Abstract
Study Design
A study of agreement between different measures of kyphosis, a clinical standing measure (Debrunner kyphometer; Protek AG, Bern, Switzerland) versus a supine radiologic measure (Cobb angle).
Objectives
To determine whether a supine radiologic measure of kyphosis in older women is a reasonable estimate of clinical kyphosis determined in the standing position, and to investigate a computerized assessment of the Cobb angle.
Summary of Background Data
Few studies have investigated kyphosis measurement agreement involving older adults.
Methods
Using data from the Fracture Intervention Trial, we randomly selected 120 women, aged 55– 80 years, who had a Debrunner kyphometer measure of kyphosis and supine lateral spine radiographs from which we measured the Cobb angle (either manually or by digitization). We calculated the intraclass correlation coefficient (ICC) from repeated measures analysis of variance to assess the agreement among the: (1) manual Cobb angle and Debrunner kyphometer, (2) digitized Cobb angle and Debrunner kyphometer, and (3) manual and digitized Cobb angle.
Results
The mean of both the manual and digitized Cobb angle was 45° (range 18°– 83°), and the mean Debrunner kyphometer reading was 48° (range 17°– 83°). The ICC between either of the 2 measures of the Cobb angle and Debrunner measurement was 0.68, indicating reasonable agreement. The ICC between the manual and digitized Cobb angle was 0.99, indicating excellent agreement.
Conclusions
There is reasonable agreement between a supine radiologic and standing clinical measurement of kyphosis in older women.
Keywords: kyphosis, hyperkyphosis, measurement, Cobb angle, Debrunner kyphometer
The dowager’s hump, an accentuated angle of thoracic’s kyphosis, is often observed in older women and is associated with osteoporosis. Also sometimes referred to as hyperkyphosis, it is associated with impaired pulmonary function,1–3 poor physical function,4 – 6 and an increased risk of mortality.7 Given that hyperkyphosis is prevalent in the older population and apparently associated with poor health, remarkably little is understood about its causes and consequences, and only a few interventions specific to hyperkyphosis have been implemented in small-scale research settings.8 –10 To understand better the causes and consequences of hyperkyphosis in older persons, large-scale epidemiologic studies are needed.
Before large-scale studies can be performed, a consistent and efficient measure of thoracic angle curvature is necessary. Many methods of measuring thoracic spinal curvature are available, including both clinical and radiologic methods. Examples of clinical measures of kyphosis include: (1) the Debrunner kyphometer (Protek AG, Bern, Switzerland), a moveable protractor placed on the spine (Figure 1); and (2) a flexicurve measurement that consists of a flexible ruler that molds to the spinal curvature, from which the outline of the spine is traced, and an angle of curvature calculated. The most widely used radiologic reading is the modified Cobb angle, that when manually performed in the traditional way, requires drawing straight lines from the superior edge of the vertebra, delineating the top of the curve and the inferior edge of the vertebra, marking the bottom of the thoracic curve (usually T4 and T12) and using a protractor to determine the angle of intersection, known as the kyphotic angle (Figure 2).
Figure 1.
The Debrunner kyphometer is shown placed on a subject’s spine.
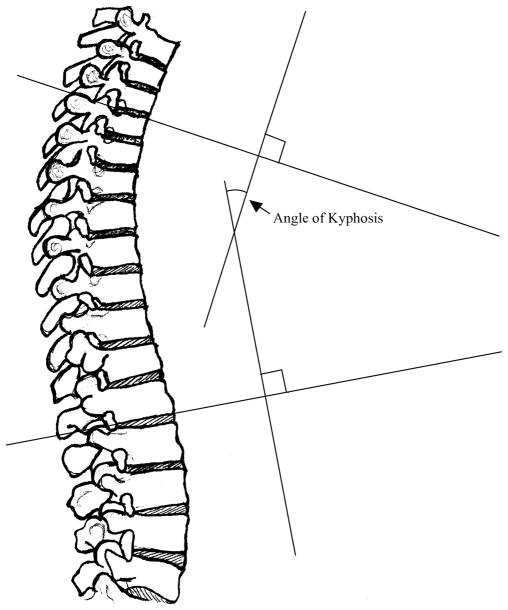
Figure 2.
The Cobb angle of kyphosis, calculated from a lateral radiograph, is shown. The higher the angle, the higher the thoracic curvature. Modern methods use T4 as the superior landmark and T12 as the inferior.
Few studies have examined the correlation between different kyphosis measurements, and most have been performed in the younger population.11–14 In addition, except for a cadaver study,13 all research measurements of kyphosis have been performed with subjects in the standing position. However, in clinical practice and osteoporosis research studies, lateral spine radiographs are often taken in the supine position for patient comfort and to reduce motion artifact. How a supine radiologic measurement of the kyphosis angle correlates with a standing measure is not known. Furthermore, particularly in the very old patient, standing measurements may be difficult to obtain so that supine measurements may be more clinically applicable.
To study the correlation between a standing clinical and supine radiologic measure of kyphosis in older women, we randomly selected a subset of 120 participants enrolled in the Fracture Intervention Trial (FIT) who had baseline measurements of kyphosis performed with the Debrunner kyphometer and compared this standing clinical measure to the Cobb angle calculated from baseline radiographs taken in the lateral supine position. We also developed a digitization program to calculate automatically the Cobb angle from digitized points, and determined the correlation between the digitized and manual Cobb angle measurements.
Methods
Study subjects were a randomly selected subset of participants from the FIT, a randomized, double-blind, placebo-controlled trial originally designed to test the hypothesis that alendronate would reduce the rate of fractures in women aged 55– 80 years with low hip bone mineral density (0.68 g/cm2). The overall study design has been previously published.15 In brief, this trial was conducted at 11 clinical centers in the United States, with a coordinating center at the University of California, San Francisco. The FIT had 2 arms: (1) the vertebral fracture arm, which included women who had at least 1 vertebral deformity (n = 2027); and (2) the clinical fracture arm, which included women without baseline vertebral fractures (n = 4432). All women provided written informed consent, and appropriate institutional review boards approved the study protocol. For the purposes of this study, all data from the participants were collected at baseline, except the manual and digitized Cobb angles, which were measured in 2003 from archived baseline radiographs.
To assess the agreement between pairs of 2 continuous measurements (kyphosis angles measured by each technique), we calculated that a study of 100 persons would offer more than 90% power to determine a correlation of ≥ 0.25 (P < 0.05). At baseline, the Debrunner kyphometer was used to measure the angle of kyphosis in all 6459 participants. We divided the entire cohort into deciles based on the Debrunner measurement, and then selected 12 subjects from each decile to ensure a good range of kyphosis measurements and allow for possible loss of subjects because of potential data acquisition problems.
Debrunner Kyphometer Measurement
Trained clinical personnel performed the clinical measurement of kyphosis in strict accordance with a standard protocol. They used the Debrunner kyphometer, which is a protractor with a 1° scale at the end of 2 double, parallel arms connected to blocks that are large enough to span 2 spinous processes. The protractor measures the angle of curvature when the blocks are placed at the upper and lower limits of the thoracic spine.
To identify the proper landmarks for block placement, a wooden positioning device was placed under an elastic band that was fastened around the subject at a level approximately three quarters of an inch above the iliac crest. By palpating the first prominence on the spine directly above the wooden positioning device, the T12 spinous process was located and marked with a dot of a pen. If not easily palpated, then the T12 spinous process was estimated by placing the dot half an inch above the wooden positioning device. The C7 spinous process was located by palpating the first prominence at the lower end of the neck and a corresponding dot made by a pen.
Following the dot placement, the subject was then asked to stand in her usual posture with her arms swinging gently at her sides. The examiner placed the kyphometer on the spine so that the upper foot of its upper block was directly over the C7 spinous process and the lower foot of its lower block was directly over the T12 spinous process, and read the angle on the protractor to the nearest degree. The examiner repeated the procedure once, and if the 2 measurements differed by more than 5°, both measurements were repeated and the second set of measurements recorded. Excellent intraobserver and interobserver reliability have been previously reported (correlation coefficients ≥ 0.91 and coefficient of variation for repeated measurements = 8.4%).16
Cobb Angle Measurement
Certified technicians obtained lateral thoracic spine radiographs according to published guidelines using medium screen film speed at a distance of 40 inches (102 cm) with a vertical beam centered on T7.17 A trained technician (L.C.), experienced in both semiquantitative method and point digitization method of assessing vertebral deformities, calculated the Cobb angle 2 ways: (1) by performing a manual reading and (2) by placing digitized points to permit an automated computer reading.
To perform the manual reading, the technician drew straight lines on the radiograph extending from the top of T4 and the bottom of T12 to the posterior of the spine. From each of these 2 lines, perpendicular lines were drawn, and the angle of intersection, or Cobb angle, was calculated using a protractor (Figure 2). To do the digitized reading, the technician had to identify and place digitized points demarcating the upper endplate inner and outer corners of T4, and lower endplate inner and outer corners of T12. The computerized program uses these 4 points to erect straight lines and determine the angle of intersection. If for any reason either the upper end of T4 or lower end of T12 were not well visualized, the adjacent above and below vertebrae were used as alternative upper or lower vertebral bodies to define the angle of curvature.
To assess intrarater reliability, 3 months after the initial study was completed, the original marks were erased, and copies of 20 randomly selected films were obtained. The technician, blinded to the original measurements, recalculated the manual Cobb angle and also redigitized the films so that the computerized Cobb angle could be repeated. Although the technician who performed the Cobb angle measurements is a health professional and an expert in vertebral morphometry, an expert radiologist (R.S.B.) reviewed 25 films to verify that the Cobb angle measurements were being performed correctly.
Statistical Analysis
To assess the agreement between the standing clinical (Debrunner) and supine radiologic (Cobb, performed either manually or by digitization), we calculated the intraclass correlation coefficient (ICC) estimated from repeated measures analysis of variance. Similar analyses were performed to assess the intrarater reliability. SAS software (SAS Institute, Cary, NC) was used for all analyses, and STATA software (StataCorp, College Station, TX) was used to generate the data figures.
Results
Women in this study were an average age of 68.6 ± 5.9 years, and 36 of the 120 participants had evidence of a baseline vertebral fracture. The Debrunner mean angle of kyphosis was 47.8° ± 12.0°, the manual Cobb mean angle was 44.8° ± 12.7°, and the digitized Cobb mean angle was 44.8° ± 12.7°, indicating that the standing measure was about 4° higher than the lying measure, as might be expected because the lying measure does not consider the effects of gravity. We found that 60% of the clinical Debrunner measurements overestimated the manual Cobb measurements, 38% of the manual Cobb measurements overestimated the Debrunner measurements, 23% of the measurements were within 2° of agreement, and 2% yielded identical readings.
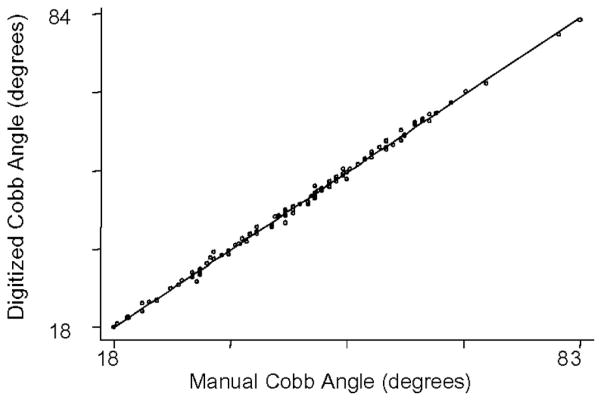
The ICC between the standing Debrunner and supine Cobb angle calculated manually was 0.68, and the ICC between the standing Debrunner and supine Cobb angle calculated by digitization was 0.68, indicating identical agreement between either Cobb angle and the clinical Debrunner measurement. Scatterplots of either the manual or digitized Cobb angle and the Debrunner measurement reveal consistent linear trends (Figures 3, 4). The ICC between the manual and digitized Cobb angle readings was 0.99, indicating near perfect agreement (Figure 5).
Figure 3.
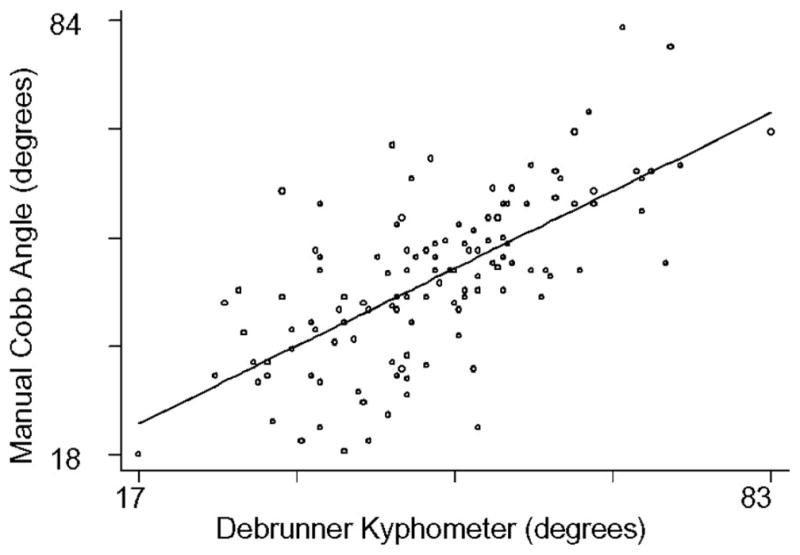
Scatterplot of the manual Cobb angle and Debrunner kyphometer.
Figure 4.
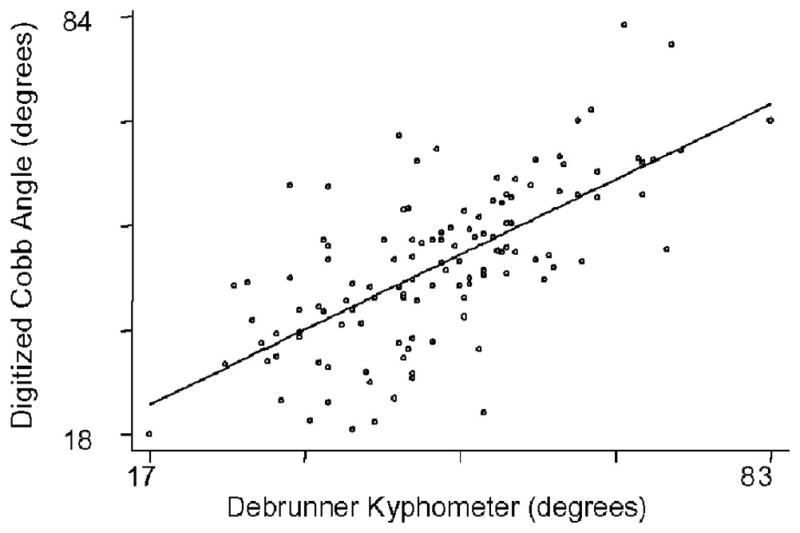
Scatterplot of the digitized Cobb angle and Debrunner kyphometer.
Figure 5.
Scatterplot of the manual and digitized Cobb angles.
Examining the raw data more closely revealed that, although there was general good agreement between the Debrunner and supine Cobb angle with 75% of the readings being in a range of agreement of about 12°, which is equal to a standard deviation of the measurement itself, 15% of the readings were off by at least 15°, and about 5% of the readings were off by ≥20°. In fact, as the differences between the 2 measures got bigger, the Debrunner measurement was twice as likely to overestimate the Cobb angle. When considering the measurement agreement only among those with higher degrees of kyphosis (manual Cobb angle ≥50°), the ICC between the Debrunner kyphometer and Cobb angle decreased to only 0.44. Comparing the manual versus digitized Cobb angles among those with a manual Cobb angle of ≥50° revealed no change in the ICC, which remained extremely high at 0.99.
Of the 120 films originally selected, 4 were unable to be read because of poor visualization of the upper thoracic vertebrae. There were 4 other films randomly selected to complete the target goal of 120 films. In the end, the technician could not visualize the upper endplate of T4 in 5 films so that T3 was used in 1 case, and T5 was used in the remaining 4. T12 was well visualized in all but 3 films, in which case T11 was used as an alternate level. Of the 25 films that the radiologist also reviewed, there was only 1 disagreement in which the radiologist believed that the subject had an extra lumbar vertebra, so that the vertebra originally labeled as T11 by the technician should have been designated as T12. The intrarater reliability ICC was 0.997 for repeated manual Cobb angle readings and 0.984 for repeated digitized readings performed in a subset of 20 participants.
Discussion
In older women, a clinical standing measure of kyphosis was significantly correlated with a supine radiologic measure, regardless if the radiologic measure was measured manually or via computer digitization. Although it is expected that gravitational forces acting on posture might worsen the degree of kyphosis when measuring thoracic spinal curvature in a standing versus lying position, the gravitational difference in actual measurement appears to be small on average, except among those patients with kyphosis readings in the higher range. Because the clinical standing measurement is taken from C7 through T12 and the radiologic measurement calculates the thoracic angle from T4 through T12, the absolute values obtained are close.
Although these results suggest an acceptable agreement between the standing Debrunner and supine Cobb angle measurements, we do not suggest that these 2 measures are measuring the same entity. Both are designed to capture upper thoracic curvature, but the range (i.e., from C7 through T12 vs. T4 through T12) and difference in positions from which they are measured suggest that there should be some differences between these 2 measures. These differences are reflected by the imperfect agreement (ICC = 0.68) that becomes more pronounced at higher degrees of kyphosis (ICC = 0.44 for those with Cobb angles ≥50°). We hypothesized that perhaps as the degree of kyphosis worsens, the effects of posture may be higher, leading to a bigger difference between the lying and standing measures. Whether gravitational postural effects on the thoracic angle of curvature are clinically important is unknown, but they deserve further consideration.
Because there was reasonable agreement between the Debrunner kyphometer and Cobb angle measurements performed in the standing versus supine position, these results suggest that either measure could potentially work in furthering the study of kyphosis curvature in older women. Unless specifically interested in studying gravitational postural effects on thoracic curvature, we suggest that lying radiographs may provide the easiest measure because many are taken in longitudinal studies of osteoporosis in the study of vertebral fractures. Furthermore, a digitized computation of the Cobb angle also could prove to be an efficient way to measure thoracic curvature because it only involves identifying correct vertebral levels and marking 2 levels on a spine so that an angle of curvature can be automatically calculated. In addition, there was outstanding agreement between the manual and digitized Cobb angle reading (ICC = 0.99), indicating that the manual versus digitized Cobb angle measurements are interchangeable.
Our study has some limitations. First, we were unable to perform a direct comparison of the same method done in different positions to more precisely isolate how gravity might influence the readings. Second, we were unable to consider how adjacent spine deformities outside the range of T4 –T12 might have influenced the angle of curvature. Our study also had some strengths. First, we had a well-powered study to detect significant correlations between 2 different measures of kyphosis performed during the same interval, but where the examiners were blinded to the results of the other measurement. Second, we had an experienced technician, blinded to the different radiologic measurements, perform the Cobb angle readings. Third, although the Cobb angle reading has been quoted as the “gold standard” measurement of kyphosis, its use in large populations has been limited because of the time-consuming cumbersome measurements.
The digitized version of the Cobb angle will offer the opportunity to expedite this process, while maintaining accuracy. Our study provides a solid basis for future research in the epidemiology of kyphosis in the older persons. Whether measured in a standing versus supine position, there was reasonable agreement between a clinical and radiologic assessment of kyphosis, and the correlation between a manual and digitized version of the Cobb angle was outstanding.
Key Points.
Few studies have investigated kyphosis measurement agreement in older persons, and, yet, the dowager’s hump is a common condition affecting older women.
There is reasonable agreement between a standing clinical (Debrunner kyphometer) and supine radiologic measure (Cobb angle) of kyphosis in older women.
The digitized Cobb angle is easier to calculate than the manual measure and may be suitable for use in large studies.
Acknowledgments
Supported by Public Health Service Grant 1K12AG01004 and 1R01AG024246, and the Claude D. Pepper Older Americans Independent Center (5P60AG10415-11).
Corporate/Industry, Federal, and Institutional funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
The authors thank Mei-Hua Huang, Crystal Leutters, Sue Hirsch, and Ana Jurado for their assistance in the preparing the figures for this manuscript.
References
- 1.Leech JA, Dulberg C, Kellie S, et al. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141:68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 2.Schlaich C, Minne HW, Bruckner T, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int. 1998;8:261–7. doi: 10.1007/s001980050063. [DOI] [PubMed] [Google Scholar]
- 3.Di Bari M, Chiarlone M, Matteuzzi D, et al. Thoracic kyphosis and ventilatory dysfunction in unselected older persons: An epidemiological study in Dicomano, Italy. J Am Geriatr Soc. 2004;52:909–15. doi: 10.1111/j.1532-5415.2004.52257.x. [DOI] [PubMed] [Google Scholar]
- 4.Chow RK, Harrison JE. Relationship of kyphosis to physical fitness and bone mass on post-menopausal women. Am J Phys Med. 1987;66:219–27. [PubMed] [Google Scholar]
- 5.Ryan SD, Fried LP. The impact of kyphosis on daily functioning. J Am Geriatr Soc. 1997;45:1479–86. doi: 10.1111/j.1532-5415.1997.tb03199.x. [DOI] [PubMed] [Google Scholar]
- 6.Kado DM, Huang MH, Barrett-Connor E, et al. Hyperkyphotic posture and poor physical functional ability in older community-dwelling men and women: the Rancho Bernardo study. J Gerontol A Biol Sci Med Sci. 2005;60:633–7. doi: 10.1093/gerona/60.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kado DM, Huang MH, Karlamangla A, et al. Hyperkyphotic posture predicts mortality in older community dwelling men and women: A prospective study. J Am Geriatr Soc. 2004;62:1662–7. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 8.Itoi E, Sinaki M. Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc. 1994;69:1054–9. doi: 10.1016/s0025-6196(12)61372-x. [DOI] [PubMed] [Google Scholar]
- 9.Greendale GA, McDivit A, Carpenter A, et al. Yoga for women with hyperkyphosis: Results of a pilot study. Am J Public Health. 2002;92:1611–4. doi: 10.2105/ajph.92.10.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teng MM, Wei CJ, Wei LC, et al. Kyphosis correction and height restoration effects of percutaneous vertebroplasty. Am J Neuroradiol. 2003;24:1893–900. [PMC free article] [PubMed] [Google Scholar]
- 11.Stotts AK, Smith JT, Santora SD, et al. Measurement of spinal kyphosis: Implications for the management of Scheuermann’s kyphosis. Spine. 2002;27:2143–6. doi: 10.1097/00007632-200210010-00013. [DOI] [PubMed] [Google Scholar]
- 12.Korovessis P, Petsinis G, Papazisis Z, et al. Prediction of thoracic kyphosis using the Debrunner kyphometer. J Spinal Disord. 2001;14:67–72. doi: 10.1097/00002517-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Goh S, Price RI, Leedman PJ, et al. A comparison of three methods for measuring thoracic kyphosis: Implications for clinical studies. Rheumatology (Oxford) 2000;39:310–5. doi: 10.1093/rheumatology/39.3.310. [DOI] [PubMed] [Google Scholar]
- 14.Lundon KM, Li AM, Bibershtein S. Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine. 1998;23:1978–85. doi: 10.1097/00007632-199809150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Black DM, Reiss TF, Nevitt MC, et al. Design of the Fracture Intervention Trial. Osteoporos Int. 1993;3(suppl 3):S29–39. doi: 10.1007/BF01623005. [DOI] [PubMed] [Google Scholar]
- 16.Ohlen G, Spangfort E, Tingvall C. Measurement of spinal sagittal configuration and mobility with Debrunner’s kyphometer. Spine. 1989;14:580–3. doi: 10.1097/00007632-198906000-00006. [DOI] [PubMed] [Google Scholar]
- 17.National Osteoporosis Foundation Working Group on Vertebral Fractures. Assessing vertebral fractures. J Bone Miner Res. 1995;10:518–23. doi: 10.1002/jbmr.5650100403. [DOI] [PubMed] [Google Scholar]