Abstract
Purpose
The study sought to examine the association of mental disorders with educational attainment in a community sample.
Methods
Data were from 5,001 respondents aged 15–54 in the 1990–1992 National Comorbidity Survey (NCS), re-interviewed in the 2001–2003 NCS follow-up (NCS-2). Discrete-time survival analysis was used to examine the association of disorders present at baseline (NCS) or having first onset after the baseline (assessed in NCS-2) with educational outcomes among 3,954 eligible respondents. Mental disorders were categorized into internalizing fear disorders (simple phobia, social phobia, panic disorder with/without agoraphobia and agoraphobia without panic disorder), internalizing anxiety-misery disorders (major depressive disorder, generalized anxiety disorder and post-traumatic stress disorder), externalizing disorders (alcohol and drug use disorders, conduct disorder) and bipolar disorder. Analyses were conducted separately in students and non-students at baseline.
Results
Among students, baseline bipolar and externalizing disorders, and fear, anxiety-misery and externalizing disorders with onset after baseline were associated with lower odds of high school graduation; baseline anxiety-misery disorders with lower odds of going to college; and baseline externalizing disorders and bipolar disorder with onset after baseline with lower odds of college graduation. Among non-students, baseline fear disorders were associated with lower odds of high school graduation and bipolar disorder with lower odds of going to college. Assuming that the regression coefficients represent causal effects, mental disorders accounted for 5.8–11.0% of high school and 3.2–11.4% of college non-completion.
Conclusions
Expanding access to mental health services for youth might have a net positive societal value by helping to prevent some of these adverse educational outcomes.
INTRODUCTION
Virtually all young people in the US have access to education through high school. However, nearly one-fourth never graduate from high school, about one-third of high school graduates do not enter college, and about half of those who enter college do not graduate from a 4-year college [1]. These truncated educational careers are important from an individual perspective because success in the educational system is critical to social and economic success [2–4] and to the development of lifestyle behaviors associated with health and well-being [5,6]. Educational attainment is also important from a societal perspective because a nation’s ability to increase its standard of living, compete in global markets, and promote participation in civic affairs all require an educated citizenry.
Associations of child and adolescent mental disorders with subsequent educational attainment have been examined in both cross-sectional and prospective studies [7–21]. Results have been inconsistent, with the majority of studies, but not all [9], finding significant gross associations of childhood and adolescent mental disorders with low levels of educational attainment and some finding that significant gross associations are explained by childhood adversities that preceded onset of the disorders [11,22]. However, these inconsistencies might be due to differences in ascertainment, specification bias, or statistical power [11], calling for additional studies based on large and prospective samples. Furthermore, the associations of mental disorders with return to schooling among individuals who experienced a disruption in education have not been examined previously. A better understanding of these associations might be useful in designing outreach programs aimed at increasing educational retention [23].
The current study uses prospective data from panel respondents in the 1990–1992 National Comorbidity Survey (NCS) and the 2001–2003 NCS follow-up (NCS-2) to examine associations of baseline mental disorders with subsequent educational attainment. Previously published cross-sectional analyses of the baseline NCS used retrospective age-of-onset reports to estimate associations of lifetime mental disorders with subsequent educational attainment, concluding that these disorders account for 14.2% of high school drop-out and 4.7% of college drop-out in the US [14]. We update these estimates in the current report based on prospective data from the NCS panel. We also examine associations of mental disorders with return to schooling among individuals who experienced a gap in their education.
METHODS
Sample
The NCS was a nationally representative survey of the US household population designed to study prevalence and correlates of DSM-III-R mental and substance disorders. The NCS was carried out by the Survey Research Center (SRC) at the Institute for Social Research at the University of Michigan (https://www.src.isr.umich.edu/), the largest academic survey research organization in the US. The baseline survey was administered to 8,098 respondents aged 15–54 in the non-institutionalized civilian population of the 48 coterminous states [24]. The response rate was 82.4%. Interviews were conducted face-to-face by professional lay interviewers and administered in two parts. Part I, which included the core diagnostic interview, was administered to all respondents. Part II, which included assessments of additional disorders and risk factors, was administered to a probability subsample of 5,877 respondents including all those in the age range 15–24, all others with any lifetime DSM-III-R disorder assessed in Part I, and a random sub-sample of other Part I respondents. The Part II sample was weighted to adjust for differential probabilities of selection and for discrepancies between the sample and the Census population on a wide range of socio-demographic and geographic variables. Further details about the NCS design and weighting are reported elsewhere [24].
The NCS-2 sought to trace and re-interview all 5,877 Part II NCS respondents. Exhaustive tracing procedure developed by SRC for were used to locate respondents. A total of 5,463 cases were successfully resolved (166 deceased, 5,001 re-interviewed), for a conditional response rate of 87.6%. The percentage of baseline respondents interviewed in both surveys was 72.2% (0.876 × 0.824). NCS-2 respondents were administered an expanded version of the baseline interview assessing onset and course of disorders between the two surveys. Relative to other baseline NCS respondents, those who were successfully followed up and re-interviewed in NCS-2 were significantly more likely to be female, well-educated, and residents of rural areas. A non-response adjustment weight corrected for these differences [25]. Analyses are based on these weighted data.
Assessments
Diagnostic assessment
The baseline NCS assessed lifetime DSM-III-R disorders using a modification of the World Health Organization Composite International Diagnostic Interview (CIDI) Version 1.1, a fully-structured, lay-administered diagnostic interview [26]. Lifetime DSM-IV disorders with first onsets between the two interviews were assessed in the NCS-2 using CIDI Version 3.0 [27].
The number of individuals in the samples for each of the individual mental disorders was quite small, resulting in unreliable estimates of the associations between individual NCS disorders and subsequent educational transitions. We addressed this problem by grouping NCS disorders into categories suggested by latent variable analyses in previous studies [28,29] into internalizing fear disorders (simple phobia, social phobia, panic disorder with/without agoraphobia and agoraphobia without panic disorder), internalizing anxiety-misery disorders (major depressive disorder, generalized anxiety disorder and post-traumatic stress disorder), and externalizing disorders (alcohol and drug use disorders, conduct disorder). A summary measure for bipolar disorder was used which combined bipolar disorder Type I and II with subclinical mania to assess broadly-defined bipolar disorder.
Alcohol and drug dependence was assessed only among individuals meeting criteria for DSM abuse. DSM organic exclusion rules were used in making diagnoses in both surveys. DSM-IV disorders reported for the first time at the NCS-2 interview but estimated by respondents to have had their onset prior to the baseline NCS interview were so coded. Blinded clinical reappraisal interviews administered to a probability sub-sample of respondents using the Structured Clinical Interview for DSM-III-R [30] in the NCS and the Structured Clinical Interview for DSM-IV (SCID) [31] in the NCS-2 documented generally good concordance between diagnoses based on the CIDI and independent diagnoses based on blinded clinical reappraisal interviews [32,33].
Education
Education was assessed by asking respondents the number of years of education they completed and whether or not they were currently students. The same questions were asked in both NCS and NCS-2. Respondents who completed 12 years of education were classified as having completed high school, those with 13+ years of education as having started college, and those with 16+ years of education as having completed college.
Childhood adversities
As detailed elsewhere [34], the NCS assessed a number of childhood family adversities that might have been common causes of mental disorders and low educational attainment. These included three parental mental disorders (major depressive disorder, generalized anxiety disorder, substance use disorder), family violence, and two aspects of exposure to child abuse (physical abuse and sexual abuse). For this study, a composite score was computed as the sum of these 6 childhood adversities.
Socio-demographic controls
The socio-demographic characteristics considered in this study included age, sex, race/ethnicity, marital status, and number of years of education of the major breadwinner of the respondent’s family of origin.
Analytic approach
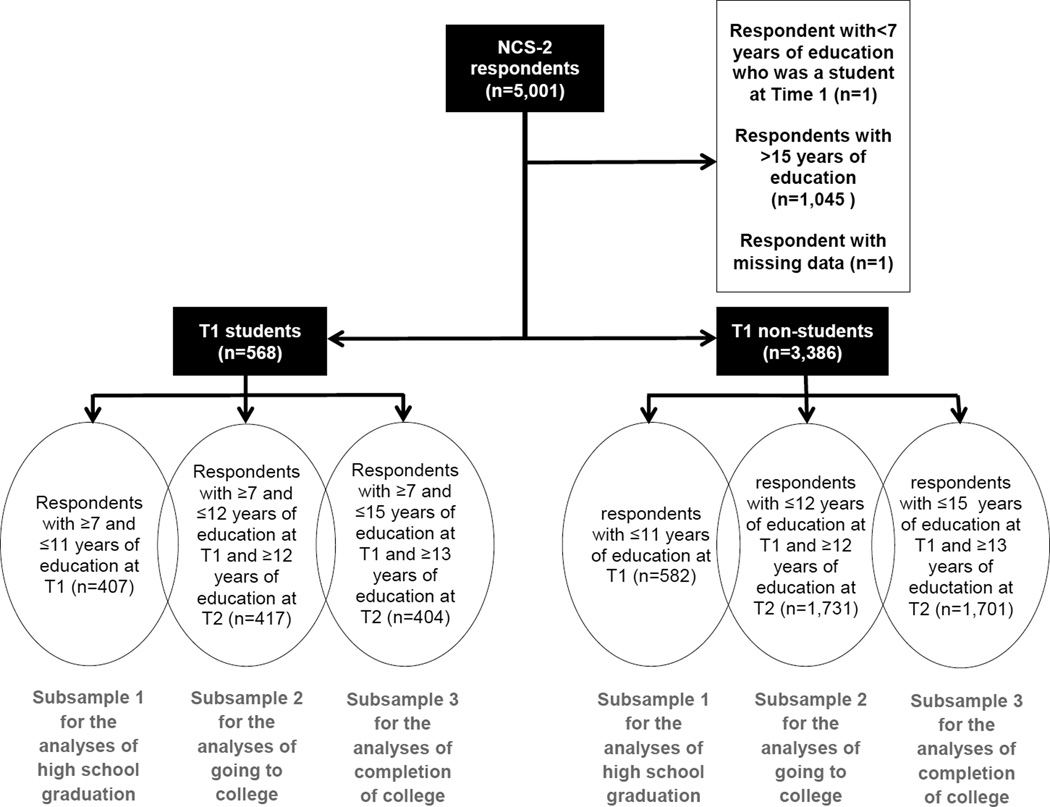
Analyses examined the associations of lifetime mental disorders assessed in the NCS (T1) and disorders with first onset after the NCS (as reported in the NCS-2 [T2]) but before the educational outcome of interest, with each of the three educational outcomes: graduation from high school, going to college, and completing college. The analyses were conducted separately in three overlapping subsamples among students and non-students (Figure 1). Each subsample was comprised of those respondents only who could potentially experience the outcome of interest. Thus, for example, 1,045 respondents with 16+ years of education at T1 were excluded from all analyses as they had already achieved all educational transitions assessed in this study. Also, the 1 respondent who was a student at T1 with less than 7 years of education was excluded as he did not make any educational advancement between baseline and follow-up. The 3 subsamples of T1 students included: 1) respondents with ≤11 years of education at T1 (n=407) for analyses of graduation from high school (transitioning from 11 to 12 years of education by T2); 2) respondents with ≤12 years of education at T1 and ≥12 years of education at T2 (n=417) for analyses of going to college (transitioning from 12 to 13 years of education by T2); and 3) respondents with ≤15 years of education at T1 and ≥13 years of education at T2 (n=404) for completing college (transitioning from 15 to 16 years of education at T2). Similarly, the 3 subsamples of T1 non-students included: 1) respondents with ≤11 years of education at T1 for analyses of graduation from high school (n=582); 2) respondents with ≤12 years of education at T1 and ≥12 years of education at T2 for the analyses of going to college (n=1,731); and 3) respondents with ≤15 years of education at T1 and >=13 years of education at T2 for analyses of graduation from college (n=1,701).
Figure 1.
Description of subsamples for analyses of the associations of mental disorders with educational attainment in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up.
The numbers of respondents in the subsamples add up to more than 5,001 because the subsamples were overlapping. The analyses included 3,954 unique respondents. The socio-demographic characteristics of the respondents in the 3 subsamples are presented in Appendix Tables A and B.
The analyses were conducted separately in student and non-student subgroups because the effect of mental disorders on continuation of schooling might be different than re-entering school. Furthermore, high school graduation, going to college and college completion represent different levels of educational ability and maturity and happen at different ages. The effect of mental disorders on educational attainment would presumably vary according to the educational level [10].
Discrete-time survival analysis models were used for these analyses. Transitions across pairs of consecutive education years were treated as separate observations clustered within individuals [35]. As noted, analyses were conducted separately for respondents who were students at T1 and those who were not.
Analyses were conducted in five stages. First, the association of each group of disorders with each of the outcomes was estimated in prediction equations that included controls for socio-demographics (age, sex, race/ethnicity, marital status, number of years of education of the major breadwinner of the family of origin). Both lifetime disorders at T1 and disorders with first onsets after T1 but before the educational outcome of interest were included in these models. Disorders with first onsets after T1 were entered into the models as time-varying variables. Second, we examined the associations of all the above disorder groups with each outcome in multivariate models having the same socio-demographic controls as in the first stage and computed separate overall χ2 tests for the joint significance of the T1 lifetime disorders and the disorders with first onsets after T1. Third, we evaluated the extent to which dose-response relationships existed between the number of mental disorders and the educational outcomes. Fourth, we evaluated the extent to which the associations of mental disorders with the educational outcomes changed when we controlled for childhood adversities. Fifth, we calculated population attributable risk proportions (PARP) of educational transitions associated with mental disorders. PARP can be interpreted as the percent with observed adverse outcomes (high school non-completion, college non-entry, college non-completion) that would have been avoided if all mental disorders could have been successfully treated or prevented based on the assumption that the survival regression coefficients accurately represent causal effects of these disorders. PARP was computed using simulation methods to generate individual-level predicted probabilities of the outcomes twice: first using all of the coefficients in the model under investigation and a second time assuming that the coefficients associated with the mental disorders were all zero. The ratio of the predicted prevalence estimates from the two specifications was then used to calculate PARP. US Census data for 2010 were used to estimate the predicted number of individuals in the US general population whose outcomes would have changed based on the estimates of PARP.
Standard errors and significance tests were estimated in each of the above steps using the Taylor series method [36] implemented in the SUDAAN software system [37] to adjust for the geographic clustering of the sample and weights. Multivariate significance was evaluated using Wald χ2 tests based on design-corrected coefficient variance-covariance matrices. Statistical significance was evaluated using two-tailed .05-level tests. All percentages reported are weighted.
RESULTS
Educational outcomes
A total of 615 (11.1%) respondents were students at T1. A majority of these students made educational transitions as of T2: 90.8% of those with less than high school graduation at T1 graduated from high school; 72.5% of those who graduated from high school entered college; and 58.4% of those who entered college graduated from college. Among T1 non-students, the corresponding percentages were 37.6%, 32.4% and 53.0%, respectively (data not shown).
Distributions of mental disorders
T1 lifetime mental disorder prevalence estimates ranged from 40.1–43.4% among T1 students to 53.5–55.7% among T1 non-students. Prevalence estimates of disorders with onsets between T1 and T2 ranged from 37.0–47.0% among T1 students and 34.8–37.6% among T1 non-students. Most mental disorder groups were strongly correlated with each other, as indicated by the high tetrachoric correlations among T1 lifetime disorders (median=.38, inter-quartile range=.29–.45) (Appendix Table C).
Associations of mental disorders with educational attainment
The four measures of T1 lifetime mental disorders and the four parallel measures of disorders with onsets after T1 were initially considered one at a time to predict each educational transition separately among T1 students and T1 non-students (i.e., a total of 48 regression models). Nine of these 48 coefficients were statistically significant at the .05 level, all showing mental disorders to be associated with decreased odds of subsequent educational transitions (Table 2). Six of the 9 involved T1 lifetime disorders and 3 disorders with onsets after T1. Five of the 9 were associated with lower odds of graduating from high school (4 among T1 students; 1 among T1 non-students), 2 with lower odds of going on to college (1 each among T1 students and non-students), and 2 with lower odds of graduating from college, both among students. Statistically significant odds-ratios were in the .17–.61 range.
Table 2.
Associations of lifetime mental disorders at T1 and first-onset disorders after T1 but before educational transitions with educational attainment at T2 in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up according to student status at T1. Each disorder group was entered into the model separately.
| Mental disorders | Students at T1 | Non-students at T1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1: graduating from high schoola (N=407) |
Model 2: going to collegeb (N=417) |
Model 3: Completing ≥4 years of collegec (N=404) |
Model 1: graduating from high schoola (N=582) |
Model 2: going to collegeb (N=1,731) |
Model 3: completing ≥4 years of collegec (N=1,701) |
|||||||
| AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | |
| T1 lifetime disorders | ||||||||||||
| Bipolar disorder | 0.21 | 0.05–0.80* | 0.51 | 0.20–1.32 | 0.60 | 0.05–7.36 | 1.12 | 0.44–2.87 | 0.34 | 0.13–0.88* | 1.02 | 0.44–2.37 |
| Any fear disorder | 0.41 | 0.16–1.02 | 0.76 | 0.37–1.56 | 0.60 | 0.36–1.01 | 0.61 | 0.39–0.95* | 1.02 | 0.75–1.41 | 0.96 | 0.75–1.24 |
| Any anxiety-misery disorder | 0.95 | 0.35–2.62 | 0.40 | 0.20–0.80* | 0.67 | 0.36–1.22 | 1.59 | 0.93–2.71 | 0.91 | 0.63–1.29 | 1.05 | 0.84–1.31 |
| Any externalizing disorder | 0.30 | 0.14–0.62** | 1.18 | 0.66–2.13 | 0.51 | 0.30–0.86* | 0.81 | 0.51–1.30 | 0.96 | 0.72–1.27 | 1.00 | 0.78–1.28 |
| Mental disorders with first onset after T1 and prior to educational transition |
||||||||||||
| Bipolar disorder | 0.69 | 0.23–2.04 | 0.52 | 0.16–1.67 | 0.32 | 0.12–0.88* | 0.37 | 0.11–1.20 | 1.47 | 0.66–3.28 | 1.22 | 0.86–1.72 |
| Any fear disorder | 0.17 | 0.08–0.34*** | 0.95 | 0.54–1.70 | 1.16 | 0.74–1.84 | 1.08 | 0.62–1.88 | 1.18 | 0.82–1.69 | 1.07 | 0.86–1.33 |
| Any anxiety-misery disorder | 0.22 | 0.06–0.73* | 0.83 | 0.35–1.93 | 0.51 | 0.25–1.02 | 0.90 | 0.39–2.07 | 1.31 | 0.79–2.16 | 1.10 | 0.78–1.56 |
| Any externalizing disorder | 0.55 | 0.21–1.43 | 0.87 | 0.46–1.64 | 0.92 | 0.54–1.54 | 0.67 | 0.42–1.08 | 0.93 | 0.58–1.47 | 0.91 | 0.60–1.38 |
Note: T1 represents the baseline National Comorbidity Survey conducted in 1990–1992 and T2, the National Comorbidity Survey-2 conducted in 2001–2003. AOR stands for adjusted odds ratio; CI for confidence interval.
Respondents with <12 years of education at T1 (students with less than 7 years of education were excluded).
Respondents with ≤12 years of education at T1 and ≥12 years of education at T2 (students with less than 7 years of education were excluded).
Respondents with ≤15 years of education at T1 and ≥13 years of education at T2 (students with less than 7 years of education were excluded).
Results are from discrete time survival models adjusting for age, sex, race/ethnicity, education level at baseline, highest education level of household bread winner when growing up, education completed at T1 and education year pairs. Each group of mental disorders was entered separately in the model, thus models did not adjust for comorbidity with disorders in other categories.
Significant at the 0.05 level, 2-sided test
Significant at the 0.001 level, 2-sided test
Significant at the 0.0001 level, 2-sided test
Surprisingly, the associations of educational outcomes with T1 lifetime disorders differed from those with first onset after T1. Specifically, among T1 lifetime disorders, bipolar disorder and externalizing disorders were associated with lower odds of graduating from high school in students; whereas, among disorders with first onsets after T1, fear and anxiety-misery disorders were the disorders associated with this outcome. Associations with going to college and graduating from college were also different for T1 lifetime disorders and disorders with first onsets after T1. Whereas lifetime anxiety-misery disorders at T1 were associated with the lower odds of going to college and T1 lifetime externalizing disorders with lower odds of graduating from college, none of the disorders with first onset after T1 were associated with going to college and only bipolar disorder with first onset after T1 was associated with the lower odds of graduating from college among students (Table 2). Among non-students, while T1 lifetime fear disorders were associated with lower odds of graduating from high school and T1 lifetime bipolar disorder was associated with lower odds of going to college, none of the disorders with onset after T1 were associated with educational outcomes at a statistically significant level (Table 2).
Results of parallel analyses in which all disorders were entered simultaneously into the models are presented in Table 3. Overall tests were statistically significant in the model predicting high school graduation among T1 students (χ28=37.4, p<.001) and non-students (χ28=18.9, p<.05) and college graduation among T1 students (χ28=35.6, p<.001) (Table 3). For T1 lifetime mental disorders, overall tests were statistically significant in models predicting going to college (χ24=10.3, p<.05) and graduating from college (χ24=13.0, p<.05) among T1 students, and graduating from high school among non-students (χ24= 12.4, p<.05) (Table 3). For disorders with first onset after T1, only overall tests for graduating from high school (χ24=19.9, p<.01) and from college (χ24=16.3, p<.01) among students were statistically significant (Table 3).
Table 3.
Associations of lifetime mental disorders at T1 and first-onset disorders after T1 but before educational transitions with educational attainment at T2 in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up according to student status at T1. All disorder groups were entered into the models at the same time.
| Mental disorders | Students at T1 | Non-students at T1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1: graduating from high schoola (N=407) |
Model 2: going to collegeb (N=417) |
Model 3: Completing ≥4 years of collegec (N=404) |
Model 1: graduating from high schoola (N=582) |
Model 2: going to collegeb (N=1,731) |
Model 3: completing ≥4 years of collegec (N=1,701) |
|||||||
| AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | AORd | 95% CI | |
| T1 lifetime disorders | ||||||||||||
| Bipolar disorder | 6.75 | 1.09–41.83* | 0.74 | 0.19–2.83 | 0.90 | 0.08–9.96 | 1.29 | 0.43–3.89 | 0.34 | 0.13–0.84* | 1.05 | 0.46–2.39 |
| Any fear disorder | 0.60 | 0.20–1.79 | 0.87 | 0.39–1.97 | 0.68 | 0.43–1.08 | 0.53 | 0.33–0.84** | 1.07 | 0.79–1.45 | 0.94 | 0.74–1.21 |
| Any anxiety-misery disorder | 1.75 | 0.42–7.31 | 0.38 | 0.18–0.82* | 0.79 | 0.42–1.50 | 1.97 | 1.14–3.38* | 0.89 | 0.62–1.27 | 1.06 | 0.85–1.32 |
| Any externalizing disorder | 0.31 | 0.12–0.80* | 1.65 | 0.94–2.89 | 0.63 | 0.37–1.06 | 0.81 | 0.50–1.32 | 0.98 | 0.75–1.27 | 0.98 | 0.77–1.25 |
| Chi-squared test for lifetime disorders at T1 (df=4) |
8.8 | 10.3* | 13.0* | 12.4* | 7.9 | 0.4 | ||||||
| Mental disorders with first onset after T1 and prior to educational transition |
||||||||||||
| Bipolar disorder | 1.49 | 0.16–14.01 | 0.69 | 0.22–2.11 | 0.33 | 0.13–0.85* | 0.35 | 0.09–1.30 | 1.45 | 0.61–3.45 | 1.20 | 0.84–1.70 |
| Any fear disorder | 0.19 | 0.08–0.44*** | 1.11 | 0.63–1.94 | 1.55 | 0.91–2.65 | 1.20 | 0.65–2.23 | 1.15 | 0.78–1.68 | 1.04 | 0.83–1.29 |
| Any anxiety-misery disorder | 0.27 | 0.06–1.22 | 0.76 | 0.31–1.84 | 0.47 | 0.23–0.96 | 0.94 | 0.37–2.43 | 1.35 | 0.82–2.23 | 1.11 | 0.77–1.59 |
| Any externalizing disorder | 0.62 | 0.27–1.42 | 0.95 | 0.49–1.85 | 1.04 | 0.63–1.72 | 0.67 | 0.42–1.05 | 0.92 | 0.59–1.45 | 0.89 | 0.58–1.38 |
| Chi-squared tests for disorders with onset after T1 prior to educational transition (df=4) |
19.9** | 1.1 | 16.3** | 5.2 | 3.0 | 1.4 | ||||||
| Overall chi-squared test (df=8) |
37.4*** | 11.9 | 35.6*** | 18.9* | 12.0 | 2.0 | ||||||
Note: T1 represents the baseline National Comorbidity Survey conducted in 1990–1992 and T2, the National Comorbidity Survey-2 conducted in 2001–2003. AOR stands for adjusted odds ratio; CI for confidence interval.
Respondents with <12 years of education at T1 (students with less than 7 years of education were excluded).
Respondents with ≤12 years of education at T1 and ≥12 years of education at T2 (students with less than 7 years of education were excluded).
Respondents with ≤15 years of education at T1 and ≥13 years of education at T2 (students with less than 7 years of education were excluded).
Results are from discrete time survival models adjusting for age, sex, race/ethnicity, education level at baseline, highest education level of household bread winner when growing up, education completed at T1 and education year pairs. All groups of mental disorders was entered simultaneously in the model.
Significant at the 0.05 level, 2-sided test
Significant at the 0.001 level, 2-sided test
Significant at the 0.0001 level, 2-sided test
Results for individual disorder groups in the analyses presented in Table 3 were largely consistent with the results of analyses in which disorder groups were entered individually (Table 2). However, the adjusted odds ratios for the association of bipolar disorder with high school graduation among T1 students was significantly larger than one (AOR=6.75, 95% CI=1.09–41.83). Similarly, in the model adjusting for all disorder groups, the association of lifetime anxiety-misery disorders with high school graduation was significantly larger than one (AOR=1.97, 95% CI=1.14–3.38), suggesting that these disorders may enhance high school graduation when other disorder groups are simultaneously taken into account.
The associations of T1 lifetime disorders with educational outcomes were for the most part not affected by controlling for childhood adversities. Furthermore, childhood adversities were not associated with educational outcomes at a statistically significant level in any of the models (data not shown). Adding the number of each of the T1 lifetime disorders to the regression models explained some of the variance in the model for going to college among T1 non-students (χ23=8.6, p=.035). The number of fear disorders in this model was associated with lower odds of going to college even after adjusting for the binary variable indicating any fear disorders (AOR=.65, 95% CI=.48–.88).
Population attributable risk proportions
The PARPs associated with mental disorders predicting educational outcomes are presented in Table 4. The largest PARPs were for graduating from college (11.4%) among T1 students and for graduating from high school among T1 non-students (11.0%). These estimates suggest that if all mental disorders could be prevented or treated so that they would not impact educational attainment, 11.4% more of current college students would graduate from college within 10 years or that 11% more of those who have experienced a gap in education before graduating from high school would go on to later graduate from high school.
Table 4.
Population Attributable Risk Proportion (PARP) associated with lifetime mental disorders at T1 and first-onset mental disorders after T1 but before educational transitions with educational attainment at T2 in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up according to student status at T1.
| Mental disorders | Students at T1 | Non-students at T1 | ||||
|---|---|---|---|---|---|---|
| Model 1: graduating from high schoola (N=407) |
Model 2: going to collegeb (N=417) |
Model 3: Completing ≥4 years of collegec (N=404) |
Model 1: graduating from high schoola (N=582) |
Model 2: going to collegeb (N=1,731) |
Model 3: completing ≥4 years of collegec (N=1,701) |
|
| Any lifetime mental disorder at T1 |
1.89 | 2.41 | 9.26 | 6.99 | 2.73 | 0.65 |
| Any mental disorder with first onset after T1 but prior to educational transition |
4.63 | 0.83 | 1.83 | 3.58 | −4.12 | −1.16 |
| Any lifetime mental disorder at T1 or first onset after T1 but prior to educational transition |
5.84 | 3.20 | 11.41 | 10.95 | −1.52 | −0.51 |
Note: T1 represents the baseline National Comorbidity Survey conducted in 1990–1992 and T2, the National Comorbidity Survey-2 conducted in 2001–2003.
Respondents with <12 years of education at T1 (students with less than 7 years of education were excluded).
Respondents with ≤12 years of education at T1 and ≥12 years of education at T2 (students with less than 7 years of education were excluded).
Respondents with ≤15 years of education at T1 and ≥13 years of education at T2 (students with less than 7 years of education were excluded).
We used data from the 2010 census of the US population to estimate the actual number of individuals that these PARPs would translate into. In 2010 a total of 161,902,094 Americans were between ages 15 and 54, the age range of NCS respondents (http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf). Assuming that 8.1% of these individuals were students with less than a high school degree in that year (based on NCS estimates) and a 90.8% prevalence of high school graduation when assessed 10 years later (based on NCS-2 data), a PARP of 5.84 translates into over 698,000 more individuals graduating from high school if the effects of mental disorders can be fully removed or prevented. Removing the effect of mental disorders on college entry and graduation would similarly result in 313,000 more current students entering college, and more than 850,000 current college students finishing college. Among the non-students with less than high school education, removing the effect of mental disorders will result in 555,000 more individuals earning a high school degree or equivalent in future years.
DISCUSSION
The associations found in this study are smaller than those obtained in previous analyses of the cross-sectional NCS data [14]. This may be due to differences in analytic approach. The earlier NCS analyses used retrospective methods while we used prospective methods in the current report. Retrospective reporting bias might have inflated the earlier NCS results. Despite the fact that the associations found here are weaker than in previous NCS analyses, the PARP estimates obtained here are in line with those for a similar range of mental disorders in a study based on data from 9 of the countries participating in the World Mental Health (WMH) survey [10], in which PARP estimates ranged from 0 to 11.37 for non-completion of high school, −0.05 to 4.65 for non-entry into college, and 0 to 2.64 for non-completion of college [10]. The similarities among these findings with those in the present study are more remarkable than the discrepancies and point to the existence of modest but consistent associations between mental disorders and subsequent educational attainment across many countries. However, due to the minimum age of NCS respondents (15 years) and the mandatory educational rules in the US we could not assess the impact of mental disorders on non-completion of primary education, an outcome for which the WMH study found very large associations for substance disorders.
Much of the past research on the impact of mental disorders on educational attainment has focused on depression [38,22,7,8,21], which was the most common disorder in the category of internalizing anxiety-misery disorders in the present study. However, the associations with education were not limited to this category of disorders. Furthermore, no groups of disorders were consistently associated with transitions across all levels of education. Fear disorders, for example, appeared to be significantly associated only with graduation from high school. Social phobia was the most common disorder in this category. In contrast, bipolar disorder appeared to be associated with educational transitions across all education levels.
It is also notable that the association of mental disorders with educational transitions appeared to be generally larger among respondents who were students at T1, especially high school students, and who participants who were typically younger. Seven of the 9 statistically significant associations in Table 2 were in the student group even though the non-student subsamples were larger in size. Thus, the effects of mental disorders on educational attainment appear to be more marked in the younger age groups. While this pattern of findings is expected with regard to externalizing disorders, with alcohol disorders being the most common disorders in this category, the finding with regard to other disorders perhaps highlights the greater ability of older students to cope with the effects of mental illness. It is also possible that respondents with more severe and impairing conditions never achieve the earlier educational transitions and thus are not eligible for future transition. Again, the finding of generally stronger associations among high school students supports this conclusion. These findings high-light the importance of early interventions to reduce the impact of mental disorder on outcomes across levels of education.
We found different patterns of associations with educational outcomes for mental disorders assessed retrospectively at T2 compared to T1 lifetime disorders. This discrepancy might reflect recall bias. It is also possible that differences in time since onset of the disorder to the outcome has influenced the results. T1 lifetime disorders could have had onsets many years before T1, whereas disorders with first onset after T1 were more recent. The effects of recent-onset disorders may be different than the effect of disorders with onset in the remote past. Finally, age-of-onset may moderate the association of mental disorders with educational and other social outcomes [39], a possibility that we could not assess in NCS panel due to inadequate statistical power. Many lifetime fear disorders in NCS had very early ages of onset [40]; whereas, first onset disorders after T1, by definition started after age 15 years.
This study had several strengths including a relatively large sample size, longitudinal design with excellent follow-up, and the use of structured interview instruments at two time points. The excellent follow-up rate was made possible by the use of exhaustive tracing procedures developed by SRC over the years in conjunction with their landmark long-term panel surveys (e.g., Panel Study of Income Dynamics, the Health and Retirement Study). The study also had a number of noteworthy limitations. First, despite the large sample size of the study, the number of respondents with individual mental disorders was too small to provide reliable estimates, requiring us to combine individual disorders into groups. Even after aggregating disorders in groups, samples for some groups were rather small for the analyses, resulting in very large confidence intervals for the some of the odds ratios. These results need to be replicated in studies including larger samples. Second, the mental disorders assessed in the NCS were incomplete and did not include psychotic disorders, attention-deficit/hyperactivity disorder, or personality disorders, which likely impact educational attainment. We also did not examine the impact of subthreshold disorders that may be associated with significant morbidity and impairment in functioning including academic functioning [41–43]. Thus, our estimate of the effect of mental disorders on educational outcomes is likely an underestimate of the total effect of all mental health morbidities. Third, although the analyses adjusted for socio-demographic and childhood adversities, the possibility of residual confounding by unmeasured or imperfectly measured variables limits causal inference. For example, social adversities besides the ones measured in NCS, childhood physical health conditions and socio-economic status not captured by the breadwinner’s education may all influence both the risk of mental disorders as well as educational outcomes. Fourth, we did not assess student performance or grade point averages, both of which could have been affected by mental disorders, although these associations were presumably picked up to some extent by the fact that poor educational performance is a major contributor to school drop-out as well as a risk factor for mental disorders [44,45]. Finally, assessment of educational attainment was based on reports of the number of completed years of schooling, not the level achieved. Years of schooling is not a perfect measure of educational attainment as some individual may have been held back in the same level for 1 year or longer.
In the context of these limitations, the findings highlight potentially significant associations between mental disorders and educational attainment. Research on treatment and prevention programs for child and adolescent mental disorders has produced promising results regarding the impact on education [46–51]. However, many schools lack adequate resources to effectively identify youth at risk or means to implement evidence-based prevention and treatment programs [52]. Even where these resources are available, many students do not access them because of stigma, low mental health literacy or because of not knowing about available resources [53]. As a result, there is a large unmet need for mental health care among both high school and college students [38,54,55]. Effective prevention of the harmful effects of mental health problems on the students’ educational attainment would likely depend on close collaboration of families, schools, healthcare system and often, social services, to detect these problems early on and to intervene effectively before they have caused significant disruption in schooling.
Increased detection and treatment of mental disorders is only one factor among many that may reduce the societal burden of educational curtailment. Treatment of mental health conditions in children and adolescents has increased in the years since early 2000s when the NCS-2 was conducted [56]. Yet, a 2010 study by Heckman and Lafontaine found a steady decline in the high school graduation rates in the US since 1970s [57]. Social and economic changes in the past decade, and especially the economic crisis of 2007 all likely impacted financial access to education [58,59]. Other social and institutional factors such as the quality of school programs and the ability of these programs to meet the student needs have also been shown to be associated with school completion [60] and may have changed over the years. The effect of individual mental health problems on educational attainment is best understood in this wider context. Initiatives to improve detection of mental disorders and access to mental health treatments can potentially be combined with broader academic, social and economic prevention programs aimed at retaining students in school [61–64].
Table 1.
Prevalence of lifetime mental disorders at T1 and first-onset disorders after T1 but before educational transitions in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up according to student status at T1.
| Mental disorders | Students at T1 | Non-students at T1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subsample 1: graduating from high schoola (N=407) |
Subsample 2: going to collegeb (N=417) |
Subsample 3: Completing ≥4 years of collegec (N=404) |
Subsample 1: graduating from high schoola (N=582) |
Subsample 2: going to collegeb (N=1,731) |
Subsample 3: completing ≥4 years of collegec (N=1,701) |
|||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| T1 lifetime disorders | ||||||||||||
| Bipolar disorder | 5 | 1.4 | 6 | 1.4 | 3 | 1.0 | 18 | 2.8 | 40 | 1.9 | 39 | 1.6 |
| Any fear disorder | 104 | 24.5 | 102 | 24.1 | 92 | 22.1 | 204 | 26.9 | 579 | 25.7 | 549 | 24.3 |
| Any anxiety-misery disorder | 61 | 14.2 | 65 | 15.6 | 60 | 14.2 | 176 | 21.5 | 518 | 23.9 | 552 | 22.7 |
| Any externalizing disorder | 84 | 17.9 | 83 | 17.2 | 95 | 22.5 | 297 | 39.8 | 796 | 35.2 | 773 | 33.1 |
| Any mental disorders | 177 | 40.2 | 177 | 40.1 | 182 | 43.4 | 424 | 55.7 | 1232 | 55.9 | 1225 | 53.5 |
| Mental disorders with first onset after T1 and prior to educational transition |
||||||||||||
| Bipolar disorder | 23 | 4.6 | 23 | 4.7 | 17 | 3.1 | 35 | 4.0 | 77 | 3.5 | 80 | 4.8 |
| Any fear disorder | 75 | 19.4 | 74 | 18.1 | 71 | 19.0 | 166 | 23.2 | 364 | 18.7 | 341 | 18.6 |
| Any anxiety-misery disorder | 33 | 8.2 | 37 | 8.8 | 49 | 12.9 | 74 | 10.7 | 191 | 10.0 | 189 | 10.2 |
| Any externalizing disorder | 83 | 19.4 | 102 | 22.8 | 113 | 29.1 | 90 | 13.2 | 252 | 13.9 | 230 | 11.6 |
| Any mental disorders | 159 | 38.3 | 174 | 41.1 | 185 | 48.4 | 259 | 37.4 | 675 | 36.4 | 639 | 33.8 |
Note: T1 represents the baseline National Comorbidity Survey conducted in 1990–1992 and T2, the National Comorbidity Survey-2 conducted in 2001–2003.
Respondents with <12 years of education at T1 (students with less than 7 years of education were excluded).
Respondents with ≤12 years of education at T1 and ≥12 years of education at T2 (students with less than 7 years of education were excluded).
Respondents with ≤15 years of education at T1 and ≥13 years of education at T2 (students with less than 7 years of education were excluded).
Acknowledgments
FINANCIAL SUPPORT
The secondary analysis of the NCS/NCS-2 data reported here was supported by National Institute of Mental Health (NIMH) (RM PI; grant number R01MH096826). The NCS data collection was also supported by NIMH (RCK PI; grant number R01MH46376), while NCS-2 data collection was supported by the National Institute on Drug Abuse (RCK PI; grant number R01DA012058). The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or U.S. Government. A complete list of NCS and NCS-2 publications can be found at http://www.hcp.med.harvard.edu/ncs. The NCS-2 is carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centres for assistance with instrumentation, fieldwork, and consultation on data analysis. These activities were supported by the NIMH (R.C.K., grant number R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R.C.K., grant numbers R13MH066849, R01MH069864, and R01DA016558), the Fogarty International Center (R.C.K., R03TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
ETHICAL STANDARDS
Original collection of NCS and NCS-2 data has been approved by the Institutional Review Board of Harvard University and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The analyses reported here have been approved by the Institutional Review Board of Johns Hopkins University, Bloomberg School of Public Health. All persons interviewed for NCS and NCS-2 surveys gave their informed consent prior to their inclusion in the study.
Dr. Mojtabai has received research funding from Bristol Myers-Squibb and Lundbeck pharmaceuticals. In the past 12 months, Dr. Kessler has served as a consultant for Hoffmann-La Roche, Inc. and the Johnson & Johnson Wellness and Prevention. Dr. Kessler has served on advisory boards for Mensante Corporation, Johnson & Johnson Services Inc. Lake Nona Life Project, and U.S. Preventive Medicine. Dr. Kessler owns 25% share in DataStat, Inc.
Appendix
Appendix Table A.
Socio-demographic characteristics of respondents of National Comorbidity Survey and National Comorbidity Survey follow-up who were students at T1.
| Subsample 1: 7–11 years of education at Time 1 N=407 |
Subsample 2: 7–12 years of education at Time 1 and 12 or more years of education at Time 2 N=417 |
Subsample 3: 7–15 years of education at Time 1 and 13 or more years of education at Time 2 N=404 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SE | IQR | N | Mean | SE | IQR | N | Mean | SE | IQR | |
| Age at Time 1 | 407 | 16.2 | 0.1 | 15–17 | 417 | 16.5 | 0.1 | 15–17 | 404 | 17.4 | 0.2 | 16–18 |
| Years of education at Time 1 |
407 | 9.8 | 0.1 | 9–11 | 417 | 10.1 | 0.1 | 9–11 | 404 | 10.9 | 0.1 | 9–12 |
| Number of years of education of the major bread winner |
407 | 11.7 | 0.3 | 11–16 | 417 | 12.1 | 0.3 | 12–16 | 404 | 13.1 | 0.3 | 12–16 |
| N | % | SE | N | % | SE | N | % | SE | ||||
| Marital status | ||||||||||||
| Married / Cohabitating | 5 | 1.3 | 0.7 | 10 | 2.2 | 1.0 | 15 | 2.8 | 0.9 | |||
| Separated / Widowed/ Divorced |
5 | 0.8 | 0.5 | 4 | 0.7 | 0.5 | 8 | 1.6 | 0.8 | |||
| Never Married | 397 | 97.9 | 0.9 | 403 | 97.0 | 1.1 | 381 | 95.6 | 1.1 | |||
| Gender | ||||||||||||
| Male | 200 | 52.2 | 2.4 | 203 | 50.3 | 2.5 | 201 | 53.1 | 2.5 | |||
| Female | 207 | 47.8 | 2.4 | 214 | 49.7 | 2.5 | 203 | 46.9 | 2.5 | |||
| Race/ethnicity | ||||||||||||
| Hispanic | 69 | 17.8 | 3.6 | 65 | 15.6 | 3.7 | 49 | 11.6 | 2.6 | |||
| Non-Hispanic black | 53 | 12.6 | 1.9 | 47 | 11.3 | 1.9 | 38 | 9.2 | 1.8 | |||
| Non-Hispanic other | 13 | 3.6 | 1.2 | 12 | 3.9 | 1.2 | 20 | 5.6 | 1.5 | |||
| Non-Hispanic white | 272 | 66.0 | 3.8 | 293 | 69.2 | 3.9 | 297 | 73.6 | 3.3 | |||
Note SE stands for standard error; IQR stands for interquartile range (25th to 75th percentile).
Appendix Table B.
Socio-demographic characteristics of respondents of National Comorbidity Survey and National Comorbidity Survey follow-up who were not students at T1.
|
Subsample 1: 0–11 years of education at Time 1 N=582 |
Subsample 2: 0–12 years of education at Time 1 and 12 or more years of education at Time 2 N=1,731 |
Subsample 3: 0–15 years of education at Time 1 and 13 or more years of education at Time 2 N=1,701 |
||||||||||
| N | Mean | SE | IQR | N | Mean | SE | IQR | N | Mean | SE | IQR | |
| Age at Time 1 | 582 | 34.7 | 0.7 | 26–44 | 1731 | 34.0 | 0.3 | 26–42 | 1701 | 33.2 | 0.4 | 25–40 |
| Years of education at Time 1 |
582 | 9.5 | 0.2 | 9–11 | 1731 | 11.8 | 0.0 | 12–12 | 1701 | 13.2 | 0.0 | 12–14 |
| Number of years of education of the major bread winner |
582 | 5.8 | 0.3 | 0–11 | 1731 | 9.0 | 0.2 | 7–12 | 1701 | 10.6 | 0.2 | 8–13 |
| N | % | SE | N | % | SE | N | % | SE | ||||
| Marital status | ||||||||||||
| Married / Cohabitating | 335 | 5.3 | 2.5 | 1006 | 66.3 | 2.1 | 886 | 59.5 | 2.2 | |||
| Separated / Widowed / Divorced |
100 | 14.9 | 2.2 | 287 | 12.6 | 1.5 | 274 | 13.6 | 1.5 | |||
| Never Married | 147 | 19.9 | 2.0 | 438 | 21.1 | 1.6 | 541 | 26.9 | 1.7 | |||
| Gender | ||||||||||||
| Male | 281 | 54.2 | 3.1 | 797 | 48.4 | 1.9 | 745 | 46.6 | 1.9 | |||
| Female | 301 | 45.8 | 3.1 | 934 | 51.6 | 1.9 | 956 | 53.4 | 1.9 | |||
| Race/ethnicity | ||||||||||||
| Hispanic | 79 | 19.7 | 4.1 | 142 | 9.4 | 2.5 | 144 | 9.8 | 2.0 | |||
| Non-Hispanic black | 72 | 13.3 | 2.9 | 178 | 11.6 | 1.4 | 200 | 14.9 | 1.6 | |||
| Non-Hispanic other | 19 | 3.3 | 1.1 | 44 | 3.0 | 0.9 | 45 | 2.8 | 0.8 | |||
| Non-Hispanic white | 412 | 63.7 | 4.7 | 1367 | 76.0 | 3.2 | 1312 | 72.4 | 2.2 | |||
Note SE stands for standard error; IQR stands for interquartile range (25th to 75th percentile).
Appendix Table C.
Tetrachoric correlations among mental disorder categories in respondents of National Comorbidity Survey and National Comorbidity Survey follow-up according to student status at T1.
| Mental disorders | Bipolar disorder |
Any fear disorder |
Any anxiety- misery disorder |
Any externalizing disorder |
|---|---|---|---|---|
| Students -Model 1a | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.98 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.11 | 0.41 | 1.00 | . |
| Any externalizing disorder | 0.53 | 0.41 | 0.31 | 1.00 |
| Students-Model 2b | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.30 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.56 | 0.42 | 1.00 | . |
| Any externalizing disorder | 0.16 | 0.39 | 0.41 | 1.00 |
| Students-Model 3c | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.22 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.62 | 0.36 | 1.00 | . |
| Any externalizing disorder | −0.04 | 0.23 | 0.24 | 1.00 |
| Non-students-Model 1d | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.40 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.30 | 0.46 | 1.00 | . |
| Any externalizing disorder | 0.72 | 0.34 | 0.29 | 1.00 |
| Non-students-Model 2e | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.45 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.45 | 0.45 | 1.00 | . |
| Any externalizing disorder | 0.41 | 0.23 | 0.29 | 1.00 |
| Non-students-Model 3f | ||||
| Bipolar disorder | 1.00 | . | . | . |
| Any fear disorder | 0.48 | 1.00 | . | . |
| Any anxiety-misery disorder | 0.27 | 0.49 | 1.00 | . |
| Any externalizing disorder | 0.37 | 0.24 | 0.29 | 1.00 |
Note: T1 represents the baseline National Comorbidity Survey conducted in 1990–1992 and T2, the National Comorbidity Survey-2 conducted in 2001–2003.
. Students with 7–11 years of education at T1.
. Students with 7–12 years of education at T1 and ≥12 years of education at T2.
. Students with 7–15 years of education at T1 and ≥13 years of education of education at T2.
. Non-student respondents with <12 years of education at T1.
. Non-student respondents with ≤12 years of education at T1 and ≥12 years of education at T2.
. Non-student respondents with ≤15 years of education at T1 and ≥13 years of education at T2.
Footnotes
CONFLICT OF INTEREST
Other authors declare no potential conflict of interest.
REFERENCES
- 1.Ryan CL, Siebens J. Educational Attainment in the United States: 2009. Current Population Reports. 2012 https://www.census.gov/prod/2012pubs/p20-566.pdf.
- 2.Dubow EF, Huesmann LR, Boxer P, Pulkkinen L, Kokko K. Middle childhood and adolescent contextual and personal predictors of adult educational and occupational outcomes: a mediational model in two countries. Developmental Psychology. 2006;42(5):937–949. doi: 10.1037/0012-1649.42.5.937. [DOI] [PubMed] [Google Scholar]
- 3.Featherman D. Schooling and occupational careers: Constancy and change in worldly success. In: Brim O, Kagan J, editors. Constancy and change in human development. Cambridge, Mass: Harvard University Press; 1980. [Google Scholar]
- 4.Avery C, Turner S. Student loans: Do college students borrow too much—or not enough? The Journal of Economic Perspectives. 2012;26:165–192. [Google Scholar]
- 5.Escobedo LG, Peddicord JP. Smoking prevalence in US birth cohorts: the influence of gender and education. American Journal of Public Health. 1996;86(2):231–236. doi: 10.2105/ajph.86.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shea S, Stein AD, Basch CE, Lantigua R, Maylahn C, Strogatz DS, Novick L. Independent associations of educational attainment and ethnicity with behavioral risk factors for cardiovascular disease. American Journal of Epidemiology. 1991;134(6):567–582. doi: 10.1093/oxfordjournals.aje.a116130. [DOI] [PubMed] [Google Scholar]
- 7.Fletcher JM. Adolescent depression: diagnosis, treatment, and educational attainment. Health Economics. 2008;17(11):1215–1235. doi: 10.1002/hec.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fletcher JM. Adolescent depression and educational attainment: results using sibling fixed effects. Health Economics. 2010;19(7):855–871. doi: 10.1002/hec.1526. [DOI] [PubMed] [Google Scholar]
- 9.Johnson JG, Cohen P, Dohrenwend BP, Link BG, Brook JS. A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. Journal of Abnormal Psychology. 1999;108(3):490–499. doi: 10.1037//0021-843x.108.3.490. [DOI] [PubMed] [Google Scholar]
- 10.Lee S, Tsang A, Breslau J, Aguilar-Gaxiola S, Angermeyer M, Borges G, Bromet E, Bruffaerts R, de Girolamo G, Fayyad J, Gureje O, Haro JM, Kawakami N, Levinson D, Oakley Browne MA, Ormel J, Posada-Villa J, Williams DR, Kessler RC. Mental disorders and termination of education in high-income and low- and middle-income countries: epidemiological study. British Journal of Psychiatry. 2009;194(5):411–417. doi: 10.1192/bjp.bp.108.054841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miech RA, Caspi A, Moffitt TE, Wright BRE, Silva PA. Low Socioeconomic Status and Mental Disorders: A Longitudinal Study of Selection and Causation during Young Adulthood 1. American Journal of Sociology. 1999;104(4):1096–1131. [Google Scholar]
- 12.Breslau J, Lane M, Sampson N, Kessler RC. Mental disorders and subsequent educational attainment in a US national sample. Journal of Psychiatric Research. 2008;42(9):708–716. doi: 10.1016/j.jpsychires.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau J, Miller E, Jin R, Sampson NA, Alonso J, Andrade LH, Bromet EJ, de Girolamo G, Demyttenaere K, Fayyad J, Fukao A, Galaon M, Gureje O, He Y, Hinkov HR, Hu C, Kovess-Masfety V, Matschinger H, Medina-Mora ME, Ormel J, Posada-Villa J, Sagar R, Scott KM, Kessler RC. A multinational study of mental disorders, marriage, and divorce. Acta Psychiatrica Scandinavica. 2011;124:474–486. doi: 10.1111/j.1600-0447.2011.01712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: Educational attainment. American Journal of Psychiatry. 1995;152(7):1026–1032. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 15.Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(9):1086–1093. doi: 10.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Freudenberg N, Ruglis J. Reframing school dropout as a public health issue. Preventing Chronic Disease. 2007;4:A107. [PMC free article] [PubMed] [Google Scholar]
- 17.Wichstrøm L. Alcohol intoxication and school dropout. Drug and Alcohol Review. 1998;17(4):413–421. doi: 10.1080/09595239800187251. [DOI] [PubMed] [Google Scholar]
- 18.Fergusson DM, Woodward LJ. Educational, psychosocial, and sexual outcomes of girls with conduct problems in early adolescence. Journal of Child Psychology and Psychiatry. 2000;41(6):779–792. [PubMed] [Google Scholar]
- 19.Fergusson DM, Horwood LJ. Early conduct problems and later life opportunities. Journal of Child Psychology and Psychiatry. 1998;39(8):1097–1108. [PubMed] [Google Scholar]
- 20.Jennison KM. The short-term effects and unintended long-term consequences of binge drinking in college: a 10-year follow-up study. The American Journal of Drug and Alcohol Abuse. 2004;30(3):659–684. doi: 10.1081/ada-200032331. [DOI] [PubMed] [Google Scholar]
- 21.Jonsson U, Goodman A, von Knorring A-L, von Knorring L, Koupil I. School performance and hospital admission due to unipolar depression: a three-generational study of social causation and social selection. Social psychiatry and psychiatric epidemiology. 2012;47(10):1695–1706. doi: 10.1007/s00127-012-0476-y. [DOI] [PubMed] [Google Scholar]
- 22.Fergusson DM, Woodward LJ. Mental health, educational, and social role outcomes of adolescents with depression. Archives of General Psychiatry. 2002;59(3):225. doi: 10.1001/archpsyc.59.3.225. [DOI] [PubMed] [Google Scholar]
- 23.Eggert LL, Thompson EA, Herting JR, Nicholas LJ. Preventing adolescent drug abuse and high school dropout through an intensive school-based social network development program. American Journal of Health Promotion. 1994;8:202–215. doi: 10.4278/0890-1171-8.3.202. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 25.Rubin DB. Propensity score methods. American Journal of Ophthalmology. 2010;149(1):7–9. doi: 10.1016/j.ajo.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 26.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, et al. The Composite International Diagnostic Interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry. 1988;45(12):1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 29.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 30.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: History, rationale, and description. Archives of General Psychiatry. 1992;49(8):624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research. New York, NY: New York State Psychiatric Institute; 2002. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) [Google Scholar]
- 32.Kessler RC, Wittchen HU, Abelson JM, Mcgonagle K, Schwarz N, Kendler KS, Knäuper B, Zhao S. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US national comorbidity survey (NCS) International Journal of Methods in Psychiatric Research. 1998;7(1):33–55. [Google Scholar]
- 33.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, Lepine JP, Mazzi F, Reneses B, Vilagut G, Sampson NA, Kessler RC. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. International Journal of Methods in Psychiatric Research. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27(5):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- 35.Willett JB, Singer JD. Investigating onset, cessation, relapse, and recovery: why you should, and how you can, use discrete-time survival analysis to examine event occurrence. Journal of Consulting and Clinical Psychology. 1993;61(6):952–965. doi: 10.1037//0022-006x.61.6.952. [DOI] [PubMed] [Google Scholar]
- 36.Wolter KM. Statistics for social and behavioral sciences. 2nd. New York: Springer; 2007. Introduction to Variance Estimation. [Google Scholar]
- 37.Research Triangle Institute. SUDAAN: Professional Software for Survey Data Analysis, 9.0. Research Triangle Park, NC: Research Triangle Institute; 2004. [Google Scholar]
- 38.Eisenberg D, Chung H. Adequacy of depression treatment among college students in the United States. General Hospital Psychiatry. 2012;34(3):213–220. doi: 10.1016/j.genhosppsych.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Kessler RC, Stein MB, Berglund P. Social phobia subtypes in the National Comorbidity Survey. American Journal of Psychiatry. 1998;155(5):613–619. doi: 10.1176/ajp.155.5.613. [DOI] [PubMed] [Google Scholar]
- 40.Magee WJ, Eaton WW, Wittchen H-U, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Archives of General Psychiatry. 1996;53(2):159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- 41.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62(1):66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 42.Kadesjö B, Gillberg C. The comorbidity of ADHD in the general population of Swedish school-age children. Journal of Child Psychology and Psychiatry. 2001;42(04):487–492. [PubMed] [Google Scholar]
- 43.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of "subthreshold" depressive symptoms. Journal of abnormal psychology. 2000;109(2):345. [PubMed] [Google Scholar]
- 44.Chassin L. Adolescent substance use and abuse. Advances in Child Behavioral Analysis & Therapy. 1984;3:99–152. [Google Scholar]
- 45.Rosenberg M, Schooler C, Schoenbach C. Self-esteem and adolescent problems: Modeling reciprocal effects. American Sociological Review. 1989;54:1004–1018. [Google Scholar]
- 46.Sinclair MF, Christenson SL, Elevo DL, Hurley CM. Dropout prevention for youth with disabilities: Efficacy of a sustained school engagement procedure. Exceptional Children. 1998;65:7–21. [Google Scholar]
- 47.Balfanz R, Herzog L, Mac Iver DJ. Preventing student disengagement and keeping students on the graduation path in urban middle-grades schools: Early identification and effective interventions. Educational Psychologist. 2007;42(4):223–235. [Google Scholar]
- 48.Hawken LS, Horner RH. Evaluation of a targeted intervention within a schoolwide system of behavior support. Journal of Behavioral Education. 2003;12(3):225–240. [Google Scholar]
- 49.Prevatt F, Kelly FD. Dropping out of school: A review of intervention programs. Journal of School Psychology. 2003;41(5):377–395. [Google Scholar]
- 50.Wilson SJ, Tanner-Smith EE, Lipsey MW, Steinka-Fry K, Morrison J. Dropout Prevention and Intervention Programs: Effects on School Completion and Dropout among School-Aged Children and Youth. Campbell Systematic Reviews. 2011 http://files.eric.ed.gov/fulltext/ED519121.pdf.
- 51.Chung H, Klein MC, Silverman D, Corson-Rikert J, Davidson E, Ellis P, Kasnakian C. A pilot for improving depression care on college campuses: results of the College Breakthrough Series–Depression (CBS-D) Project. Journal of American College Health. 2011;59(7):628–639. doi: 10.1080/07448481.2010.528097. [DOI] [PubMed] [Google Scholar]
- 52.Langley AK, Nadeem E, Kataoka SH, Stein BD, Jaycox LH. Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health. 2010;2(3):105–113. doi: 10.1007/s12310-010-9038-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eisenberg D, Golberstein E, Gollust SE. Help-seeking and access to mental health care in a university student population. Medical Care. 2007;45(7):594–601. doi: 10.1097/MLR.0b013e31803bb4c1. [DOI] [PubMed] [Google Scholar]
- 54.Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health. 2010;46(1):3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 55.Said D, Kypri K, Bowman J. Risk factors for mental disorder among university students in Australia: findings from a web-based cross-sectional survey. Social Psychiatry and Psychiatric Epidemiology. 2013;48(6):935–944. doi: 10.1007/s00127-012-0574-x. [DOI] [PubMed] [Google Scholar]
- 56.Olfson M, Blanco C, Wang S, Laje G, Correll CU. National trends in the mental health care of children, adolescents, and adults by office-based physicians. JAMA Psychiatry. 2014;71(1):81–90. doi: 10.1001/jamapsychiatry.2013.3074. [DOI] [PubMed] [Google Scholar]
- 57.Heckman JJ, LaFontaine PA. The American high school graduation rate: Trends and levels. The review of economics and statistics. 2010;92(2):244–262. doi: 10.1162/rest.2010.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pan W, Ost B. The impact of parental layoff on higher education investment. Economics of Education Review. 2014;42:53–63. [Google Scholar]
- 59.Greenglass E, Antonides G, Christandl F, Foster G, Katter JK, Kaufman BE, Lea SE. The financial crisis and its effects: Perspectives from economics and psychology. Journal of Behavioral and Experimental Economics. 2014;50:10–12. [Google Scholar]
- 60.Rumberger R, Lim SA. Why students drop out of school: A review of 25 years of research. Santa Barbara, CA: California Dropout Research Project; 2008. http://cdrp.ucsb.edu/dropouts/pubs_reports.htm. [Google Scholar]
- 61.Hardre PL, Reeve J. A motivational model of rural students' intentions to persist in versus drop out of, high school. Journal of educational psychology. 2003;95(2):347. [Google Scholar]
- 62.Somers CL, Piliawsky M. Drop-Out Prevention among Urban, African American Adolescents: Program Evaluation and Practical Implications. Preventing School Failure. 2004;48(3):17–22. [Google Scholar]
- 63.Christenson SL, Thurlow ML. School dropouts prevention considerations, interventions, and challenges. Curr Dir Psychol Sci. 2004;13(1):36–39. [Google Scholar]
- 64.Rumberger RW. Why students drop out of school and what can be done. Paper presented at the Dropouts in America: How Severe is the Problem? What Do We Know about Intervention and Prevention?; January 13, 2001; Harvard University. 2001. [Google Scholar]