 variables used in our propensity score model. Other limitations include data derived from a single state during 1998–2001 may limit generalizability to more contemporary HF patients. However, resource utilization and prognostic characteristics of patients with end-stage HF have remained mostly unchanged in the past decade.35, 38 Further, a recent study of a 5% random national sample of Medicare beneficiaries from January 1, 2004 to December 31, 2009 demonstrated a very similar reduction in the risk of 30-day all-cause readmission associated with hospice enrollment within 30 days of hospital admission (adjusted HR, 0.12; 95% CI, 0.118–0.131).39 Most of the recent changes in the management of HF are more relevant to younger HF patients with low EF. Patients in our study had a mean age of 79 years and over half of them had preserved EF. We had no data on patient and care characteristics such as advance directive and indicators of end-stage HF such as symptoms status and in-hospital inotrope use that are often considered for hospice referral.24, 40 Finally, we had no data on socio-economic and personal preferences of patients and/or their family members and other psycho-social factors, which may potentially influence hospice referral and partly explain our findings.
In conclusion, most HF patients who died within 6 months of hospital discharge did not receive a discharge hospice referral, which was associated with lower 30-day all-cause readmission among Medicare beneficiaries hospitalized for decompensated HF. These data will likely stimulate much needed research to develop and test tools to identify hospice-eligible patients, and derive evidence regarding the impact of hospice care on 30-day all-cause readmission, for which HF is the leading cause and currently there are few sustainable effective interventions.
Supplementary Material
Acknowledgments
Source of Funding
Dr. Ahmed is supported by funds from the Veterans Affairs Capitol Health Care Network (VISN 5) to the Center for Health and Aging and was also in part supported by the National Institutes of Health through grants (R01-HL085561, R01-HL085561-S and R01-HL097047) from the National Heart, Lung, and Blood Institute. Dr. Bakitas was in part supported by a pilot/exploratory grant from the National Palliative Care Research Center.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the Veterans Health Administration, or the National Palliative Care Research Center.
Footnotes
Disclosures
None.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Rau J. Hospitals face pressure to avert readmissions. The new york times; New york: [December 2, 2012]. Published: November 26, 2012. Http://www.Nytimes.Com/2012/11/27/health/hospitals-face-pressure-from-medicare-to-avert-readmissions.Html?_r=0. [Google Scholar]
- 3.Feltner C, Jones CD, Cene CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, Arvanitis M, Lohr KN, Middleton JC, Jonas DE. Transitional care interventions to prevent readmissions for persons with heart failure: A systematic review and meta-analysis. Ann Intern Med. 2014;160:774–784. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- 4.Bourge RC, Fleg JL, Fonarow GC, Cleland JG, McMurray JJ, van Veldhuisen DJ, Gheorghiade M, Patel K, Aban IB, Allman RM, White-Williams C, White M, Filippatos GS, Anker SD, Ahmed A. Digoxin reduces 30-day all-cause hospital admission in older patients with chronic systolic heart failure. Am J Med. 2013;126:701–708. doi: 10.1016/j.amjmed.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashim T, Elbaz S, Patel K, Morgan CJ, Fonarow GC, Fleg JL, McGwin G, Cutter GR, Allman RM, Prabhu SD, Zile MR, Bourge RC, Ahmed A. Digoxin and 30-day all-cause hospital admission in older patients with chronic diastolic heart failure. Am J Med. 2014;127:132–139. doi: 10.1016/j.amjmed.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed A, Bourge RC, Fonarow GC, Patel K, Morgan CJ, Fleg JL, Aban IB, Love TE, Yancy CW, Deedwania P, van Veldhuisen DJ, Filippatos GS, Anker SD, Allman RM. Digoxin use and lower 30-day all-cause readmission for medicare beneficiaries hospitalized for heart failure. Am J Med. 2014;127:61–70. doi: 10.1016/j.amjmed.2013.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanam K, Bhatia V, Parvataneni S, Morgan CJ, Lloyd S, Hage FD, P S, Fonarow GC, Aronow WS, Mujib M, Deedwania P, Butler J, White M, Anker SD, Allman RM, Ahmed A. Discharge initiaion of ace inhibitors or arbs is associaed with significantly lower 30-day all-cause readmission in hospitalized older patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2014;63:12s. [Google Scholar]
- 8.Bhatia V, Bajaj NS, Sanam K, Hashim T, Morgan CJ, Prabhu SD, Fonarow GC, Deedwania P, Butler J, Carson P, Love TE, Kheirbek R, Aronow WS, Anker SD, Waagstein F, Fletcher R, Allman RM, Ahmed A. Beta-blocker use and 30-day all-cause readmission in medicare beneficiaries with systolic heart failure. Am J Med. 2014 Dec 29; doi: 10.1016/j.amjmed.2014.11.036. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inampudi C, Parvataneni S, Morgan CJ, Deedwania P, Fonarow GC, Prabhu SD, Butler J, Zile MR, Aronow WS, Sanders PW, Allman RM, Ahmed A. Lack of association between spironolactone use and 30-day all-cause readmission in hospitalized medicare beneficiaries with systolic heart failure eligible for spironolactone therapy. J Card Failure. 2014;20:58S. [Google Scholar]
- 10.Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O’Connor CM, Sun JL, Yancy CW, Young JB Investigators O-H, Hospitals. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: A report from the optimize-hf registry. J Am Coll Cardiol. 2007;50:768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 11.Bakitas M, Macmartin M, Trzepkowski K, Robert A, Jackson L, Brown JR, Dionne-Odom JN, Kono A. Palliative care consultations for heart failure patients: How many, when, and why? J Card Fail. 2013;19:193–201. doi: 10.1016/j.cardfail.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feller MA, Mujib M, Zhang Y, Ekundayo OJ, Aban IB, Fonarow GC, Allman RM, Ahmed A. Baseline characteristics, quality of care, and outcomes of younger and older medicare beneficiaries hospitalized with heart failure: Findings from the alabama heart failure project. Int J Cardiol. 2012;162:39–44. doi: 10.1016/j.ijcard.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 14.Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- 15.Ahmed A, Husain A, Love TE, Gambassi G, Dell’Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: An observational study using propensity score methods. Eur Heart J. 2006;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, Adams KF, Gheorghiade M. Digoxin and reduction in mortality and hospitalization in heart failure: A comprehensive post hoc analysis of the dig trial. Eur Heart J. 2006;27:178–186. doi: 10.1093/eurheartj/ehi687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed A, Fonarow GC, Zhang Y, Sanders PW, Allman RM, Arnett DK, Feller MA, Love TE, Aban IB, Levesque R, Ekundayo OJ, Dell’Italia LJ, Bakris GL, Rich MW. Renin-angiotensin inhibition in systolic heart failure and chronic kidney disease. Am J Med. 2012;125:399–410. doi: 10.1016/j.amjmed.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmed A, Rich MW, Zile M, Sanders PW, Patel K, Zhang Y, Aban IB, Love TE, Fonarow GC, Aronow WS, Allman RM. Renin-angiotensin inhibition in diastolic heart failure and chronic kidney disease. Am J Med. 2013;126:150–161. doi: 10.1016/j.amjmed.2012.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mujib M, Patel K, Fonarow GC, Kitzman DW, Zhang Y, Aban IB, Ekundayo OJ, Love TE, Kilgore ML, Allman RM, Gheorghiade M, Ahmed A. Angiotensin-converting enzyme inhibitors and outcomes in heart failure and preserved ejection fraction. Am J Med. 2013;126:401–410. doi: 10.1016/j.amjmed.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenbaum PR. Sensitivity to hidden bias. In: Rosenbaum PR, editor. Observational studies. New York: Springer-Verlag; 2002. pp. 105–170. [Google Scholar]
- 21.Zile MR, Gaasch WH, Anand IS, Haass M, Little WC, Miller AB, Lopez-Sendon J, Teerlink JR, White M, McMurray JJ, Komajda M, McKelvie R, Ptaszynska A, Hetzel SJ, Massie BM, Carson PE Investigators IP. Mode of death in patients with heart failure and a preserved ejection fraction: Results from the irbesartan in heart failure with preserved ejection fraction study (i-preserve) trial. Circulation. 2010;121:1393–1405. doi: 10.1161/CIRCULATIONAHA.109.909614. [DOI] [PubMed] [Google Scholar]
- 22.Kheirbek RE, Alemi F, Citron BA, Afaq MA, Wu H, Fletcher RD. Trajectory of illness for patients with congestive heart failure. J Palliat Med. 2013;16:478–484. doi: 10.1089/jpm.2012.0510. [DOI] [PubMed] [Google Scholar]
- 23.Barnes S, Gott M, Payne S, Parker C, Seamark D, Gariballa S, Small N. Predicting mortality among a general practice-based sample of older people with heart failure. Chronic Illn. 2008;4:5–12. doi: 10.1177/1742395307083783. [DOI] [PubMed] [Google Scholar]
- 24.Levenson JW, McCarthy EP, Lynn J, Davis RB, Phillips RS. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc. 2000;48:S101–109. doi: 10.1111/j.1532-5415.2000.tb03119.x. [DOI] [PubMed] [Google Scholar]
- 25.Enguidanos S, Vesper E, Lorenz K. 30-day readmissions among seriously ill older adults. J Palliat Med. 2012;15:1356–1361. doi: 10.1089/jpm.2012.0259. [DOI] [PubMed] [Google Scholar]
- 26.National Hospice and Palliative Care Organization. Nhpco’s facts and figures: Hospice care in america 2014 edition. 2014 Http://www.Nhpco.Org/sites/default/files/public/statistics_research/2014_facts_figures.Pdf.
- 27.Wachterman MW, Marcantonio ER, Davis RB, McCarthy EP. Association of hospice agency profit status with patient diagnosis, location of care, and length of stay. JAMA. 2011;305:472–479. doi: 10.1001/jama.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adler ED, Goldfinger JZ, Kalman J, Park ME, Meier DE. Palliative care in the treatment of advanced heart failure. Circulation. 2009;120:2597–2606. doi: 10.1161/CIRCULATIONAHA.109.869123. [DOI] [PubMed] [Google Scholar]
- 29.Goodlin SJ. Palliative care in congestive heart failure. J Am Coll Cardiol. 2009;54:386–396. doi: 10.1016/j.jacc.2009.02.078. [DOI] [PubMed] [Google Scholar]
- 30.Heart Failure Society of A. Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN. Hfsa 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16:e1–194. doi: 10.1016/j.cardfail.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Solomon DH, Rassen JA, Glynn RJ, Lee J, Levin R, Schneeweiss S. The comparative safety of analgesics in older adults with arthritis. Arch Intern Med. 2010;170:1968–1976. doi: 10.1001/archinternmed.2010.391. [DOI] [PubMed] [Google Scholar]
- 32.Peacock WF, Hollander JE, Diercks DB, Lopatin M, Fonarow G, Emerman CL. Morphine and outcomes in acute decompensated heart failure: An adhere analysis. Emerg Med J. 2008;25:205–209. doi: 10.1136/emj.2007.050419. [DOI] [PubMed] [Google Scholar]
- 33.Cuffe MS, Califf RM, Adams KF, Jr, Benza R, Bourge R, Colucci WS, Massie BM, O’Connor CM, Pina I, Quigg R, Silver MA, Gheorghiade M. Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure I. Short-term intravenous milrinone for acute exacerbation of chronic heart failure: A randomized controlled trial. JAMA. 2002;287:1541–1547. doi: 10.1001/jama.287.12.1541. [DOI] [PubMed] [Google Scholar]
- 34.Packer M, Carver JR, Rodeheffer RJ, Ivanhoe RJ, DiBianco R, Zeldis SM, Hendrix GH, Bommer WJ, Elkayam U, Kukin ML, Mallis GI, Sollano JA, Shannon J, Tandon PK, DeMets DL. Effect of oral milrinone on mortality in severe chronic heart failure. The promise study research group. N Engl J Med. 1991;325:1468–1475. doi: 10.1056/NEJM199111213252103. [DOI] [PubMed] [Google Scholar]
- 35.Teno JM, Plotzke M, Gozalo P, Mor V. A national study of live discharges from hospice. J Palliat Med. 2014;17:1121–1127. doi: 10.1089/jpm.2013.0595. [DOI] [PubMed] [Google Scholar]
- 36.Konstam MA. Heart failure in the lifetime of musca domestica (the common housefly) JACC-Heart Failure. 2013;1:178–180. doi: 10.1016/j.jchf.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 37.Greener DT, Quill T, Amir O, Szydlowski J, Gramling RE. Palliative care referral among patients hospitalized with advanced heart failure. J Palliat Med. 2014;17:1115–1120. doi: 10.1089/jpm.2013.0658. [DOI] [PubMed] [Google Scholar]
- 38.Unroe KT, Greiner MA, Hernandez AF, Whellan DJ, Kaul P, Schulman KA, Peterson ED, Curtis LH. Resource use in the last 6 months of life among medicare beneficiaries with heart failure, 2000-2007. Arch Intern Med. 2011;171:196–203. doi: 10.1001/archinternmed.2010.371. [DOI] [PubMed] [Google Scholar]
- 39.Holden TR, Smith MA, Bartels CM, Campbell TC, Yu M, Kind AJ. Hospice enrollment, local hospice utilization patterns, and rehospitalization in medicare patients. J Palliat Med. 2015 doi: 10.1089/jpm.2014.0395. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Butler J, Binney Z, Kalogeropoulos A, Owen M, Clevenger C, Gunter D, Georgiopoulou V, Quest T. Advance directives among hospitalized patients with heart failure. JACC Heart Fail. 2015;3:112–21. doi: 10.1016/j.jchf.2014.07.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


